Abstract
Domperidone (DOP) is extensively applied orally in the management of nausea and vomiting. Upon oral administration, its bioavailability is very poor due to its poor solubility in alkaline media. Therefore, the aim of this work was to investigate DOP-loaded solid lipid nanoparticles (DOP-SLNs) in order to sustain its release pattern and to enhance oral bioavailability. DOP-SLNs were prepared using four different lipids. Prepared DOP-SLNs were characterized for “polydispersity index (PDI), particle size, zeta potential, % entrapment efficiency (% EE), and drug release behavior.” Differential scanning calorimetry (DSC) study was carried out to illustrate the physical form of DOP and excipients. The morphology of DOP-SLNs was confirmed by scanning electron microscopy (SEM). Pharmacokinetic study on optimized DOP-SLN in comparison to tablet was performed in rats. The “particle size, PDI, zeta potential, and % EE” of optimized formulation (F5) were recorded as 201.4 nm, 0.071, − 6.2 mV, and 66.3%, respectively. DSC thermograms suggested amorphous state of DOP in various SLNs. Surface morphology of SLNs using SEM suggested spherical shape of the nanoparticles within nanometer size range. In vitro release studies confirmed that all SLN formulations possessed a sustained release over a period of 12 h (51.3% from optimized formulation) in comparison with immediate release from conventional tablets (100% after 90 min). Pharmacokinetic study showed significant enhancement in oral absorption of DOP from optimized SLN in comparison with DOP tablet. The enhancement in relative bioavailability of DOP from optimized SLN was 2.62-fold in comparison with DOP tablet.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
INTRODUCTION
The physicochemical limitations of drugs including “poor solubility, low permeability, short half-life, high molecular weight, side effects, and systemic toxicity” can be overcome by developing nanoparticulate-based carriers such as “liposomes, dendrimers, polymeric nanoparticles, and solid lipid nanoparticles (SLNs)” (1).
SLNs are colloidal lipid-based drug carriers which have been proposed as a promising alternative to colloidal drug delivery system, polymeric nanoparticles, and liposomes (1,2). These systems offer several advantages such as good tolerability, lower cytotoxicity, and higher bioavailability by oral administration and also increase the drug stability in comparison with conventional drug carriers (2). The use of solid lipids as a substitute of liquid lipids in SLNs is helpful in achieving controlled rate drug release behavior of hydrophobic drugs. Additionally, they are also helpful in avoiding biotoxicity of organic solvents (3,4).
Domperidone (DOP), an antidopaminergic drug, is used generally to suppress nausea and vomiting. It is also useful in the treatment of other diseases (4,5,6,7). The solubility of DOP in acidic media is good but its solubility in alkaline media has been reported as very poor (8). Due to poor solubility of DOP in alkaline media, it shows very low bioavailability (13–17%) after oral administration (9). Accordingly, DOP requires longer treatment and repetitive dosing which make this drug an interesting candidate for development of SLN. In literature, solid dosage forms of DOP including fast dissolving tablets (10,11), floating matrix tablets (12), orodispersible tablets (13), microspheres (14), and hot-melt extruded films (15) have been investigated extensively. Transdermal patches of DOP have also been investigated in literature (16). Self-microemulsifying drug delivery system of DOP has also been investigated for its bioavailability and solubility enhancement (17). Nanoparticle film, nanostructured lipid carrier, and SLN of DOP have also been studied in literature (18,19). However, SLNs of DOP were not investigated for its in vivo characterization. Thus, the objectives of this work were to develop and investigate DOP-loaded SLNs (DOP-SLNs) for a sustained release, to study the effect of composition of lipid materials on particle size and in vitro drug behavior, and to enhance its bioavailability.
