Abstract
This study aimed to enhance the dissolution of simvastatin (SMV) through its formulation in liquisolid tablets (LSTs) to improve its bioavailability and hypolipidemic activity after oral administration. SMV-LSTs were optimized using Box-Behnken design to maximize the rate and extent of SMV dissolution. The optimized SMV-LST was evaluated for pharmacokinetic parameters and potential hypolipidemic activity on induced hyperlipidemic rats. The dissolution parameters revealed a shortening of mean dissolution time from 10.99 to 6.82 min, increasing of dissolution rate during the first 10 min from 1253.15 to 1667.31 μg/min, and enhancing of dissolution efficiency after 60 min from 71.92 to 86.93% for SMV-LSTs versus the commercial SMV tablets. The obtained data reflected an improvement in the relative bioavailability of SMV with 148.232% which was confirmed by the significant reduction of the levels of circulating total cholesterol, triglycerides that reached the normal level after 12 h. In particular, the optimized SMV-LSTs reduced serum low-density lipoproteins (LDL) by 44.6% which was significantly different from the commercial SMV tablets. In contrast, the level of serum high-density lipoprotein (HDL) was significantly augmented after 4 h in rats treated with the optimized SMV-LSTs by 47.6%. Finally, the optimized SMV-LSTs showed a significant lower atherosclerotic index value which could maximize its potential in decreasing the risk of coronary disease and atherosclerosis. Overall enhancement in pharmacokinetics and pharmacodynamics in comparison with the commercial tablets confers the potential of the liquisolid approach as a promising alternative for improved oral bioavailability, hypolipidemic, and cardioprotective effects of SMV.

Graphical abstract
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
INTRODUCTION
A great number of the newly developed active pharmaceutical ingredients (APIs), whatever their origin (natural, synthetic, or semi-synthetic), are hydrophobic. Accordingly, these APIs are of limited solubility and dissolution rate [1,2,3]. Many formulation strategies have been reported to enhance the solubility and dissolution rate of poorly water-soluble APIs such as solid dispersion, inclusion complexation, nanosuspension formation, micronization, self-nanoemulsions, polymeric, and lipid-based nanoparticles [4,5,6,7,8,9,10,11,12].
SMV faced limited bioavailability (5%) after oral administration due to its poor aqueous solubility (≈ 0.03 g/L), slow dissolution rate, and extensive hepatic metabolism [13, 14]. Consequently, it is necessary to propose effective strategies to improve the solubility of SMV that could enhance the drug bioavailability and hypolipidemic effect. From these strategies, development of self-microemulsifying delivery system [15], self-nanoemulsifying granules [16], transdermal delivery system [17,18,19], nanostructured lipid carrier [13], nanosuspension [20], spherical mesocellular foam [21], encapsulation in polymeric micelles of HPMC [22], and complexation with hydroxypropyl b-cyclodextrin [23] have been reported.
Most of these approaches require sophisticated preparation methods and/or advanced equipment and so high production costs. Recently, the liquisolid technique has been introduced to improve the dissolution and to overcome drawbacks of the aforementioned approaches [24, 25]. In this method, liquid drug(s), solution, or suspension of water-insoluble APIs are converted into non-adherent, free-flowing, and easy compressible dry powder mixtures by mixing with proper excipients (carriers and coating materials). The obtained dry powder mixtures are finally formulated into fast release solid dosage form [26, 27]. Drugs formulated into the liquisolid system are present in a complete or partial molecular dispersion state that improves the dissolution rate by enhancing their aqueous solubility, improving the wetting properties, or increasing the surface area accessible for dissolution medium [28,29,30,31,32]. Liquisolid technique reveals several benefits such as simple processing, low production costs in comparison with the soft gelatin capsules, and superior release of its drug content. The key advantage is the greater bioavailability of the liquid drug produced by its loading on silica which maximizes the surface area available for absorption. Enhancement in the drug bioavailability is expected to have a direct effect on reducing the drug dose and side effect. Other advantages of the liquisolid technique include decreasing the influence of pH variation on drug dissolution profile [33], enhancing drug photostability [34], and recently this technique has been examined in drug release enhancement or modification [35,36,37,38,39].
SMV like other statin drugs exerts its hypolipidemic effect by inhibiting the enzyme 3-hydroxy-3-methyl-glutaryl-coenzyme A reductase (HMG-CoA) leading to decrease the synthesis of cholesterol and increase the removal of LDL circulating in the body [40, 41]. It has been reported that the cardioprotective property of SMV may not only achieved by inhibition of HMG CoA activity thereby reducing endogenous cholesterol biosynthesis but may also include induction of lecithin:cholesterol acyltransferase (LCAT) activity that promote the esterification of free cholesterol.
SMV possesses high permeability through biological body membranes, but due to its very low aqueous solubility, its absorption after oral administration is restricted by its low dissolution rate. Therefore, the use of the liquisolid technique was chosen to improve the dissolution behavior of SMV and consequently enhancing its oral bioavailability, hypolipidemic, and cardioprotective effects.
MATERIALS AND METHODS
Materials
Simvastatin (SMV) was kindly donated by the Saudi Arabian Japanese Pharmaceutical Company (Jeddah, Saudi Arabia). Propylene glycol (PG) was obtained from Fluka (Steinheim, Germany). Span 80, Tween 20, Tween 60, Tween 80, and triacetin were procured from Sigma-Aldrich (St. Louis, MO, USA). Glycerin was purchased from Crescent Diagnostics (Jeddah, Saudi Arabia). Methanol and polyethylene glycol (PEG) 400 were supplied from BDH laboratory reagents (Poole, England). PEG 200 was obtained from Merck-Schuchardt (Hohenbrunn, Germany). Polyvinylpyrrolidone/vinyl acetate copolymer (PVP/VA 50/50 w/w) 73 and 64 all PVP/VAs were gifted from Shanghai Yuking Water Soluble Material Tech. Co. Ltd. (Shanghai, China). Talc powder was purchased from Whittaker Clark & Daniels (South Plainfield, NJ, USA). Microcrystalline cellulose (Avicel PH 101) was procured from Fluka (Hach Lange, Ireland). Polyvinylpyrrolidone, average M.W. 8.000, K16-18 was obtained from Acros Organics (Fair Lawn, NJ, USA). Croscarmellose sodium (Ac-Di-Sol) was purchased from FMC BioPolymer (Philadelphia, PA, USA). Acetonitrile HPLC grade was procured from Merck Inc., (Darmstadt, Germany). Phosphoric acid was procured from Riedel-de Haën AG (Seelze, Germany).
Solubility Studies
SMV solubility was determined in glycerin, PG, PEG 200, PEG 400, Span 80, Tween 20, Tween 60, Tween 80, PVP/VA 73, PVP/VA 64, triacetin, and distilled water as previously published [29, 42]. Briefly, SMV was mixed with a known volume of the studied solvents in 10-ml vials to prepare a saturated system of the drug. The mixture was kept shaken in a water bath (GFL type 1083, Germany) for 48 h at room temperature. The prepared mixtures were centrifuged at 15,000 rpm for 30 min (Sigma type 3 k30, Germany), filtered (0.2 μm, Millipore), and finally analyzed for SMV concentration spectrophotometrically at 239 nm (UV-Vis spectrophotometer, Jenway 67 series).
