Abstract
Antibodies (Abs) against infliximab (IFX) increase IFX clearance and can result in treatment failure and acute hypersensitivity reactions. However, interpretation of their clinical value is complicated by individual differences in Ab responses and methods used for quantification. The increase in IFX clearance imposed by anti-IFX Abs has generally been evaluated using a binary classification, i.e., positive or negative. This analysis aimed to investigate if anti-IFX Ab concentrations provide a more adequate prediction of alterations in clearance. Data originated from a clinical trial on Crohn’s disease patients with IFX treatment failure. The trial was not originally designed for pharmacokinetic analysis. Therefore, published pharmacokinetic models were utilized as priors to enable covariate investigation. The impact of anti-IFX Abs on clearance was assessed using different mathematical relationships and exploiting information from two different quantification assays, measuring semi-quantitative “total” or “unbound neutralizing” concentrations of anti-IFX Ab, respectively. Inclusion of anti-IFX Ab status/concentration improved the model’s performance for all investigated relationships. The anti-IFX Ab concentrations were superior to the binary classifications, indicating that the magnitude of increase in IFX clearance imposed by anti-IFX Abs closely relates to their concentration. Furthermore, total anti-IFX Ab concentrations appeared superior to the unbound neutralizing fraction in identifying high clearance individuals. Simulations showed that even at low concentrations, anti-IFX Abs lead to sub-therapeutic IFX concentrations, supporting a need of treatment interventions in all anti-IFX Ab positive patients. The developed model can serve as a basis for further investigations to refine treatment recommendations for patients with anti-IFX Abs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
The pharmacokinetic processes of monoclonal antibodies (mAbs) are mechanistically different from those of small molecule drugs (1,2). In addition, immunological recognition of the mAb as a non-self antigen results in some patients in formation of anti-drug antibodies (Abs), which can influence the pharmacokinetics and compromise efficacy and safety of mAb therapy (3–9). Infliximab (IFX) is a widely used anti-tumor necrosis factor α (TNFα) mAb indicated for several chronic autoimmune diseases, such as inflammatory bowel disease (IBD), i.e., Crohn’s disease and ulcerative colitis. Anti-IFX Abs are detected in about one third of IBD patients on IFX maintenance therapy and are associated with increased IFX elimination, low IFX concentrations, diminished or even eradicated clinical effect, and acute hypersensitivity reactions (5–7,10–14). To restore response in patients with treatment failure in the presence of anti-IFX Abs and low/absent circulating IFX concentrations, a switch to a different TNFα inhibitor is recommended based on clinical trials and observational data (15–21).
Evaluation of the clinical implications of anti-drug Abs is, however, not always straightforward. The interpretation can be challenged by lack of chronology between the detection of anti-drug Abs and symptoms of treatment failure, and/or by transiently detectable anti-drug Abs (22–28). Individual differences in terms of binding characteristics and avidities to the TNFα inhibitor, immunoglobulin (sub)type, and anti-drug Ab concentration may also result in variable effects imposed by anti-drug Abs on the pharmacokinetics of mAbs (8,29,30). Finally, detection and quantification is highly variable between different types of bioanalytical methods, due to both external and internal factors including the following: interference of circulating TNFα inhibitor; detection of low affinity anti-drug Abs; immunoglobulin types and subtypes; measure of abundance (titer vs. mass-based concentrations, total vs. unbound concentration); and type of anti-drug Ab species (neutralizing vs. non-neutralizing) (8,22,29,31,32).
For IFX, the increase in IFX clearance imposed by anti-IFX Abs has generally been evaluated using a binary classification, i.e., anti-IFX Ab positive (+) vs. negative (−) patient. Anti-IFX Ab+ status is associated with a 1.3–2.7-fold increased IFX clearance (4–6,33–35). The aim of this analysis was to evaluate if the actual concentration of anti-IFX Abs provides additional information regarding the pharmacokinetics of IFX as compared to the binary classification in patients with Crohn’s disease. Furthermore, anti-IFX Ab concentrations assessed by two different commonly used anti-IFX Ab assays were compared for this purpose. A population pharmacokinetic modeling approach was applied as this allows for simultaneous characterization of the typical behavior in a population as well as the variability both between and within patients. It also enables incorporation of patient-specific characteristics to explain variability (36). Previously developed pharmacokinetic models for IFX in Crohn’s disease were exploited as frequentist’s priors to facilitate model development from the sparse IFX data available (5,37–39).
