Abstract
Amorphous solid dispersions (ASD) are one of the most important supersaturating drug delivery systems (SDDS) for poorly water-soluble drugs to improve their bioavailability. As a result of thermodynamic instability, drug molecules tend to precipitate during storage and dissolution in gastrointestinal tract. Various precipitation inhibitors (PI) have been widely used to improve the stability in the past decade. However, most studies have investigated the inhibiting capability of PI on drug precipitation, rarely considering their potential hindering effect on the drug dissolution. The present study designed an ASD of Indomethacin (IND) and Eudragit® EPO by hot melt extrusion to investigate the influence of the added PI (PVP-K30) into ASD both on dissolution and precipitation. The precipitation study by solvent shift method indicated PVP-K30 could inhibit the precipitation of IND significantly. The dissolution study in different concentrations of PVP-K30 showed when the concentration increased above 50 μg/mL, PVP-K30 displayed an acceptable precipitation inhibition without drug concentration decline but an unexpected dissolution impediment with the reduction of maximum concentration platform. The dissolution tests of physical mixtures (PMs) of ASD and PVP-K30 also showed the precipitation inhibition and dissolution impediment when more than 2% PVP-K30 in PMs. This opposed effect of PVP-K30 was strengthen in ternary systems prepared by hot melt extruding the mixtures of IND, Eudragit® EPO and PVP-K30. All of these results proved the PI may be a double-edged sword for the opposed effects of precipitation inhibition and dissolution impediment, which should be carefully considered in the design and development of SDDS.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
INTRODUCTION
With the application of combinatorial chemistry and high-throughput screening in drug discovery, an increase of poorly water-soluble drug candidates with compromised therapeutic efficacy has emerged (1). It is estimated approximately 40% of marketed drugs and up to 75% of compounds under development are poorly water-soluble (2,3), dramatically challenging their oral bioavailability due to inadequate dissolution and subsequently poor absorption in the gastrointestinal (GI) tract. Therefore, the enhancement of solubility and dissolution rate is important to obtain acceptable oral bioavailability in the design and development of such drugs. Thus far, several strategies have been investigated to address the poor water solubility problem, such as micronization (4), cyclodextrin complexation (5), salt formation (6), cocrystal formation (7), use of surfactants, and solid dispersion (8). Among these, salt/cocrystal formations and amorphous solid dispersions (ASD) have been called as supersaturating drug delivery systems (SDDS) owing to their significant enhancement of apparent drug solubility (9,10). SDDS are defined as systems that contain the drug in a high-energy state or otherwise in a rapidly dissolving form so that the concentration of dissolved drugs in GI tract can be much higher than the equilibrium solubility, providing sufficient drug concentration to promote drug absorption (11,12,13).
Polymer-based ASD, in which the drug is molecularly dispersed in appropriate polymeric carriers, has been increasingly utilized as an effective SDDS because of its rapid dissolution and uncomplicated scale-up manufacturing (14). Attributing to the lack of ordered crystal lattice, the drugs dissolve rapidly and generate the concentration higher than the thermodynamic equilibrium solubility of the stable crystal form (15,16,17). Obviously, this high concentration is thermodynamically unstable so that the drug molecule probably precipitates in vivo before being absorbed, resulting in compromised bioavailability (9,18,19). Therefore a major challenge in developing such SDDS is to maintain the high energetic supersaturated state for a sufficient duration and to prevent the drug precipitation (11,13,20). Recently precipitation inhibitors (PI) have been widely explored to preserve drugs in the supersaturated state by inhibiting the nucleation and/or the crystal growth involved in the precipitation process (9,21,22). Vandecruys et al. (23) investigated the precipitation inhibitory effect of various excipients on 25 drugs and found that cyclodextrin (CD), hydroxypropylmethyl cellulose (HPMC), and polyvinylpyrrolidone (PVP) could maintain the supersaturation of drugs for a relative long time. Chauhan et al. (24) reported that the strength of molecular interaction between drugs and polymers was extremely important, which led to the rank order of precipitation inhibitory effect on Indomethacin with PVP-K90 > Eudragit® E100 > HPMC. Patel and Anderson (25) explored the mechanism of inhibitory effect by different PI, and found that CD could reduce the driving force for crystal growth, while PVP obstructed crystallization through the adsorption on growing drug crystals.
So far as we know, most of the current studies have focused on the effect of PI on drug precipitation process in SDDS to prolong supersaturation time as well as to promote drug dissolution. However, there is a lack of research focusing on the impediment effect of PI on drug dissolution related to its concentration, even as it is well known the polymer will impact the drug dissolution through changing the wettability of drugs and the viscosity of the environment. The present study aimed to delve into the multiple effects of PI both on drug dissolution and precipitation based on ASD prepared by hot melt extrusion. Indomethacin (IND), a poorly soluble nonsteroidal anti-inflammatory drug, was chosen as a model drug, for IND has been a favored compound for dynamic crystallization study (25,26,27,28) and the studies about IND ASD were frequently reported (29,30,31,32).