MATERIALS AND METHODS
Materials
Softisan® 154, Imwitor® 900 K, and Dynasan® 118 were obtained from “Sasol Germany GmbH (Witten, Germany).” DOP and sodium deoxycholate were obtained from “Sigma Aldrich (St. Louis, MO, USA).” Stearic acid, glucose, and Tween 80 were obtained from “BDH Chemicals (Poole, England, UK).” Dialysis membrane (pore size = 2.4 nm and MWCO = 12,000–14,000 Da) was obtained from “Sigma Aldrich (St. Louis, MO, USA).” All other chemicals used were of analytical/pharmaceutical grades.
Preparation of DOP-SLNs
DOP-SLNs were prepared using hot homogenization followed by ultrasonication method (19,20). The specified amounts (listed in Table I) of different solid lipids (e.g., Imwitor® 900 K, stearic acid, Softisan® 154, and Dynasan®) were heated at the temperature which was 10°C above of the melting points of particular solid lipid. Approximately 50 mg of DOP was dispersed in the lipid phase SLNs (melted lipid). The aqueous solution of surfactant (containing 1% of Tween 80 and 0.5% of sodium deoxycholate) was also heated at the same temperature and referred as aqueous phase. The aqueous phase and lipid phase were then mixed properly using Homogenizer at 20000 rpm for about 5.0 min. The obtained dispersion was sonicated with the help of a “Probe Sonicator” for about 3 min at 40% voltage efficiency. The obtained lipid emulsion was then dispersed in chilled 5% glucose solution with vigorous stirring for about 3 min with the help of a magnetic stirrer. Glucose solution was used a cryoprotector. The obtained SLNs dispersions were stabilized by lyophilization for 72 h with the help of a “Freeze-Drying Apparatus (Alpha 1-4 LD-2, Martin Christ, Osterode, Germany)” at standard conditions (20).
Particle Size, Zeta Potential, and Polydispersity Index of SLNs
The mean values of particle size, zeta potential, and polydispersity index (PDI) of the prepared SLNs were measured using “Photon Correlation Spectroscopy (Brookhaven Instruments Corporation, Holtsville, NY, USA).” The SLNs were diluted with distilled water (1:100) and the measurements were done at 25°C. For the measurement of particle size and PDI, samples were taken in disposable plastic cuvettes. However, for zeta potential measurement, the samples were taken in glass cuvettes. The scattering angle for measurement was 90°. All experiments were performed in triplicate.
Entrapment Efficiency (%)
The samples were centrifuged at 4°C and 50,000 RPM for about 30 min with the help of an “Ultracentrifuge (Optima MAX-E ultracentrifuge, Beckman Coulter, Inc., Nyon, Switzerland).” The free quantity of DOP in the supernatant was analyzed with the help of high-performance liquid chromatography (HPLC). The percent drug entrapment efficiency (% EE) of the prepared SLNs was calculated using Eq. (1):
Where DOPt and DOPf are the amounts of total and free DOP, respectively.
Differential Scanning Calorimetry
“DSC Shimadzu DSC-60 equipped with an intercooler (Shimadzu Corporation, Koyoto, Japan)” was used for obtaining the thermograms of pure drug, lipids, blank SLN, and drug-loaded SLNs. The calibration of apparatus was carried out using indium/zinc standard. The specified amounts of each sample were taken into aluminum pan which were hermetically sealed. The samples were heated at the range of 25–200°C at the heating rate of 10°C/min. The gas used was nitrogen gas which was purged at a flow rate of 50 ml/min.
Scanning Electron Microscopy
The shape and morphology of the surface of the prepared SLNs was evaluated with the help of a “SEM Microscope (Zeiss EVO LS10; Cambridge, UK).” The samples were fixed on stubs with the help of “Double-Sided Adhesive Carbon Tape (SPI Supplies, West Chester, USA)” and coated using gold in a “Q150R Sputter Coater Unit (Quorum Technologies Ltd., East Sussex, UK)” under vacuum in an argon atmosphere at 20 mA for 120 s.
