Abstract
This study reports the microemulsion (ME) effects on the permeation of genistein across normal (intact) and microporated human skin. The genistein formulation was optimized to know the stable ME region in the pseudo-ternary phase diagrams and to maximize the skin permeation and retention of genistein. The phase diagrams were constructed with different oil phases, surfactants, and their combinations. The influence of formulation factors on the permeation through intact and microporated human skin was determined. Based on its wide ME region, as well as permeation enhancement effects, oleic acid was used as an oil phase with various surfactants and co-surfactants to further maximize the ME region and skin permeation. The water content in the formulation played an important role in the ME stability, droplet size, and flux of genistein. For example, the ME with 20% water exhibited 4- and 9-fold higher flux as compared to the ME base (no water) and aqueous suspension, respectively. Likewise, this formulation had demonstrated 2- and 4-fold higher skin retention as compared to the ME base (no water) and aqueous suspension, respectively. The skin microporation did not significantly increase the skin permeation of genistein from ME formulations. The ME composition, water content, and to a lesser extent the ME particle size played a role in improving the skin permeation and retention of genistein.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
INTRODUCTION
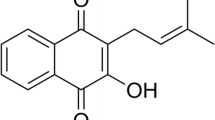
Genistein is a well-known soy isoflavone compound with antioxidant and anti-proliferative properties and is effective in preventing UV-induced skin damage (1,2). It has been demonstrated that genistein can alleviate hormone-dependent physiological symptoms (3), prevent skin aging and inhibit the UVB-induced skin carcinogenesis and photo-damage in animals (4,5,6). The possible mechanisms of the anti-carcinogenic action include scavenging of reactive oxygen species (7,8), blocking of oxidative and photodynamic damage to DNA (9), inhibition of tyrosine protein kinase (10), down-regulation of mitogen-activated protein kinases (MAPK) activation, and suppression of oncoprotein expression in UVB-irradiated cells (11). Various formulations such as gel (12), emulsion (13), amorphous particles (14), and liposome (15) have been attempted to enhance the skin permeation of genistein. However, the effectiveness of genistein was hindered due to its low permeability as well as low solubility in both aqueous and organic media (16). Studies have shown that topical administration of genistein to mouse skin demonstrated acceptable safety levels without genotoxicity or carcinogenicity (17,18). Thus, topical administration of genistein is considered to be a viable alternative for prevention and treatment of pre-malignant skin lesions (19). Also, the topical delivery may be suitable route for genistein to attain systemic bioavailability (20).
Microemulsion improves the topical or transdermal drug delivery of various naturally derived phytochemicals (21,22,23,24). Microemulsion is a spontaneously formed dispersion, which is transparent, optically isotropic, thermodynamically stable system and are very suitable for transdermal application (25,26). Several mechanisms have been proposed to explain the enhanced permeation of microemulsion (ME)-based formulations: the high drug loading capacity, in situ super-saturation providing a higher concentration gradient, the penetration enhancing effect of the ME components, direct transfer of drug from the ME droplet to the stratum corneum, and excellent spreading (low interfacial tension) and contact between the ME and skin surface, which enable enhanced skin permeation of drugs (27,28,29,30). In this study, the ME formulation was optimized to maximize the permeation and retention of genistein in dermatomed human skin. The influence of various ME formulation factors on the permeation through intact and microporated human skin was determined.
MATERIALS AND METHODS
Reagents and Chemicals
Genistein was obtained from LC laboratories (Woburn, MA). Oleic acid was purchased from Spectrum Chemical Corporation (Gardena, CA); Cremophor EL and Cremophor RH40 were provided by BASF (Ludwigshafen, Germany). Ethanol USP and polysorbate 80 NF were purchased from Letco Medical (Decatur, AL). Labrafac WL 1349 (caprylic/capric triglycerides) and Transcutol P (diethylene glycol monoethyl ether) were provided by Gaffeose (Cedex, France). Trifluoroacetic acid and acetonitrile were purchased from EMD Chemical Inc. (Gibbstown, NJ). All other reagents were purchased from VWR International (West Chester, PA).
