Abstract
The liquid and semisolid matrix technology, filling liquids, semi-solids and gels in hard gelatin capsule are promising, thus, there is a need of enhanced research interest in the technology. Therefore, the present study was aimed to investigate isoniazid (freely soluble) and metronidazole (slightly soluble) gels filled in hard gelatin capsules for the effect of poloxamers of different viscosities on release of the drugs. Gel of each drug (10% w/w, particle size 180–250 μm), prepared by mixing poloxamer and 8% w/w hydrophilic silicon dioxide (Aerosil® A200), was assessed for rheology, dispersion stability and release profile. Both the drugs remained dispersed in majority of gels for more than 30 days, and dispersions were depended on gels’ viscosity, which was further depended on viscosity of poloxamers. A small change in viscosity was noted in gels on storage. FTIR spectra indicated no interactions between components of the gels. The gels exhibited thixotropic and shear-thinning behaviour, which were suitable for filling in hard gelatin capsules without any leakage from the capsules. The release of both drugs from the phase-stable gels for 30 days followed first-order kinetics and was found to be correlated to drugs’ solubility, poloxamers’ viscosity, polyoxyethylene contents and proportion of block copolymer (poloxamers) in the gels. The findings of the present study indicated that release of drugs of different solubilities (isoniazid and metronidazole) might be modified from gels using different poloxamers and Aerosil® A200.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
INTRODUCTION
The hard gelatin capsule technology, originally used for filling solids, is now being extended to fill liquids showing the Newtonian behaviour and semi-solids such as thixotropic mixtures, thermosoften materials, matrices gels and pastes (1–7) and is known as the liquid semisolid matrix (LSSM) technology. This technology may be used to address the limitations associated with soft gelatin capsules and has the potentials to combine/translate the benefits associated with powder filling in hard gelatin capsules and that of the liquids filling in soft gelatin capsules.
The process of dry filling of capsule is associated with dust generation possibly leading to cross contamination, variations in fill weight due to varied flowability of powders owing to their physical properties and poor control on release of poorly soluble drugs. The technology of filling soft materials in hard gelatin capsules is devoid of complications associated with the conventional hard-gelatin technology (8). This approach is also capable of resolving problems related to liquid dosage forms including inconvenient handling, transport and storage issues due to bulkiness, poor aqueous stability of hydrolysable ingredients, need of antimicrobial preservatives, dependency of accurate dose on the ability of patients to use or a volumetric dropper and unpleasant drug taste (9). In the liquid semisolid matrix technology, the formulations can be prepared without liquid handling, difficulties in exact measurement of the doses and a clean administration. However, the problem of content leakage from the closed capsule can be addressed using viscous formulations to be retained in capsule or alternatively sealing capsules in a way that keeps enclosed material inside (10, 11). The filling and sealing technologies of hard capsules further provide wider chances of improvements and applications of such dosage forms (4).
There are certain specific requirements of filling liquid/semisolid materials in hard gelatin capsules. In general, the materials with thixotropic shear-thinning behaviour are desired for satisfactory capsule filling at the ambient temperature such that the apparent viscosity of the formulation decreases during shear, subjected on the material during filling process, but increases once the formulation is filled in the capsules (1). There is a need to control pH, temperature, types and amounts of polymers and excipients in the formulations, which affect the thixotropic property (1, 12). The formulation rheology must be compatible with the liquid pumping capacity of the automatic filling machinery, the range of which is proposed to be 0.1–25 Pa s. For a dispersion of solid drug particles in the molten excipient, the rheology is affected by the properties of the disperse phase (particle size and concentration) and the continuous phase (molecular weight and viscosity), leading to filling limitations (13). Satisfactory capsule filling of molten dispersions can be achieved up to a limiting concentration of disperse phase, dependent on particle size distribution and continuous phase viscosity (14). Changing the chemical nature of the gels using hydrophilic or hydrophobic silicon dioxide in liquid poloxamers of different ratios of polyoxyethylene and polyoxypropylene groups have a considerable effect on gel viscosity and hence capsule filling properties (15). The aim of this research was to investigate the effect of poloxamers, block copolymer of polyoxyethylene and polyoxypropylene of various viscosities and molecular weights on the rheological parameters and release of highly soluble isoniazid and slightly soluble metronidazole of particular size (180–250 μm) from the poloxamers/A200 (hydrophilic silicone dioxide) hard gelatin capsule-filled gels.