MATERIALS AND METHODS
Materials
Indomethacin (IND) was purchased from Henan Mingzhe Biotechnology Co., Ltd. (Henan, China). Eudragit® EPO (EEP) was donated by Evonik Industries AG (Darmstadt, Germany). Polyvinylpyrrolidone (PVP)-K30 was purchased from Anhui Sunhere Pharmaceutical Excipients Co., Ltd. (Anhui, China). All other reagents were of analytical grade and used without further purification.
Preparation of IND solid dispersions by hot melt extrusion
Hot melt extrusion was performed by using a laboratory scale instrument (MiniCTW; Thermo Fisher Scientific, Germany). For the binary system (IND-EEP), IND was extruded with EEP at the ratio of drug to polymer of 4:1 (w/w) while IND to PVP-K30 (IND-PVP) of same ratio was used as a control. For the ternary system (IND-EEP-PVP), IND and EEP were extruded with PVP-K30 together at which the ratio of IND to EEP remained 4:1 (w/w) unchanged with various amounts of PVP-K30. The temperature and speed of the extrusion were selected at 140°C and 30 rpm. Finally, the hot melt extrudates (HMEs) were collected, allowed to cool, milled using mortar, and screened through a 120 mesh sieve.
Preparation of Physical Mixtures (PMs) of IND-EEP HMEs and PVP-K30
The IND-EEP HMEs (screened through a 120 mesh sieve) were mixed gently yet homogenously with different quantity of precipitation inhibitor PVP-K30 (sieved through a 120 mesh sieve). For well-distributed, PMs were sieved through an 80 mesh sieve three times.
Differential Scanning Calorimetry (DSC)
DSC1/700 (Mettler-Toledo, Zurich, Switzerland) was used to conduct DSC tests of IND, EEP, IND-EEP HMEs, and PMs of IND and EEP. About 5 mg powder samples were weighed into aluminum pans and heated from 25 to 200°C at a heating rate of 10°C/min under a nitrogen atmosphere.
Powder X-ray diffraction (PXRD)
The physical states of IND, EEP, IND-EEP HMEs, and PMs of IND and EEP were analyzed by X-ray diffractometer (X’Pert PRO, PNAlytical, Netherlands). The Patterns were obtained by means of a step width of 0.02°C with a detector resolution in 2θ between 5° and 45° at ambient temperature.
The precipitation inhibition of PVP-K30 in supersaturated solution
The solvent shift method (33) was used to observe the effect of PVP-K30 on drug precipitation in IND supersaturated solution. Supersaturation was generated by adding 0.5 mL of IND solution (5 mg/mL in methanol) rapidly to 50 mL of media (0.1 N hydrochloric acid) with continuous stirring at 37°C in a jacketed beaker. Different concentrations of PVP-K30 were pre-dissolved in 0.1 N hydrochloric acid, while the precipitation media without polymers was used as a control. Meanwhile, drug concentrations in media were measured as a function of time using UV-Vis spectrophotometer coupled with an in situ fiber optic probe (AvaSpec-ULS2048CL, Avantes, Holland). The difference in absorbance at 320 nm and extinction at 450 nm was calculated and converted to concentrations using calibration curves (34).
Dissolution studies
The USP II dissolution apparatus (Tianda Tianfa Technology Co., Ltd., Tianjin, China) was used to monitor the dissolution profiles of the powders of IND, IND-EEP HMEs, IND-EEP PMs, IND-PVP HMEs, and IND-EEP-PVP HMEs. Dissolution studies were carried out with samples containing 25 mg IND in 900 mL 0.1 N hydrochloric acid at 37°C and 100 rpm with the USP rotating paddle method. 10 mL aliquot was removed and replaced with same fresh dissolution medium at the predetermined intervals. The aliquot was then passed through a 0.45 μm membrane filter, and drug concentration in the aliquot was determined UV-spectrophotometrically (New Century UV-Vis spectrophotometer T6, General Analysis Beijing General Instrument Co., Ltd.) at 265 nm for IND. Additionally, dissolution tests of IND-EEP HMEs in 0.1 N hydrochloric acid solutions with different pre-dissolved PVP-K30 also were performed at same methods. All dissolution tests were performed in triplicates.