In Vitro Release Study
Drug release studies were accomplished with the help of dialysis membrane (pore size = 2.4 nm and MWCO = 12,000–14,000 Da). The membrane was treated according to instructions given by the manufacturer before mounting in a Franz diffusion cell. Each of the crushed marketed conventional DOP tablet and pure DOP (10 mg) were suspended in the buffer used (pH 6.8). A volume of 2 ml (containing equivalent amounts of DOP) of the suspended DOP and the prepared SLNs was taken into donor chamber of the cells. The receiver chamber was filled using a phosphate buffer (pH 6.8). The receiver compartment was controlled at the temperature of 37 ± 0.5°C and stirred at 100 rpm. At different intervals of time, 1 ml of the sample was carefully withdrawn from receiver chamber and replaced with drug-free fresh phosphate buffer (pH 6.8). The samples were analyzed by HPLC method.
HPLC Analysis of DOP in In Vitro Samples
The “HPLC system (Waters™ 600 controller, USA)” equipped with “Wavelength Detector (Waters™ 2487 a dual absorbance detector, USA),” “Pump (Waters™ 1252 a binary pump, USA),” and an “Automating Sampling System (Waters™ 717 Plus Autosampler, USA)” was utilized for the analysis of DOP in in vitro samples. The HPLC system was monitored by “Empower (Water)” software. DOP was investigated using mobile phase composed of acetonitrile/water (31:69) adjusted to pH 2.5 using orthophosphoric acid. The mobile phase delivered over a reversed-phase “C18 column (μBondapak™, 4.6 × 150 mm, 10 μm particle size, Waters, USA)” at a flow rate of 1 ml/min. The volume of injection for each DOP sample was set at 20 μl. The samples were detected by UV detector at 284 nm. The whole analysis was performed at room temperature (21).
In Vivo Pharmacokinetic Study
In vivo pharmacokinetic study on optimized formulation F5 was accomplished in comparison with DOP conventional tablet in Wistar male rats. The protocol for this work was accepted by the “Institutional Animal Ethics Committee of Pharmacy College, King Saud University, Riyadh, Saudi Arabia.”
Animals
Adult male Wistar Albino rats (weighing about 200–300 g, aging approximately 3 months) were taken from the “Animal Care Center, College of Pharmacy, King Saud University, Riyadh, Saudi Arabia.” The obtained rats were kept in metabolic cages under controlled conditions of temperature and relative humidity (RH) (25°C, 65% RH) with 12 h light/dark cycles. All the rats were provided free access to “standard rat pellet diet and tap water.” This study was followed the instruction of the “Research Ethics Committee of College of Pharmacy, King Saud University, Riyadh, Saudi Arabia.”
Study Protocol
The animals (six animals in each group) were made unconscious temporarily by exposing to ether vapors. A single dose of 1.64 mg of DOP from optimized SLN F5 and suspension of DOP conventional tablets was administered orally in adult male Wistar Albino rats (22). Required modifications were carried out and animal dose was calculated with the help of human dose using the conversion factor (23). The selected formula was administered after about 8 to 10 h of fasting. At appropriate predetermined intervals of time (0.5, 1, 2, 4, 6, 8, 10, 14, 15, and 24 h), blood samples were taken from the retro-orbital plexus of the rat eye by puncturing the retro-orbital venous plexus with the help of fine capillary tubes. The blood samples were collected in heparinized tubes. The blood samples were centrifuged at 5000×g for 10 min and plasma was collected. Plasma samples were stored at − 20°C until further analysis.
Analysis of DOP Concentration in Rat Plasma by HPLC-UV
The same apparatus and chromatographic conditions as described for analysis of DOP in in vitro samples were also utilized for the quantification of DOP in rat plasma except propranolol was used as internal standard (IS) in this analysis.