HPLC Analysis of Genistein
High-performance liquid chromatography (HPLC) system equipped with PDA-UV detector (Alliance 2695 Separation module and 2998 PDA detector, Waters Corporation, Milford, MA) was used for genistein sample analysis. The system was interfaced with Empower 3 software. The chromatographic separation was carried out on a reversed phase Phenomenex, Luna® C18 Column (5 μm, 250 × 4.6 mm). The HPLC method for genistein in the ME formulation was developed and validated. A stability indicating HPLC method for genistein extracted from the emulsion was optimized by controlling the parameters such as extraction solvent, mobile phase composition, flow rate, injection volume, and run time, and the method was validated as detailed in the Supplemental section. The optimized method has the mobile phase composition of 35%:65% acetonitrile and water (both containing 0.1% trifluoroacetic acid), which is set at a flow rate of 1.5 ml/min. The samples were prepared in ethanol water 9:1. The PDA-UV detector was set at 262 nm, and the injection volume was 25 μl.
Solubility Studies
Saturation solubility of genistein in various oils (oleic acid and medium chain triglycerides), surfactants (polysorbate 80, Cremophor-EL and Cremophor-RH40), and co-surfactants (ethanol and Transcutol P) was determined. An excess amount of genistein was added to each liquid (5 ml) in glass vials with polytetrafluoroethylene (PTFE) lined screw caps (sealed with Parafilm®), and then the resulting mixture was shaken reciprocally at 37°C for 72 h and further equilibrated for 24 h. The samples were then centrifuged for 10 min at 12,000 rpm (31). The supernatant was centrifuged at 12,000×g, filtered through Nylon membrane filter (0.45 μm), and the filtrate was diluted appropriately with the HPLC solvent and analyzed as described under HPLC section.
Construction of Pseudo-ternary Phase Diagrams
The ME stability is dependent on its formulation components which can be evaluated by the construction of a pseudo-ternary phase diagram to understand the phase behavior and miscibility of various ME components. For each phase diagram, a specific surfactant to co-surfactant ratio (S/CoS), the mixture of oil, surfactant, and co-surfactant were prepared at 0.5:9.5, 1:9, 1.5:8.5, 2:8, 2.5:7.5, 3:7, 4:6, 5:5, 6:4, 7:3, 7.5:2.5, 8:2, 8.5:1.5, 9:1, and 9.5:0.5 weight ratios respectively (32). Water was added dropwise to each mixture with continuous stirring at 37°C until the mixture became cloudy at a certain point and at that point quantity of water to induce the cloudiness was determined. The area under curve (AUC) of the ME region in the phase diagram was determined for the following formulation factors: types of oil phase, surfactant (S), co-surfactant (Co-S), and different S/CoS ratios. The S/CoS value varied as 5:11, 1:1, and 11:5. Based on the results, appropriate concentrations of oil, surfactant, and co-surfactant were selected and used in the preparation of MEs containing genistein.
Preparation of Genistein ME
Genistein loaded MEs (Table I) were prepared by adding appropriate amount of genistein in the mixture of oil, surfactant, and co-surfactant; then, appropriate amount of water was added with stirring at 37°C. The systems were equilibrated with gentle magnetic stirring for 1 h. The concentration of genistein in MEs was 2% (w/w). The particle size of genistein added to the microemulsions was the resultant MEs were equilibrated for 24 h at room temperature before further studies.
Characterization of ME
The MEs were examined for homogeneity, phase separation, and optical clarity. The droplet size distribution and polydispersity index were determined by dynamic light scattering method using Nicomp 380 ZLS Particle Size Analyzer (Particle Sizing Systems, Santa Barbara, CA). The mean particle size and polydispersity index of the formulations after appropriate dilutions were determined. The pH of MEs was measured using Accumet Excel XL15 pH Meter (Fisher Scientific, Suwannee GA). The viscosity of MEs was measured by Brookfield DV-II PCP pro viscometer using spindle 40Z, and the viscosity in cps was recorded.
In Vitro Permeation Studies
Dermatomed human skin (thickness 0.50 mm) was obtained from a skin bank (Allosource, Cincinnati, Ohio). The protocol for collecting the dermatomed human skin for this study was approved by the skin bank. The skin was collected from a single donor within 8 h of death and frozen at − 70°C until use. The skin was preserved in 50% glycerol in normal saline. Prior to skin permeation experiments, the frozen skin was thawed at ambient temperature for about 20 min. The skin was washed and thoroughly rinsed with phosphate buffered saline pH 7.4 (PBS) to remove any traces of glycerol. The skin was examined microscopically for the absence of any visible damage. For some permeation experiments, skin microporation was induced by 20 passes of solid metallic MN arrays of a Dermaroller™ (Dermaoller Deutschland, Wolfenbuttel, Germany) according to our previous procedure (33).