RESULTS AND DISCUSSION
Characterization of IND-EEP HMEs
Numerous researches about IND ASD have been reported recently due to its excellent solubility promotion ability. Compared with other carriers, EEP could significantly enhance the dissolution rate of IND ASD in hydrochloric acid, showing a typical “spring” effect with rapid initial buildup of the drug supersaturation but subsequent precipitation of the drug (29,35). And a higher supersaturation could be achieved with an increase of EEP in such IND ASD (36). However, Sun and Lee (37) proved that the high level of supersaturation was not always good for drug dissolution as the maximum achievable supersaturation of the amorphous solids increased, the rate of concentration decline in the de-supersaturation phase increased. Considering this, the ASD with a low carrier content was prepared by hot melt extrusion at the ratio of drug (IND) to polymer (EEP) of 4:1 (w/w).
Dissolution profiles of IND, PMs of IND and EEP (4:1, w/w), and IND-EEP HMEs are presented in Fig. 1, from which we could see that very few drugs were dissolved for the sample of IND owing to the poor solubility (1.5 μg/mL at pH 1.2) (31,34). After mixed with EEP, IND showed only a negligible improvement of dissolution in PMs, which was agree with the results reported by Prasad et.al (32). However, similar to the earlier reports (29,35,36), IND-EEP HMEs exhibited a rapid burst of drug dissolution to the maximum drug concentration of 14.43 μg/mL at 5 min and subsequently followed by a concentration decline triggered by the precipitation of dissolved IND. This suggested that EEP was an effective dissolution-promoting agent but not an acceptable precipitation inhibitor for IND ASD.
In order to explain the “spring” effect of drug dissolution, DSC and PXRD were used to verify the final physical states of IND-EEP HMEs and compared with those of IND, EEP, and IND-EEP PMs. As presented in Fig. 2, IND drug substance exhibited a melting endotherm at 161.92°C and EEP showed a Tg of 56.83°C. For IND-EEP PMs, the endothermic peak was slightly moved to the left (160.33°C) and became broader compared with IND (161.92°C), indicating that IND and EEP had a molecular interaction in their PMs with hydrogen bond between drug and polymer (32,38). However, the presence of two slight peaks in IND-EEP HMEs at 59.01°C and 151.69°C demonstrated that a small quantity of incorporated drug was still in crystalline form at such a high drug loading HMEs. And the movement of the peak in IND-EEP HMEs suggested that there was a stronger interaction between the IND and EEP compared with their PMs.
PXRD patterns of IND, EEP, IND-EEP HMEs, and IND-EEP PMs are displayed in Fig. 3. IND exhibited characteristic peaks over the 2θ range at 11.6°, 12.7°, 17.0°, 19.6°, 21.9°, 24.0°, 26.6°, 29.4°, 33.6°, 37.5° which showed a typical crystalline profile of γ-polymorph and was in accordance with previous studies (39,40), whereas EEP used in the present study showed broad amorphous bands and IND-EEP PMs showed same characteristic peaks with IND. As expected, the characteristic peaks of IND-EEP HMEs at 17.0°, 24.0°, 29.4°, and 33.6° were evidently weaker than those presented with IND-EEP PMs, demonstrating there were partial amorphous drugs in IND-EEP HMEs.
Although Prasad et.al (32) reported the solid dispersion of 90%IND and 10%EEP prepared by solvent evaporation method could be amorphous completely, the DSC and PXRD patterns in Figs. 2 and 3 show that a small part of drugs was crystalline in INE-EEP HMEs. But it could be concluded the vast majority of drugs in IND-EEP HMEs were amorphous for there was still a striking “spring” effect of the dissolved IND in dissolution profiles which came from the high-energy state such as the amorphous form.
Effect of PVP-K30 on drug precipitation of supersaturated solution
In order to reduce or eliminate the subsequent drug precipitation, it is a common practice to employ suitable PI acted as “parachute” to retard the decline of drug concentration. One of the most widely used PI is PVP due to its strong precipitation inhibition, good biocompatibility, and low cost. To study the inhibitory effect of PVP-K30 on IND precipitation, the initial supersaturated concentration in solutions was generated by adding 0.5 mL of 5 mg/mL IND methanolic solution to 50 mL of precipitation medium. Concentration-time profiles of supersaturated IND solution in the absence of polymer as well as in the presence of pre-dissolved PVP-K30 with different concentrations are presented in Fig. 4. The percentage of IND precipitated at 30 min, which was calculated by the difference in initial IND concentration and final concentration, is shown in Fig. 5.
