Abstract
The establishment of an in vitro–in vivo correlation (IVIVC) is considered the gold standard to establish in vivo relevance of a dissolution method and to utilize dissolution data in the context of regulatory bioequivalence questions, including the development of dissolution specifications. However, several recent publications, including industry surveys and reviews from regulatory agencies, have indicated a low success rate for IVIVCs, especially for immediate-release formulations. In recent years, the use of physiologically based pharmacokinetics (PBPK) and absorption modeling, as a tool to facilitate formulation development, has been attracting increased attention. This manuscript provides an industry perspective on the current challenges with establishing IVIVCs and the potential PBPK and absorption modeling offer to increase their impact. Case studies across both immediate-release and extended-release formulations from five pharmaceutical companies are utilized to demonstrate how physiologically based IVIVC (PB-IVIVC) may facilitate drug product understanding and to inform bioequivalence assessment and clinically relevant specifications. Finally, PB-IVIVC best practices and a strategy for model development and application are proposed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Biopharmaceutics Classification System (BCS) guidance, first issued by the Food and Drug Administration (FDA) in 2000, provided a clear path to utilization of dissolution data as a surrogate for bioequivalence for BCS I, and, more recently, for BCS III compounds, in rapidly dissolving formulations (1). Outside the BCS I/III space, the establishment of in vitro–in vivo correlations (IVIVCs), a concept initially developed for extended-release (ER) dosage forms (2), has been historically viewed as the primary way to establish in vivo relevance of a dissolution method. Thus, an IVIVC is considered the primary approach to utilization of dissolution data for regulatory questions, related to bioequivalence or for the establishment of clinically relevant dissolution specifications. According to the USP, level A IVIVCs are defined as point-to-point relationships between in vitro dissolution and the in vivo input rate of the drug from the dosage form (3). In the past, several techniques have been applied to develop an IVIVC, including convolution- and deconvolution-based methods. With convolution-based approaches, the link between in vitro dissolution and plasma drug concentrations is established in a single step by directly predicting oral exposure based on the in vitro dissolution profile. This is the simplest IVIVC approach and is well-suited for compounds that exhibit dose-linear, time-invariant disposition and for which no intravenous, oral solution, or IR reference dose is available (4). Deconvolution-based IVIVCs are two-step modeling approaches. First, a deconvolution method is applied to estimate the time course of in vivo input based on a plasma concentration–time profile. Such methods include Wagner-Nelson (5), Loo-Riegelmann (6), or general numerical methods. In the second step, an IVIVC model is developed to relate the in vitro release profile to the time course of in vivo release or absorption. While deconvolution-based methods are widely used (7), one disadvantage is that they rely on the assumption of linear pharmacokinetics, which is often violated. In such cases, the use of physiologically based absorption modeling approaches can bring advantages as it is more mechanistic and considers the separate processes of drug release, dissolution, and permeation across the intestinal membranes. In addition, recent publications by the FDA indicate that the utilization and success rates of IVIVCs remain relatively low and practically non-existent for immediate-release (IR) products (8,9). In recent years, the use of physiologically based absorption modeling, as a tool to facilitate formulation development, has been well-documented in the literature, with several recent reviews available by both regulators and industrial scientists (10,11,12), and has been also the subject of public workshops (13). The purpose of this manuscript is to provide an industry perspective on the current challenges with establishing IVIVCs and the potential for physiologically based pharmacokinetics (PBPK) and absorption modeling to increase their impact. Case studies across both IR and ER formulations are utilized to demonstrate the opportunity of establishing clinically relevant specifications.
Current Status of IVIVC and Physiologically Based Absorption Modeling in Pharmaceutical Development
While the term IVIVC is usually associated with late-stage development activities and regulatory applications for post-approval biowaivers, in practice, the efforts for establishing an in vitro–in vivo link start as early as in first-in-human (FIH) studies. Data from such early studies can be analyzed to understand in vivo absorption rates for formulations and to start attempting correlations to in vitro data (14). Parallel to the generation of clinical data, dissolution methods evolve from using biorelevant media, such as simulated gastric fluid (SGF) or fasted-state simulated intestinal fluid (FaSSIF) in earlier stages of development, to more quality control (QC) standard buffers. If possible, in later development stages, clinically relevant dissolution methods are obtained (15). During this development period, clinical data are generally widely utilized to understand the relevance of dissolution observations. In the simplest form, this could be a confirmation of rank ordering of different formulation technologies that may be tested in relative bioavailability studies.
While, in our experience, IVIVC workflows are typically well-established in different companies for modified-release (MR) products, significant challenges remain in the space of IR formulations for BCS II/IV compounds. Despite the efforts to establish robust IVIVCs, the final success rate and regulatory applications remain low. The challenges for establishing IVIVCs have been highlighted in previous publications and are also summarized briefly here. In a survey published in 2013, inherent compound and formulation properties and lack of predictive dissolution methods were among two of the top technical difficulties identified (16). A more recent survey, conducted as part of the Oral Biopharmaceutics Tools (OrBiTo) Innovative Medicines Initiative project, generally highlighted quite significant variability in the success rate and strategies, among respondents, and, similarly, the 2013 survey also identified compound properties and complexity of required dissolution methods as hurdles from the technical side (17). In this OrBiTo survey, which included specific examples from the different EFPIA (European Federation of Pharmaceutical Industries and Associations) responders, most of the level A examples provided were for ER products. Outside the issues identified in these publications, perhaps one of the challenges to successful establishment of IVIVCs is inherent limitations related to the convolution/deconvolution methodologies employed. For example, the 2013 survey by Fotaki et al. indicated that the traditional method is, by far, the most used methodology (16). However, it is generally acknowledged that this procedure has limitations when applied to compounds with non-linear pharmacokinetics (e.g., due to metabolism) or compounds with incomplete absorption. While for ER formulations, the IR counterpart usually serves as the reference for deconvolution, for IR formulations that are fast dissolving, a reference for deconvolution may not be available. In addition, a “true” oral solution or an intravenous solution formulation may not be readily achievable for very poorly soluble compounds. The reasonably fast dissolution of IR dosage forms in regulatory (sometimes referred to as QC) dissolution methods also can present challenges in establishing the correlation due to significant difference in timeframes of in vitro dissolution and in vivo absorption. While alternate methodologies, such as convolution-based approaches, may help with some of these limitations, these seem even less frequently employed; recently, it was highlighted that such approaches require a predefinition of the correlation function which may not be really known (18).