Samples were prepared by protein precipitation method using dichloromethane (DCM). Plasma samples (100 μl) were transferred to 1.5 ml centrifuge tubes and 100 μl of DOP solution (5.0 μg/ml in mobile phase) and 100 μl of IS (150 ng/ml in methanol) were added. The samples were vortexed for about 5.0 min and 3.0 ml of DCM was added. The samples were again vortex mixed for 10 min followed by centrifugation at 3000×g for 10 min. After centrifugation, the supernatant was evaporated under dryness in order to obtain residue. The obtain residue was then reconstituted using 100 μl of mobile phase and 20 μl of sample was injected into HPLC system for analysis (24).
Pharmacokinetic Data Analysis
Various pharmacokinetic parameters including “area under the drug-concentration time-curve (AUC), half-life (t1/2) and relative bioavailability” were calculated with the help of non-compartmental analysis. However, the values of “maximum plasma concentration (Cmax) and time to reach Cmax (Tmax)” were obtained directly from the plasma concentration-time curve (25).
Statistical Analysis
In vitro parameters were estimated using one-way ANOVA followed by Dunnett’s test. Unpaired T test was applied for statistical comparison of pharmacokinetic parameters. “Graphpad Instat Software (San Diego, CA, USA)” was used for statistical analysis and P < 0.05 was considered as significant.
RESULTS AND DISCUSSION
Mean Particle Size, PDI, and Zeta Potential
Figure 1 depicts the mean particle size of the prepared SLN formulations. According to this figure, the mean particle size was found as 171.3 ± 8.01, 191.4 ± 5.11, 149.4 ± 0.99, and 201.4 ± 6.12 nm for SLNs prepared using Imwitor 700 K (F2), stearic acid (F3), Softisan 154 (F4), and Dynasan 118 (F5), respectively. It was observed that the SLNs containing Dynasan lipid showed the biggest particle size. However, formulation containing Softisan 154 showed the smallest one. This small particle size of the developed SLNs was possible due to the presence of Tween 80 which is capable of reducing the interfacial tension between lipid matrix and external medium. Tween 80 also stabilizes the SLN formulations as reported in literature (26). The difference in particle size among different SLNs may be not only due to difference in the fatty chain length of the lipids but also to differences in melting points. The melting points have been reported as 75, 70, 61, and 57°C for Dynasan, stearic acid, Imwitor 700 K, and Softisan 154, respectively (27). It has been proposed that the higher melting points of lipids related with higher particle size (28).
The PDI values of different SLNs are presented in Fig. 2. From this figure, it was found that PDI of the prepared SLNs is less than 0.1. This indicates that the preparations have an ideal and a narrow size distribution and are monodispersions (29).
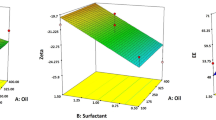
Figure 3 exhibits the mean zeta potential of the prepared SLNs. From this figure, it was observed that the zeta potential values of prepared SLNs were negative and varied between − 4.6 and − 30.4 mV. The negative values of the zeta potential indicated the stability of the prepared SLNs by maintaining electrostatic repulsion between the particles (30). Lipid type had an impact on the zeta potential value of the SLNs. SLNs of Imwitor showed the maximum negative zeta potential value which might be due to the fact that highly negative charges are distributed at the surface of these SLNs. However, the negative value of SLNs of Softisan 154 showed the lowest negative zeta potential value (31).
% EE of SLNs
Figure 4 depicts the results of % EE of the SLN formulations. It was noticed that the % EE of SLNs prepared using stearic acid had higher value (79.4 ± 0.2), while that of SLNs containing Softisan 154 had the lowest value (41.1 ± 0.6). This might be due to the fact that stearic acid is long-chain fatty acid which could create a less ordered solid lipid matrix and leaves enough space to accommodate drug molecules (32). This could also might be due to the solubility of the drug in the melted stearic acid (33).