In absence of PVP-K30 (No PVP-K30), IND precipitated rapidly with the sharply dropping in concentration (Fig. 4) attributed by the nucleation and the growth of crystals, in which the concentration of IND decreased from 50 μg/mL to 7.7 μg/mL with the precipitation percentage of 81.42 ± 3.02% in 30 min (Fig. 5). In the presence of pre-dissolved PVP-K30 with 0.7 μg/mL, there was no significant effect on drug precipitation at such a low concentration with 81.94 ± 3.74% IND precipitated in 30 min as shown in Fig. 5 (p > 0.05, compared with No PVP-K30). However, as the PVP-K30 increased to 2 μg/mL, the decline rate of dissolved IND became mild (Fig. 4) and the percentage of precipitated IND from supersaturated solution slightly decreased (63.89 ± 4.36%) compared with the reference group without PVP-K30 (p < 0.05). With the further increase of the PI to 50 μg/mL, it was obvious that PVP-K30 retarded the precipitation rate of IND with only 27.57 ± 8.88% IND precipitated in 30 min. Unexpectedly, when the concentration of pre-dissolved PVP-K30 in medium was further improved to 1 mg/mL, no distinct changes of concentration-time profiles were observed compared to 50 μg/mL pre-dissolved PVP-K30 in medium with 38.00 ± 0.03% IND precipitated in 30 min (p > 0.05, compared with 50 μg/mL PVP-K30). The above results indicated PVP-K30 was an effective precipitation inhibition for IND. The presence of PVP-K30, even with a very low concentration of 2 μg/mL, could have a significant effect on drug precipitation inhibition. However, surplus pre-dissolved PVP-K30 made no big difference, which meant no further advance of the inhibiting ability was achieved.
Effect of PVP-K30 on drug dissolution of IND-EEP HMEs
Although the utilization of PVP-K30 could retard precipitation and maintain supersaturation to produce adequate drug absorption, the presence of PVP might affect drug molecules to contact with water as well as the diffusion of drug molecules, causing complicated influence of drug dissolution. The dissolution tests of IND-EEP HMEs in different pre-dissolved PVP-K30 were performed to investigate the effect of PI on drug dissolution.
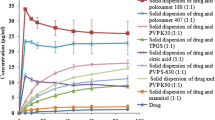
As shown in Fig. 6 (a), with low concentration of pre-dissolved PVP-K30 at 2 or 10 μg/mL, PVP-K30 in medium had no influence on initial accumulation of drug supersaturation with comparison of the absence of PVP-K30. And the IND concentration rapidly achieved the maximum of 14.45 μg/mL and 14.08 μg/mL at 5 min, respectively. However, compared to the reference group of No PVP-K30, the reduction rate of drug concentration in pre-dissolved PVP-K30 of 2 and 10 μg/mL became slower after 5 min, which suggested that at such low concentrations PVP-K30 did not impact initial drug release but interfered with drug nucleation and/or crystal growth. When further increasing the pre-dissolved PVP-K30 to 50 μg/mL in medium, the IND concentration reached the plateau at 10 min and could be sustained within an hour. This agreed with above results in drug precipitation of solvent shift method, confirming that the PVP-K30 of 50 μg/mL in medium could strongly inhibit the precipitation of IND supersaturated solution.
When further increasing the pre-dissolved PVP-K30 in dissolution medium, there was a negative influence on drug dissolution of IND-EEP HMEs as shown in Fig. 6 (b). Although the concentration decline disappeared in the presence of pre-dissolved PVP-K30 at 0.5, 1.0, 5.0 mg/mL, the initial buildup of drug supersaturation became slower and the plateau concentration became lower with the concentration of PVP-K30 increased, which led to a stronger hindrance to drug dissolution.
As previous studies about effect of PI on drug precipitation process reported (11,21,41,42), PI can act by numerous possible mechanisms to retard drug precipitation including: (1) nucleation interference; (2) enhancement of viscosity to limit diffusion through the diffusion layer from the supersaturated bulk to the crystal solid surface during crystal growth; (3) adsorption onto the crystal surface to affect the integration of drug molecules into the crystal. Among these, PVP-K30 as an effective PI can adsorb onto IND crystal surfaces providing an interfacial barrier for crystal growth (25). However, the drug dissolution profile is the macroscopic reflection of two radical processes, dissolution, and precipitation, which may occur at the same time. Despite of a great inhibitory effect on drug precipitation, the surplus addition of PVP-K30 possibly affect the drug diffusion from particle surface to bulk medium, resulting in negative impact on the drug dissolution rate.
Effect of mixing PVP-K30 with IND-EEP HMEs on drug dissolution
Above results confirmed that the presence of pre-dissolved PVP-K30 in medium had significant impact on drug dissolution besides playing a crucial role in the inhibition of drug crystallization and precipitation, so different proportion of PMs with IND-EEP HMEs and PVP-K30 were prepared to investigate the effect of PI in SDDS on drug dissolution.