The promise of using physiologically based absorption modeling to establish an in vitro–in vivo link could be considered obvious, considering the underlying structure of such mechanistic absorption models. Dissolution and permeation processes are modeled mechanistically, allowing for a direct link of each process independently to available data (dissolution data or particle size and solubility information). Non-linearities in either absorption (due to solubility limitations or regio-specific permeability) or metabolism (e.g., due to saturation of first-pass metabolism) can be accounted for in the model independently. In addition, transit functions are also available and can be applied to soluble and insoluble fractions in the lumen of the gastro-intestinal (GI) tract, according to the formulation type and prandial state. Finally, local conditions of pH and volume are varied along the GI tract, to match a healthy, diseased, or pharmacologically altered physiology, which allows in vivo dissolution to be calculated by the model, on the basis of drug substance or drug product particle size. More recently, the ability to model mechanistically the in vitro data provides an additional level of model development that can be leveraged to develop an IVIVC (19,20). As already mentioned, physiologically based absorption modeling is now commonly used during early formulation development, typically with input from biorelevant dissolution data. The successes reported across many manuscripts clearly indicate that an underlying IVIVR is achieved, although perhaps not meeting the criteria which are sought for regulatory applications of a level A IVIVC. In the subsequent sections of this manuscript, case studies are presented to highlight the promise these PBPK models present, in establishing a clear in vitro–in vivo link, and the potential application of these established PB-IVIVCs is discussed. The input parameters for all case studies are provided in detail as Supplementary Material.
Case Study 1—PB-IVIVC for A BCS Class II IR Formulation Under Fed Conditions
This example illustrates the use of PB-IVIVC modeling for a BCS class II development compound, basmisanil, formulated for immediate release. The objectives were to establish a mechanistic model based on drug and formulation properties, to predict basmisanil release and absorption and, then, to demonstrate IVIVC using plasma concentrations from early clinical studies.
Basmisanil is poorly water-soluble but well-permeable and was formulated as a micronized drug in an IR tablet for early clinical studies (21). Phase 1 data showed a dose-proportional increase in Cmax and AUC in the dose range from 1.5 to approximately 160 mg, but increases were less than dose proportional above 160 mg. This pharmacokinetic behavior over the entire dosing range could be very well captured using mechanistic absorption modeling in GastroPlus™ v9.0 (Simulations Plus, Lancaster, CA). The model suggested two different rate-limiting steps for absorption (Fig. 1a). At low doses, the compound was completely soluble in the fed-state intestine and absorption was mainly dissolution-rate limited. However, at high-dose levels, after an initial dissolution rate limit, the intestinal fluids became saturated, and, thus, absorption was solubility limited (21). This resulted in incomplete absorption during intestinal transit at higher doses.
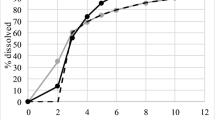
a Open squares, mean observed ± standard deviation and simulated (continuous line) dose normalized Cmax; b correlation between in vitro and in vivo dissolution data obtained following deconvolution of in vivo profiles using the GastroPlus Mechanistic Absorption Model; observed versus predicted c Cmax and d AUC values resulting from the IVIVC model developed using the GastroPlus mechanistic absorption model as deconvolution method and by fitting a double Weibull’s function to the in vivo dissolution data. The open symbols represent the two datasets used for IVIVC model development; filled symbols represent datasets used for model verification
Basmisanil exposure was shown to be particularly sensitive to drug and formulation properties in the lower dose range. The development of a biorelevant in vitro dissolution method in combination with an IVIVC model was, therefore, of high interest to support further formulation development. As deconvolution methods for modeling the in vivo dissolution profiles of basmisanil, the Loo-Riegelmann, the numerical deconvolution, and the mechanistic absorption models were compared. The mechanistic absorption method resulted in an excellent correlation between deconvoluted in vivo dissolution profiles and in vitro dissolution in FeSSIF (Fig. 1b), which was clearly superior to the traditional deconvolution methods (Table I). These PB-IVIVC model predictions were accurate over the entire dosing range from 1.5 to 1000 mg under fed-state conditions and for different IR formulations (tablet, film-coated tablet, granules in sachet formulation), as shown in Fig. 1c, d.
The traditional dissolution methods are typically used under fasted-state conditions and for compounds and formulations exhibiting linear and non-saturable absorption. However, in the case of basmisanil, drug absorption was either dissolution rate or solubility limited depending on the dose. Also, absorption was influenced by the food status of the study subjects, which affects, for example, the GI transit time and intestinal solubility. In such cases, the use of the mechanistic deconvolution method provides a clear benefit in terms of IVIVC model performance. This study highlights the value of generating a good mechanistic understanding of oral formulation performance in order to select appropriate IVIVC techniques and, thus, to support drug product design early in clinical development.
Case Study 2—PB-IVIVC for A BCS Class II IR Formulation Under Fasted Conditions
This example highlights the use of a mechanistic model to extract a product-specific particle size distribution (P-PSD), for various lesinurad clinical and commercial batches, and the use of this P-PSD as an input to a PBPK model to establish a mechanistic IVIVC. This IVIVC is, then, used to verify that the proposed dissolution specification sits within a bioequivalent space, by determining the edge of failure for in vitro dissolution (22).
