Abstract
Background
Use of targeted therapy for human epidermal growth factor receptor-2 (HER2)-positive breast cancer has led to improvements in survival. Furthermore, neoadjuvant chemotherapy (NAC) with dual HER2 agents demonstrated improved pathological complete response (pCR) rates. With these data, and with US FDA approval in September 2013 of pertuzumab in the neoadjuvant setting, we hypothesized that the use of NAC for early-stage HER2-positive patients is increasing.
Methods
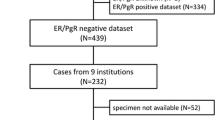
With Institutional Review Board approval, we reviewed 267 patients with 268 clinical T1 and T2 HER2-positive tumors treated from October 2008 to September 2014. We compared treatment in the early (October 2008–September 2013) to recent (October 2013–September 2014) periods. Statistical analysis was performed using Chi square tests.
Results
Mean patient age was 59 years. Clinical T stage included 6 (2 %) T1mic, 11 (4 %) T1a, 41 (15 %) T1b, 95 (35 %) T1c, and 115 (43 %) T2. Targeted therapy included combinations of trastuzumab, lapatinib, pertuzumab, and neratinib. NAC use increased from 53/219 (24.2 %) in the early group to 19/49 (38.8 %) in the recent group (p = 0.04). Forty-two percent (8/19) of patients in the recent group received neoadjuvant pertuzumab versus 0/53 in the early group (p < 0.0001). More clinically node-negative (cN0) patients received NAC in the recent (12/41, 29.3 %) versus early (20/167, 12.0 %) period (p = 0.01). For T1 tumors, the use of NAC more than doubled between the two time periods (5.6–17.2 %; p = 0.06), while NAC use increased from 48 to 70 % for T2 tumors (p = 0.08). The overall pCR rate after NAC was 48.6 % (35/72).
Conclusions
NAC for HER2-positive breast cancer patients is increasing. Most striking was a substantial increase in NAC for patients with T1 tumors and cN0 disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Historically, the use of neoadjuvant chemotherapy (NAC) for breast cancer patients was directed towards those with locally advanced disease. Its current role has expanded to the treatment of early breast cancer, and especially favorable responses are seen for certain subtypes, namely human epidermal growth factor receptor-2 (HER2)-positive and triple-negative tumors.
Trastuzumab is a humanized monoclonal antibody directed against the extracellular domain of HER2.1 Randomized phase III trials demonstrated that the combination of trastuzumab with standard chemotherapy resulted in an improvement in disease-free survival (DFS) and overall survival (OS) compared with standard chemotherapy alone in patients with metastatic breast cancer.2 Over the last decade, trastuzumab, with or without cytotoxic chemotherapy, has become standard therapy for patients with metastatic and non-metastatic HER2-positive breast cancer, specifically in patients with tumors >1 cm and who are found to have node-positive disease.3 Other agents that target HER2 have been developed since the introduction of trastuzumab, including lapatinib, pertuzumab, ado-trastuzumab emtansine (T-DM1), and neratinib, all of which have been investigated alone or in combination with trastuzumab.
Remarkable increases in pathological complete response (pCR) rates have recently been demonstrated by the addition of pertuzumab to trastuzumab and chemotherapy, leading to US FDA approval in September 2013 of pertuzumab in the neoadjuvant setting.4,5 In the NeoSphere trial, the pCR rate was 45.8 % in patients receiving pertuzumab plus trastuzumab and chemotherapy compared with a 29 % pCR rate in patients who received trastuzumab and chemotherapy.4 Similar results were demonstrated in the TRYPHAENA trial, where treatment with the dual HER2-targeting agents resulted in pCR rates of up to 52 %.5
Improvements in breast cancer survival over recent decades have been attributed to screening mammography and advances in systemic treatment.6 As a result of improved detection and awareness, diagnosis of early-stage breast cancer is increasing and many of these small tumors have an excellent prognosis; however, some small node-negative tumors have a biologically unfavorable subtype. The role of neoadjuvant and adjuvant systemic therapy for these patients is undefined. With a growing body of evidence showing the benefit of HER2-targeted treatment, along with FDA approval in September 2013 of pertuzumab in the neoadjuvant setting,7 it is likely that patients with early-stage HER2-positive breast cancer are increasingly offered NAC. The aim of this study was to evaluate recent trends in the use of NAC for early-stage HER2-positive tumors.