The skin was mounted between the donor and receptor halves of the vertical Franz diffusion cell apparatus (PermeGear, Bethlehem, PA). The surface area of the skin exposed to the formulation was 0.64 cm2. Receptor cell was filled with 5 ml of 0.01 M phosphate buffered saline pH 7.4 (PBS) and ethanol with the volume ratio of 8 to 2. The receptor cell was stirred with a magnetic bead at 600 rpm. A water circulation jacket (37°C) surrounded the receptor cell to maintain the receptor cell and the under surface of the skin temperature at a physiologic level. The skin was mounted on the cells approximately 30 min before application of the formulations. Each formulation (0.5 ml) was applied over the surface of the epidermis and the donor cell was occluded with Parafilm® to prevent evaporation of water from the formulations (12). Samples (1 ml) were taken from the receptor cell to measure the amount of drug transported across the skin at 1, 2, 4, 6, 8, 12, and 24 h and replenished with the fresh buffer solution, and a correction factor was applied to account for drug removed due to sampling.
Skin Retention
At the end of the skin permeation experiment, the residual drug formulation on the surface of the skin was removed by wiping of the emulsion with absorbable cotton tip (Q-tip). The skin surface was further cleaned using cotton tips (Q-tips) by swabbing and dabbing the surface for six alternate times using 200 μl of a solution of ethanol and water (1:1) at each time. This procedure was determined to be optimum to remove all the drug adhering to the skin surface and not to remove drug from the skin layers. The active diffusion area of the skin was then collected using a 9-mm-diameter biopsy punch for determining the drug content in the skin. The weights of the skin discs were recorded, then minced into small pieces, placed in glass vials and 1 ml of a solution of ethanol and water (1:1) was added, sonicated for 15 min, and placed in refrigerator overnight. The samples were then taken out of refrigerator, let it warm to room temperature, and sonicated for 15 min. The supernatant was filtered using 0.22-μm syringe filters into HPLC vials for the assay (12).
Statistical Analysis
The cumulative amount of genistein permeated across the skin was plotted as a function of time. The slope was calculated from the linear portion of the permeation plot which is presented as steady-state flux (μg/cm2/h). The amount of drug retained in the skin was calculated and normalized to micrograms of genistein per gram of the skin. Data were subjected to one-way analysis of variance (ANOVA) followed by Tukey’s test to determine the level of significance among the flux or skin retention data of various formulations (GraphPad Prism Version 3.0). The data were considered significant at P < 0.05.
RESULTS
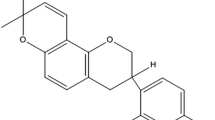
Table II presents the solubility data of genistein in different components of ME formulation. The solubility of genistein in Labrafac WL 1349 and oleic acid was low. Among surfactants, the solubility of genistein was highest in polysorbate 80 (42.91 mg/g), followed by Cremophor EL (19.44 mg/g) and Cremophor RH40 (8.02 mg/g). Among co-surfactants, the solubility was higher in ethanol (18.99 mg/g) than in Transcutol P (5.3 mg/g). All these solvents were used in the formulation of MEs. The pseudo-ternary phase diagrams with the surfactant (S) co-surfactant (Co-S) combinations (S/CoS) are illustrated in Figs. 1 and 2. The ME region in the phase diagram is defined based on the existence of transparent emulsion in the presence of a definite amount of water. Figure 1 shows that the formulation with oleic acid has 2.5-fold higher ME region as compared to Labrafac WL 1349 (38.1% versus 14.4%). The surfactant plays an important role in decreasing the interfacial tension between oil and water, leading to the formation of ME (34). There is no significant difference in ME formation region for different surfactants. The ME regions were 36.7%, 36.6%, and 35.4% for polysorbate 80, Cremophor RH40, and Cremophor EL, respectively, as shown in Fig. 2a–c. Incorporation of co-surfactant further could reduce the interfacial tension between the oil and water in the ME (35). The ternary phase diagrams constructed from ethanol and Transcutol P based ME systems are shown in Fig. 2c, d. There is no significant difference in ME formation region for ethanol and Transcutol P (35.4% versus 34.6%). The area of ME isotropic region changed slightly in size with increased S/CoS value (Km). In system using Cremophor EL/ethanol (S/CoS), the area of ME was the largest when Km was 5 to 11, then followed by 1 to 1 and 11 to 5 (Fig. 2c, e, f).