MATERIAL AND METHOD
Materials
Isoniazid and metronidazole were obtained as gift from Schazoo Zaka Pharmaceutical (Pvt.) Ltd., Lahore, Pakistan, and Mediceena Pharma (Pvt.) Ltd., Lahore, Pakistan, respectively. Analytical grade liquid poloxamers (Pluronics PE/L31, PE/L43, PE/L62, PE/64, PE/L92 (BASF, Germany) were procured from the local market. The silicone dioxide (A200), a hydrophilic-natured silicon (Degussa, UK), was gifted by Schazoo Zaka Pharmaceutical (Pvt.) Ltd., Lahore, Pakistan.
METHODS
Preparation of Gels
Thixotropic gels (100 g), without drugs, labelled as control/simple gels, were prepared using methods described earlier (5, 15, 16). Briefly, 8% w/w hydrophilic silicon dioxide (Aerosil®, A200) was incorporated into the respective poloxamers (Table I) at room temperature using a paddle mixer (Heidolph, RZR 2051 Controlled, Germany). The resulting mixture was mixed at 100 rpm for 90 min (16, 17). The prepared gel was then kept in vacuum chamber for 30 min to remove air (5) and then stored in glass bottles having plastic closure at room temperature (20 ± 2°C) for 30 days for rheological investigation.
For preparation of drug containing gels, 10% w/w of isoniazid or metronidazole (both of particle size, 180–250 μm, separated by the Retsch Sieve Shaker (AS-200, Pennsylvania, USA), was incorporated in a simple gel of respective poloxamers so that the final weight of the gel was 100 g. The mixing which was employed for preparation of simple gel was extented to 45 min for appropriate dispersion of drugs in respective gels.
CHARACTERISATION OF GELS
Physical Appearance
Physical appearance of each control gel and gels containing isoniazid or metronidazole was observed at room temperature (25°C) after 2 and 24 h and then after 7, 14 and 30 days of their preparation.
Evaluation of Phase Separation
The gel systems were kept undisturbed and dispersion stability was assessed by visual inspection, drug’s settling or phase separation. Observations were made after 2 and 24 h and then after 7, 14 and 30 days to record the time of phase separation, if any. The sedimentation was also confirmed by comparing rheology data obtained after 2 and 24 h.
Determination of Drug Contents in Gels
The contents of isoniazid or metronidazole were determined in respective gels using UV-VIS spectrophotometer (T 70 PG Instrument Ltd., UK). For isoniazid, absorbance of the filtered sample was measured at 263 nm, whereas the absorbance of metronidazole was measured at 278 nm. Each sample was analysed in triplicate and quantification was performed from the respective calibration curves.
Rheological Characterisation
Rheograms of each poloxamer, control gel and gels containing isoniazid or metronidazole were taken at room temperature (25°C) at Rheometer (TA Instrument Ltd. AR. 1500) with cone and plate geometry. The shear rate was uniformly increased from 0 to 1000 s−1 over 1 min and then decreased to zero over 1 min at room temperature. The rheograms were taken at 2 and 24 h and then at 7, 14 and 30 days to study the time-dependent rheology of the gels. The yield of each simple gel was also noted once at 2 h. The viscosity of each poloxamer was measured once, whereas gels containing isoniazid or metronidazole were investigated for viscosity at the same time intervals as above considering the highest shear rate of 990 s−1 (Pa s).
Filling of Gels Containing Drugs in Hard Gelatin Capsule
The gels containing drugs were hand filled at room temperature, using syringe into size 1 transparent hard gelatin capsules, having individual fill weights of about 450 mg. The filled capsules were stored at room temperature in sealed containers for 24 h so that a strong gel structure could be formed (17).