Methods
Patients
This study was approved by the Mayo Clinic Institutional Review Board. All women treated at the Mayo Clinic in Rochester for clinical T1 or T2 HER2-positive breast cancer between October 2008 and September 2014 were identified from our prospective breast surgery database. Clinical tumor stage was determined according to the American Joint Committee on Cancer (AJCC) 7th edition staging using the largest single dimension of the tumor on preoperative imaging and clinical assessment.8 HER2 expression was determined by immunohistochemistry (IHC), as assessed on the initial diagnostic core biopsy specimen, and was reported as 0, 1+, 2+ or 3+. Fluorescence in situ hybridization (FISH) was performed on all HER2 2+ cases, and a HER2/chromosome enumeration probe 17 (CEP17) signal ratio of 2.0 or higher was defined as positive. HER2 was reported as negative for IHC 0, 1+, and IHC 2+/FISH-negative cases, and positive for IHC 2+ FISH-positive and 3+ cases. pCR at surgery was defined as no evidence of invasive disease in the breast or axilla (ypT0 or ypTis, ypN0). Electronic medical records were used to review patient and tumor characteristics, neoadjuvant and adjuvant treatment details, surgical procedure, and final pathology.
Statistical Analysis
Two time periods were defined as early (October 2008–September 2013, prior to the approval of pertuzumab) and recent (October 2013–September 2014, subsequent to pertuzumab approval). Comparisons between the time periods (early vs. recent) were performed using Wilcoxon rank-sum tests for continuous variables, Chi square or Fisher’s exact tests for nominal variables, and the Cochran–Armitage trend test for ordinal variables. p values <0.05 were considered significant. Analysis was performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
A total of 268 cases were identified among 267 unique patients who were diagnosed with HER2-positive clinical T1 and T2 tumors. The mean patient age was 59 years (range 28–92 years). Clinical T-stage distribution was 6 (2 %) T1mic, 11 (4 %) T1a, 41 (15 %) T1b, 95 (35 %) T1c, and 115 (43 %) T2. Baseline patient and clinicopathologic characteristics between the early and recent time periods are compared in Table 1.
Treatment with NAC showed an increasing trend over time (p = 0.002), while a corresponding decreasing trend for the use of adjuvant therapy was noted (Fig. 1). The use of NAC significantly increased from 53 of 219 (24.2 %) in the early group to 19 of 49 (38.8 %) in the recent group (p = 0.04). Interestingly, however, the graph demonstrates that the use of NAC had increased markedly earlier than the most recent year and was actually slightly higher between October 2012 and September 2013 (47 %) versus October 2013–September 2014 (39 %); however, this difference was not significant (p = 0.44), and each of these time periods since October 2012 was significantly higher than the years prior (p < 0.01).
The agents used included standard chemotherapy regimens in addition to targeted HER2 therapy. In the neoadjuvant setting, all patients were treated with regimens that included chemotherapy and HER2-targeted therapies. In patients treated with adjuvant therapy, nine were treated with HER2-targeted therapy alone. HER2-targeted therapies used in patients treated with NAC included trastuzumab, lapatinib, neratinib, and pertuzumab. In the recent group, 42 % (8 of 19) of patients received neoadjuvant pertuzumab compared with none of 53 patients in the early group (p < 0.0001). In the early period, 51/53 (96.2 %) neoadjuvant patients received single therapy with trastuzumab only, while 2/53 (3.8 %) received dual therapy with trastuzumab and neratinib during this time. The use of dual therapy increased significantly (p < 0.0001) in the recent period to 9/19 (47.4 %) patients, with a combination of trastuzumab and pertuzumab in eight patients and trastuzumab with lapatinib in one patient; single therapy was used in 10/19 (52.6 %) patients from this time period, with trastuzumab only in nine patients and lapatinib in one patient. There was a small but not statistically significant (p = 0.56) difference, with 7/40 (17.5 %) clinically node-positive patients treated with dual therapy versus 4/32 (12.5 %) clinically node-negative patients in the neoadjuvant subset treated with dual therapy.
Mean age of patients treated with NAC did not differ for the early versus recent period (55 years; p = 0.94). Table 2 shows the percentage treated with NAC in the two time periods stratified by different clinical features. More clinically node-negative patients received NAC in the recent period (12/41, 29.3 %) versus the early period (20/167, 12 %) (p = 0.01). For T1 tumors, the use of NAC more than doubled between the two time periods, from 5.6 % (7/124) to 17.2 % (5/29) (p = 0.06). NAC use increased from 48.4 % (46/95) to 70 % (14/20) for T2 tumors (p = 0.08). Overall pCR rate was 48.6 % (35/72); a pCR rate of 49 % (30/61) for patients treated with single-agent HER2-targeted therapy, and 45 % (5/11) for patients treated with dual-agent HER2-targeted therapy (p = 0.82). pCR was strongly associated with estrogen receptor (ER)-negative tumors, for which 23/32 (71.9 %) had pCR compared with 12/40 (30 %) for ER-positive tumors (p = 0.0003).