Lesinurad is a weak acid, BCS class II drug with limited solubility in acidic conditions but rapid and complete dissolution in intestinal conditions. This drug also exhibits irregular gastric emptying phases with multiple absorption peaks in 30% of the subjects. Due to this variability, the mechanistic absorption model set-up was undertaken on individual PK data using intravenous and oral plasma concentration time profiles. For this work, several ways to integrate dissolution in PBPK were attempted to recommend a mechanistic approach suited for IR formulations. Successful PB-IVIVCs rely on means to integrate product batch-specific dissolution data in PBPK models that are clinically relevant. Depending on the solubility constraints in vivo, dissolution data obtained in typically higher than physiological volumes, with sometimes synthetic surfactants and regular agitation rates, may not necessarily be representative of the in vivo dissolution rate for IR products. Mechanistic approaches to integration of dissolution data are not new, and the work done by Takano et al. (23) in introducing the Z-factor, has shown that a “unique” parameter describing the effect of particle size can be derived from dissolution data and can be used as an input to predict dissolution in lower volumes, for different doses or different solubility conditions. There are limitations to the Z-factor, in that it cannot be used when product dissolution follows multiple phases (fast and slow or variable rate), whether this was engineered in the formulation or whether it was resulting from process or formulation parameters. Weibull’s fit of dissolution data or use of tabulated dissolution data is not mechanistic and will “force” dissolution to happen in vivo at the in vitro rate and extent. Following dissolution, the drug can be absorbed or precipitate depending on the local conditions and model parameters. The determination of a P-PSD allows a 10-bin particle size distribution to be determined using dissolution data obtained with appropriate discriminant conditions on various formulation batches. A 10-bin particle size distribution is enough to capture simple to complex dissolution rates in various media. The P-PSD is then used to verify if the product in vitro dissolution can be adequately predicted in various conditions of pH, volume, dose, type, and level of surfactant. If the agreement with in vitro data is good, the P-PSD can then be used as batch representative input for the PBPK model in conjunction with mechanistic dissolution models of the software. Using this approach, the in vivo dissolution simulated by the software is fully mechanistic and will depend on transit time, local conditions of pH, volume, human bile salt levels, dose to be dissolved, absorption rate, or efflux. This approach is particularly useful for IR formulations in conjunction with virtual trials, as it will generate in vivo dissolution profiles for the simulation which will be different between- and within-subject, depending on the local conditions in the gastrointestinal tract and on variability in the permeability and efflux.
For lesinurad, this approach was used and shown to be able to predict the outcome of a clinical trial where non-bioequivalence to a reference clinical batch was observed using a mechanistic absorption model based on GastroPlus v9.0. The model was, then, used with virtual trials to predict the edge of failure for dissolution, i.e., the dissolution rate of a virtual batch that would still be bioequivalent to the clinical rapid-dissolving reference. This edge of failure was used to justify the proposed dissolution specification for Zurampic® at the time of submission to the FDA (Q80 at 30 min) and later used for regulatory flexibility for Duzallo® (lesinurad/allopurinol) fixed-dose combination, to set the dissolution specification of lesinurad to Q80 at 45 min (Fig. 2). Lessons learnt from this exercise were that it is important to generate data proactively in the drug development, to be able to justify proposed product specifications based on modeling if possible, or on in vivo data. Regulatory flexibility can come from PB-IVIVC and can help increase drug product specifications based on mechanistic IVIVC.
Case Study 3—PB-IVIVC for A BCS Class IV Compound to Set Clinically Relevant Specifications
During commitment site stability testing of simeprevir formulations, significantly lower QC dissolution results were obtained compared to the release measurements. For packaging configurations and storage conditions presenting stability dissolution results near the specifications limits, the clinical relevance of the observations was investigated using PB-IVIVC. The in silico approach aimed to determine the main drivers in the absorption process and to evaluate the potential effect of a slower dissolution rate on the PK profile of the compound.
Simeprevir is a BCS class IV compound, characterized by low solubility and poor permeability. The compound is formulated as the amorphous sodium salt and made commercially available in IR capsules. The compound shows non-linear pharmacokinetics explained by the combined mechanisms of saturation of liver metabolism, gut metabolism, hepatic transporters, and active intestinal efflux transporters (P-gp) (24). A mechanistic absorption model (ACAT model of GastroPlus™ v8.5) was used in combination with a simplified compartmental disposition model, to integrate the interplay between drug product dissolution, permeation, and active efflux and metabolism of simeprevir. Pharmacokinetic data of the human absolute bioavailability study were used for verification of the PBPK model. In this study, a low isotopically labeled intravenous dose was administered on top of a 50 or 150 mg non-labeled oral dose. Absolute oral bioavailability, fraction absorbed, and the fraction escaping gut wall and liver extraction could be derived at the two dose levels by combining the clinical data with the information obtained from metabolic profiling in feces. Using these data, model parameters for gut CYP3A4 and P-gp saturation could be verified. The dissolution rates of reference formulations and formulations showing slower QC dissolution profiles were experimentally derived, in conditions simulating the physiologic gastrointestinal conditions of fed adult humans. The dissolution rates (the “Z-factor”) were calculated from these data and were used in the model. As such, the impact of a slower dissolution rate, which would result in lower simeprevir concentrations at the level of the enzymes and transporters in the gut, could be predicted by the model.
In Fig. 3, an overlay of the observed data in healthy male subjects and the simulated average is shown for a single-dose administration of 50 and 150 mg simeprevir together with the corresponding absorption–dissolution curves. For both doses, the increase in drug amount dissolved in function of time is much faster than the increase in drug amount absorbed. This means that relative to the permeability, the dissolution rate is less important in determining the amount absorbed and subsequently entering the portal vein and systemic circulation.