As shown in Fig. 7, when 1% PVP-K30 was added in PMs (HMEs-PVP 5:0.05 PMs), the decrease of IND concentration after 5 min became much slower than that of IND-EEP HMEs, suggesting that PVP-K30 was an effective PI which made obvious inhibitory effect even at such a small amount. But there was still a tendency of drug decline in HMEs-PVP 5:0.05 PMs in an hour. While PVP-K30 in PMs increased to 2% (HMEs-PVP 5:0.1 PMs), a high supersaturated concentration of 13.10 μg/mL was achieved in 10 min and sustained for an hour without any decline. Interestingly, when PVP-K30 further increased to 9 and 17%, that was HMEs-PVP 5:0.5 PMs and HMEs-PVP 5:1 PMs, the maximum achieved concentration was reduced significantly compared to 5:0.1 PMs, with 10.81 μg/mL and 8.99 μg/mL at an hour, respectively. All of these results illustrated that although PVP-K30 showed an excellent effect of precipitation inhibition, the drug dissolution rate was undoubtedly hindered with PVP-K30 increased in PMs, which confirmed that PI had opposed effects of drug dissolution and precipitation with the quantity dependence. .
Moreover, compared dissolution profiles of pre-dissolved PVP-K30 (Fig. 6) with those of HMEs-PVP PMs (Fig. 7), it was worth noting that the amount of PVP-K30 added in PMs was much lower than that of pre-dissolved in medium with the similar effect on dissolution and precipitation. For instance, HMEs-PVP 5:0.05 PMs had an almost same dissolution profile with that in the presence of pre-dissolved PVP-K30 of 10 μg/mL, while HMEs-PVP 5:0.1 PMs was same as in the presence of pre-dissolved PVP-K30 of 1 mg/mL. Assuming that PVP-K30 in HMEs-PVP 5:0.05 PMs and HMEs-PVP 5:0.1 PMs was completely dissolved in medium, concentrations of PI were 0.35 μg/mL and 0.7 μg/mL in bulk, respectively. As mentioned above (Fig. 4), at such low concentrations PVP-K30 did not show obvious effect of precipitation inhibition. However, the reduction rate of dissolved IND in HMEs-PVP 5:0.05 PMs was much slower than that of IND-EEP HMEs after 5 min. And the precipitation of supersaturated IND solution was completely inhibited during the dissolution of HMEs-PVP 5:0.1 PMs for no decline of IND concentration was observed. A rational explanation might be the local concentration of PI surrounding the drug particles was higher in the system of HMEs-PVP PMs.
In order to explain the behavior of drug molecules in the medium, the following steps including dissolution and precipitation can occur in HMEs-PVP PMs (Fig. 8): (1) Drug particles are wetted with the medium and dissolved, forming the dissolution diffusion layer. (2) Dissolved drug molecules are diffused through the layer to the bulk medium (43). (3) The accumulation of drugs in bulk medium reaches the supersaturated concentration as well as the formation of critical nuclei (27). (4) To form larger crystals from critical nuclei, the dissolved drug molecules diffuse from bulk to the crystal growing interface. (5) The dissolved drug molecules incorporate into the crystal lattice, causing the growth of crystals and drug precipitation (18,26). PVP-K30 as a sensitive PI could impede the step (5) of crystals growth by adsorbing on surface of IND crystals (25,28,44), which led to sustained supersaturation even at low concentration of PVP-K30. When PVP-K30 was increased in SDDS, the step (2) of diffusion in dissolution process was hindered due to enhanced viscosity of diffusion layer, causing a dramatic reduction of drug dissolution rate. Therefore, although the addition of PVP-K30 could reduce the precipitation from supersaturated solution, the dissolution rate was also reduced at the same time resulting from the decrease of diffusion in step (2). When the rate of drug dissolution was reduced to the level of precipitation, the plateau concentration was maintained which was decreased when the amount of PVP-K30 increased as shown in Figs. 6 and 7.
Dissolution studies of ternary IND-EEP-PVP HMEs
To investigate the opposed effect of PVP-K30 on the dissolution further, the ternary systems of IND, EEP, and PVP-K30 were prepared by hot melt extrusion with the ratio of 4:1:0.01, 4:1:0.05, and 4:1:1 (w/w/w, IND-EEP-PVP). The results of dissolution profiles of ternary IND-EEP-PVP HMEs in 0.1 N hydrochloric acid are presented in Fig. 9, from which we could see the decline of IND concentration disappeared completely in all ternary HMEs. Compared to PMs of IND-EEP and PVP-K30 at the same ratio, all of the ternary HMEs showed a much lower dissolution rate. When PVP-K30 in ternary HMEs was more than 1% (IND-EEP-PVP 4:1:0.05 and 4:1:1 HMEs), the dissolved IND was increased slowly with the concentration below 6 μg/mL in an hour. When PVP-K30 in ternary HMEs was decreased to 0.2% (IND-EEP-PVP 4:1:0.01 HMEs), the drug dissolution was obviously improved with a concentration of 7.66 μg/mL at 5 min and then maintained the level without the trend of decline. This suggested that co-extrusion of PVP-K30 with IND and EEP strengthened the opposed effects on drug dissolution and precipitation due to a higher local concentration of PI surrounding the drug particles.