MATERIALS AND METHODS
Study Design and Study Population
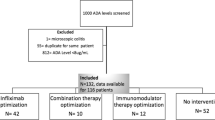
Data originated from a 12-week, single-blind, multicenter, investigator-initiated clinical trial with a 20-week follow-up period (18,19). A total of 69 adult patients with Crohn’s disease who previously had favorable clinical effect of IFX maintenance therapy (5 mg/kg every 5–8 weeks) had been included. At time of inclusion, all patients exhibited treatment failure. Patients had been equally randomized to receive either the following: (i) intensified IFX dosing frequency of 5 mg/kg every 4 weeks or (ii) personalized treatment according to a treatment algorithm based on IFX and anti-IFX Ab concentrations. The algorithm also included treatment alternatives leading to IFX discontinuation, e.g., a switch to other mAb therapy (Fig. 1) (15).
Dosing algorithm based on IFX serum concentrations and anti-IFX Abs used in the clinical trial. anti-IFX Abs anti-infliximab antibodies, CD Crohn’s disease, IFX infliximab, iv intravenous, sc subcutaneous, TNF tumor necrosis factor. Adapted from (15,18). Reproduced and modified with permission from BMJ Publishing Group Ltd from: (18)
Serum samples for quantification of IFX and anti-IFX Abs had been collected at time of screening, and at study weeks 12 and 20. Markers of disease activity, clinical chemistry, patient characteristics, and demographics had been recorded at all study visits (weeks 0, 4, 8, 12, and 20) (18,19). For this analysis, data obtained at study weeks following a switch to a different mAb were excluded due to interference with the used quantification assays. Two serum samples were excluded from this analysis a priori because of (i) an acute infusion reaction leading to incomplete IFX infusion and (ii) a pharmacokinetically implausible concentration (increasing concentration without new dosing).
IFX and Anti-IFX Ab Quantification
IFX and anti-IFX Abs were quantified in serum by use of two mechanistically different assays as detailed in the references (40–42).
In brief, the reporter gene assay (RGA) is a cell-based assay, which quantifies unbound IFX and “unbound neutralizing” anti-IFX Ab concentrations by assessing the biological activity of TNFα at the cellular TNFα receptor level. The lower limit of quantification (LLOQ) for IFX is 0.65 μg/mL and LLOQ for anti-IFX Abs is 20 units (U)/mL (42).
The homogenous mobility shift assay (HMSA) is a high-performance liquid chromatography method, which quantifies unbound IFX by detecting a shift of its peak induced by binding to TNFα. The LLOQ is 1.0 μg/mL for IFX. For anti-IFX Ab quantification, the sample is pre-treated with acid to evoke dissociation of IFX-anti-IFX Abs complexes. Thus, the assay quantifies both unbound and IFX-bound anti-IFX Abs. In addition, HMSA does not differentiate between neutralizing and non-neutralizing anti-IFX Abs as opposed to RGA. Hence, HMSA quantifies the total concentration of both these aspects, hereafter referred to as “total.” The LLOQ for anti-IFX Ab concentration is 3.13 U/mL. Of note, since there is no anti-IFX Ab calibrator commercially available, all anti-IFX Ab concentrations referred to in this paper are (i) relative measurements and (ii) reported in assay specific units, which cannot be directly compared.
IFX concentrations determined by HMSA and RGA have been shown to correlate well (42). In this analysis, IFX concentrations quantified by HMSA were selected for pharmacokinetic model development. Conversely, anti-IFX Ab concentrations from these assays do not correlate well and both assays were thus investigated to evaluate which anti-IFX Ab concentration proved most informative with respect to prediction of IFX clearance.
Handling of Missing Data
Three samples had been analyzed by RGA only. A regression analysis was performed on all samples with an IFX concentration >LLOQ for which both assays had been utilized, in order to impute the missing HMSA values based on the RGA values (see Supplementary Material). As for the anti-IFX Ab concentration, the three missing HMSA anti-IFX Ab concentrations were imputed as having a concentration <LLOQ since they (i) were quantified as <LLOQ by RGA and (ii) all other samples from these individuals were <LLOQ by both assays.
One sample had only been analyzed by HMSA. The missing anti-IFX Ab value for RGA was imputed as <LLOQ although it had quantifiable anti-IFX Ab concentration by HMSA. The impact of this imputation was investigated during model development.
Pharmacokinetic Analysis
Derivation and Development of Prior Model
The clinical study forming the basis of this analysis was not originally designed for pharmacokinetic analysis and included sparse IFX sampling. To enable model development, two published population pharmacokinetic models of IFX in Crohn’s disease were exploited (5,37). For comparability, the two models were re-parameterized and the parameters normalized to a body weight of 65 kg (see Supplementary Material). The models were compared internally as well as to general traits of pharmacokinetics of mAbs (1,43). The resulting model and model parameters were implemented using the prior functionality in NONMEM (v. 7.3), i.e., using a frequentist’s prior (38,39).