The pseudo-ternary phase diagram of oleic acid, ethanol, and water system with different surfactants: polysorbate 80 (a), Cremophor RH40 (b), and Cremophor EL (c); different co-surfactants: ethanol (c) and Transcutol P (d); different Km values: 1:1 (c), 11:5 (e), and 5:11 (f). The ME area more or less the same for various surfactants and co-surfactants studied demonstrating high physical stability the ME system made with oleic acid
As water plays an important role in both ME formulation super saturation and associated skin permeation (36), the ME formulation as per Fig. 2f was prepared to contain different amounts of water and the particle size and viscosity were determined. The MEs were generally clear, homogenous systems with no phase separation. The particle size of the formulations usually remained below 100 nm for various MEs when the water content was kept below 20%, within the ME region of the phase diagram. A typical composition was derived from Fig. 2f [oleic acid 20%, Cremophor EL/ethanol (5:11) 80%] based on its large ME region. This composition remained clear as surfactant mixture was substituted by water up to 20%. However, the particle size increased dramatically to 4 μm with 30% water substitution, and it is increased up to 7 μm with 40% water, suggesting the coalescence of droplets leading to loss of ME phase in the formulations with 30% and 40% water content. The pH of the formulation remained constant in the range of 4.5 to 5.0 for various formulations studied. The viscosity of the formulation with no water was 10 cps and this value did not appreciably increase due to presence of water up to 20%. The value showed steep increase to ~ 20 cps with the formulation containing 30% water and then to 27 cps with the one containing 40% water.
Figure 3 and Table III show the influence of the type of surfactant and co-surfactant on the skin permeation of genistein ME. It appears that formulations with Cremophor EL and Cremophor RH40 have similar skin permeation rate, while the one with polysorbate 80 has slightly lower skin permeation. Ethanol as a co-surfactant demonstrated 9-fold higher skin permeation rate (flux) as compared to Transcutol P (P < 0.001). Similarly, ethanol showed 2.5-fold higher retention versus Transcutol P (P < 0.001). The effect of the ratio of S/CoS (Km) on the permeation and skin retention of genistein is shown in Fig. 4 and Table III. The value of S/CoS significantly (P < 0.001) affected the flux and skin retention of genistein. As the ratio altered from 11:5 to 5:11, the flux and skin retention of genistein were increased up to 3- and 6-fold, respectively. The genistein permeations across both intact human skin and microneedle-treated skin under different amounts of water and two controls, aqueous base and emulsion base, are presented (Figs. 5 and 6; Table III). Genistein permeation with changed water content exhibited parabolic profile in both intact skin and microneedle-treated skin. Increasing the amount of water led to improved skin permeation as well as skin retention of genistein. The formulation with 20% water demonstrated 4-fold higher flux as compared to the ME with no water (P < 0.001). Meanwhile, the flux decreased with 40% water content in intact skin but remained at the same level as of 30% water by the microporated skin. Overall, it is interesting to note that genistein retention on both intact skin and microneedle-treated skin demonstrated similar trend as in the permeation studies, with no appreciable increase in the flux due to microneedles.
DISCUSSION
The solubility of genistein in various topical ingredients was determined to identify appropriate components for ME preparation. From the solubility data (Table II), it is evident that the genistein has high solubility in surfactants and co-surfactants compared to the oil phase (oleic acid, Labrafac WL 1349). It is therefore possible for genistein to accumulate at the droplet interfaces at higher amounts, rather than staying in the oil or continuous phase. This high drug concentration would result in a higher concentration gradient, which might account for increased skin permeation (35). Oleic acid was chosen as the oil phase for the ME formulation for two reasons. First, oleic acid is a powerful permeation enhancer for topical delivery (37), second, the lower drug solubility in the oil phase means that lesser is the affinity of genistein to the oil phase and higher would be the thermodynamic activity of the ME formulation leading to better skin permeation (38). The construction of pseudo-ternary phase diagrams with water titration method makes it easy to know the concentration range of components that provide ME formulation. The main factor determining the range of formation of ME zone is the physicochemical properties of components in the formulation. The penetration and association of oil molecules with interfacial surfactant film are important for providing a stable ME (39). As the oleic acid has better miscibility with other components of ME than Labrafac WL 1349, it favors the formation of oil in water type of ME. The surfactant plays an important role in decreasing interfacial tension between oil and water, leading to the formation of ME (34). There is no significant difference in ME formation region using three different surfactants. It can be due to the similar hydrophilic-lipophilic balance (HLB) values for these surfactants, as HLB is the critical parameter in characterizing the ability of surfactants to decrease surface tension. However, usual surfactants are unable to lower the interfacial tension between oil and water to such ultra-low values; co-surfactants are frequently necessary in the ME system. Incorporation of co-surfactant can further reduce the interfacial tension between the oil and water in the ME, adjust the flexibility of the interfacial membrane, and reduce the amount of surfactant needed (35). The area of ME isotropic region increased with increased S/CoS value (Km). In system using oleic acid, Cremophor EL, and ethanol (Fig. 3c, e, f), the area of ME was the largest when Km was 5 to 11 and then followed by 1 to 1 and 11 to 5. This suggested that increasing the amount of ethanol facilitated the formation of ME. The ethanol has good miscibility with surfactant and oil phase (40).