In Vitro Drug Release Studies
The in vitro release of drugs was carried out for only the gels which, showed phase stability for more than 30 days. The release of drugs was investigated in the dissolution apparatus I (Erweka Dissolution Tester (FRL 700, Heusenstamm, Germany) using 900 mL water for isoniazid and 0.1 N HCl for metronidazole. The media were maintained at 37 ± 0.5°C and the basket was rotated at 100 rpm. Six capsules for the stable gels of respective drugs from each poloxamers were tested individually. An aliquot (10 mL) was withdrawn at regular intervals of 30 to 180 min while maintaining the volume in the vessels with the same dissolution medium. The samples were analysed in triplicate at respective wavelengths and quantified from the respective calibration curves. Different kinetic models were applied to find release rate and release mechanisms from their respective gels (18–21).
Fourier Transform-Infrared Spectroscopy
The gels were taken in a diffuse reflectance sampler and IR spectra were recorded by scanning in the wavelength region of 4000–400 cm−1 in a Fourier transform-infrared spectrophotometer (FTIR Nicolet 6700 ZnSe Optics, Thermoelectronics, USA). The spectra obtained were observed for incompatibilities between components and the chemical integrity of the drug in the gels after preparation and over the time.
RESULTS
The simple gels and those containing drugs were found to be smooth and stable. The smoothness and stability were not found to be affected immediately by the properties of poloxamers, such as viscosities, molecular weights and ratios of polyoxyethylene and polyoxy-propylene contents (Table I).
Sedimentation
Isoniazid gel containing poloxamer L62 (F03) and metronidazole gels having poloxamers L43 (M02) and L92 (M05) exhibited sedimentation at 24 h of their preparation (Table II).
Drug Contents in Gels
Table II shows the percent content of isoniazid and metronidazole.
Rheological Characteristics
Figure 1a shows that the poloxamers exhibit Newtonian behaviour. The viscosity of the poloxamers under study was within the range of 100–270,000 mPa s (Table I), and the filling of gels in the hard gelatin capsule did not pose any problem.
All the rheograms of the simple gels taken at 2 and 24 h, and then, 7, 14 and 30 days exhibited a hysteresis loop (Fig. 1b–f) along with plastic and pseudoplastic behaviour with fluctuations, being prominent in the rheograms obtained after 24 h. Comparison of the rheograms of simple gels at 2 and 24 h, indicated a slight increase in viscosity (Fig. 1b–f).
During storage for 30 days, all the simple gels, except that contained L64 exhibited plastic flow along with thixotropic behaviour (Fig. 2a–e). The gels prepared with poloxamer L64 exhibited pseudoplastic flow.
The rheograms of the gels containing isoniazid or metronidazole at 2 and 24 h and 7, 14 and 30 days exhibited a hysteresis loop (Figs. 3a–e and 4a–e). Like the simple gels, a slight increase in the viscosity was observed in the isoniazid and metronidazole gels at 2 and 24 h, as shown in Figs. 3a–e and 4a–e, respectively.
The rheograms of stable gels containing isoniazid or metronidazole at 7 to 30 days (Figs. 5a–d and 6a–c, respectively) showed the time-dependent rheology. The rheological profile of each selected gel after 24 h is also shown in Figs. 5a–d and 6a–c, respectively, for comparison to that of the 7 and 30 days to observe the change after formation of gel structure at 24 h. During storage for 30 days, all the selected gels retained their plastic or pseudoplastic flow along with the thixotropic behaviour.
Table III shows that the apparent viscosity (ƞ a ) was maintained reasonably well over the whole storage period of 30 days although there were some minor variations.
Plastic Flow and Yield Value
The curves shown in Fig. 1b–d, f indicated plastic flow in the gels. No yield values were demonstrated in a pseudoplastic system (Fig. 1e). The viscosity of pseudoplastic gels decreased on increasing rate of shear (Table IV).