Design and Formulation of SMV-Liquisolid Tablets Using Box-Behnken Design
Response surface methodology was employed to evaluate the effect of three independent variables namely, liquid load factor (X1), the excipient ratio (X2), and the Ac-Di-Sol concentration (X3) in three levels on the dissolution behavior of SMV-liquisolid tablets (LSTs). The liquid load factor was ranged from 0.25 to 0.35, the excipient ratio was 5–15, and the Ac-Di-Sol concentration was ranged from 4 to 6%. The low and high levels of these variables have been selected based on the results of the preliminary study of the holding capacity of excipients and the flow and compressibility behaviors of the liquisolid powder blends. These constraints ensure the potential of the formulations to be free-flowing and compressed into tablets with acceptable quality attributes. Statgraphics Centurion 18 software, Statgraphics Technologies, Inc. (Virginia, USA), was used to assess the effect of the independent variables on the dissolution rate at the first 10 min (Y1), and the dissolution efficiency percent after 60 min (Y2). The composition of the optimized LSTs, with improved dissolution pattern, was obtained utilizing numerical optimization and desirability approach.
Pre-compression Evaluation of the Liquisolid Powder Blends
Evaluation of Powder Flow Properties and Compressibility
Flow properties of the powder blends were evaluated by the angle of repose method according to the USP29-NF24 (General Chapters: <1174> Powder flow) [43]. This was carried out by allowing the powder to drop from a funnel on a table surface to form a pile, then the height of the powder cone was measured and finally the tan of the angle of repose was measured from Eq. 1.
Compressibility properties of the powder blends were evaluated according to the USP29-NF24 (General Chapters: <1174> Powder flow) [43]. A specific volume of the sample was gently transferred into a graduated cylinder and accurately weighed. Then, the sample was mechanically tapped several times until no further volume changes occur. The bulk and tapped volumes were determined. All measurements were done in triplicate. The bulk (BD) and tapped densities (TD) (g/mL) were calculated. The compressibility index (CI) was estimated from Eq. 2.
Compression and Evaluation of SMV-Liquisolid Tablets
Fifteen batches of SMV-LST formulations (LS-1 to LS-15) were prepared as per suggested by Box-Behnken design (BBD). SMV was dissolved in the selected non-volatile solvent and triturated well with Avicel PH-101 and fumed silica. All ingredients were de-lumped individually through no. 40 mesh sieve and mixed with other excipients such as binder and disintegrant for 15 min. The glidant and lubricant were also de-lumped through the 40-mesh sieve, then added to the powder blend and mixed for 3 min. The powder blends were compressed at 10-kN compression force with a single punch tablet press (Erweka, GmbH, Heusenstamm, Germany) equipped with 9-mm flat face round punches. The tablet weight of the prepared tablets was approximately 300 mg containing 20 mg of SMV. The tablet dimensions were measured for 10 tablets using a digital micrometer (Mitutoyo, Japan). The prepared tablets were tested for the average weight using a Mettler Toledo balance (Mettler Toledo, Switzerland). Hardness was determined using hardness tester (Erweka TBH200, Germany). Tablet friability was estimated using a PharmaTest PTF10ER Friabilator (Hainburg, Germany), and the disintegration time was determined using a PharmaTest PTZ3 disintegration test apparatus (Hainburg, Germany). Finally, the SMV content of the prepared batches was determined using the high-performance liquid chromatography (HPLC) instrument (Agilent Technologies, Palo Alto, CA). All the methods used during the quality control testing complied with the USP Pharmacopeia [44].
In Vitro Dissolution Studies
The USP apparatus II (paddle type) was used to study the in vitro dissolution of SMV from the prepared LST formulations. A dissolution medium of 900 ml of distilled water containing 0.5% sodium dodecyl sulfate to maintain sink condition as previously reported [45, 46] at 37 ± 0.5°C was used at a rotation of 75 rpm. Samples of 5 ml were withdrawn at predetermined time intervals of 5, 10, 15, 30, 45, and 60 min and filtered through 0.45-μm Millipore filter (Millipore Corp., Bedford, MA, USA). Samples removed were replenished immediately with the same volume of fresh media. The concentration of SMV was determined using the previously reported and validated analytical chromatographic method using the HPLC instrument (Agilent Technologies, Palo Alto, CA) equipped with HP 1200 UV detector (Hewlett-Packard, USA) that was set at 238 nm. An HP 1200 autosampler and a quaternary HP 1200 pump were used. Acetonitrile–phosphate buffer (pH 6.8; 0.01 M) (40:60, v/v) was used as a mobile phase that was pumped at a flow rate of 1.2 mL/min under an isocratic condition [47]. The cumulative percentage of dissolved SMV released was calculated regarding determined content and plotted versus time. Dissolution studies were performed in triplicate.
To investigate the significance of variation among the dissolution profiles of SMV from the prepared LSTs, the dissolution rate during the first 10 min (DR10) was calculated using Eq. 3.
where M is the total quantity of SMV in each tablet (20,000 μg) and D designates the percentage of drug dissolved during the first 10 min.
Also, other non-model parameters such as the mean dissolution time (MDT) and the dissolution efficiency at 60 min (DE60) were calculated from the in vitro release data using DDSolver (An Add-In Program for Modeling and Comparison of Drug Dissolution Profiles) [48]. These parameters were computed according to Eqs. 4 and 5 to compare the different dissolution profiles of the LS formulations.
where (j) is the sample number, n is the number of dissolution sample times, (\( {t}_j^{\mathrm{AV}} \)) is the time at the midpoint between t and t − 1 (calculated with (t + t − 1)/2), and (∆Qj) is the additional amount of drug dissolved between t and t − 1.
The dissolution efficiency was computed as the percent ratio of area under the dissolution curve up to the time, t, to that of the corresponding area of the rectangle described by 100% dissolution at the same time [49,50,51,52].
where (Q) is the percent of drug released at each time interval, (t) is the total duration of drug release, and (Q100) is the 100% drug release.
Data Analysis and Prediction of the Optimized SMV-LS Formulation
Analysis of variance and multiple response optimization, using Statgraphics software, was performed to investigate the effect of each input variable and its interaction with other variables to predict the optimized SMV-liquisolid tablets. The proposed optimized SMV-LST formulation was prepared, fully characterized, and compared to the commercial SMV tablets (Simva 20 mg, Jamjoom Pharmaceuticals Co., Jeddah, SA) using a model-independent method by calculation of MDT, DR10, and DE60 parameters as well as by the use of fit factors like the difference factor (f1) (Eq. 6), and the similarity factor (f2) (Eq. 7) [53,54,55,56]. Analysis of the dissolution data and calculation of all the studied parameters were performed using the DDSolver (An Add-In Program for Modeling and Comparison of Drug Dissolution Profiles) [48].
where n is the number of dissolution sampling times, and Rt and Tt represent the individual or mean percent dissolved at each time point, t, for the reference and test dissolution profiles, respectively. Finally, the optimized formulation was scaled up to be evaluated in vivo for its pharmacokinetic parameters and pharmacodynamic effect in induced hyperlipidemic rats.