The parameter precision of the structural parameters in the prior model was set to the reported values. The degree of freedom (df) of the (inverse Wishart distributed) between-subject variability parameters were calculated according to Eq. 1, in which Ωprior is the prior estimate of the variability and SEΩ,prior is the standard error of Ωprior. The maximum df was equal to the number of patients in the dataset of the prior analysis (39).
IFX serum concentrations were transformed to a logarithmic scale for the analysis. Samples with an IFX concentration <LLOQ were accounted for using a likelihood-based approach (44,45), in which the <LLOQ samples were modeled as a probability of being <LLOQ. The estimation method was Laplacian conditional estimation with interaction. The standard errors of the parameter estimates were obtained from the variance-covariance matrix estimated in NONMEM.
Residual variability models approximating proportional and combined additive-proportional variability on the normal scale were explored. No prior estimate was incorporated for the residual variability because the IFX quantification assays differed between the present and the two published studies.
Standard goodness-of-fit plots were generated to evaluate model performance, including observed IFX concentration vs. population and individual predicted concentrations, and plots assessing the conditional weighted residuals (CWRES) and the normalized prediction distribution errors (NPDE). Visual predictive checks (n = 500) were performed to ensure that simulations from the model generate plausible concentrations (46). Outlier and influence analysis was performed using case deletion diagnostics. Perl speaks NONMEM (PsN, v. 4.2), Pirana (v. 2.9), and R (v. 3.1) with the packages Xpose and ggplot2 were used for model diagnostics and/or to facilitate the modeling process (47–49).
Covariate Model Development
The influence of patient-specific characteristics (=covariates) was investigated on IFX clearance. The impact of anti-IFX Abs was considered first. The anti-IFX Ab information from the two quantification assays was investigated separately using three different mathematical relationships:
-
(I)
As a fractional change in clearance using anti-IFX Ab information as a binary covariate on the patient level (“anti-IFX Ab+/Ab− patient”). A patient was considered anti-IFX Ab+ if exhibiting ≥1 sample with quantifiable anti-IFX Abs.
-
(II)
As a fractional change of clearance using anti-IFX Ab information as a binary covariate on the sample level. That is, similar to item (I) but adding a time-varying aspect.
-
(III)
Anti-IFX Ab concentration included as a continuous covariate with a linear relationship to clearance. Anti-IFX Ab concentrations reported as <LLOQ were considered to be zero, which would correspond to no immune reaction (i.e., anti-IFX Ab−).
Model discrimination was performed using the objective function value, computed as −2 times the log-likelihood, and graphical evaluation including standard goodness-of-fit plots and visual predictive checks. A reduction in objective function value of 3.84 when adding one parameter (df = 1) into a nested model was considered significant on the α level of 0.05 (χ 2-distributed).
Next, other clinically plausible covariates were screened by graphical analysis (individual clearance estimates vs. covariate). Covariates with an apparent relationship were subsequently evaluated in a stepwise inclusion (α = 0.05) and exclusion (α = 0.001) procedure (50). Categorical covariates were included as fractional change of clearance. Continuous covariates were modeled as power functions and/or linear functions on clearance, normalized to the population median values of the covariates.
Clinical Impact of Identified Covariates
Deterministic simulations were performed using the selected pharmacokinetic model in order to illustrate the impact of identified covariates on IFX exposure. The simulated dosing regimen was the standard maintenance regimen of 5 mg/kg every 8 weeks. The covariate values used for simulation were selected from the observed distributions of that covariate (median, 5th and 95th percentiles); anti-IFX Abs were assumed to arise at the 3rd IFX infusion for illustration purposes.
RESULTS
Study Population and Serum Samples
The characteristics of the 68 Crohn’s disease patients included for data analysis are detailed in Table I. The numbers of patients on different IFX dosing regimens per visit are depicted in Fig. 2 (left). As a result of the dosing algorithm (Fig. 1), the number of patients on an every 4 weeks regimen decreases over time; these patients either discontinued IFX or returned to longer dosing intervals of IFX. In total, 152 IFX and anti-IFX Abs concentrations (including imputed values) were available for the pharmacokinetics analysis (1–3 samples/patient). The distribution of time after dose of the serum samples is provided in Fig. 2 (right). Of the IFX samples, 21.1% were <LLOQ, out of which 37.5% were anti-IFX Ab+ by HMSA and 31.3% by RGA (21.9% identified by both).