The top figures represent the overlay linear plots of simulated and observed simeprevir plasma concentration–time profiles following single oral dosing at 50 mg (left) and 150 mg (right). The red lines are the observed data, and the black line represents the simulated simeprevir concentration–time profile in a virtual average male healthy subject. The bottom figures represent the corresponding absorption–dissolution curves. The amount dissolved is shown in red, the amount absorbed in cyan, the cumulative amount that entered the portal vein in blue, and the cumulative amount that entered the systemic circulation in green
Figure 4 shows the impact of lowering the in vitro dissolution rate (Z-factor) in the biorelevant media on the amount of simeprevir that enters the portal vein. As the model did not account for saturation of hepatic transporters and enzymes in a mechanistic way, the overall impact on the peak plasma concentration (Cmax) and area under the plasma concentration–time curve (AUC) is not shown. Nevertheless, the result of the sensitivity analysis enables to define a range between which the tested biorelevant dissolution profiles would result in comparable fraction reaching the portal vein. Only a significant decrease in the in vitro dissolution rate is predicted to impact the bioavailability. No effect is to be expected when the dissolution rate modestly changes for the formulations. The toleration window for dissolution rate in biorelevant media is also visualized in Fig. 4 by the green lines. The observed biorelevant dissolution profiles of the reference and stability batches are all within the range where it is predicted that differences in dissolution rate will have no effect on exposure.
Visualization of the impact of the dissolution rate on the amount entering the portal vein as evaluated by parameter sensitivity analysis. The data points in red and blue are correspond to the data derived from the reference formulation (blue) and stability samples (red) (left). The outcome was translated in a range of biorelevant dissolution profiles resulting in comparable pharmacokinetics (green lines) in comparison with observed biorelevant dissolution profiles from reference (blue) and stability (red) samples with slower quality control dissolution profiles (black lines) (right)
The study illustrates the suitability of PB-IVIVC to explore the relationship between in vitro dissolution and in vivo drug exposure by integrating all components of absorption in a physiological context. The PB-IVIVC model was used as supportive information in regulatory communications for post-approval change of the dissolution specification criterion to clinical relevance, which was accepted by the major regulatory agencies.
Case Study 4—PB-IVIVC for a MR Formulation for A BCS III Compound with Regio-Dependent Absorption
Compounds with regio-dependent permeability, which can result in various extent of absorption from different ER formulations, have been considered potentially difficult cases to establish IVIVC with traditional methodologies. This example demonstrates the development of a PB-IVIVC for ER formulations of MK-0941, a BCS III compound with lower colonic absorption.
MK-0941 mesylate salt exhibited high solubility across the physiological pH range and was a good candidate for both hydroxypropyl methylcellulose (HPMC) matrix and ethylcellulose (EC)-based multi-particulate formulations. Formulations with differing release rate corresponding to a T80 (time to 80% dissolved) of approximately 8, 12, and 16 h were manufactured for each system and tested clinically. As described in the original publication (25), the formulations exhibited different bioavailability with the 8, 12, and 16 h release formulations resulting in 65, 67, and 52% relative bioavailability to the IR reference for the matrix and 74, 72, and 54% for the multi-particulates. To facilitate further formulation development and future manufacturing changes, an IVIVC was sought. A level A IVIVC model via the traditional deconvolution/convolution approach was only possible by adopting a piecewise linear correlation with the IVIVC correlation parameters changing approximately at the 5 h timepoint. Even with the adoption of the two-stage procedure, it was difficult to fully meet prediction error criteria for Cmax for the matrix system with an approximately 15% average prediction error.
Since commonly used physiologically based absorption models break down the intestine to distinct compartments, they allow for incorporation of regional permeability in the absorption process. For MK-0941, such a physiologically based model was developed using GastroPlus v8.0. Regional permeabilities were fitted across the observed data for MR formulations, while the in vitro dissolution was used as input. The optimized permeabilities suggested regio-dependent absorption with low permeability in the large intestine that resulted in the differential bioavailability of especially the slowest releasing formulation. Two separate PB-IVIVC models were developed for the two formulation technologies; overall, these resulted in accurate prediction of the plasma concentration profiles as shown in Fig. 5, as well as in improved prediction errors relative to the traditional IVIVC approach for the respective technology. For both technologies, prediction errors were less than 10% on average for both AUC and Cmax.
It should be acknowledged that in a PB-IVIVC setting there may be some interdependencies of parameters; for example, in the case of MK-0941 MR formulation, it is practically very difficult to fully decouple the impact of regional permeability from potential deviations between in vitro and in vivo release rates, as these may have directionally the same effect on plasma concentration profiles. In a traditional deconvolution/convolution approach, these interdependencies may be less obvious as they are combined in the different terms of the mathematical correlation, such as time scaling and absorption scaling, without a physiological meaning. For example, the correlation change point of 5 h used for the traditional IVIVC for MK-0941 does not directly correspond to the generally accepted small intestinal transit time of 3.5 h. Thus, in our opinion, this example demonstrates the potential for PB-IVIVC to play a complementary role to traditional deconvolution/convolution-based IVIVC in the MR formulation space. Furthermore, the PB-IVIVC setting may provide the opportunity to link such correlations better to the general biopharmaceutics knowledge for the compound/formulation, and, in the case of MK-0941, it reflected the anticipation of lower colonic permeability.
Case Study 5—IVIVC for A BCS Class I MR Formulation Under Fasted and Fed Conditions
This example compares a mechanistic approach to establishing IVIVC using Simcyp® v15/R1 and GastroPlus™ v9.0 and a mathematical deconvolution incorporating a Qgut model to extract in vivo absorption rates for zolpidem IR and MR formulations (26). Zolpidem hemitartrate is a BCS class I drug with good in vitro permeability and good solubility throughout the physiological pH range. The dissolution rate of IR tablets is rapid as per BCS definitions.
In vivo plasma profiles were simulated with both software platforms using a “middle-out” approach, where the disposition parameters are calculated from intravenous pharmacokinetic data and where the dissolution rate of zolpidem formulation measured in various fluids was tested as input (using a Weibull’s function fit for GastroPlus™ and tabulated data with piecewise cubic polynomial interpolation for Simcyp®). The prediction of the observed negative food effect was also verified. The “top-down” approach used an algebraic deconvolution of plasma profiles based on up to 4 fractions of dose which can be absorbed independently with different absorption rates and lag times.