CONCLUSION
The presence of PI in a SDDS can successfully retard the precipitation process by interfering with nucleation and/or crystal growth of the drug molecules in a high-energy sate, generating a sustained supersaturating concentration. However, the unexpected changes in drug dissolution from SDDS caused by PI have barely been studied, which may challenge the therapeutic effect of the drugs. The present study comprehensively investigated such changes of drug dissolution caused by adding PI (PVP-K30) to an ASD of IND and EEP produced by hot melt extrusion. It was found that although PVP-K30 was an excellent PI to control the precipitation of IND supersaturated solution, it did negatively impact the dissolution of IND with a behavior of PVP quantity dependence in the situations of pre-dissolved PVP-K30 solution, powder mixing of PVP-K30 with the IND-EEP extrudates or ternary IND-EEP-PVP extrudates. Interestingly, co-extrusion of PVP-K30 with IND and EEP deteriorated the dissolution behavior of extrudates as a result of strengthened impediment on drug dissolution and precipitation for a higher local concentration of PI surrounding the drug particles. To take full advantages of SDDS for overcoming the problem of solubility-limited oral bioavailability, more research is needed to fully and in-depth understand the impact of PI on dissolution, crystallization, and precipitation of drug molecules in SDDS, providing theoretical basis for the rational design and development of SDDS for poorly water-soluble drugs.
References
Lipinski CA. Drug-like properties and the causes of poor solubility and poor permeability. J Pharmacol Toxicol Methods. 2000;44:235–49. https://doi.org/10.1016/S1056-8719(00)00107-6.
Di L, Kerns EH, Carter GT. Drug-like property concepts in pharmaceutical design. Curr Pharm Des. 2009;15(19):2184–94. https://doi.org/10.2174/138161209788682479.
Williams HD, Trevaskis NL, Charman SA, Shanker RM, Charman WN, Pouton CW, et al. Strategies to address low drug solubility in discovery and development. Pharmacol Rev. 2013;65(1):315–499. https://doi.org/10.1124/pr.112.005660.
Kawabata Y, Wada K, Nakatani M, Yamada S, Onoue S. Formulation design for poorly water-soluble drugs based on biopharmaceutics classification system: basic approaches and practical applications. Int J Pharm. 2011;420(1):1–10. https://doi.org/10.1016/j.ijpharm.2011.08.032.
Otero-Espinar FJ, Torres-Labandeira JJ, Alvarez-Lorenzo C, Blanco-Méndez J. Cyclodextrins in drug delivery systems. J Drug Deliv Sci Technol. 2010;20(4):289–301. https://doi.org/10.1016/s1773-2247(10)50046-7.
Guzman HR, Tawa M, Zhang Z, Ratanabanangkoon P, Shaw P, Gardner CR, et al. Combined use of crystalline salt forms and precipitation inhibitors to improve oral absorption of celecoxib from solid oral formulations. J Pharm Sci. 2007;96(10):2686–702. https://doi.org/10.1002/jps.20906.
Shayanfar A, Asadpour-Zeynali K, Jouyban A. Solubility and dissolution rate of a carbamazepine–cinnamic acid cocrystal. J Mol Liq. 2013;187:171–6. https://doi.org/10.1016/j.molliq.2013.06.015.
Yang W, Mcginity JW, Williams RO, Dinunzio JC, Miller DA. Amorphous compositions using concentration enhancing polymers for improved bioavailability of itraconazole. Mol Pharm. 2008;5(6):968–80. https://doi.org/10.1021/mp800042d.
Xu S, Dai WG. Drug precipitation inhibitors in supersaturable formulations. Int J Pharm. 2013;453(1):36–43. https://doi.org/10.1016/j.ijpharm.2013.05.013.
Taylor LS, Zhang GGZ. Physical chemistry of supersaturated solutions and implications for oral absorption. Adv Drug Deliv Rev. 2016;101:122–42. https://doi.org/10.1016/j.addr.2016.03.006.
Brouwers J, Brewster ME, Augustijns P. Supersaturating drug delivery systems: the answer to solubility-limited oral bioavailability? J Pharm Sci. 2009;98(8):2549–72. https://doi.org/10.1002/jps.21650.
Augustijns P, Brewster ME. Supersaturating drug delivery systems: fast is not necessarily good enough. J Pharm Sci. 2012;101(1):7–9. https://doi.org/10.1002/jps.22750.