As water plays an important role in both ME formulation super-saturation and associated skin permeation (36), the ME formulation as per Fig. 2f was prepared to contain different amounts of water. This composition remains as clear ME in the presence of water up to 20%. At higher percentage of water, the particle size and viscosity were increased suggesting the coalescence of droplets leading to loss of ME phase in the formulations. The higher amount of water substitution led to decreased percentage of surfactant and co-surfactant and then caused enhanced surface tension and a coarse emulsion formation.
Cremophor EL and Cremophor RH40 based MEs have a similar skin permeation rate, while polysorbate 80 has slightly lower skin permeation. The similar skin permeation rates of genistein MEs by different surfactants may be due to the similar hydrophilic lipophilic balance (HLB) values of the surfactants used in this study. Generally, nonionic surfactants have low toxicity (41,42); this group of surfactants has enhancement effect in human skin permeation which could be attributed to disruption of lipid bilayers in SC. High permeation rate of microemulsions might attribute to the high concentration of surfactants in microemulsions as permeation enhancers (43). Then, the system with ethanol as a co-surfactant demonstrated much higher skin permeation and retention, respectively, as compared to Transcutol P. Ethanol has a superior ability in facilitating skin permeation of drugs, as known from its use in many commercial topical products, and has excellent miscibility with other components of ME. It can alter the solubility properties with a consequent improvement of drug partitioning into the membrane (44). Additionally, it is also feasible the rapid permeation of ethanol or evaporative loss of this volatile solvent, from the ME, which modifies the thermodynamic activity of the drug within the formulation (45). The value of S/CoS mixture in ME affected the skin permeation rate of genistein significantly (Fig. 4). As the ratio altered from 11:5 to 5:11, the skin permeation rate of genistein increased by 3-fold. This further confirms that ethanol contributed to improved permeation of genistein across intact skin. Water is a critical factor that affects the transdermal delivery of drugs (38). Genistein permeation with changed water content exhibited parabolic profile in both intact skin and microneedle-treated skin. Increasing the amount of water led to improved skin permeation and retention of genistein up to 30% water. This is because that genistein must be dissolved in the aqueous phase and provide a concentration gradient for better diffusion into the skin lipid bilayer for permeation. These results suggest that the droplet size of the microemulsion formulation appears to have a lesser role in the skin permeation of genistein than the presence of higher soluble fraction (providing higher concentration gradient) of the drug leading to higher skin permeation. The genistein retention on both intact skin and microneedle-treated skin demonstrated similar trend as in the permeation studies. These results can be explained by two possible mechanisms: One is that the decreased soluble fraction of drug in the formulation as the percentage of water increased. The other one is that the thermodynamic activity decreased with increased water content, which then impaired the skin penetration. The outermost layer of skin, the stratum corneum (SC), presents a significant barrier to the transdermal delivery of drugs (46,47). Microneedles were used to overcome the stratum corneum barrier. Surprisingly, microneedle-treated skin did not significantly increase the permeation and retention of genistein from any of the formulation compositions (P > 0.05) compared to intact skin. Microporation technique works better for the drugs with higher water solubility as SC is the rate limiting barrier for these drugs (48). The extreme insolubility of genistein might be the reason for the lack of microneedle effects on the skin permeation.
CONCLUSION
Various factors affecting the ME formulation, skin permeation, and deposition of genistein were studied. The ME composition, water content, and to a lesser extent the ME particle size played a role in improving the skin permeation and retention of genistein. The supersaturation induced by the presence of optimum amount of water appears to have major role in the skin permeation and retention of genistein rather than the droplet size of the ME.
References
Piovesan AC, Soares Júnior JM, Mosquette R, Simões MD, Simões RD, Baracat EC. Morphological and molecular effects of isoflavone and estrogens on the rat mammary gland. Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(4):204–9.
Brand RM, Jendrzejewski JL. Topical treatment with (−)-epigallocatechin-3-gallate and genistein after a single UV exposure can reduce skin damage. J Dermatol Sci. 2008;50(1):69–72. https://doi.org/10.1016/j.jdermsci.2007.11.008.