Discussion
Our study demonstrates an increasing trend towards neoadjuvant treatment for early-stage HER2-positive breast cancer patients, particularly among those with smaller tumors and those who are clinically node-negative at diagnosis. Vast advances have been made in breast cancer systemic therapy over the last two decades. The role of drug development and approval has evolved over the years, from drug development and testing in the metastatic setting to a move to include the neoadjuvant setting, with the endpoint being disease response at surgery. The benefits of these systemic therapies have been demonstrated in large randomized clinical trials and meta-analyses, and have translated to improved patient survival, as evidenced by a reduction in breast cancer recurrence events and an increase in OS.9,10 Unfortunately, the challenge within the current economic climate lies with conducting costly, large randomized trials that require long-term follow-up. As such, neoadjuvant trials are ideal, providing an opportunity to evaluate the benefits of systemic treatments in a shorter time where response to treatment provides prognostic and predictive information and helps inform decisions about further adjuvant therapy. In addition, achievement of a pCR in the breast and lymph nodes provides valuable information as a pCR after NAC has been shown to correlate with improved prognosis.11,12 A longstanding argument in favor of NAC has been the potential to downstage breast tumors and make breast conservation feasible.11 Patients with HER2-positive tumors have been shown to demonstrate a remarkable response in terms of pCR rates after NAC.5,13–15 Our study demonstrates the changing trends in the treatment of T1 and T2 HER2-positive tumors over a 6-year period, with an overall uptake of treatment with targeted HER2 therapies, a move to treatment in the neoadjuvant setting, and the use of dual HER2-targeting agents with the goal of achieving a greater demonstrable response to therapy.
Studies to date have shown that the addition of trastuzumab to chemotherapy in patients with HER2-positive breast cancer results in an improved outcome. The NOAH trial was an early trial of neoadjuvant treatment with trastuzumab. Patients were randomized to receive neoadjuvant anthracycline and taxane-based chemotherapy with or without trastuzumab. The study reported an increase in pCR rates in the breast and axilla with the addition of trastuzumab to chemotherapy compared with no trastuzumab (38 and 19 %, respectively; p = 0.001). Subsequent trials have helped in setting a standard for timing and duration of treatment.16,17 Furthermore, the role of dual HER2-targeted therapy was addressed in the NeoALLTO trial, where the addition of the reversible tyrosine kinase inhibitor lapatinib to trastuzumab, and in combination with chemotherapy, resulted in a further increase in pCR rates compared with treatment with trastuzumab and chemotherapy alone. More recently, pertuzumab, a monoclonal antibody directed against HER2 dimerization, was investigated in the NeoSphere and TRYPHAENA trials in combination with trastuzumab with or without chemotherapy. A significant increase in the pCR rate to 45.8 and 52 %, respectively, was reported. The number of patients in HER2 studies with small tumors, specifically T1 tumors, is limited and as such it is difficult to extrapolate results from these trials. The NeoSphere and TRYPHAENA trials included patients with tumors of at least 2 cm. However, where investigated in earlier trials, a benefit from the addition of trastuzumab to standard chemotherapy was seen.18 The BCIRG-006 trial included patients with tumors <2 cm in size, and an analysis by tumor size was performed that showed significant benefits for patients with small tumors. Among patients with tumors measuring 1 cm or less, the estimated 5-year DFS rates were 86 % in the group receiving AC-T (doxorubicin, cyclophosphamide followed by docetaxel) plus trastuzumab, and 86 % in the group receiving TC (docetaxel,carboplatin) plus trastuzumab, compared with 72 % in the group receiving AC-T (p = 0.03).