Individual pharmacokinetic profiles for intravenous and oral routes and subject co-variates were used to extract individual disposition parameters, predict first-pass gut extraction from the Qgut model, and calculate fraction absorbed and absorption rate. This top-down analysis was done using an Excel® tool developed for this purpose. The top-down analysis revealed that the in vivo absorption profiles for IR zolpidem 10 mg IR tablets are de-coupled from in vitro dissolution whereas the correlation between MR in vivo absorption rate and in vitro dissolution for 10 and 12.5 mg MR formulations enables a level A IVIVC with time shift corresponding to the lag phases observed (Fig. 6). Another lesson from this work was that the variability observed between- and within-subjects could be linked to gastric emptying profiles and observed lag times. Over the 72 individual administrations, lag times were found to range from 0.05 to 1.5 h (arithmetic mean ± SD of 0.54 h ± 0.28). The within-subject variability in lag times was 33%, expressed as relative standard deviation (RSD), and ranged from 0 to 150%, while the between-subject variability was 50% RSD and did not depend on the formulation type. These lag times are similar to those observed for lesinurad (22) (see case study 2). After the lag times, zolpidem absorption rate from the IR formulation is rapid and consistent with the drug substance properties. Because of variable gastric emptying patterns, the average absorption profile extracted from average PK data for the IR formulation does not reflect the in vivo dissolution rate for that formulation. This example illustrates the difficulty of a classical IVIVC, which uses the IR profile as a reference to calculate the unit impulse response. Even with an IR formulation or a solution, the gastric emptying time may lead to variability which will, on the average, lead to an underestimation of the in vivo absorption rate and may lead to issues in differentiating between absorption and elimination when intravenous references are not available (27).
Individual absorption profiles calculated from deconvolution analysis for the IR Stilnox® 10 mg (a), 10 mg MR Ambien® CR (c), and 12.5 mg MR Ambien® CR (e) (left panel), and comparison of the mean absorption to the in vitro dissolution rate for the IR Stilnox® 10 mg (b), 10 mg MR Ambien® CR (d), and 12.5 mg MR Ambien® CR (f) formulations from the bioavailability study (right panel). Standard deviations are indicated with the error bars
The other learning from the top-down approach was that the food effect or the variability in the fasted state was mainly related to the in vivo fraction absorbed. For the IR 10 mg formulation, the between-subject variability in Fh or Fg amounted to less than 10% RSD whereas the Fa RSD was approximately 20%.
The “middle out” approach using both Simcyp® and GastroPlus™ for predicting fasted- and fed-state individual pharmacokinetic profiles has shown that it is important to de-couple gastric emptying patterns with the in vitro dissolution data. One subject was shown to have up to 6 h stomach retention in the fed state and rapid release after this period. All the plasma concentrations were adequately predicted except Cmax which was over-estimated compared to the measured one. This is probably because the Cmax was missed in the in vivo study due to the spacing of PK sampling time points after 6 h post-dose administration. Experiments in milk and FeSSGF, both complex high-fat environments, showed that both rate and extent of drug release were affected, and this could explain the negative observed food effect for zolpidem. Other explanations could be found in the more unfavorable hydrodynamics in the fed state which could lead to slower and incomplete release (28,29).
Case Study 6—PB-IVIVC for a Prodrug Formulated in an Extended-Release Matrix
BMS-663068 is a highly soluble HIV-1 attachment inhibitor phosphate ester prodrug developed for oral administration as an ER 600 mg hydrophilic matrix tablet. The prodrug to parent conversion by alkaline phosphatase can occur in the GI tract brush boarder membrane and facilitate absorption of the more permeable parent compound. Preliminary studies to develop an IVIVC and associated PBPK model leveraged clinical experience provided by a human site of absorption study that employed InteliSite® capsules and gamma scintigraphy imaging (30). The model was applied to a series of drug release profiles typical of hydrophilic matrix ER tablets (release over the range of 3–24 h) to provide simulations of the pharmacokinetic behavior expected from 600 mg doses. These simulations demonstrated the potential for achieving the desirable target pharmacokinetic profile having a Cmax reduction combined with increased Cmin (Ctau). However, a predictive IVIVC was not initially realized when formulations spanned a wide release range that mixed multiple-release mechanisms (erosion and diffusion). Mechanistic deconvolution from the GastroPlus™ model (Fig. 7) demonstrates deviations that are most apparent after the first several hours, which is consistent with diffusion-dominated in vitro release that does not imitate the extent of in vivo erosion. During the late-stage development of MR tablet formulations, additional clinical studies (described subsequently) were conducted to establish a definitive mechanistic IVIVC for the primary-release mechanism (diffusion from hydrophilic matrix) that would cover critical tablet performance attributes (polymer composition and tablet dimensions).
Virtual trial population simulations were conducted (GastroPlus™ v8.5) on a range of theoretical dissolution profiles centered on observed release kinetics of the reference 600 mg tablet formulation to define compositions that could be evaluated in the clinic to support commercial product release rate specifications. Several theoretical dissolution profiles ranging from 85 to 120% of the reference formulation release at each time point were used first to establish the predicted range of AUC and Cmax values. From this, appropriate profiles were taken forward to virtual trial populations simulations in a crossover design, which was replicated using five distinct populations to assess variability. The virtual trial population simulation results for mean exposure and confidence intervals were analyzed to establish release rates that could be expected to exhibit exposure outside of the bioequivalence range defined by the reference tablet. These selected release rates were then compared to a range of in vitro dissolution profiles from batches manufactured with different levels of polymer content (drug-to-polymer ratio, DPR) and physical dimensions (surface area to volume ratio, SAVR) to identify target compositions. These PBPK-predicted exposures served as a response surface (Fig. 8) for the tablet design space to guide just-in-time interim selection of target formulation compositions for clinical testing. Three initial release profiles predefined by PBPK model simulations were introduced into the clinic, followed by three subsequent clinical observations that leveraged integrated PBPK simulations to rapidly introduce new drug product compositions in the clinic that would maximize knowledge and establish a robust formulation design space and IVIVC. This integrated use of PBPK model to design formulations for an IVIVC study and to include real-time treatment decisions based on simulations demonstrated by strong predictability. Together, the model and accumulated clinical data provided extensive representation of performance across a wide design space that was used to facilitate appropriate formulation and process quality controls. The formulation and process controls were selected to achieve consistent dissolution behavior such that the IVIVC supported equivalent clinical performance.