Fong SY, Bauer-Brandl A, Brandl M. Oral bioavailability enhancement through supersaturation: an update and meta-analysis. Expert Opin Drug Deliv. 2017;14(3):403–26. https://doi.org/10.1080/17425247.2016.1218465.
He Y, Ho C. Amorphous solid dispersions: utilization and challenges in drug discovery and development. J Pharm Sci. 2015;104(10):3237–58. https://doi.org/10.1002/jps.24541.
Grohganz H, Priemel PA, Löbmann K, Nielsen LH, Laitinen R, Mullertz A, et al. 2014. Refining stability and dissolution rate of amorphous drug formulations. Expert Opin Drug Deliv. 2014;11(6):977–89. https://doi.org/10.1517/17425247.2014.911728.
Vasconcelos T, Marques S. das Neves J, Sarmento B. amorphous solid dispersions: rational selection of a manufacturing process. Adv Drug Deliv Rev. 2016;100:85–101. https://doi.org/10.1016/j.addr.2016.01.012.
Laitinen R, Lobmann K, Grohganz H, Priemel P, Strachan CJ, Rades T. Supersaturating drug delivery systems: the potential of co-amorphous drug formulations. Int J Pharm. 2017;532(1):1–12. https://doi.org/10.1016/j.ijpharm.2017.08.123.
Alonzo DE, Zhang GGZ, Zhou D, Gao Y, Taylor LS. Understanding the behavior of amorphous pharmaceutical systems during dissolution. Pharm Res. 2010;27(4):608–18. https://doi.org/10.1007/s11095-009-0021-1.
Gao P, Shi Y. Characterization of supersaturatable formulations for improved absorption of poorly soluble drugs. AAPS J. 2012;14(4):703–13. https://doi.org/10.1208/s12248-012-9389-7.
Chavan RB, Thipparaboina R, Kumar D, Shastri NR. Evaluation of the inhibitory potential of HPMC, PVP and HPC polymers on nucleation and crystal growth. RSC Adv. 2016;6(81):77569–76. https://doi.org/10.1039/c6ra19746a.
Warren DB, Benameur H, Porter CJ, Pouton CW. Using polymeric precipitation inhibitors to improve the absorption of poorly water-soluble drugs: a mechanistic basis for utility. J Drug Target. 2010;18(10):704–31. https://doi.org/10.3109/1061186X.2010.525652.
Pinto JMO, Leao AF, Riekes MK, Franca MT, Stulzer HK. HPMCAS as an effective precipitation inhibitor in amorphous solid dispersions of the poorly soluble drug candesartan cilexetil. Carbohydr Polym. 2018;184:199–206. https://doi.org/10.1016/j.carbpol.2017.12.052.
Vandecruys R, Peeters J, Verreck G, Brewster ME. Use of a screening method to determine excipients which optimize the extent and stability of supersaturated drug solutions and application of this system to solid formulation design. Int J Pharm. 2007;342(1–2):168–75. https://doi.org/10.1016/j.ijpharm.2007.05.006.
Chauhan H, Kuldipkumar A, Barder T, Medek A, Gu CH, Atef E. Correlation of inhibitory effects of polymers on indomethacin precipitation in solution and amorphous solid crystallization based on molecular interaction. Pharm Res. 2014;31(2):500–15. https://doi.org/10.1007/s11095-013-1178-1.
Patel DD, Anderson BD. Effect of precipitation inhibitors on indomethacin supersaturation maintenance: mechanisms and modeling. Mol Pharm. 2014;11(5):1489–99. https://doi.org/10.1021/mp400658k.
Patel DD, Joguparthi V, Wang Z, Anderson BD. Maintenance of supersaturation I: indomethacin crystal growth kinetic modeling using an online second-derivative ultraviolet spectroscopic method. J Pharm Sci. 2011;100(7):2623–41. https://doi.org/10.1002/jps.22478.
Patel DD, Anderson BD. Maintenance of supersaturation II: indomethacin crystal growth kinetics versus degree of supersaturation. J Pharm Sci. 2013;102(5):1544–53. https://doi.org/10.1002/jps.23498.
Prasad D, Chauhan H, Atef E. Role of molecular interactions for synergistic precipitation inhibition of poorly soluble drug in supersaturated drug-polymer-polymer ternary solution. Mol Pharm. 2016;13(3):756–65. https://doi.org/10.1021/acs.molpharmaceut.5b00655.
Liu H, Wang P, Zhang X, Shen F, Gogos CG. Effects of extrusion process parameters on the dissolution behavior of indomethacin in Eudragit E PO solid dispersions. Int J Pharm. 2010;383(1–2):161–9. https://doi.org/10.1016/j.ijpharm.2009.09.003.