In the present study, the yield values of all the five poloxamers were recorded once at 2 h and were given in Table V. The apparent viscosity and yield values of simple gels and gels containing drugs are given in Table III. The apparent viscosity of the simple, isoniazid or metronidazole gels were recorded at 2 and 24 h and then at 7, 14 and 30 days considering the highest shear rate of 990 s−1 (Pa s) (Table V). The addition of isoniazid or metronidazole in the simple gels caused an increase in the yield value (Table V) and apparent viscosity (Table III) over the period of 1 month.
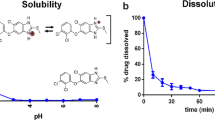
In Vitro Release of Isoniazid and Metronidazole from Gels
The calibration curves of isoniazid and metronidazole along with the linear regression equation and correlation coefficient are given in Fig. 7a, b. The isoniazid release from the selected phase-stable isoniazid gels is given in Table VI and Fig. 8a. The isoniazid gels labelled as F01, F02, F04 and F05 exhibited the first-order kinetics (Table VII). The slope obtained from graph revealed that all the gels showed different release rates. The formulations F01 and F04 showed 100.11 and 104.25% drug release, respectively, in 3 h. For the formulation F02 with L43 poloxamer, the drug release within 30 min was found to be 81.84%. On the other hand, F04 containing L64 poloxamer held drug release for 30 min liberating only 14.49% drug and rapidly released the remaining drug subsequently. The isoniazid gel (F04) containing L64-A200 showed the highest release. The extent of drug release for F01 was lesser as compared to F04. However, F05 exhibited lesser rate and extent of drug release.
The release of metronidazole gels M02 (containing poloxamer L43) and M05 (formulated with poloxamer L92) were not studied because of occurrence of sedimentation in 24 h (Fig. 4b, e). Based on the percent release of metronidazole (Table VI and Fig. 7b), the release kinetics for the selected metronidazole gels, determined by regression coefficient, R 2, is shown in Table VII. The gels, M01, M03 and M 04, exhibited the first-order kinetics (Table VII). However, the release rates of metronidazole from different gels were different as indicated by the slope values. The metronidazole gels M01 and M04 showed 100.64 and 106.39% drug release, respectively, while M03 exhibited 50% release at the end of 3 h. The metronidazole gel M04 (which was prepared using the L64-A200) showed the highest release of the drug. On the other hand, metronidazole gel, M03 (prepared using L62), showed the least release (50%) as compared to M01 (L31/A200) which showed 100% release in 3 h.
Fourier Transform-Infrared Spectra
Fourier transform-infrared spectra of the pure isoniazid (Fig. 9a–c) showed the characteristic peaks of the pure drug, which were masked in the phase-stable isoniazid gels. The bands corresponding to N-H and C-H stretching (in region 3100, 3000 to 2800 cm−1) and bands of C-O, C-N and C-C were masked by a broad peak appearing in a region of 1150 to 1000 cm−1 (22). The FTIR spectrum of metronidazole (Fig. 10a–c) has shown all the major peaks characteristics of the pure drug (22). However, in all the phase-stable metronidazole gels prepared employing respective poloxamer masked the bands in 3000 to 2850 cm−1 corresponding to the OH, CH-CH stretching and bands in 1100 to 1000 cm−1 corresponding to CN, C-C and NO.
Discussion
In this study, the gels were prepared using five poloxamers (Table I) and 8% w/w Aerosil® A200 to incorporate 10% w/w of the model drugs, isoniazid and metronidazole (particle size 180–250 μm). The above percentages of Aerosil® A200 and drugs were taken from the literature (16, 17, 23). The simple gels were characterised in terms of appearance, phase separation, rheology and the Fourier transform-infrared spectroscopy. The gels containing drugs were additionally assessed for the drug contents. All the gels were smooth and stable immediately after their preparation. However, after 24 h of preparation, some gels viz., isoniazid gel containing poloxamer L62 and metronidazole gels with L43 and L92 showed sedimentation (Table II) which was also supported by the rheograms of the above gels, where hysteresis loops of the gels at 24 h were lower than that of the taken after 2 h (Figs. 3c and 4b, e). The percent contents of isoniazid and metronidazole (Table II) in their respective gels were within the reported standard concentrations (24).