In Vivo Studies on the Poloxamer-Induced Hyperlipidemic Rats
Experimental Design
In this study, a single-dose one-period parallel design was used. The study was performed following the European Medicines Agency (EMA), International Conference on Harmonization (ICH), Good Clinical Practice (GCP), and Food and Drug Administration (FDA) guidelines. The animal experimental protocol was revised and approved by the Research Ethics Committee, Faculty of Pharmacy, King Abdulaziz University (Approval No. PH-111-41). The study was achieved according to the Declaration of Helsinki, the Guiding Principle in Care and Use of Animals (DHEW production NIH 80±23), and the “Standards of Laboratory Animal Care” (NIH distribution #85±23, reconsidered in 1985).
Animal Handling
Twenty-four male Wistar rats, weighing 200–250 g, were used in this study. Twelve rats were used for the pharmacokinetic (PK) and twelve were used for pharmacodynamic (PD) evaluation. This number of rats was considered enough for blood sampling by an alternative method. The rats were housed in cages and kept on a 12-h light/dark at room temperature (25°C) and relative humidity of 55 ± 10%. Rats were maintained with free access to water and ad libitum. General and environmental conditions were strictly monitored. The animals were divided into two groups of six animals. The two groups were nominated as a test group that received an oral SMV-LSTs while the reference group administered the commercial SMV tablet (Simva 20 mg, Jamjoom Pharmaceuticals Co., Jeddah, SA). Hyperlipidemia was induced in the studied animals by intraperitoneal injection of 0.25 g/kg poloxamer 407 that was dissolved in 0.9% saline [57, 58]. After 24 h, the reference and test groups were orally administered 1 ml of 0.5% carboxymethyl cellulose aqueous suspensions containing the pulverized SMV tablet (equivalent to 10 mg/kg body weight) through esophageal intubation.
Blood Sampling
Blood samples (250 μL) were collected in heparinized tubes under light ether anesthesia by a retro-orbital puncture at 0.5, 1, 1.5, 2, 3, 4, 6, 8, 12, and 24 h. The collected blood samples were centrifuged at 3000 rpm for 5 min to separate the plasma that was collected and stored at − 20°C until performing the analysis.
Evaluation of Pharmacokinetic Parameters
The pharmacokinetic parameters of the optimized SMV-LSTs were evaluated and compared to that of the commercial drug tablets. After the oral administration of the optimized SMV-LSTs and the commercial tablets as described above, the following pharmacokinetic parameters were determined by the non-compartmental extravascular pharmacokinetic model using PKsolver (an add-in program for pharmacokinetic data). Maximum (peak) plasma concentration over the time specified (Cmax) and time point to reach the maximum plasma concentration (Tmax) were specified. The area under the plasma concentration-time curve from zero time to the last measurable concentration (AUC0–t) was estimated by the linear trapezoidal method, and the area under the plasma concentration-time curve from time zero to infinity (AUC0–inf) was calculated as the sum of the AUC0–t plus the ratio of the last measurable plasma concentration to the elimination rate constant. The area under the first moment of the plasma concentration-time curve was from time zero to infinity (AUMC0–inf), also, the individual estimate of the terminal elimination rate constant (Lambda_z). The mean residence time (MRT0–inf) is calculated by the ratio of AUMC to AUC. The elimination half-life (t1/2) was calculated as 0.693/Lambda_z. Moreover, the apparent total body clearance of the drug from plasma after oral administration (Cl/F) was calculated by dividing the dose by AUC. The apparent volume of distribution during the terminal phase after non-intravenous administration (Vz/F) was calculated by multiplying the total body clearance by MRT. Finally, the relative bioavailability of optimized liquisolid tablets (AUC test/AUC reference × 100) was determined.
Chromatographic Conditions
The plasma SMV concentration was determined using an isocratic HPLC chromatographic condition. The HPLC instrument was equipped with a variable wavelength ultraviolet spectroscopic detector adjusted at 236 nm along with a quaternary pump, autosampler, vacuum degasser, and Winchrom software was used. The chromatographic separation was performed on a Phenomenex, RP Hi-Q-Sil C18 column (Phenomenex, Torrance, CA) at room temperature. Acetonitrile-0.1% phosphoric acid at 70:30 v/v was used as a mobile phase that was pumped at a flow rate of 1 ml/min. For SMV extraction from the plasma samples, 1 ml of an acetonitrile-methanol (1:1) mixture was added, vortexed for 1 min, and centrifuged for 10 min at 5000 rpm. The organic phase was taken and evaporated to dryness under a stream of nitrogen at 50°C. The residue was reconstituted in 80 μl of the mobile phase and a volume of 20 μl was injected. An internal standard (IS) solution was prepared by dissolving a specified amount of atorvastatin in a known volume of the mobile phase to prepare a 100 μg/ml solution. Two milliliters of the IS was added to 500 ml of the supernatant followed by extraction with diethyl ether and potassium hydroxide solution. The supernatant was evaporated under nitrogen and the residue was constituted with 200 ml of the mobile phase. The chromatographic condition utilized in this method was in-house validated and considered accurate, precise, sensitive, selective, and robust. The limits of SMV quantitation and detections were 2 and 0.5 ng/ml, respectively.
Measurement of SMV Hypolipidemic Activity
The hypolipidemic activity of SMV-LSTs was determined in comparison with SMV commercial tablet over a 24 h after an oral administration of a single-dose of SMV (10 mg/kg body weight). Blood samples were collected and the serum was separated by centrifugation at 10,000 rpm for 5 min. The collected serum samples were analyzed for total cholesterol, total triglycerides, LDL, and HDL by the enzymatic colorimetric method using in vitro diagnostic kits (Egy Chemical for Lab Tech & BioMed Diagnostics, Egypt) [59]. Before blood sampling, the studied animals have fasted overnight, and blood samples were collected through retro-orbital puncturing at zero time to determine the baseline levels of TC, TG, HDL, and LDL. These biochemical parameters have been re-determined after administering SMV to the studied groups and comparing results with the corresponding baseline values assuming that each animal served as its own control.
Statistical Analysis
All statistical analyses were performed using GraphPad Prism, version 8.4.2 Software (San Diego, CA, USA). Regarding the plasma concentration-time curve, two-way ANOVA followed by Sidak’s multiple comparisons test was done to compare each means with the other at all time points to assess the significance between groups. The biochemical parameters were assessed for their statistical difference using the (multiple t tests) Holm-Sidak method with alpha = 0.05 to analyze each time point individually. Finally, a two-tailed unpaired t test was used to assess the pharmacokinetic parameters of the formulations. Results with P < 0.05 were considered significant.