Liu H, Zhu L, Wang P, Zhang X, Gogos CG. Effects of screw configuration on indomethacin dissolution behavior in Eudragit E PO. Adv Polym Technol. 2012;31(4):331–42. https://doi.org/10.1002/adv.20256.
Sun DD, Lee PI. Probing the mechanisms of drug release from amorphous solid dispersions in medium-soluble and medium-insoluble carriers. J Control Release. 2015;211:85–93. https://doi.org/10.1016/j.jconrel.2015.06.004.
Prasad D, Chauhan H, Atef E. Amorphous stabilization and dissolution enhancement of amorphous ternary solid dispersions: combination of polymers showing drug-polymer interaction for synergistic effects. J Pharm Sci. 2014;103(11):3511–23. https://doi.org/10.1002/jps.24137.
Raina SA, Van Eerdenbrugh B, Alonzo DE, Mo H, Zhang GGZ, Gao Y, et al. Trends in the precipitation and crystallization behavior of supersaturated aqueous solutions of poorly water-soluble drugs assessed using synchrotron radiation. J Pharm Sci. 2015;104(6):1981–92. https://doi.org/10.1002/jps.24423.
Xie T, Gao W, Taylor LS. Impact of Eudragit EPO and hydroxypropyl methylcellulose on drug release rate, supersaturation, precipitation outcome and redissolution rate of indomethacin amorphous solid dispersions. Int J Pharm. 2017;531(1):313–23. https://doi.org/10.1016/j.ijpharm.2017.08.099.
Chokshi RJ, Shah NH, Sandhu HK, Malick AW, Zia H. Stabilization of low glass transition temperature indomethacin formulations: impact of polymer-type and its concentration. J Pharm Sci. 2008;97(6):2286–98. https://doi.org/10.1002/jps.21174.
Sarode AL, Sandhu H, Shah N, Malick W, Zia H. Hot melt extrusion (HME) for amorphous solid dispersions: predictive tools for processing and impact of drug-polymer interactions on supersaturation. Eur J Pharm Sci. 2013;48(3):371–84. https://doi.org/10.1016/j.ejps.2012.12.012.
Sun DD, Lee PI. Evolution of supersaturation of amorphous pharmaceuticals: the effect of rate of supersaturation generation. Mol Pharm. 2013;10(11):4330–46. https://doi.org/10.1021/mp400439q.
Liu H, Zhang X, Suwardie H, Wang P, Gogos CG. Miscibility studies of indomethacin and Eudragit(R) E PO by thermal, rheological, and spectroscopic analysis. J Pharm Sci. 2012;101(6):2204–12. https://doi.org/10.1002/jps.23075.
Chamsai B, Sriamornsak P. Physical stabilizing effect of biopolymers on solid dispersions containing indomethacin and polyethylene glycol. Adv Mater Res. 2012;506:307–10. https://doi.org/10.4028/www.scientific.net/AMR.506.307.
Shi NQ, Wang SR, Zhang Y, Huo JS, Wang LN, Cai JH, et al. Hot melt extrusion technology for improved dissolution, solubility and "spring-parachute" processes of amorphous self-micellizing solid dispersions containing BCS II drugs indomethacin and fenofibrate: profiles and mechanisms. Eur J Pharm Sci. 2019;130:78–90. https://doi.org/10.1016/j.ejps.2019.01.019.
Lindfors L, Forssen S, Westergren J, Olsson U. Nucleation and crystal growth in supersaturated solutions of a model drug. J Colloid Interface Sci. 2008;325(2):404–13. https://doi.org/10.1016/j.jcis.2008.05.034.
Surwase SA, Itkonen L, Aaltonen J, Saville D, Rades T, Peltonen L, et al. Polymer incorporation method affects the physical stability of amorphous indomethacin in aqueous suspension. Eur J Pharm Biopharm. 2015;96:32–43. https://doi.org/10.1016/j.ejpb.2015.06.005.
Siepmann J, Siepmann F. Mathematical modeling of drug dissolution. Int J Pharm. 2013;453(1):12–24. https://doi.org/10.1016/j.ijpharm.2013.04.044.
Patel DD, Anderson BD. Adsorption of Polyvinylpyrrolidone and its impact on maintenance of aqueous Supersaturation of indomethacin via crystal growth inhibition. J Pharm Sci. 2015;104(9):2923–33. https://doi.org/10.1002/jps.24493.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, W., Li, M., Yang, Q. et al. The Opposed Effects of Polyvinylpyrrolidone K30 on Dissolution and Precipitation for Indomethacin Supersaturating Drug Delivery Systems. AAPS PharmSciTech 21, 107 (2020). https://doi.org/10.1208/s12249-020-01647-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-020-01647-7