Poloxamers are the non-ionic surfactants and block copolymers of a central hydrophobic chain of polyoxypropylene flanked by two hydrophilic chains of polyoxyethylene with different viscosities. The viscosity of the poloxamers increased with the increase in their molecular weight across the poloxamer series (Tables I and V). The viscosity of the poloxamers under study was within the range of 100–270,000 mPa s (Table I), which indicated their suitability for filling into hard gelatin capsules (25). Smith et al. (8) has reported viscosity 0.027 Pa s (27 mPa s) as too low to optimally pump and to avoid the formulation losses by splashing during the filling process. Hawley (26) found 24000 m Pa s viscosity was high to cause problems with filling of materials in capsules. In this study, the filling of gels in the hard gelatin capsule did not pose any problem during filling.
The purpose of rheograms of simple gels at 2 h was to compare them to the rheograms of 24 h to assess whether the gel structure had been formed, indicated by viscosity increase. The rheograms at 7 to 30 days were obtained to observe the time-dependent rheological modifications in gels, which might be relevant for suitability of the filling in capsules. The hysteresis loop in the rheograms of the simple gels (Fig. 1b–f) taken at the above time intervals is the characteristics of the materials with plastic or pseudoplastic flow along with thixotropic behaviour. Fluctuations were noted in the rheograms of all simple gels after 24 h, which may be attributed to the increase in viscosity and formation of strong gel structure between poloxamer and silicon dioxide after 24 h. The addition of drug into the simple gels of all poloxamers led more prominent fluctuations in a rheogram even at 2 h due to a further increase in viscosity and gel formulation. This trend of fluctuation was continued after 24 h and 7, 14 and 30 days of preparation.
A slight increase in viscosity in the rheograms of simple gels at 24 h (Fig. 1b–f), seemingly pointing to the development of a gel structure between the respective poloxamers and silicon dioxide. After the formation of gel structure, the asymmetric arrangement in molecules would have occurred. Thus, along with hydrogen bonding between hydrophilic silicon dioxide and respective poloxamer drug gel formation, it increases the viscosity and forms a three-dimensional structure (5).
The rheological profiles of each gel after 24 h (Fig. 2a–e) were compared to that at 7 and 30 days to observe the change in viscosity after gel structure formation. After 30 days storage, the exhibition of plastic flow along with thixotropic behaviour in the simple gels containing poloxamers other than L64 was likely due to the development of a strong gel structure. The pseudoplastic flow shown by gels prepared with poloxamer L64 might be ascribed to re-alignment of polymer. Thus, the gels were shown to be suitable for filling into capsules. It was further expected that there were no storage-dependent rheological behaviour changes, which might limit the material filling into capsules.
The exhibition of hysteresis loop in the rheograms of the isoniazid or metronidazole gels at all the time intervals was the specific feature of materials with plastic or pseudoplastic flow along with thixotropic behaviour. The presence of the hysteresis loop indicates the occurrence of a breakdown in gel structure, and the area within the loop may reflect an index for the degree of breakdown or thixotropy (Figs. 3a–e and 4a–e). Similar to the simple gels, increase in the viscosity of gels after 24 h (Figs. 3a–e and 4a–e, respectively) demonstrated the development of gel structure in all gels except in isoniazid gel prepared using L62 and metronidazole gels formulated using L43 and L92. Each gels showed comparable results in preliminary work with the isoniazid, where L31 and L64 were investigated by using silicon dioxide (1–10% w/w) to observe the dispersion stability (stable isoniazid gels after 24 h) and release rate (16).