RESULTS AND DISCUSSION
In this study, LST formulations of SMV were prepared as suggested by BBD (Table I). To develop LSTs characterized by higher SMV release rate, the drug solubility in the commonly used non-volatile water-miscible solvents, some nonionic surfactants like Spans, Tweens, and PVP/VA copolymers were investigated. It has been previously reported that the drug release from the liquisolid formulation is mainly dependent on the drug solubility in the studied liquid vehicle [60]. Tween 80 was selected as a non-volatile solvent as it demonstrates the highest solubilization capacity of SMV (98.34 mg/ml) while its solubility in water was 0.22 mg/ml (Fig. 1). This finding confirms that SMV is very slightly soluble in water as described by the USP since it needs from 1000 to 10,000 ml to dissolve 1 g. The proposed fifteen formulations were prepared by direct compression technique using Avicel PH-101 and fumed silica as carrier and coating materials, respectively. Ac-Di-Sol (Croscarmellose sodium) was used as superdisintegrant and polyvinylpyrrolidone (PVP K16-18) was added to maintain the aqueous supersaturation of SMV via its adsorption on the surface and inhibition of the crystal growth at a high degree of supersaturation [61]. The data obtained from pre-compression parameters such as the angle of repose and Carr’s index were found to be within acceptable pharmacopeia range (Table II). Though some formulations have shown good flow properties, incorporation of the glidant was essential to improve the flow properties of all formulations. The flow properties of the LS powder blends expressed in the form of the angle of repose were varied from 42.3° to 25.1° indicating a passable to excellent flow characteristics. It was obvious from the data presented in Table II that the formulations (LS-11 and LS-5) had passable flow property because they have the highest values of liquid load factor and the excipient ratio, and the formulations LS-4, LS-9, and LS-12 had fair flow. On the other hand, the rest of the remaining formulations exhibited good to excellent flow behavior and can be compressed without aid. Also, the compression properties of the formulations represented by Carr’s index showed good compressibility as most of the formulations have Carr’s index values less than 21% [62].
After successful compression of the LS formulations, the compressed tablets were evaluated for their quality attributes like weight uniformity, content uniformity, hardness, friability, and in vitro disintegration. The post-compression properties of the prepared LSTs presented in Table II revealed their uniformity regarding the weight of tablets and SMV content of all formulations. SMV content was found to be in the range of 96.99 to 99.98% for LS-12 and LS-3, respectively. These results comply with the official specifications of the USP and reflect the uniformity of weight in all the studied formulations [63]. Also, the observed ranges for the friability and the hardness were 0.13–0.57%, and 42.6–70.2 N, respectively. These results met the compendial limits of friability (< 1%) and reflect the acceptable mechanical properties of the prepared LSTs and the good compressibility of the powder blends. Finally, the disintegration time of the prepared tablets was ranged from 58 to 302 s for LS-4 and LS-10, respectively, which denotes that the disintegration time of all the studied formulations met the pharmacopoeial requirements.
In Vitro Dissolution Studies
The dissolution studies of the liquisolid tablets were performed in distilled water containing 0.5% sodium dodecyl sulfate dissolution medium to maintain the sink condition of SMV during the study. In vitro dissolution profiles of the fifteen LS formulations are presented in Fig. 2. In a good agreement with the monographs in the pharmacopeia specification USP 34, all formulations released more than 75% of their SMV content in 30 min except LS-6 which released only 66.94% in this period. Moreover, drug release from LS-5 was very fast (82.73% in 10 min) while LS-6 observed very slow SMV release (53.59% in 10 min). Similar to our previous observation, the drug release rate was impacted by the hardness of the tablets [64]. The rate of disintegration is influenced by the rate of influx of the dissolution medium into the tablets. Also, the Ac-Di-sol percentage in the formulation has an impact on the dissolution rate regardless of the other solid components in the formulation. Formulations with a high percentage of Ac-Di-Sol would most likely decrease the disintegration time and consequently enhances the dissolution rate and efficiency of SMV as noticeably observed in formulations LS-3, LS-4, LS-5, and LS-7. In contrast, formulations containing a low percentage of Ac-Di-Sol (LS-6, LS-9, LS-10, and LS-12) showed the lowest cumulative amount of SMV released. This result might be attributed to the long disintegration time of LSTs that led to a decrease in the surface area exposed to the medium and so to a decrease in the dissolution and bioavailability of the drug and vice versa [65].
The dissolution rate during the first 10 min (DR10) was taken as a measure for the extent and rate of drug dissolved from the prepared formulations. It was observed that the DR10 was increased upon increasing the solubility of the drug in the non-volatile solvent that was used in the preparation of the LS formulations. The obtained result was also supported by further analysis of the dissolution data using the mean dissolution time (MDT) and dissolution efficiency after 60 min (DE60). All formulations revealed low values of MDT that ranged from 7.65 min to 13.54 min (Table II) that was reflected in the high values of DR10, ranged from 1071.97 to 1654.55 μg/min, and high values of DE60 that ranged from 64.17 to 86.33% (Table III). These findings indicate the enhancement of the rate and extent of SMV dissolution.
Quantitative Estimation and Mathematical Modeling of the Dissolution Data
Table IV illustrates the estimated effect of factors, F-ratio, and P values for Y1 and Y2 obtained from the two-way analysis of variance (ANOVA). It was obvious that the liquid load factor (X1), excipient ratio (X2), and Ac-Di-Sol percent (X3) had significant positive effects on the dissolution rate during the first 10 min (Y1) with P values of 0.0160, 0.0030, and 0.0001, respectively. The quadratic term of X3 had a significant negative effect on Y1 with a P value of 0.0270. Also, it was found that X2 and X3 had significant positive effects on the dissolution efficiency (Y2) with P values of 0.0164 and 0.0003, respectively, while X1 had no significant effect on Y2. The R-squared statistic specifies that the model as fitted explains 97.9135% and 95.4209% of the variability in DR10 and DE60, respectively. Upon analysis of the data, a mathematical model for each variable was produced. These models are represented in Eqs. 7 and 8 that illustrate the quantitative effects of the studied variables on the dependent responses (Y1–Y2).
It is clear from the regression Eq. 7, the statistical analysis (Table IV), and the Pareto chart (Fig. 3a) as well as the 3D response surface plots (Fig. 3b–d) that Y1 is significantly influenced by X1, X2, and X3. An increase in the liquid load factor (X1) from 0.25 to 0.35, at the same level of X2 and X3, led to an increase in Y1 from 1459.56 to 1591.33 μg/min for LS-2 and LS-14, respectively. A similar observation was noticed for LS-7 and LS-5 where Y1 increased from 1505.27 to 1654.55 μg/min, and from 1158.04 to 1207.89 μg/min for LS-10 and LS-9, respectively. Also, the same finding was confirmed for LS-11 and LS-13 that illustrated an increase in the Y1 value from 1264.88 to 1362.22 μg/min, respectively. A similar trend was observed with a direct relationship between DR10 (Y1) and the excipient ratio (X2) and Ac-Di-Sol percent (X3).