Vera JC, Reyes AM, Velasquez F, Rivas CI, Zhang RH, Strobel P, et al. Direct inhibition of the hexose transporter GLUT1 by tyrosine kinase inhibitors. Biochemistry. 2001;40(3):777–90. https://doi.org/10.1021/bi001660j.
Wei H, Zhang X, Wang Y, Lebwohl M. Inhibition of ultraviolet light-induced oxidative events in the skin and internal organs of hairless mice by isoflavone genistein. Cancer Lett. 2002;185(1):21–9. https://doi.org/10.1016/s0304-3835(02)00240-9.
Widyarini S, Husband AJ, Reeve VE. Protective effect of the isoflavonoid equol against hairless mouse skin carcinogenesis induced by UV radiation alone or with a chemical cocarcinogen. Photochem Photobiol. 2005;81(1):32–7. https://doi.org/10.1562/2004-06-02-ra-183.1.
Shyong EQ, Lu Y, Lazinsky A, Saladi RN, Phelps RG, Austin LM, et al. Effects of the isoflavone 4′, 5, 7-trihydroxyisoflavone (genistein) on psoralen plus ultraviolet A radiation (PUVA)-induced photodamage. Carcinogenesis. 2002;23(2):317–21. https://doi.org/10.1093/carcin/23.2.317.
Peak MJ, Peak JG. Solar-ultraviolet-induced damage to DNA. Photo-Dermatology. 1989;6(1):1–5.
Beehler BC, Przybyszewski J, Box HB, Kulesz-Martin MF. Formation of 8-hydroxydeoxyguanosine within DNA of mouse keratinocytes exposed in culture to UVB and H2O2. Carcinogenesis. 1992;13(11):2003–7. https://doi.org/10.1093/carcin/13.11.2003.
Kim SY, Na YJ, Kim D, Kim Y, Kim HM, Hwang SH, et al. Development of estimation methods of skin oxidation and evaluation of anti-oxidative effects of genistein in topical formulations. The Korean Journal of Physiology & Pharmacology. 2012;16(3):205–9. https://doi.org/10.4196/kjpp.2012.16.3.205.
Foti P, Erba D, Riso P, Spadafranca A, Criscuoli F, Testolin G. Comparison between daidzein and genistein antioxidant activity in primary and cancer lymphocytes. Arch Biochem Biophys. 2005;433(2):421–7. https://doi.org/10.1016/j.abb.2004.10.008.
Pavese JM, Farmer RL, Bergan RC. Inhibition of cancer cell invasion and metastasis by genistein. Cancer Metastasis Rev. 2010;29(3):465–82. https://doi.org/10.1007/s10555-010-9238-z.
Chadha G, Sathigari S, Parsons DL, Jayachandra BR. In vitro percutaneous absorption of genistein from topical gels through human skin. Drug Dev Ind Pharm. 2011;37(5):498–505. https://doi.org/10.3109/03639045.2010.525238.
Silva AP, Nunes BR, De Oliveira MC, Koester LS, Mayorga P, Bassani VL, et al. Development of topical nanoemulsions containing the isoflavone genistein. Die Pharmazie-An International Journal of Pharmaceutical Sciences. 2009;64(1):32–5. https://doi.org/10.1691/ph.2009.8150.
Del Gaudio P, Russo P, Dorado RR, Sansone F, Mencherini T, Gasparri F, et al. Submicrometric hypromellose acetate succinate particles as carrier for soy isoflavones extract with improved skin penetration performance. Carbohydr Polym. 2017;165:22–9. https://doi.org/10.1016/j.carbpol.2017.02.025.
Kang KH, Kang MJ, Lee J, Choi YW. Influence of liposome type and skin model on skin permeation and accumulation properties of genistein. J Dispers Sci Technol. 2010;31(8):1061–6. https://doi.org/10.1080/01932690903224813.
Kitagawa S, Inoue K, Teraoka R, Morita SY. Enhanced skin delivery of genistein and other two isoflavones by microemulsion and prevention against UV irradiation-induced erythema formation. Chem Pharm Bull. 2010;58(3):398–401. https://doi.org/10.1248/cpb.58.398.
Huang ZR, Hung CF, Lin YK, Fang JY. In vitro and in vivo evaluation of topical delivery and potential dermal use of soy isoflavones genistein and daidzein. Int J Pharm. 2008;364(1):36–44. https://doi.org/10.1016/j.ijpharm.2008.08.002.