The retaining of plastic or pseudoplastic flow along with the thixotropic behaviour in the selected isoniazid and metronidazole gels during storage for 30 days indicated stability and suitability of the above gels for filling in the hard gelatin capsules. Thixotropic behaviour is induced by the specific arrangement of asymmetric molecules of a material along the line of its flow. Such systems have the reduced apparent viscosity during the high-shear processes, such as mixing and filling into capsules followed by increased apparent viscosity after filling. Thixotropic systems are composed of asymmetric macromolecules, which are capable of interacting by numerous secondary bonds to produce a loose three-dimensional structure, so that the material is gel-like when un-sheared. The energy imparted during shearing disrupts these bonds and the flowing elements become aligned and the viscosity falls, as a gel-sol transformation occurs. When the shear stress is eventually removed, the structure tends to reform, although the process is not immediate and increases with time as the molecules return to the original state under the influence of the Brownian motion (27). The apparent viscosity (ƞ a ) was related to the viscosity of the original poloxamer given in Table V, which also supported the increase in ƞ a of the gels.
The curves shown in Fig. 1b–d, f represent a body that exhibits plastic flow. The curve on a plot of stress vs. shear of plastic materials does not pass through the origin, but rather intercepts the shearing stress axis at a particular point, referred to as the yield value (27). Materials with such curves are known as the Bingham body and do not begin to flow until a shearing stress corresponding to the yield value exceeds. At stresses below the yield, the substance acts as an elastic material. Bingham bodies that exhibit yield value are classified as solid, whereas substances that begin to flow at the smallest shearing stress and show no yield value are defined as liquids.
Plastic flow is associated with the presence of flocculated particles in concentrated suspensions. As a result, a continuous structure is set up throughout the system. A yield value exists because of the contacts between adjacent particles (brought about by the Van der Waals force), which must be broken down before flow can occur. Consequently, the yield value is an indication of forces of flocculation; the more flocculated the suspension, the higher will be the yield value. Frictional forces between moving particles can also contribute to yield value. Therefore, a plastic system resembles to a Newtonian system at shear stresses above the yield value (27).
In contrast to the plastic systems, the consistency curve in pseudoplastic materials begins at the origin, indicating no yield value as shown in a plastic system (Fig. 1e). Furthermore, since no part of the curve is linear, the viscosity of a pseudoplastic material cannot be expressed by a single value. The viscosity of a pseudoplastic substance decreases with increasing rate of shear (Table IV). The curved rheogram for pseudoplastic materials results from a shearing action on long-chain molecules of materials such as linear polymers. As shearing stress is increased, normally disarranged molecules begin to align along their long axes in the direction of flow. This orientation reduces internal resistance of the material and allows a greater rate of shear at each successive shearing stress, thereby decreases the apparent viscosity. On adding isoniazid or metronidazole in the simple gels increased the yield value and apparent viscosity (Table III) over the period of one month revealed a high stability of the internal structure of the gel (28).
The linear curves between concentration and absorbance curves for isoniazid and metronidazole (Fig. 7) were appropriate for conversion of absorbance to concentration of the respective drugs.
The present findings for isoniazid release are comparable to the preliminary investigations where the gels containing 8% w/w silicon dioxide with the poloxamers L31 and L64, released 100% isoniazid (used as received, without characterised particle size) in approximately 3 h (16). The gel F02 with L43 poloxamer released 81.84% drug within 30 min displaying burst release characteristics. On the other hand, F04 gel containing L64 poloxamer held drug release for 30 min liberating only 14.49% drug and rapidly released the remaining drug subsequently. This pattern of drug release from the gels is related to polyoxyethylene (POE) contents and viscosity of poloxamers (16). From poloxamer-silicon dioxide gels, the release also depends on the hydrophilicity of silicon dioxide and the physicochemical properties of the drug (1, 29). However, in this study, viscosity of poloxamers exhibited domineering effect in controlling drug release compared to the POE contents. As a normal trend in this study, when POE contents were decreased, the amount of drug release was appreciably retarded. Such as we observed that the isoniazid gel, F04 containing L64-A200 showed the highest release as it contained 40% POE and its molecular weight was approximately 1750 for the polyoxypropylene (POP) portion (Table I). Gel F01 composing L31 and F02, L43 has 10 and 30% of POE contents, respectively; hence, the extent of drug release was lesser as compared to gel F04. It was expected that the gel, F05 with 20% polyoxyethylene, by virtue of containing L92 should exhibit the drug release in between that shown by F01 (with POE 10%) and F04 (with POE 30%), but the F05 exhibited lesser rate and extent of drug release. Thus, the contribution of the effect of POE content on the isoniazid release from F05 gel might has surrendered against the effect of viscosity of L92, which had the highest value, i.e. 740 Pa s (Table I) as compared to all of its counterparts under the study.