Also, it is obvious from the regression Eq. 8, the statistical analysis (Table IV), and the Pareto chart (Fig. 4a) as well as the 3D response surface plots (Fig. 4b–d) that Y2 is significantly influenced by X2 and X3 while X1 had no significant effect on DE60. An increase in the Ac-Di-Sol percent (X3) from 4 to 6%, at the same level of X1 and X2, led to an increase in Y2 from 64.17 to 82.72% for LS-6 and LS-3, respectively. A similar observation was found in LS-12 and LS-4 where Y2 increased from 72.21 to 85.33%, and from 1158.04 to 1207.89 μg/min for LS-10 and LS-9, respectively. Also, the same finding was confirmed for LS-10 and LS-7 that illustrated an increase in Y2 from 69.95 to 82.54%, respectively. A similar trend was observed with a direct relationship between DE60 (Y2) and the excipient ratio (X2). The enhancement in drug release could be attributed to the expected increase in the drug solubility in the liquid vehicle of the liquisolid system. Also, the liquid vehicle may act as a co-solvent in the release microenvironment at the solid-liquid interface between the individual liquisolid primary particle and the release medium which permit easy diffusion of a single liquisolid particle together with the drug molecules and increase the solubility of the drug [66]. The overall increase in the solubility of the many drugs after the development of liquisolid systems was confirmed in several works [67, 68]. Moreover, the use of Tween 80 as a non-volatile solvent in the formulations, being a surface-active agent, could improve the wetting of the liquisolid particles as previously reported [42, 69].
It is well known that the tablet disintegration has a great impact on the drug dissolution from the studied tablets. From the above finding, it is clear that the presence of Ac-Di-Sol in the formulation in a high percent mainly affects the disintegration and hence the dissolution rate and dissolution efficiency (Y1 and Y2) as previously reported [66]. Also, the excipient ratio (X2) plays an important role in the enhancement of drug dissolution especially if Avicel and silica are used as a carrier and a coating material, respectively. Liquisolid formulations with high values of X2, high amounts of Avicel, and low amounts of silica are associated with enhanced wicking, disintegration, and thus enhanced drug release. Moreover, a high amount of silica, being hydrophobic, could retard the drug release [70].
Prediction and Validation of the Optimized SMV-LSTs
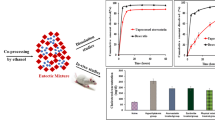
To verify the practicality of the BBD results, a new formulation was prepared and evaluated for the responses (Y1 and Y2). The independent variable levels, which maximize the desirability function, were 0.34, 11.59, and 5.95% for X1, X2, and X3, respectively. The observed values of the studied responses were compared with the predicted values and the obtained results revealed no substantial residuals, signifying that the BBD was quite valuable for maximizing the release parameters. The MDT was noticeably shortened from 10.99 min for the commercial tablets to 6.82 min for SMV-LSTs. Also, DR10 and DE60 of the SMV-LSTs were 1667.31 μg/min and 86.93% versus 1253.15 μg/min and 71.92% for the commercial tablets. The comparison between the dissolution profiles of both formulations revealed values of 23.52 and 39.47 for (f1) and (f2) parameters, respectively. According to the FDA, f1 values greater than 15 and f2 values less than 50 should ensure the difference between the dissolution curves, which indicate an average difference greater than 10% at the sample time points. Accordingly, the dissolution curves corresponding to the optimized SMV-LSTs would be different from those obtained with the commercial tablets [71]. All these observations reflect the enhanced release behavior of SMV from the liquisolid formulation as depicted in Fig. 5 a.
Pharmacokinetic Parameters Evaluation
The plasma concentration-time profiles for the optimized SMV-LST formulation and the commercial drug tablet are signified in Fig. 5 b. The values of the pharmacokinetic parameters for SMV from both formulations are summarized in Table V. This data indicated that LSTs improved the relative bioavailability of SMV over the commercial tablets by 148.232%. The value of Cmax of the optimized SMV-LSTs was 62.00 ng/ml versus 46.333 ng/ml for the commercial tablets, and the tmax of optimized SMV-LSTs shortened to 90 min instead of 120 min for the commercial tablets. This finding indicates an enhancement in the absorption of SMV from LSTs. The two-way analysis of variance showed a significant difference among the studied groups (P < 0.05) at most of the sampling points which indicates the significant improvement achieved by the liquisolid technique. This improvement will be assessed and confirmed by the biochemical analysis of TC, TG, HDL, and LDL as well as the calculation of the atherosclerotic index (AI), as a marker of cardiovascular disease.
Effect of SMV-LST on the Total Cholesterol and Triglycerides
The effect of SMV-LST formulation on the serum total cholesterol and triglycerides levels was assessed in a hyperlipidemic rat model in which the circulating levels of total cholesterol, triglycerides, and LDL were largely increased following administration of poloxamer 407. The induction of hyperlipidemia was confirmed by the milky appearance of the blood sample withdrawn from the rats after 24 h of poloxamer injection and by the significant elevation of the lipid profile parameters of the model group with the normal rat group. It is worthy to note that a group of animals that received the plain tablets (without SMV) that was considered a negative control has been carried out during the preliminary (pilot) study, and this group showed no significant difference when compared with the model group. SMV-LSTs at a single dose of 10 mg/kg body weight significantly reduced the serum total cholesterol by ~ 33% after half an hour. After an hour, SMV-LST formulation reduced the total cholesterol by ~ 50% which was significantly different from the corresponding commercial SMV tablets (P < 0.05) (Fig. 6a). The percent of total cholesterol reduction gradually increased by time until 4 h of administration in rats pre-treated with poloxamer 407. This result is in agreement with a previous report by Wang et al., who reported that at a higher dose, SMV reduced total circulating cholesterol by 37% in LDLR-KO mice [72].
The effect of SMV on triglycerides in hyperlipidemic rats is shown in Fig. 6 b. The levels of triglycerides in the hyperlipidemic group were significantly higher than those in the control group (P < 0.0001). After half an hour of treatment with commercial SMV and SMV-LST formulation, the levels of triglycerides were significantly decreased by 16.67% (P < 0.001) and 40.30% (P < 0.0001) compared with the hyperlipidemic group. After 1 h, both drug formulations gradually and significantly decreased the levels of triglycerides, compared to the hyperlipidemic group, until they reached the normal level (140 mg/dl) at 12 h (Fig. 6b). Interestingly, the optimized SMV-LST formulation significantly lowered the triglyceride at 0.5, 1.5, and 2 h of treatment versus the commercial SMV tablets. These results indicated that the optimized SMV-LST formulation was more effective than the commercial SMV tablets in reducing the lipid contents in the serum of hyperlipidemic rats.
Effect of SMV-LST on Serum Lipoproteins
As shown in Fig. 6 c, the treatment of hyperlipidemic rats with SMV, in the form of commercial tablets or the prepared optimized SMV-LST formulation tended to increase serum levels of HDL compared to the model group. Unlikely, the difference was not significant versus the model, before 4 h. However, after 4, 6, and 8 h, the optimized SMV-LST formulation significantly augmented the serum HDL levels compared to the commercial SMV tablets by 47.6%, 35.89%, and 28.6% respectively (Fig. 6c).
Based on these results, HDL was expressed as a percentage of all cholesterol or the atherosclerotic index (AI), a marker of cardiovascular disease. The AI was calculated according to this formula, log(Triglyceride / HDL-Cholesterol) for all groups [73, 74]. When AI was calculated, the net benefit of the treatments was more obvious as shown in Fig. 7. The optimized SMV-LST formulation showed a significant decrease in the AI value at 1.5 h compared to the model group (P < 0.01). Furthermore, higher significances were reached at 2 h and more (P < 0.0001). The commercial SMV tablets started to show lower AI value with a higher significance difference at 4 h (P < 0.0001).