DSC Study
Differential scanning calorimetry (DSC) thermograms of DOP, lipids, and SLNs are shown in Fig. 5. The thermogram of DOP was characterized by melting endotherm at 253.79°C with a fusion enthalpy (ΔH) value of − 40.19 kj/mol. The melting temperature of DOP obtained in this study was same as reported in literature (10). Therefore, DSC results of DOP were in accordance with literature. This sharp endothermic peak of the DOP suggested the pure crystalline state of this drug. DSC study is shown that the endothermic peak of the DOP was completely disappeared in the thermograms of DOP-loaded SLNs for all lipids used. This observation suggested the complete solubilization of DOP inside the lipid matrix (34). The disappearance of the endothermic peak of the DOP in SLNs could be attributed to the presence of the DOP in the amorphous state in the melted lipids (35).
SEM Study
The scanning electron microscopy (SEM) photograph of the selected formulations (F3 and F5) is shown in Fig. 6. It was noticed that the SLNs were spherical in shape with a smooth surface. The SEM image showed that some of the nanoparticles were adhered together and this might be due to the nature of lipid used. This adhesion could also be due to preparation of the formulations prior to SEM analysis (36).
In Vitro Release Study
The in vitro drug release patterns of conventional DOP tablets, DOP (F1), and DOP-loaded SLNs (F2–F5) are shown in Fig. 7. From this figure, it was found that the percent cumulative amount of DOP released from F1 was smaller than other formulations and this might be attributed to the basic nature of the drug which has limited solubility at higher pH values (37). On the other hand, the percent cumulative amount of DOP released from the conventional DOP tablets was higher than other formulations and 100% was obtained after about 90 min.
Regarding formulations F2–F5, it was observed that the release of DOP was burst release from all formulations at first step which was possible due to the presence of the DOP molecules at the outer surface layer of the particles. The cumulative percent release values were 51.3 ± 2.84%, 11.31 ± 1.96%, 11.52 ± 3.15%, 10.56 ± 3.23%, and 7.42 3.2% for F1, F2, and F3, F4, and F5, respectively. This pattern might be attributed to the length of the triglyceride chains of the lipid. Dynasan 118 in F5 contains long glyceride chain as compared to other lipids in other formulae (Imwitor 900 K in F1, stearic acid in F2, and Softisan 154 in F3). That is to say a delayed drug release for F4 than that for formulations having shorter chains (F1, F2, and F3) (38). Generally, the release of DOP was slow and sustained from all SLN formulations. This might be due to the fact that the drug is strongly bound with the lipids. Many researchers reported this biphasic type of release from SLNs (39,40,41). This biphasic release pattern might be attributed to lack of uniformity in drug distribution in SLNs leads to adsorption of the drug on the outer surface of the formed SLNs (41).
In Vivo Pharmacokinetic Studies of DOP
The most significant cause in terms of product performance is the evaluation of their in vivo bioavailability. SLN formulations were investigated successfully in order to enhance the bioavailability of various poorly soluble drugs in humans and animals (39,40,41).
It is well known that DOP absorbed completely from the gut (42). Thus, when the marketed DOP conventional tablet is administered orally in Wistar rat, it was absorbed rapidly. The Cmax value was obtained as 25.31 μg/ml within 2 h. The drug plasma concentration declined quickly after the first 2 h. However, there was no drug being detected after 10 h of oral administration (42).
Figure 8 exhibits the mean plasma concentration-time curves of DOP upon oral administration of DOP tablet and optimized SLN F5 into rats at a dose of 10 mg/kg body weight. Different pharmacokinetic parameters for DOP from conventional tablets and optimized SLN F5 are presented in Table II.