Moore JO, Wang Y, Stebbins WG, Gao D, Zhou X, Phelps R, et al. Photoprotective effect of isoflavone genistein on ultraviolet B-induced pyrimidine dimer formation and PCNA expression in human reconstituted skin and its implications in dermatology and prevention of cutaneous carcinogenesis. Carcinogenesis. 2006;27(8):1627–35. https://doi.org/10.1093/carcin/bgi367.
Andrade LM, de Fátima RC, Maione-Silva L, Anjos JL, Alonso A, Serpa RC, et al. Impact of lipid dynamic behavior on physical stability, in vitro release and skin permeation of genistein-loaded lipid nanoparticles. Eur J Pharm Biopharm. 2014;88(1):40–7. https://doi.org/10.1016/j.ejpb.2014.04.015.
Busby MG, Jeffcoat AR, Bloedon LT, Koch MA, Black T, Dix KJ, et al. Clinical characteristics and pharmacokinetics of purified soy isoflavones: single-dose administration to healthy men. Am J Clin Nutr. 2002;75(1):126–36. https://doi.org/10.1093/ajcn/75.1.126.
Rangsimawong W, Wattanasri P, Tonglairoum P, Akkaramongkolporn P, Rojanarata T, Ngawhirunpat T, et al. Development of microemulsions and microemulgels for enhancing transdermal delivery of Kaempferia parviflora extract. AAPS PharmSciTech. 2018;23:2058–67. https://doi.org/10.1208/s12249-018-1003-6.
Tabosa MA, de Andrade AR, Lira AA, Sarmento VH, de Santana DP, Leal LB. Microemulsion formulations for the transdermal delivery of lapachol. AAPS PharmSciTech. 2018;19(4):1837–46. https://doi.org/10.1208/s12249-018-0995-2.
Lv X, Liu T, Ma H, Tian Y, Li L, Li Z, et al. Preparation of essential oil-based microemulsions for improving the solubility, pH stability, photostability, and skin permeation of quercetin. AAPS PharmSciTech. 2017;18(8):3097–104. https://doi.org/10.1208/s12249-017-0798-x.
Panapisal V, Charoensri S, Tantituvanont A. Formulation of microemulsion systems for dermal delivery of silymarin. AAPS PharmSciTech. 2012;13(2):389–99. https://doi.org/10.1208/s12249-012-9762-y.
Hashem FM, Shaker DS, Ghorab MK, Nasr M, Ismail A. Formulation, characterization, and clinical evaluation of microemulsion containing clotrimazole for topical delivery. AAPS PharmSciTech. 2011;12(3):879–86. https://doi.org/10.1208/s12249-011-9653-7.
Kantarcı G, Özgüney I, Karasulu HY, Arzık S, Güneri T. Comparison of different water/oil microemulsions containing diclofenac sodium: preparation, characterization, release rate, and skin irritation studies. AAPS PharmSciTech. 2007;8(4):75–81. https://doi.org/10.1208/pt0804091.
Salerno C, Carlucci AM, Bregni C. Study of in vitro drug release and percutaneous absorption of fluconazole from topical dosage forms. AAPS PharmSciTech. 2010;11(2):986–93. https://doi.org/10.1208/s12249-010-9457-1.
Kogan A, Garti N. Microemulsions as transdermal drug delivery vehicles. Adv Colloid Interf Sci. 2006;123:369–85. https://doi.org/10.1016/j.cis.2006.05.014.
Kreilgaard M. Influence of microemulsions on cutaneous drug delivery. Adv Drug Deliv Rev. 2002;54:S77–98. https://doi.org/10.1016/s0169-409x(02)00116-3.
Dreher F, Walde P, Walther P, Wehrli E. Interaction of a lecithin microemulsion gel with human stratum corneum and its effect on transdermal transport. J Control Release. 1997;45(2):131–40. https://doi.org/10.1016/s0168-3659(96)01559-3.
Qi X, Qin J, Ma N, Chou X, Wu Z. Solid self-microemulsifying dispersible tablets of celastrol: formulation development, characterization and bioavailability evaluation. Int J Pharm. 2014;472(1–2):40–7. https://doi.org/10.1016/j.ijpharm.2014.06.019.
Patel MR, Patel RB, Parikh JR, Solanki AB, Patel BG. Effect of formulation components on the in vitro permeation of microemulsion drug delivery system of fluconazole. AAPS PharmSciTech. 2009;10(3):917–23. https://doi.org/10.1208/s12249-009-9286-2.