The balance between treatment toxicity and oncologic benefit is an important consideration in recommending adjuvant treatment for breast cancer. Data on the benefit of treatment in patients with smaller tumors are more limited. A study from the MD Anderson Cancer Center reported on the risk of recurrence in women diagnosed with T1a/b, node-negative, HER2-positive breast cancer who were not treated with chemotherapy.19 The study showed that patients with HER2-positive breast cancer had worse recurrence-free survival (RFS) than patients with HER2-negative breast cancer (77.1 vs. 93.7 % at 5 years; p < 0.0001). There were no differences in RFS estimates in patients who had HER2-positive and hormone-receptor-negative tumors compared with patients who had HER2-positive and hormone-receptor-positive tumors. In addition, patients who had HER2-positive breast cancer had worse distant RFS than patients who had HER2-negative breast cancer (86.4 vs. 97.2 % at 5 years; p < 0.0001). The study concluded that patients with HER2-positive T1abN0M0 tumors have a significant risk of relapse, and recommended consideration for systemic, anti-HER2, adjuvant therapy. In contrast, two more recent studies addressed the outcomes of treatment in patients with small node-negative breast cancer, and reported a lower incidence of recurrence in patients with T1a tumors. Fehrenbacher et al. investigated the risk of invasive recurrence in 234 patients with HER2-positive T1aN0M0 or T1bN0M0 disease.20 Fifteen invasive recurrences were documented and the overall 5-year disease-free interval was 97 %. The number of patients with 1.0-cm tumors was larger than other groups and were therefore analyzed both as part of the T1b group and separately. The invasive recurrence-free interval for T1b tumors of 1.0 cm was found to be significantly lower than that for T1a tumors (84.5 vs. 97.4 %; p = 0.009). The study results should be interpreted with caution as they included patients treated and not treated with trastuzumab. Regardless, the reported rates of distant recurrence were low. A second study by Vaz-Luis et al. evaluated the outcomes of 4113 patients from the National Comprehensive Cancer Network Database with T1a and T1bN0,M0 breast cancers.21 This included patients with all subtypes. Survival outcomes were analyzed for patients treated and not treated with chemotherapy with or without trastuzumab. In the overall cohort, the 5-year DFS for treated patients with T1a tumors was 100 % for all subgroups, and ranged between 94 and 96 % for patients with T1b tumors, indicating that, overall, women with T1a and T1b tumors have an excellent prognosis even without chemotherapy. Specifically in the HER2-positive subgroup, the 5-year DFS for patients with T1bN0 tumors who did not receive chemotherapy or trastuzumab was 94 % for both hormone-receptor-positive and -negative HER2-positive patients. In those patients who received chemotherapy with or without trastuzumab, the 5-year DFS was 96 % in HER2-positive/hormone-receptor-positive tumors and 94 % in HER2-positive/hormone-receptor-negative tumors. Thus, in this cohort of patients the absolute benefit from chemotherapy with or without trastuzumab is small.
A strength of our study is that we report on a recent well-characterized patient group with robust review of tumor pathology. This study is limited by its retrospective nature and by the relatively small study cohort. Specifically, the number of patients in the T1 group may prohibit strong conclusions being reached. However, despite these limitations we found a trend for increased use of targeted therapies for patients with smaller T1 HER2-positive tumors over time.
Conclusions
Our study shows that patients with HER2-positive breast cancer are increasingly being treated with neoadjuvant therapy. Over a very short time period we noted a tripling of neoadjuvant therapy administration for patients with T1 tumors and a doubling for clinically node-negative patients, as well as a substantial increase for patients with T2 tumors. Further study is needed to evaluate the efficacy of this approach to the treatment of early HER2-positive breast cancers in terms of oncologic outcomes and toxicity.
References
Goldenberg MM. Trastuzumab, a recombinant DNA-derived humanized monoclonal antibody, a novel agent for the treatment of metastatic breast cancer. Clin Ther. 1999;21(2):309–18.
Slamon DJ, Leyland-Jones B, Shak S, Fuchs H, Paton V, Bajamonde A, et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med. 2001;344(11):783–92.
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology (NCCN Guidelines®): breast cancer. Fort Washington: National Comprehensive Cancer Network; 2015.
Gianni L, Pienkowski T, Im YH, Roman L, Tseng LM, Liu MC, et al. Efficacy and safety of neoadjuvant pertuzumab and trastuzumab in women with locally advanced, inflammatory, or early HER2-positive breast cancer (NeoSphere): a randomised multicentre, open-label, phase 2 trial. Lancet Oncol. 2012;13(1):25–32.
Schneeweiss A, Chia S, Hickish T, Harvey V, Eniu A, Hegg R, et al. Pertuzumab plus trastuzumab in combination with standard neoadjuvant anthracycline-containing and anthracycline-free chemotherapy regimens in patients with HER2-positive early breast cancer: a randomized phase II cardiac safety study (TRYPHAENA). Ann Oncol. 2013;24(9):2278–84.
Siegel RL, Miller KD, Jemal A. Cancer statistics 2015. CA Cancer J Clin. 2015;65(1):5–29.