As revealed in Table II, AUC0–24 values of F5 and conventional DOP tablet were obtained as 205.43 ± 30.61 μg/ml/h and 78.40 ± 70.19 μg/ml/h. This reflected that formulation F5 showed AUC0–24 significantly higher than that of conventional DOP tablet (P < 0.01). Regarding Cmax, the value from F5 (22.97 ± 7.22 μg/ml) was significantly low than that from conventional DOP tablet (25.31 ± 10.67 μg/ml) (P < 0.01). Based on a comparison of the Tmax values, the Cmax reached time in F5 group (10 ± 0.19 h) was significantly longer in comparison with conventional DOP tablet group (2 ± 0.3 h) (P < 0.01). Hence, sustained drug plasma levels were obtained with formulation F5 suggesting rate-controlled drug release behavior of DOP from F5 in comparison with conventional DOP tablet. AUC0–24 of DOP suspension after oral administration has been reported as 1.74 μg/ml/h after oral administration in rats (17). In this work, AUC0–24 of DOP conventional tablets and optimized formulation F5 were obtained as 78.40 and 205.43 μg/ml/h, respectively, which were significant in comparison with reported value (P < 0.01). The Tmax and Cmax of DOP suspension after oral administration in rats have been reported as 0.50 h and 0.24 μg/ml, respectively (17). In this work, the Tmax and Cmax of DOP from DOP tablet after oral administration in rats were obtained as 2.00 h and 25.31 μg/ml, respectively, which were also significant in comparison with reported values (P < 0.01). The relative bioavailability of optimized formulation F5 with respect to DOP conventional tablets was recorded as 262.00%. The in vivo absorption of DOP from optimized SLN F5 resulted in 2.62-fold enhancement in oral bioavailability as compared with its conventional tablets. The possible reason for enhancement in oral absorption/bioavailability of DOP from SLN F5 was possible due to the particle size in nanometer range, sustained DOP release profile, and the presence of solubilizers and bioenhancers such as Tween-80 and Dynasan 118 in SLN F5 in comparison with conventional tablets.
CONCLUSIONS
In order to obtain sustained release profile and to enhance oral bioavailability of DOP, various SLN formulations were developed and evaluated using different excipients in this work. Prepared formulation was characterized physicochemically and evaluated for in vitro drug release studies. Formulation F5 was optimized and chosen for in vivo pharmacokinetic studies in rats. Pharmacokinetic studies in rats suggested that optimized SLN F5 controlled the absorption of DOP as compared with DOP conventional tablets. The oral bioavailability of DOP from SLN F5 was around 2.62 times higher than DOP conventional tablets. These results suggested that the developed SLN formulation could be used as an alternative of tablet dosage form of DOP for an effective treatment of nausea and vomiting.
References
Gasco MR. Lipid nanoparticles: perspectives and challenges. Adv Drug Deliv Rev. 2007;59:377–8.
Mehnert W, Mader K. Solid lipid nanoparticles. Production, characterization and applications. Adv Drug Deliv Rev. 2001;47:165–96.
Bunjes H, Drechsler M, Koch MHJ, Westesen K. Incorporation of the model drug ubidecarenone into solid lipid nanoparticles. Pharm Res. 2001;18:287–93.
Muller RH, Radtke M, Wissing SA. Solid lipid nanoparticles (SLN) and nanostructured lipid carriers (NLC) in cosmetic and dermatological preparations. Adv Drug Deliv Rev. 2002;54:S131–55.
Ahmad N, Keith-Ferris J, Gooden E, Abell T. Making a case for domperidone in the treatment of gastrointestinal motility disorders. Curr Opin Pharmacol. 2006;6:571–6.
Silvers D, Kipnes M, Broadstone V, Patterson D, Quigley EM, McCallum R, et al. Domperidone in the management of symptoms of diabetic gastroparesis: efficacy, tolerability, and quality-of-life outcomes in a multicenter controlled trial. DOM-USA-5 Study Group. Clin Ther. 1998;20:438–53.
Shindler JS, Finnerty GT, Towlson K, Dolan AL, Davies CL, Parkes JD. Domperidone and levodopa in Parkinson’s disease. Br J Clin Pharmacol. 1984;18:959–62.