a Number of patients on each IFX dosing regimen at each study visit. “Discontinued” includes patients having discontinued IFX therapy, who are treated with small molecule drugs or no drug therapy but serum samples for IFX and anti-IFX antibodies were collected after discontinuation. “Excluded” includes patients having switched to treatment with another mAb (excluded from 1st dose of new therapy due to assay interferences); loss of follow-up; and one patient with acute infusion reaction. Numbers within brackets below are the total number of patients at each visit included in the present analysis. b–d Number of available samples vs. weeks after last dose: b samples with an IFX concentration above the LLOQ; c samples with an IFX concentration below the LLOQ; d all samples. Color indicates if the sample contained anti-IFX Abs (quantified by homogenous mobility shift assay). As a result of the varying regimens (e.g., IFX discontinuation), samples are available up to 32 weeks after last dose. Abs antibodies, IFX infliximab, LLOQ lower limit of quantification, qXw every X weeks
Pharmacokinetic Model Development
Prior Model
Although reporting different structural models, the two models available in literature showed good agreement, both when compared internally as well as with typical traits of the mAb drug class. The Fasanmade model included body weight as a covariate on all structural parameters, while in the Ternant model it was included on volume of distribution only. For consistency with pharmacokinetics of the mAb drug class and in agreement with allometric scaling principles, the derived prior model was a linear two-compartment drug disposition model with all structural parameters scaled with body weight (BW) with fixed exponents (Eq. 2). Two priors were used for clearance (θpriors). See Supplementary Material for exhaustive comparison and rational of the selection.
The relative standard error for the structural parameters was low (<10%) and the df for the variability parameters was equal to the number of patients in the two prior datasets (692 and 111, respectively), meaning that the prior model can be considered highly informative. When estimating using the prior functionality, the estimates of central and peripheral volumes of distribution (V1, V2), the inter-compartmental clearance (Q), and their respective between-subject variability parameters did not deviate from the original prior parameter values. Consequently, these parameters were fixed during further model development. The estimates of clearance and between-subject variability of clearance were approximately equal to the mean of the two original prior estimates (Table II). See “DISCUSSION” for comments on information content in data.
The goodness-of-fit plots showed overall adequate agreement of predicted and observed IFX concentrations and no notable trend was apparent in the CWRES distribution (Fig. 3). The NPDE distribution was similar to the CWRES (not shown). However, there was a trend in the deviation between individual and typical parameter values (η Clearance) with increasing anti-IFX Ab concentrations (Fig. 4, left). Indeed, a visual predictive check stratified on anti-IFX Ab+/Ab− samples demonstrated that the model under-predicted for anti-IFX Ab− samples and over-predicted for anti-IFX Ab+ samples (Fig. 5, top).
Scatter plots of ln-transformed observations vs. population predictions (a, d) and individual predictions (b, e) as well as CWRES vs. weeks after last dose (c, f), for prior model (a–c) and selected anti-IFX Ab covariate model (d–f), respectively. Inset plots in c and f show the distribution of CWRES. Black line in a, b, d, e—line of identity. Black line in c, f—CWRES = 0. Gray line—median CWRES. Diamond shaped data—one anti-IFX Ab+ patient showing low clearance. It should be noted that only the IFX data above LLOQ can be depicted in these plots. Ab antibody, CWRES conditional weighted residuals, IFX infliximab, LLOQ lower limit of quantification
Scatter plots of random parameters of clearance (η Clearance) vs. total anti-IFX Ab concentration as quantified by homogenous mobility shift assay, for prior model (a) and anti-IFX Ab covariate model (b), respectively. Diamond shaped data—one anti-IFX Ab positive patient showing low clearance. Black line—loess smooth, shaded area—95% confidence interval around smooth. Ab antibody, IFX infliximab
Visual predictive checks for derived prior model (a–d) and anti-IFX Abs covariate model (e–h) stratified by anti-IFX Ab−/Ab+ samples (a, c, e, g vs. b, d, f, h). a, b, e, and f show IFX concentration vs. weeks after last dose. c, d, g, and h show the fraction below the quantification limit. Lines—10th, 50th, and 90th percentiles (blue, observed; black, simulated). Shaded areas—95% confidence interval of the respective percentiles. Anti-IFX Ab + /Ab − anti-drug antibody (positive/negative), BQL below the lower limit of quantification, IFX infliximab
Anti-IFX Ab Covariate Model
All evaluated anti-IFX Ab covariate models (3 models × 2 anti-IFX Ab fractions) improved the prediction of IFX concentrations compared to the fitted prior model (Table II). Comparisons of the mathematical relationships of anti-IFX Abs and clearance (see section “Covariate Model Development” items I-III) revealed similar trends for the two anti-IFX fractions: the anti-IFX Ab concentration provided the best predictor of increased IFX clearance (item III) followed by the fractional change on the sample level (item II) and lastly on the patient level (item I). Comparison of the two different anti-IFX Ab concentrations revealed similar trends for the three mathematical relationships: the total anti-IFX Ab concentration yielded a larger reduction in objective function value as well as better improvement in model evaluation plots as compared to the unbound neutralizing anti-IFX Ab concentration. As expected, the population estimate of clearance was lower in all the anti-IFX Ab covariate models as compared to the prior model since this value represents the entire population in the prior model and the anti-IFX Ab− subgroup in the covariate model. The decreases were larger utilizing the total as compared to the unbound neutralizing anti-IFX concentration.