In contrast to HDL, the level of LDL was decreased in the serum of hyperlipidemic rats treated with the commercial SMV tablets and the optimized SMV-LST formulation. In particular, at 0.5 h, the optimized SMV-LST formulation reduced the serum LDL by 23.8% (P < 0.01) compared to the model group. At 1 h, the serum LDL was reduced by 44.6% (P < 0.0001) which is significantly different from the commercial SMV tablets (P < 0.05) (Fig. 6d). These results indicated that SMV could decrease the risk of coronary disease and atherosclerosis by raising the level of HDL and lowering LDL levels.
Results obtained from the pharmacokinetic and pharmacodynamic studies indicated an enhancement in SMV bioavailability and hypolipidemic activity after treatment with the LST formulation. This enhancement is expected to decrease the drug dose and side effect. A more potent pharmacological activity is expected from the SMV-LSTs containing the same drug dose available in the corresponding commercial product.
CONCLUSIONS
In the present study, the liquisolid technique was shown to be an appropriate method for improvement of the rate and extent of SMV dissolution. Box-Behnken design was successfully employed to achieve this goal by optimizing the formulation factors of the liquisolid formulation that shorten the MDT and maximize both DR10 and DE60. With the use of the optimized SMV-LST formulation, the oral bioavailability of SMV has been improved with 148.232% when compared with the commercial tablets on the induced hyperlipidemic rats. This improvement was confirmed by the significant reduction of the levels of circulating total cholesterol, triglycerides that reached the normal level after 12 h. In particular, the optimized SMV-LST formulation reduced the serum LDL by 44.6% and increased the level of serum HDL by 47.6% in the rats treated with the optimized SMV-LSTs. Finally, the optimized SMV-LST formulation showed a significantly lower atherosclerotic index value which could maximize its potential in decreasing the risk of coronary disease and atherosclerosis by raising HDL and lowering LDL levels.
References
Stegemann S, Leveiller F, Franchi D, de Jong H, Lindén H. When poor solubility becomes an issue: from early stage to proof of concept. Eur J Pharm Sci Elsevier. 2007;31:249–61.
Wang D, Xing H, Jiang J, Chen X, Yang T, Wang D, et al. Liquisolid technique and its applications in pharmaceutics. Asian J Pharm Sci [Internet]. Elsevier B.V.; 2017;12:115–23. Available from: https://doi.org/10.1016/j.ajps.2016.09.007
Amidon GL, Lennernäs H, Shah VP, Crison JR. A theoretical basis for a biopharmaceutic drug classification: the correlation of in vitro drug product dissolution and in vivo bioavailability. Pharm Res An Off J Am Assoc Pharm Sci. 1995;12:413–20.
Rasenack N, Müller BW. Micron-size drug particles: common and novel micronization techniques. Pharm Dev Technol Informa Healthcare. 2004[cited 2014 Oct 24];9:1–13. Available from: http://informahealthcare.com/doi/abs/10.1081/PDT-120027417.
Ahmed TA, Suhail MAA, Hosny KM, Abd-allah FI. Clinical pharmacokinetic study for the effect of glimepiride matrix tablets developed by quality by design concept. Drug Dev Ind Pharm [Internet]. Informa Healthcare USA, Inc; 2017;0:1–16. Available from: https://doi.org/10.1080/03639045.2017.1371740.
Ahmed T. Preparation of finasteride capsules-loaded drug nanoparticles: formulation, optimization, in vitro, and pharmacokinetic evaluation. Int J Nanomedicine Dove Press. 2016;11:515–27.
Ahmed TA, El-Say KM. Transdermal film-loaded finasteride microplates to enhance drug skin permeation: Two-step optimization study. Eur J Pharm Sci. Elsevier B.V. 2016;88:246–56.
Al-Subaie MM, Hosny KM, El-Say KM, Ahmed TA, Aljaeid BM. Utilization of nanotechnology to enhance percutaneous absorption of acyclovir in the treatment of herpes simplex viral infections. Int J Nanomedicine. 2015;10:3973–3985. Available from: http://www.dovepress.com/permissions.php.
El-Say KM, Ahmed TA, Ahmed OAA, Hosny KM, Abd-Allah FI. Self-nanoemulsifying lyophilized tablets for flash oral transmucosal delivery of vitamin K: development and clinical evaluation. J Pharm Sci. 2017;106:2447–56.
de Lima IA, Khalil NM, Tominaga TT, Lechanteur A, Sarmento B, Mainardes RM. Mucoadhesive chitosan-coated PLGA nanoparticles for oral delivery of ferulic acid. Artif Cells, Nanomedicine Biotechnol. 2018;46:993–1002.
Shegokar R, Athawale R, Kurup N, Yang R, Chougule MB. Lipid-based nanoparticles for targeted drug delivery of anticancer drug. Nanotechnology-Based Approaches Target Deliv Drugs Genes. Academic Press. 2017:287–321.
Ahmed TA. Formulation and clinical investigation of optimized vinpocetine lyoplant-tabs: new strategy in development of buccal solid dosage form. Drug Des Devel Ther Dove Press. 2019 [cited 2019 Jan 20];13:205–220. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30643387.
Tiwari R, Pathak K. Nanostructured lipid carrier versus solid lipid nanoparticles of simvastatin: comparative analysis of characteristics, pharmacokinetics and tissue uptake. Int J Pharm Elsevier BV. 2011 [cited 2019 Jan 20];415:232–243. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0378517311004753.
Murtaza G. Solubility enhancement of simvastatin: a review. Acta Pol Pharm. 2012 [cited 2015 Feb 23];69:581–590. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22876598.
Kang BK, Lee JS, Chon SK, Jeong SY, Yuk SH, Khang G, et al. Development of self-microemulsifying drug delivery systems (SMEDDS) for oral bioavailability enhancement of simvastatin in beagle dogs. Int J Pharm. 2004 [cited 2014 Oct 26];274:65–73. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15072783.
Dixit RP, Nagarsenker MS. Self-nanoemulsifying granules of ezetimibe: design, optimization and evaluation. Eur J Pharm Sci. 2008 [cited 2014 Jan 31];35:183–192. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18652892.
Naseera K, Sajeeth CI, Santhi K. Formulation, optimization, and evaluation of matrix type of transdermal system of simvastatin using permeation enhancers. Int J Curr Pharm Res. 2012;4:79–87.
Singh S, Mandoria N, Shaikh A. Preformulation studies of simvastatin for transdermal drug delivery system. Int Res J Pharm. 2012;3:159–61.
El-Say KM, Ahmed TA, Badr-Eldin SM, Fahmy U, Aldawsari H, Ahmed OAA. Enhanced permeation parameters of optimized nanostructured simvastatin transdermal films: ex vivo and in vivo evaluation. Pharm Dev Technol. 2015 [cited 2014 Oct 20];20:919–926. Available from: http://informahealthcare.com/doi/abs/10.3109/10837450.2014.938859.