Nagarsenker MS, Garad SD, Ramprakash G. Design, optimization and evaluation of domperidone coevaporates. J Control Release. 2000;63:31–9.
Reddymasu SC, Soykan I, McCallum RW. Domperidone: review of pharmacology and clinical applications in gastroenterology. Am J Gastroenterol. 2007;102:2036–45.
Patel DM, Patel SP, Patel CN. Formulation and evaluation of fast dissolving tablet containing domperidone ternary solid dispersion. Int J Pharm Investig. 2014;4:174–82.
Shailendra B, Shailendra M, Manish J, Singh TY, Priti T. Design and optimization of domperidone fast dissolving tablet using central composite design. Curr Drug Deliv. 2015;12:736–44.
Prajapati S, Patel L, Patel C. Floating matrix tablets of domperidone formulation and optimization using simplex lattice design. Iranian J Pharm Res. 2011;10:447–55.
Daraghmeh N, Chowdhry BZ, Leharne SA, Al-Omari MMH, Badwan AA. Co-processed chitin-mannitol as a new excipient for oro-dispersible tablets. Mar Drugs. 2015;13:1739–64.
Yadav AV, Mote HH. Development of biodegradable starch microspheres for intranasal delivery. Indian J Pharm Sci. 2008;70:170–4.
Palem CR, Dudhipala NR, Battu SK, Repka MA, Rao YM. Development, optimization and in vivo characterization of domperidone-controlled release hot-melt-extruded films for buccal delivery. Drug Dev Ind Pharm. 2016;42:473–84.
Prabhu P, Shah S, Gundad S. Formulation development and investigation of domperidone transdermal patches. Int J Pharm Invest. 2011;1:240–6.
Jakki R, Syed MA, Kandadi P, Veerabrahma K. Development of a self-microemulsifying drug delivery system of domperidone: in vitro and in vivo characterization. Acta Pharma. 2013;63:241–51.
Patel R, Shah D. Nanoparticles loaded sublingual film as an effective treatment of chemotherapy induced nausea and vomiting. Int J Pharm Technol Res. 2015;8:77–87.
Thatipamula RP, Palem CR, Gannu R, Mudragada S, Yamsani MR. Formulation and in vitro characterization of domperidone loaded solid lipid nanoparticles and nanostructured lipid carriers. Daru. 2011;19:23–32.
Yassin AEB, Anwer MK, Mowafy HA, El-Bagory IM, Bayomi MA, Alsarra IA. Optimization of 5-fluorouracil solid-lipid nanoparticles: a preliminary study to treat colon cancer. Int J Med Sci. 2010;7:398–408.
Madishetti SK, Palem CR, Gannu R, Thatipamula RP, Panakanti PK, Yamsani MR. Development of domperidone bilayered matrix type transdermal patches: physicochemical, in vitro and ex vivo characterization. Daru. 2010;18:221–9.
Qi X, Qin J, Ma N, Chou X, Wu Z. Solid self-microemulsifying dispersible tablets of celastrol: formulation development, charaterization and bioavailability evaluation. Int J Pharm. 2014;472:40–7.
Reagan-Shaw S, Nihal M, Ahmad N. Dose translation from animal to human studies revisited. FASEB J. 2008;22:659–61.
Klimkowska MB, Zywiec K, Poteulas A, Szutowski M. Impact of the changes in P-glycoprotein activity on domperidone pharmacokinetics in rat plasma. Pharmacol Rep. 2007;59:752–6.
Gibaldi M, Perrier D. Pharmacokinetics. 2nd ed. New York: Marcel Dekker; 1982.
Venkateswarlu V, Manjunath K. Preparation, characterization and in vitro release kinetics of clozapine solid lipid nanoparticles. J Control Release. 2004;95:627–38.
Torchilin V. Handbook of nanobiomedical research: fundamentals, applications and recent developments, vol. 1–4. World Scientific Publishing, Singapore, Hackensack (NJ), London, 2014.