Recommendations and Perspective on Future Directions
The case studies provided in this report clearly demonstrate the advantages of PB-IVIVCs for compounds and formulations exhibiting complex absorption behavior. While traditional IVIVC methods may be adequate for highly permeable compounds exhibiting linear PK (7), the PB-IVIVC approach has shown its utility for poorly permeable drugs too or when saturable mechanisms are limiting fraction bioavailable. It allows to go beyond simple dissolution–exposure relationships by accounting for multiple pre- and post-absorption factors, such as saturation of liver and gut metabolism, intestinal efflux transporters, or regional-dependent absorption, as shown in case studies 3 and 4. The increasing number of poorly soluble and/or poorly permeable molecules in pharmaceutical development pipelines (31) stresses the need for such advanced IVIVC and modeling techniques. PB-IVIVC was also shown to be a suitable approach for predicting drug exposure under fed-state conditions (case study 1), whereas traditional IVIVC methods are typically applied to fasted-state data (21).
Establishing a link between in vitro performance and oral exposure is important at early stages of drug product development. IVIVC approaches often provide fundamental understanding of drug and formulation performance in vivo which is an important element of the Quality by Design (QbD) strategy for drug product development in the pharmaceutical industry (2). Such mechanistic understanding of drug product performance is key for rational decision-making and to guide development activities or clinical study design strategies. During early pharmaceutical development, IVIVCs are typically developed with a limited set of clinical data or a reduced number of different formulation types or strengths. The main purpose is to generate knowledge on the in vivo absorption performance of a drug candidate and clinical formulation. At this stage, IVIVC models often do not fulfill the requirements for a regulatory submission and are not adequate, for example, to justify a waiver for a bioequivalence study. Nevertheless, such studies have been shown to be extremely helpful for internal decision-making and de-risking development strategies (e.g., bioequivalence studies). While early stage IVIVCs may be developed based on data generated specifically for the generation of an IVIVC model (e.g., as for development of a MR formulation (25)), in other cases, an early IVIVC may be established based on existing data obtained from comparative bioavailability studies with formulations exhibiting different release mechanisms. A successful PB-IVIVC is then extremely valuable for exploring the observed differences and identifying formulation attributes that are critically impacting oral exposure (21).
The use of IVIVCs is also typically associated with late-stage development and regulatory applications, for example to support flexibility in drug product manufacture, enabling changes in manufacturing sites, raw material suppliers, or minor changes in formulation or manufacturing process. Such late-stage uses are very valuable as drug product changes are common and successful IVIVC can replace bioequivalence trails and thus avoid unnecessary clinical studies while accelerating development and saving resources (32). Aside from a surrogate for late-stage formulation bridging, in a regulatory application setting, the PB-IVIVC may help fill in the current gap in IVIVC applications for IR products towards establishment of clinically relevant specifications. This is exemplified by case study 2, where using product particle size distribution estimated from the dissolution data allowed the development of a PB-IVIVC model that was used to estimate an in vivo and in vitro bioequivalence space that was subsequently used to set release specification. It is worth highlighting that for such application to specifications as demonstrated in case studies 2 and 3, dissolution kinetics can come from more compendial dissolution methods (often referred to as QC methods) rather than from the dissolution methods in biorelevant media that are used in earlier development stages for other physiologically based modeling applications, such as formulation selection or food effect projections.
A question that is often raised for PB-IVIVC is that of model verification (for the purposes of this manuscript, the term verification includes the procedures outlined as internal/external validation in the original IVIVC guidance), especially in a regulatory application setting. Although, recently, both EMA and FDA published draft guidances on use of PBPK models in regulatory applications, the focus is largely on simulations for drug–drug interactions (DDIs). Thus, the only available guidance on criteria for IVIVC model development/qualification remains the one from the original FDA IVIVC guidance for the conventional IVIVC methodologies. In our view, the multiple publications on physiologically based oral absorption modeling suggest that the underlying principles of the models can be considered qualified. Thus, the verification question shifts more towards the individual compound model and the question for which the model is applied.
We believe that the near future will bring more examples of PB-IVIVC applications and alignment of the industry, academia, and regulators on the strategies to adopt depending on the nature of the drug substance and drug product. The principles outlined in the available regulatory guidances, that model robustness needs to be ensured with use of appropriate input parameters, relevant parameter sensitivity analysis, and estimation of the prediction errors, are acceptable. For the examples presented in this manuscript which are focusing on questions around bioequivalence and/or specification settings, we generally applied similar concepts to what is outlined in the existing IVIVC guidance for model qualification and utilized prediction error estimates to assess model behavior. One deviation from the existing IVIVC guidance was that for some of the examples presented, model development and verification was done on average data, rather than on individual data. In the traditional IVIVC model setting, individual data are used to estimate individual subject absorption rate and extent, although final model qualification (and future projections) is based on average data. Although it remains an open question, whether for compounds with moderate to low variability this approach provides significant advantages over use of average data, this can be considered common practice. In a PBPK model setting, aside from the use of individual-subject unit-impulse-response data that can be accomplished with either methodology, individual measurement of underlying physiological parameters (e.g., gastric and intestinal transit, pH values, permeability) remains a hurdle in clinical practice but can be applicable when simple biomarkers are available and can be used in the clinic in the target population. As shown in case studies 2 and 5, stomach residence times were obtained from fitting to observed lag times.
Population virtual trials are usually employed to verify the range of exposure predicted and compare these to clinical measurements. This approach cannot alone ensure the validity of the model, since distinct parameters could lead to the same effect on exposure as highlighted in case study 4. In preparation of a virtual trial, sensitivity analysis is key to determine the physiological or drug-related parameters, which are most influential on human exposure. With careful selection of within- and between-subject variability of the model underlying parameters, PB-IVIVC models allow, contrary to the traditional IVIVC, to simulate the impact of more parameters, run virtual trials to predict bioequivalence of different batches, or predict exposure in different populations. The variability sources can be tied to key physiological parameters (e.g., gastric pH and stomach transit time for a weak base) and be informed by population physiological databases or by individual clinical data of pilot studies.