US FDA. FDA approves Perjeta for neoadjuvant breast cancer treatment. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm370393.htm. Accessed 10 Apr 2015.
American Joint Committee on Cancer (2010) Breast cancer staging. Cancer staging manual 7. American Joint Committee on Cancer, New York.
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2012;365(9472):1687–717.
McGale P, Taylor C, Correa C, Cutter D, Duane F, Ewertz M, et al. Effect of radiotherapy after mastectomy and axillary surgery on 10-year recurrence and 20-year breast cancer mortality: meta-analysis of individual patient data for 8135 women in 22 randomised trials. Lancet. 2014;383(9935):2127–35.
Fisher B, Brown A, Mamounas E, Wieand S, Robidoux A, Margolese RG, et al. Effect of preoperative chemotherapy on local-regional disease in women with operable breast cancer: findings from national surgical adjuvant breast and bowel project B-18. J Clin Oncol. 1997;15(7):2483–93.
Bear HD, Anderson S, Smith RE, Geyer CE, Mamounas EP, Fisher B, et al. Sequential preoperative or postoperative docetaxel added to preoperative doxorubicin plus cyclophosphamide for operable breast cancer: national surgical adjuvant breast and bowel project protocol B-27. J Clin Oncol. 2006;24(13):2019–27.
Baselga J, Bradbury I, Eidtmann H, Di Cosimo S, De Azambuja E, Aura C, et al. Lapatinib with trastuzumab for HER2-positive early breast cancer (NeoALTTO): a randomised, open-label, multicentre, phase 3 trial. Lancet. 2012;379(9816):633–40.
Von Minckwitz G, Untch M, Blohmer JU, Costa SD, Eidtmann H, Fasching PA, et al. Definition and impact of pathologic complete response on prognosis after neoadjuvant chemotherapy in various intrinsic breast cancer subtypes. J Clin Oncol. 2012;30(15):1796–804.
Untch M, Loibl S, Bischoff J, Eidtmann H, Kaufmann M, Blohmer JU, et al. Lapatinib versus trastuzumab in combination with neoadjuvant anthracycline-taxane-based chemotherapy (GeparQuinto, GBG 44): a randomised phase 3 trial. Lancet Oncol. 2012;13(2):135–44.
Perez EA, Romond EH, Suman VJ, Jeong JH, Davidson NE, Geyer CE, et al. Four-year follow-up of trastuzumab plus adjuvant chemotherapy for operable human epidermal growth factor receptor 2-positive breast cancer: joint analysis of data from NCCTG N9831 and NSABP B-31. J Clin Oncol. 2011;29(25):3366–73.
Goldhirsch A, Gelber RD, Piccart-Gebhart MJ, De Azambuja E, Procter M, Suter TM, et al. 2 years versus 1 year of adjuvant trastuzumab for HER2-positive breast cancer (HERA): an open-label, randomised controlled trial. Lancet. 2013;382(9897):1021–8.
Slamon D, Eiermann W, Robert N, Pienkowski T, Martin M, Press M, et al. Adjuvant trastuzumab in HER2-positive breast cancer. N Engl J Med. 2011;365(14):1273–83.
Gonzalez-Angulo AM, Litton JK, Broglio KR, Meric-Bernstam F, Rakkhit R, Cardoso F, et al. High risk of recurrence for patients with breast cancer who have human epidermal growth factor receptor 2-positive, node-negative tumors 1 cm or smaller. J Clin Oncol. 2009;27(34):5700–6.
Fehrenbacher L, Capra A, Quesenberry Jr C, Fulton R, Shiraz P, Habel L. Distant invasive breast cancer recurrence risk in human epidermal growth factor receptor 2-positive T1a and T1b node-negative localized breast cancer diagnosed from 2000 to 2006: a cohort from an integrated health care delivery system. J Clin Oncol. 2014;32(20):2151–8.
Vaz-Luis I, Ottesen RA, Hughes ME, Mamet R, Burstein HJ, Edge SB, et al. Outcomes by tumor subtype and treatment pattern in women with small, node-negative breast cancer: a multi-institutional study. J Clin Oncol. 2014;32(20):2142–50.
Disclosure
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Al-Hilli, Z., Boughey, J.C., Hoskin, T.L. et al. Increasing Use of Neoadjuvant Treatment for T1 and T2 HER2-Positive Tumors. Ann Surg Oncol 22, 3369–3375 (2015). https://doi.org/10.1245/s10434-015-4718-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-4718-6