Doijad RC, Manvi FV, Godhwani DM, Joseph R, Deshmukh NV. Formulation and targeting efficiency of cisplatin engineered solid lipid nanoparticles. Indian J Pharm Sci. 2008;70:203–7.
Gaumet M, Vargas A, Gurny R, Delie F. Nanoparticles for drug delivery: the need for precision in reporting particle size parameters. Eur J Pharm Biopharm. 2008;69:1–9.
Gupta M, Vyas SP. Development, characterization and in vivo assessment of effective lipidic nanoparticles for dermal delivery of fluconazole against cutaneous candidiasis. Chem Phys Lipids. 2012;165:454–61.
Varshosaz J, Minayian M, Moazen E. Enhancement of oral bioavailability of pentoxifylline by solid lipid nanoparticles. J Liposome Res. 2010;20:115–23.
Sanna V, Caria G, Mariani A. Effect of lipid nanoparticles containing fatty alcohols having different chain length on the ex vivo skin permeability of econazole nitrate. Powder Technol. 2010;201:32–6.
Abbasalipourkabir R, Fallah M, Sedighi F, Maghsood AH, Javid S. Nanocapsulation of nitazoxanide in solid lipid nanoparticles as a new drug delivery system and in vitro release study. J Biol Sci. 2016;16:120–7.
Kotikalapudi LS, Adepu L, Ratna JV, Diwan PV. Formulation and in vitro characterization of domperidone loaded solid lipid nanoparticles. Int J Pharm Biomed Res. 2012;3:22–9.
Dudhipala N, Janga KY. Lipid nanoparticles of zaleplon for improved oral delivery by Box–Behnken design: optimization, in vitro and in vivo evaluation. Drug Dev Ind Pharm. 2017;43:1205–14.
Kelidari HR, Saeedi M, Akbari J, Morteza-semnani K, Valizadeh H, Maniruzzaman M, et al. Development and optimisation of spironolactone nanoparticles for enhanced dissolution rates and stability. AAPS PharmSciTech. 2017;18:1469–74.
Assaf SM, Qandil AM, Al-Ani EA. Fast and pH-dependent release of domperidone from orally disintegrating tablets. Pharm Dev Technol. 2013;18:897–905.
Jain A, Jain SK. In vitro and cell uptake studies for targeting of ligand anchored nanoparticles for colon tumors. Eur J Pharm Sci. 2008;35:404–16.
Liu J, Hu W, Chen H, Ni Q, Xu H, Yang X. Isotretinoin-loaded solid lipid nanoparticles with skin targeting for topical delivery. Int J Pharm. 2007;328:191–5.
Rahman Z, Zidan S, Khan MA. Non-destructive methods of characterization of risperidone solid lipid nanoparticles. Eur J Pharm Biopharm. 2010;76:127–37.
Kushwaha AK, Vuddanda PR, Karunanidhi P, Singh SK, Singh S. Development and evaluation of solid lipid nanoparticles of raloxifene hydrochloride for enhanced bioavailability. Biomed Res Int. 2013;2013:E584549.
Heykants J, Knaeps A, Meuldermans W, Michiels M. On the pharmacokinetics of domperidone in animals and man I. Plasma levels of domperidone in rats and dogs. Age related absorption and passage through the blood brain barrier in rats. Eur J Drug Metab Pharmacokinet. 1981;6:27–36.
Acknowledgements
“The authors would like to extend their sincere appreciation to the Deanship of Scientific Research at King Saud University for funding the work through research group project No. RGP-139.”
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Shazly, G.A., Alshehri, S., Ibrahim, M.A. et al. Development of Domperidone Solid Lipid Nanoparticles: In Vitro and In Vivo Characterization. AAPS PharmSciTech 19, 1712–1719 (2018). https://doi.org/10.1208/s12249-018-0987-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1208/s12249-018-0987-2