Similarly to traditional IVIVC, when possible, verification of the model against a non-bioequivalent batch should be undertaken. This is, generally, easily accomplished for MR formulations where sufficient difference in dissolution rate can be easily obtained, and this is demonstrated in case studies 4 and 6. However, in our experience, this may be more difficult for an IR formulation or may require manufacturing of a batch significantly outside the intended manufacturing space. However, if feasible, then, that batch can be used to qualify the model, as shown in case study 2. As more experience is obtained with PB-IVIVC from both industry and regulatory sides and with the steady increase in publications on this topic, we believe that best practices will start to be adopted and may eventually lead to adoption of a regulatory guidance on the topic, similar to the traditional IVIVC.
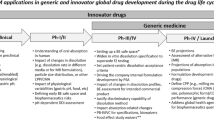
The strategy we propose to follow to establish PB-IVIVC is to start on selected compounds, which have demonstrated proof of concept (phases 1–2) and are likely to reach late development. The objectives are to support specifications and QbD of the commercial formulation (Fig. 9). Criteria for the development of PB-IVIVC are based on the nature of the compound and preliminary evaluation of in vitro and in vivo data to define, through sensitivity analysis, the main factors limiting absorption in human. These factors could be used to recommend the use of specific biomarkers in the clinic, to mechanistically understand the within- or between-subject variability when expected to be large. In vitro data may be preliminary or conflicting at this stage, such as when the drug self-micellizes, since it may, despite large apparent solubility, impact absorption by reducing the free drug fraction. Following this initial evaluation, the likelihood of success for PB-IVIVC can be assessed and commercially relevant variants could be prepared and tested with existing dissolution methods. Once the human study is conducted, a PBPK model based on preferably individual data, if biomarkers were used, or average profiles, can be used to extract in vivo dissolution rates and compare in vitro dissolution to in vivo dissolution. Dissolution methods that are clinically relevant can subsequently be developed using in vivo absorption rates as the blueprint if the preliminary methods failed the correlation. The full package consisting of clinically relevant methods for commercially representative variants and PB-IVIVC can then be used to justify the product specifications and design space, the size of the bioequivalent space, and the minor changes occurring during the life of the product on the market. Finally, once PK-PD or PK-safety data become available, these mechanistic models can be used to improve the reference commercial formulation which could lead to new life cycle management (LCM) products.
Proposed strategy to develop PB-IVIVC and use mechanistic oral absorption modeling to cover late-stage product development. Highlighted in gray are the steps where absorption modeling and/or PB-IVIVC are applied (MR, modified release; IR, immediate release; QC, quality control; LCM, life cycle management; PBPK, physiologically based pharmacokinetics; PK, pharmacokinetics; QbD, quality by design)
Conclusions
Physiologically based absorption modeling can nowadays provide an alternative methodology for the development of in vitro–in vivo correlations. The case studies presented in this manuscript demonstrate how PB-IVIVC can address, when needed, the challenges with traditional IVIVC models for MR systems such as accounting for regio-dependent absorption (case study 4), lag in stomach emptying (case study 5), or use of a prodrug (case study 6). Perhaps, more importantly, the PB-IVIVC approach opens more possibilities for establishing IVIVCs for IR products, for which success rates have been historically reported quite low. Three case studies are presented in the manuscript where a PB-IVIVC was used to guide formulation understanding (case study 1) or set clinically relevant specifications (case studies 2–3). The mechanistic and separate modeling of the dissolution and absorption process in the PB-IVIVC model allowed for a successful correlation between in vitro and in vivo dissolution in the presence of food for basmisanil and zolpidem and in the fasted state for lesinurad and simeprevir. For lesinurad and simeprevir, the modeling of the dissolution data allowed for the translation of the dissolution kinetics from the in vitro setting to the in vivo situation by accounting for changes in the dissolution environment which cannot be accomplished in the traditional IVIVC setting. With the increased adoption of PB-IVIVC, we expect that best practices in development and verification of these models will be established that can eventually inform a regulatory guidance.
References
U.S. Department of Health and Human Services, F.a.D.A., Center for Drug Evaluation and Research (CDER). Guidance for industry: waiver of in vivo bioavailability and bioequivalence studies for immediate-release solid oral dosage forms based on a biopharmaceutics classification system. 2017.
U.S. Department of Health and Human Services, F.a.D.A., Center for Drug Evaluation and Research (CDER). Guidance for industry: extended release oral dosage forms: development, evaluation, and application of in vitro/in vivo correlations. 1997.
USP 41 chapter <1088> In vitro and in vivo evaluation of dosage forms, in United States Pharmacopeia, U.S.P.C. Inc., Editor. 2018.
Gillespie WR. Convolution-based approaches for in vivo-in vitro correlation modeling. In: Young D, Devane JG, Butler J, editors. In vitro-in vivo correlations. Boston: Springer US; 1997. p. 53–65.
Wagner JG. Method for estimating rate constants for absorption, metabolism, and elimination from urinary excretion data. J Pharm Sci. 1967;56(4):489–94.
Loo JCK, Riegelman S. New method for calculating the intrinsic absorption rate of drugs. J Pharm Sci. 1968;57(6):918–28.
Margolskee A, Darwich AS, Galetin A, Rostami-Hodjegan A, Aarons L. Deconvolution and IVIVC: exploring the role of rate-limiting conditions. AAPS J. 2016;18(2):321–32.
Kaur P, Jiang X, Duan J, Stier E. Applications of in vitro-in vivo correlations in generic drug development: case studies. AAPS J. 2015;17(4):1035–9.
Suarez-Sharp S, Li M, Duan J, Shah H, Seo P. Regulatory experience with in vivo in vitro correlations (IVIVC) in new drug applications. AAPS J. 2016;18(6):1379–90.
Jiang W, Kim S, Zhang X, Lionberger RA, Davit BM, Conner DP, et al. The role of predictive biopharmaceutical modeling and simulation in drug development and regulatory evaluation. Int J Pharm. 2011;418(2):151–60.