The release of metronidazole gels M02 (containing poloxamer L43) and M05 (formulated with poloxamer L92) were not studied because of occurrence of sedimentation (Fig. 4b, e) in 24 h. The gels, M01, M03 and M 04 exhibited first-order kinetics (Table VII). The release of the metronidazole from the gels was also affected by POE contents and the viscosity of the poloxamers as reported (16). It was because the release of drugs from poloxamer-silicon dioxide gels had also been related to the hydrophilicity of silicon dioxide and the physicochemical properties of the drug (1, 29). The metronidazole gel M04 (which was prepared using the L64-A200) showed the highest release of the drug since it contains 40% POE and its molecular weight is approximately 1750 for the POP portion. On the other hand, metronidazole gel, M03 (prepared using L62), showed the least release (50%) as compared to M 01 (L31/A200) which showed 100% release in 3 h containing 20 and 10% POE contents, respectively.
In the phase-stable gels containing isoniazid and metronidazole, the Fourier transform-infrared spectra of the respective pure drugs (Figs. 9 and 10) showed the masking of characteristic peaks might be due to the excess of poloxamer and silicon dioxide in isoniazid gels, rather than due to a chemical change.
CONCLUSION
The pure poloxamers showed Newtonian behaviour while the simple, isoniazid and metronidazole gels exhibited plastic or pseudoplastic along with thixotropic behaviour. The stable gels of both drugs showed the dispersion stability for 1 month. Poloxamer L64 showed the maximum drug release for freely soluble isoniazid and slowly soluble metronidazole from their gels. Poloxamer L92 and L62, respectively, exhibited the least release of isoniazid and metronidazole from their gels. The FTIR indicated no interaction between the components of gels and the drugs. The hydrophilic gel system prepared by different poloxamers and silicon dioxide may be used to modify the release rate of the drugs having different solubility. The rheological characteristics of theses gels are such that they can be easily filled in hard gelatin capsules without leakage issue. This study may enhance the viability, research and use of liquid semisolid matrix technology.
References
Walters P, Rowley G, Pearson J, Taylor C. Formulation and physical properties of thixotropic gels for hard gelatin capsules. Drug Dev Ind Pharm. 1992;18(15):1613–31.
Walker S, Ganley J, Bedford K, Eaves T. The filling of molten and thixotropic formulations into hard gelatin capsules. J Pharm Pharmacol. 1980;32(1):389–93.
Cuine A, Francois D. British Patent 1590864. 1978.
Djimbo M, Moes AJ. Release of drugs formulated as hard pastes filled into hard gelatin capsules. J Pharm Belg. 1984;39(1):36–42.
Saeed T. Rheological characterization of poloxamer/silicon dioxide gels for liquid-filled hard gelatin capsule. PhD Thesis, University of Sunderland. 1999.
Hawley AR, Rowley G, Lough WJ, Chatham SM. The physical and chemical characterization of thermosoftened bases for molten filled hard gelatin capsules. Drug Dev Ind Pharm. 1992;18(16):1719–39.
Cade D, Cole ET, Mayer JP, Wittwer F. Liquid filled and sealed hard gelatin capsules. Drug Dev Ind Pharm. 1986;12(11-13):2289–300.
Smith A, Lampard J, Carruthers K, Regan P. The filling of molten ibuprofen into hard gelatin capsules. Int J Pharm. 1990;59(2):115–9.
Pharmaceutics A’s. The science of dosage form design. 2nd ed. UK: Elsevier Science limited; 2002.
Jones BE. Hard gelatin capsules and pharmaceutical formulation. Pharm Technol. 1985;9:106–12.
Rowley G. Filling of liquids and semi solids into two piece capsules, chapter 9, pharmaceutical capsules. 2nd ed. UK: Pharmaceutical press; 2004.