Kolli CS, Xiao J, Parsons DL, Babu RJ. Microneedle assisted iontophoretic transdermal delivery of prochlorperazine edisylate. Drug Dev Ind Pharm. 2012;38(5):571–6. https://doi.org/10.3109/03639045.2011.617753.
Moghadam SH, Saliaj E, Wettig SD, Dong C, Ivanova MV, Huzil JT, et al. Effect of chemical permeation enhancers on stratum corneum barrier lipid organizational structure and interferon alpha permeability. Mol Pharm. 2013;10(6):2248–60. https://doi.org/10.1021/mp300441c.
Chen L, Tan F, Wang J, Liu F. Microemulsion: a novel transdermal delivery system to facilitate skin penetration of indomethacin. Die Pharmazie. 2012;67(4):319–23. https://doi.org/10.1692/ph.2012.1150.
Williams AC, Barry BW. Penetration enhancers. Adv Drug Deliv Rev. 2012;64:128–37. https://doi.org/10.1016/j.addr.2012.09.032.
Francoeur ML, Golden GM, Potts RO. Oleic acid: its effects on stratum corneum in relation to (trans) dermal drug delivery. Pharm Res. 1990;7(6):621–7.
Ellaithy HM, El-Shaboury KM. The development of Cutina lipogels and gel microemulsion for topical administration of fluconazole. AAPS PharmSciTech. 2002;3(4):77–85. https://doi.org/10.1208/pt030435.
Malcolmson C, Satra C, Kantaria S, Sidhu A, Lawrence MJ. Effect of oil on the level of solubilization of testosterone propionate into nonionic oil-in-water microemulsions. J Pharm Sci. 1998;87(1):109–16. https://doi.org/10.1021/js9700863.
Berner B, Mazzenga GC, Otte JH, Steffens RJ, Juang RH, Ebert CD. Ethanol: water mutually enhanced transdermal therapeutic system II: skin permeation of ethanol and nitroglycerin. J Pharm Sci. 1989;78(5):402–7. https://doi.org/10.1002/jps.2600780512.
Sarpotdar PP, Zatz JL. Percutaneous absorption enhancement by nonionic surfactants. Drug Dev Ind Pharm. 1986;12(11–13):1625–47. https://doi.org/10.3109/03639048609042599.
Sarpotdar PP, Zatz JL. Evaluation of penetration enhancement of lidocaine by nonionic surfactants through hairless mouse skin in vitro. J Pharm Sci. 1986;75(2):176–81. https://doi.org/10.1002/jps.2600750216.
Hu L, Hu Q, Yang J. Enhancement of transdermal delivery of ibuprofen using microemulsion vehicle. Iranian journal of basic medical sciences. 2014;17(10):760–6.
Pershing LK, Lambert LD, Knutson K. Mechanism of ethanol-enhanced estradiol permeation across human skin in vivo. Pharm Res. 1990;7(2):170–5.
Megrab NA, Williams AC, Barry BW. Oestradiol permeation across human skin, silastic and snake skin membranes: the effects of ethanol/water co-solvent systems. Int J Pharm. 1995;116(1):101–12. https://doi.org/10.1016/0378-5173(94)00321-u.
Notman R, Anwar J. Breaching the skin barrier—insights from molecular simulation of model membranes. Adv Drug Deliv Rev. 2013;65(2):237–50. https://doi.org/10.1016/j.addr.2012.02.011.
Lane ME. Skin penetration enhancers. Int J Pharm. 2013;447(1–2):12–21. https://doi.org/10.1016/j.ijpharm.2013.02.040.
Pawar KR, Smith F, Kolli CS, Babu RJ. Effect of lipophilicity on microneedle-mediated iontophoretic transdermal delivery across human skin in vitro. J Pharm Sci. 2013;102(10):3784–91. https://doi.org/10.1002/jps.23694.
Acknowledgements
This study received financial support from Auburn University Research Initiative in Cancer (AURIC) and the intramural grant program (IGP) from the Auburn University, AL.
Author information
Authors and Affiliations
Corresponding author
Additional information
Guest Editor: S. Narasimha Murthy
Electronic Supplementary Material
ESM 1
(DOCX 71 kb)
Rights and permissions
About this article
Cite this article
Chen, L., Annaji, M., Kurapati, S. et al. Microemulsion and Microporation Effects on the Genistein Permeation Across Dermatomed Human Skin. AAPS PharmSciTech 19, 3481–3489 (2018). https://doi.org/10.1208/s12249-018-1150-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1208/s12249-018-1150-9