Kesisoglou F, Chung J, van Asperen J, Heimbach T. Physiologically based absorption modeling to impact biopharmaceutics and formulation strategies in drug development-industry case studies. J Pharm Sci. 2016;105(9):2723–34.
Kostewicz ES, Aarons L, Bergstrand M, Bolger MB, Galetin A, Hatley O, et al. PBPK models for the prediction of in vivo performance of oral dosage forms. Eur J Pharm Sci. 2014;57:300–21.
Zhang X, Duan J, Kesisoglou F, Novakovic J, Amidon GL, Jamei M, et al. Mechanistic oral absorption modeling and simulation for formulation development and bioequivalence evaluation: report of an FDA public workshop. CPT Pharmacometrics Syst Pharmacol. 2017;6(8):492–5.
Cook JA. Development strategies for IVIVC in an industrial environment. Biopharm Drug Dispos. 2012;33(7):349–53.
Grady H, Elder D, Webster GK, Mao Y, Lin Y, Flanagan T, et al. Industry's view on using quality control, biorelevant, and clinically relevant dissolution tests for pharmaceutical development, registration, and commercialization. J Pharm Sci. 2018;107:34–41.
Fotaki N, Gray V, Kesisoglou F, Mayock S, Mirza T, Salt A, et al. Survey results for in vitro-in vivo correlations (IVIVC): critical variables for success. Dissolut Tech. 2013;20(2):48–50.
Nguyen MA, Flanagan T, Brewster M, Kesisoglou F, Beato S, Biewenga J, et al. A survey on IVIVC/IVIVR development in the pharmaceutical industry—past experience and current perspectives. Eur J Pharm Sci. 2017;102:1–13.
Kakhi M, Suarez-Sharp S, Shepard T, Chittenden J. Application of an NLME-stochastic deconvolution approach to level a IVIVC modeling. J Pharm Sci. 2017;106(7):1905–16.
Kesisoglou F. The role of physiologically based oral absorption modelling in formulation development under a quality by design paradigm. J Pharm Sci. 2017;106(4):944–9.
Pathak SM, Ruff A, Kostewicz ES, Patel N, Turner DB, Jamei M. Model-based analysis of biopharmaceutic experiments to improve mechanistic oral absorption modeling: an integrated in vitro in vivo extrapolation perspective using ketoconazole as a model drug. Mol Pharm. 2017;14(12):4305–20.
Stillhart C, Parrott NJ, Lindenberg M, Chalus P, Bentley D, Szepes A. Characterising drug release from immediate-release formulations of a poorly soluble compound, Basmisanil, through absorption modelling and dissolution testing. AAPS J. 2017;19(3):827–36.
Pepin XJ, et al. Justification of drug product dissolution rate and drug substance particle size specifications based on absorption PBPK modeling for Lesinurad immediate release tablets. Mol Pharm. 2016;13(9):3256–69.
Takano R, Sugano K, Higashida A, Hayashi Y, Machida M, Aso Y, et al. Oral absorption of poorly water-soluble drugs: computer simulation of fraction absorbed in humans from a miniscale dissolution test. Pharm Res. 2006;23(6):1144–56.
Snoeys J, Beumont M, Monshouwer M, Ouwerkerk-Mahadevan S. Mechanistic understanding of the nonlinear pharmacokinetics and intersubject variability of simeprevir: a PBPK-guided drug development approach. Clin Pharmacol Ther. 2016;99(2):224–34.
Kesisoglou F, Xia B, Agrawal NG. Comparison of deconvolution-based and absorption modeling IVIVC for extended release formulations of a BCS III drug development candidate. AAPS J. 2015;17(6):1492–500.
Andreas CJ, Pepin X, Markopoulos C, Vertzoni M, Reppas C, Dressman JB. Mechanistic investigation of the negative food effect of modified release zolpidem. Eur J Pharm Sci. 2017;102:284–98.
Chan KKH, Langenbucher F, Gibaldi M. Evaluation of in vivo drug release by numerical deconvolution using oral solution data as weighting function. J Pharm Sci. 1987;76(6):446–50.
Cvijic S, Parojcic J, Langguth P. Viscosity-mediated negative food effect on oral absorption of poorly-permeable drugs with an absorption window in the proximal intestine: in vitro experimental simulation and computational verification. Eur J Pharm Sci. 2014;61:40–53.
Colon-Useche S, et al. Investigating the discriminatory power of BCS-biowaiver in vitro methodology to detect bioavailability differences between immediate release products containing a class I drug. Mol Pharm. 2015;12(9):3167–74.
Brown J, Chien C, Timmins P, Dennis A, Doll W, Sandefer E, et al. Compartmental absorption modeling and site of absorption studies to determine feasibility of an extended-release formulation of an HIV-1 attachment inhibitor phosphate ester prodrug. J Pharm Sci. 2013;102(6):1742–51.
Jermain SV, Brough C, Williams RO. Amorphous solid dispersions and nanocrystal technologies for poorly water-soluble drug delivery—an update. Int J Pharm. 2018;535(1–2):379–92.
Mitra A, Kesisoglou F, Dogterom P. Application of absorption modeling to predict bioequivalence outcome of two batches of etoricoxib tablets. AAPS PharmSciTech. 2015;16(1):76–84.
Author information
Authors and Affiliations
Corresponding author
Additional information
Guest Editors: Marilyn N. Martinez, Sandra Suarez, and Andreas Abend
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Cordula Stillhart, Xavier Pepin, Christophe Tistaert, David Good, Neil Parrott, and Filippos Kesisoglou contribute equally to the authoring of the manuscript.
Electronic supplementary material
ESM 1
(DOCX 54 kb)
Rights and permissions
About this article
Cite this article
Stillhart, C., Pepin, X., Tistaert, C. et al. PBPK Absorption Modeling: Establishing the In Vitro–In Vivo Link—Industry Perspective. AAPS J 21, 19 (2019). https://doi.org/10.1208/s12248-019-0292-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12248-019-0292-3