Pandya V, Patel J, Patel D. Formulation and optimization of nanosuspensions for enhancing simvastatin dissolution using central composite design. Dissolution Technol. 2011;18:40–5.
Zhang Y, Zhang J, Jiang T, Wang S. Inclusion of the poorly water-soluble drug simvastatin in mesocellular foam nanoparticles: drug loading and release properties. Int J Pharm. 2011 [cited 2014 Oct 24];410:118–124. Available from: http://www.sciencedirect.com/science/article/pii/S0378517310005673.
Pandya P, Gattani S, Jain P, Khirwal L, Surana S. Co-solvent evaporation method for enhancement of solubility and dissolution rate of poorly aqueous soluble drug simvastatin: in vitro-in vivo evaluation. AAPS PharmSciTech. 2008 [cited 2014 Oct 24];9:1247–1252. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2628261&tool=pmcentrez&rendertype=abstract.
Jun SW, Kim M-S, Kim J-S, Park HJ, Lee S, Woo J-S, et al. Preparation and characterization of simvastatin/hydroxypropyl-beta-cyclodextrin inclusion complex using supercritical antisolvent (SAS) process. Eur J Pharm Biopharm 2007 [cited 2014 Oct 24];66:413–421. Available from: http://www.sciencedirect.com/science/article/pii/S0939641106003365.
Elkordy AA, Tan XN, Essa EA. Spironolactone release from liquisolid formulations prepared with Capryol™ 90, Solutol® HS-15 and Kollicoat® SR 30 D as non-volatile liquid vehicles. Eur J Pharm Biopharm. 2013;83:203–23.
Suliman AS, Anderson RJ, Elkordy AA. Norfloxacin as a model hydrophobic drug with unique release from liquisolid formulations prepared with PEG200 and Synperonic PE/L-61 non-volatile liquid vehicles. Powder Technol; Elsevier. 2014;257:156–67.
Javadzadeh Y, Siahi MR, Asnaashari S, Nokhodchi A. Liquisolid technique as a tool for enhancement of poorly water-soluble drugs and evaluation of their physicochemical properties. Acta Pharma. 2007;57:99–109.
Kapure VJ, Pande V V, Deshmukh PK. Dissolution enhancement of rosuvastatin calcium by liquisolid compact technique. J Pharm. Hindawi Publishing Corporation. 2013 [cited 2019 May 3];2013:1–9. Available from: https://doi.org/10.1155/2013/315902.
Walke P, Pawar A, Sonawane D, Bhamber R. Liquisolid : a novel technique to enhance solubility and dissolution rate of BCS class II pharmaceuticals. J Pharm Res. 2011;4:4011–4.
Saeedi M, Akbari J, Morteza-Semnani K, Enayati-Fard R, Sar-Reshteh-Dar S, Soleymani A. Enhancement of dissolution rate of indomethacin using liquisolid compacts. Iran J Pharm Res. Shahid Beheshti University of Medical Sciences. 2011;10:25–34.
Sanka K, Poienti S, Mohd AB, Diwan PV. Improved oral delivery of clonazepam through liquisolid powder compact formulations: in-vitro and ex-vivo characterization. Powder Technol. Elsevier. 2014;256:336–44.
Komala DR, Janga KY, Jukanti R, Bandari S, Vijayagopal M. Competence of raloxifene hydrochloride loaded liquisolid compacts for improved dissolution and intestinal permeation. J Drug Deliv Sci Technol. 2015;30:232–41.
Fahmy R, Kassem M. Enhancement of famotidine dissolution rate through liquisolid tablets formulation: in vitro and in vivo evaluation. Eur J Pharm Biopharm. 2008[cited 2018 Oct 20];69:993–1003. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0939641108000556.
El-Hammadi M, Awad N. Investigating the use of liquisolid compacts technique to minimize the influence of pH variations on loratadine release. AAPS PharmSciTech Springer. 2012;13:53–8.
Khames A. Liquisolid technique: a promising alternative to conventional coating for improvement of drug photostability in solid dosage forms. Expert Opin Drug Deliv. 2013;10:1335–43.
Badawy MA, Kamel AO, Sammour OA. Use of biorelevant media for assessment of a poorly soluble weakly basic drug in the form of liquisolid compacts: in vitro and in vivo study. Drug Deliv. 2016;23:808–17.
Siju VV, Soniwala M, Nagar S. A novel technique to enhance dissolution rate of Cilnidipine using Liquisolid compact and wet granulation. Int J Pharm Sci Drug Res. 2017[cited 2018 Oct 20];9:160–168. Available from: http://ijpsdr.com/index.php/ijpsdr/article/view/551.
Lu M, Xing H, Yang T, Yu J, Yang Z, Sun Y, Ding P. Dissolution enhancement of tadalafil by liquisolid technique. Pharm Dev Technol [Internet]. Taylor & Francis; 2017;22:77–89. Available from: https://doi.org/10.1080/10837450.2016.1189563
Pavani E, Noman S, Syed IA. Liquisolid technique based sustained release tablet of trimetazidine dihydrochloride. Drug Invent Today. 2013;5:302–10.
Nokhodchi A, Aliakbar R, Desai S, Javadzadeh Y. Liquisolid compacts: the effect of cosolvent and HPMC on theophylline release. Colloids Surf B: Biointerfaces. 2010;79:262–9.
Shitara Y, Sugiyama Y. Pharmacokinetic and pharmacodynamic alterations of 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitors: drug-drug interactions and interindividual differences in transporter and metabolic enzyme functions. Pharmacol Ther. 2006;112:71–105.
Adekunle AS, Fatoki JO, Adelusi TI. Antihyperlipidemic and antiatherogenic activity of simvastatin may involve modulation of the expression of lecithin: cholesterol acyl transferase. Acta Biochim Pol 2013 [cited 2020 May 2];60:579–583. Available from: https://pubmed.ncbi.nlm.nih.gov/24273760/.
Nokhodchi A, Javadzadeh Y, Siahi-Shadbad MR, Barzegar-Jalali M. The effect of type and concentration of vehicles on the dissolution rate of a poorly soluble drug (indomethacin) from liquisolid compacts. J Pharm Pharm Sci [Internet]. 2005;8:18–25 Available from: http://www.ncbi.nlm.nih.gov/pubmed/15946594.
Sheehan C. General chapters: <1174> powder flow. USP29-NF24. 2013. p. 3017. Available from: http://www.pharmacopeia.cn/v29240/usp29nf24s0_c1174.html.
The United States Pharmacopeial Convention. Uniformity of dosage units. Stage 6 Harmonization (905). 2011.
Guzik L, Mrozik W, Kamysz W. Determination of simvastatin in pharmaceutical dosage forms by optimized and validated method using HPLC / UV. Croat Chem Acta. 2010;83:371–7.
El-Say KM, Ahmed OAA, Aljaeid BM, Zidan AS. Matrix-type transdermal films to enhance simvastatin ex vivo skin permeability. Pharm Dev Technol. 2017[cited 2018 Oct 20];22:492–499.
Zidan AS, Hosny KM, Ahmed OA, Fahmy UA. Assessment of simvastatin niosomes for pediatric transdermal drug delivery. Drug Deliv. 2016;23:1536–49.