Lee CH, Moturi V, Lee Y. Thixotropic property in pharmaceutical formulations. J Control Release. 2009;136(2):88–98.
Kattige A, Rowley G. The effect of poloxamer viscosity on liquid-filling of solid dispersions in hard gelatin capsules. Drug Dev Ind Pharm. 2006;32(8):981–90.
Kattige A, Rowley G. Influence of rheological behaviour of particulate/polymer dispersions on liquid-filling characteristics for hard gelatin capsules. Int J Pharm. 2006;316(1):74–85.
Saeed T, Rowley G, Walters PA, Bowley W. The effect of disperse phase particle size and continuous phase viscosity on the filling and stability properties of thixotropic gels for hard gelatin capsules. Proc Pharm Tech Conf. 1998;18:85.
Sultana M, Hassan SS, Saeed T, Mahmood R, Tariq I, Shah P, et al. The effect of silicon dioxide concentrations on drug release from poloxamer/silicon dioxide gel formulations and their rheological characterization. Lat Am J Pharm. 2013;32(6):911–7.
Ellison MJH, Rowley G, Walters PA, Barnes DMH. Release of drug from gel thixotropic triglyceride formulations, liquid filled in hard gelatin capsules. Proc Pharm Tech Conf. 1995;14:91.
Hadjiioannou TP, Christian GD, Koupparis MA, Macheras PE. Quantitative calculations in pharmaceutical practice and research. New York: VCH Publishers Inc; 1993. p. 345–8.
Bourne DWA. Pharmacokinetics. In: Banker GS, Rhodes CT, editors. Modern pharmaceutics. 4th ed. Marcel Dekker Inc: NewYork; 2002. p. 67–92.
Higuchi T. Mechanism of sustained‐action medication. Theoretical analysis of rate of release of solid drugs dispersed in solid matrices. J Pharm Sci. 1963;52(12):1145–9.
Korsmeyer RW, Gurny R, Doelker E, Buri P, Peppas NA. Mechanisms of solute release from porous hydrophilic polymers. Int J Pharm. 1983;15(1):25–35.
Clarke’s analysis of drugs and poison. Third edition, vol.2, Pharmaceutical Press UK; 2004.
Benedict T, Rowley G, Walters PA. The effect of silicon dioxide concentration on drug release from triglyceride formulations, liquid filled in hard gelatin capsule. Proc Pharm Tech Conf. 1997;16:237.
British pharmacopoeia. Printed in the United Kingdom by the Stationary Office N5669694 C34 8/2008. 2009.
McTaggart C, Wood R, Bedford K, Walker SE. The evaluation of an automatic system for filling liquids into hard gelatin capsules. J Pharm Pharm. 1984;36(2):119–21.
Hawley AR. Investigation of thermosoftened solid dispersion formulations of ibuprofen for hard gelatin capsules. PhD Thesis, University of Sunderland, 1993.
Martin AN, Sinko JP. Physical pharmacy and pharmaceutical sciences: physical chemical and biopharmaceutical principles in the pharmaceutical sciences. 6th Edition Lippincott Williams & Wilkins, 2011.
Bodek KH. Evaluation of properties microcrystalline chitosan as a drug carrier. Part 1. In vitro release of diclofenac from mictocrystalline chitosan hydrogel. Acta Pol Pharm. 2000;57(6):431–42.
Walters PA, Rowley G, Pearson JT, Tayler CJ. In vitro drug release by colloidal silicon dioxide in a semisolid matrix hard gelatin capsule formulation. Int Symp Control Rel Bioact Mater. 1991;18:65.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Sultana, M., Butt, M.A., Saeed, T. et al. Effect of Rheology and Poloxamers Properties on Release of Drugs from Silicon Dioxide Gel-Filled Hard Gelatin Capsules—A Further Enhancement of Viability of Liquid Semisolid Matrix Technology. AAPS PharmSciTech 18, 1998–2010 (2017). https://doi.org/10.1208/s12249-016-0674-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1208/s12249-016-0674-0