Zhang Y, Huo M, Zhou J, Zou A, Li W, Yao C, et al. DDSolver: an add-in program for modeling and comparison of drug dissolution profiles. AAPS J. 2010 [cited 2017 Nov 18];12:263–271. Available from: http://pubmedcentralcanada.ca/pmcc/articles/PMC2895453/pdf/12248_2010_Article_9185.pdf.
Badr-Eldin SM, Elkheshen SA, Ghorab MM. Improving tadalafil dissolution via surfactant-enriched tablets approach: statistical optimization, characterization, and pharmacokinetic assessment. J Drug Deliv Sci Technol Elsevier. 2017;41:197–205.
Ahuja N, Katare OP, Singh B. Studies on dissolution enhancement and mathematical modeling of drug release of a poorly water-soluble drug using water-soluble carriers. Eur J Pharm Biopharm. 2007 [cited 2018 Oct 20];65:26–38. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16962750.
Chella N, Narra N, Rao TR. Preparation and characterization of liquisolid compacts for improved dissolution of telmisartan. J Drug Deliv. 2014;692793:10.
Bernal NP, Calpena AC, Mallandrich M, Ruiz A, Clares B. Development, physical-chemical stability, and release studies of four alcohol-free spironolactone suspensions for use in pediatrics. Dissolution Technol. 2014 [cited 2018 Oct 20];21:19–30. Available from: http://www.dissolutiontech.com/DTresour/201402Articles/DT201402_A03.pdf.
Simionato LD, Petrone L, Baldut M, Bonafede SL, Segall AI. Comparison between the dissolution profiles of nine meloxicam tablet brands commercially available in Buenos Aires, Argentina. Saudi Pharm J. 2018[cited 2018 Oct 20];26:578–584. Available from: https://doi.org/10.1016/j.jsps.2018.01.015.
Gohel MC, Sarvaiya KG, Mehta NR, Soni CD, Vyas VU, Dave RK. Assessment of similarity factor using different weighting approaches. Dissolution Technol. 2005 [cited 2018 Oct 20];12:22–7. Available from: https://pdfs.semanticscholar.org/1b8c/7123cbc98f3006fdd85cde07b2c7c0893198.pdf.
Costa P. An alternative method to the evaluation of similarity factor in dissolution testing. Int J Pharm. 2001 [cited 2018 Oct 20];220:77–83. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11376969.
Shah VP, Tsong Y, Sathe P, Liu JP. In vitro dissolution profile comparison- statistics and analysis of the similarity factor, f2. Pharm Res. 1998[cited 2018 May 29];15:889–896.
Chaudhary HR, Brocks DR. The single dose poloxamer 407 model of hyperlipidemia; systemic effects on lipids assessed using pharmacokinetic methods, and its effects on adipokines. J Pharm Pharm Sci. 2013;16:65–73.
Kurakula M, Ahmed T. Co-delivery of atorvastatin nanocrystals in PLGA based in situ gel for anti-hyperlipidemic efficacy. Curr Drug Deliv. 2015;13:211–20.
Elimam H, Ramadan BK. Comparative study of the possible prophylactic and curative effects of flaxseed oil on the lipid profile and antioxidant status of hyperlipidaemic rats. J Appl Pharmacol. 2018;10:1–6.
Khanfar M, Salem MS, Hawari R. Formulation factors affecting the release of ezetimibe from different liquisolid compacts. Pharm Dev Technol. 2013;18:417–27.
Patel DD, Anderson BD. Adsorption of polyvinylpyrrolidone and its impact on maintenance of aqueous supersaturation of indomethacin via crystal growth inhibition. J Pharm Sci. 2015;104:2923–33.
Staniforth JN, Aulton ME. Powder flow. In: Aulton ME, editor. Ault pharm des Manuf med. 3rd ed. London: Churchill Living stone Elservier; 2007. p. 168–80.
The United States Pharmacopeia TNF. USP 28/NF 23. Rockville: US Pharmacopoeial Convention Inc.; 2005.
El-Say KM, Ahmed OAA, Aldawsari HM, Badr-Eldin SM. Influence of different variables on the dissolution behavior of carvedilol from liquisolid compacts using response surface methodolgy. Dig J Nanomater Biostructures. 2019;14:879–94.
Patel DS, Pipaliya RM, Surti N. Liquisolid tablets for dissolution enhancement of a Hypolipidemic drug. Indian J Pharm Sci Wolters Kluwer-Medknow Publications; 2015 [cited 2018 May 29];77:290–298. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26180274.
Nokhodchi A, Hentzschel CM, Leopold CS. Drug release from liquisolid systems: speed it up, slow it down. Expert Opin Drug Deliv. 2011;8:191–205.
Yadav VB, Yadav AV. Improvement of solubility and dissolution of indomethacin by liquisolid and compaction granulation technique. J Pharm Sci Res. 2009;1:44–51.
Khames A. Investigation of the effect of solubility increase at the main absorption site on bioavailability of BCS class II drug (Risperidone) using liquisolid technique. Drug Deliv. 2017;24:328–38.
Javadzadeh Y, Siahi MR, Asnaashari S, Nokhodchi A. An investigation of physicochemical properties of piroxicam liquisolid compacts. Pharm Dev Technol. 2007;12:337–43.
El-Say KM, Samy AM, Fetouh MI. Optimization of rofecoxib liquisolid tablets using Box-Behnken design and desirability function. J Pharm Res. 2010;3:2388–92.
Diaz DA, Colgan ST, Langer CS, Bandi NT, Likar MD, Van Alstine L. Dissolution similarity requirements: how similar or dissimilar are the global regulatory expectations? AAPS J. Springer. 2016;18:15–22.
Wang YX, Martin-McNulty, Baby, Huw LY, da Cunha V, Post J, Hinchman, Josephine, Vergona R, Sullivan ME, et al. Anti-atherosclerotic effect of simvastatin depends on the presence of Apolipoprotein E. Atherosclerosis. 2002;162:23–31.
Kanthe PS, Patil BS, Bagali S, Deshpande A, Shaikh GB, Aithala M. Atherogenic index as a predictor of cardiovascular risk among women with different grades of obesity. Int J Collab Res Intern Med Public Heal. 2012;4:1767–74.
Dobiásová M, Frohlich J. The plasma parameter log (TG/HDL-C) as an atherogenic index: correlation with lipoprotein particle size and esterification rate in apoB-lipoprotein-depleted plasma (FER(HDL)). Clin Biochem. 2001;34:583–8.
Acknowledgments
This project was funded by the Deanship of Scientific Research (DSR) at King Abdulaziz University, Jeddah, under grant no. G:177-166-1440. The authors, therefore, acknowledge with thanks DSR for the technical and financial support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
El-Say, K.M., Ahmed, T.A., Ahmed, O.A.A. et al. Enhancing the Hypolipidemic Effect of Simvastatin in Poloxamer-Induced Hyperlipidemic Rats via Liquisolid Approach: Pharmacokinetic and Pharmacodynamic Evaluation. AAPS PharmSciTech 21, 223 (2020). https://doi.org/10.1208/s12249-020-01754-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-020-01754-5