Taken together, the total anti-IFX Ab concentration most adequately described the observed increase of IFX clearance. The visual predictive checks (Fig. 5, bottom), which also depict the proportion <LLOQ, shows that incorporation of the total anti-IFX Ab concentration largely corrected for the misspecification of the prior model. Moreover, the trend toward more positive η Clearance values with higher anti-IFX Ab concentration is no longer present, with η Clearance values being scattered around zero after inclusion (Fig. 4, right).
Evaluation of Additional Covariates
η-shrinkage in clearance in the selected anti-IFX Ab covariate model was 17%. Graphical screening of covariates (listed in Table I) vs. individual parameters identified the following candidates (in alphabetic order): age; concomitant immunosuppressive therapy; C-reactive protein concentration; disease location; disease duration; luminal vs. fistulizing disease; previous segmental surgery; serum albumin concentration; sex; smoking status; and weeks on IFX therapy. None of these covariates were found to be statistically significant after the backward deletion step.
Consequently, the selected model was a two-compartment disposition model with body weight included according to allometric principles on all structural parameters and total anti-IFX Ab concentration included on clearance (Eq. 3). The residual variability model was additive on the log-scale.
Case deletion diagnostics identified two individuals having high impact on parameter estimates, particularly on the residual variability (decreased if removed). However, the conclusions for the covariate analysis were the same when repeating the estimation without these individuals. As the highest impact was on the residual variability parameter, which is of minor relevance for the research question, the influential individuals were kept for final parameter estimation. Estimation with and without the imputed anti-IFX Ab value for RGA did not affect parameter estimates.
Impact of Identified Covariates
Based on the developed pharmacokinetic model, a total anti-IFX Ab concentration of 12.6 U/mL (=median in dataset) as quantified by HMSA leads to a 60.6% increase of clearance compared to the clearance of IFX in anti-IFX Ab− patients (0.464 vs. 0.289 L/day). The impact of different anti-IFX Ab concentrations on IFX concentrations after the standard dosing of 5 mg/kg every 8 weeks is depicted in Fig. 6.
Simulated IFX concentration-time profiles illustrating the impact of different anti-IFX Ab concentrations (0, 4.06 (5th percentile), 12.6 (median), and 23.5 (95th percentile) U/mL). The dosing regimen is 5 mg/kg infusions every 8 weeks corresponding to the maintenance phase. Ab antibody, IFX infliximab
DISCUSSION
IFX maintenance therapy induces an undesirable immunological reaction, characterized by generation of anti-IFX Abs, in about one third of IBD patients and with similar frequencies in other chronic inflammatory diseases (32). Anti-IFX Abs typically inhibit the binding of IFX to TNFα and can lead to increased IFX clearance, insufficient TNFα inhibition, and ultimately result in treatment failure (5–7,10–14,51,52). Thus far, anti-IFX Abs and their impact on pharmacokinetics have generally been reported as a binary variable according to the detection limit of the assay utilized (4–6,33–35). By combining data collected as part of a randomized clinical trial with prior knowledge of the pharmacokinetics of IFX, this analysis shows that the magnitude of increased IFX clearance relates to the concentration of anti-IFX Abs. Furthermore, this analysis suggests that quantification of total anti-IFX Ab concentration as compared to measurement of the unbound neutralizing anti-IFX Ab fraction alone more accurately identifies high IFX clearance individuals.
The clinical trial forming the basis for this analysis was not designed for pharmacokinetic analysis. The use of previously published population pharmacokinetic models enabled further model development and covariate analysis. Two population pharmacokinetic models of IFX in Crohn’s disease were available in literature (5,37). The present population comprised Crohn’s disease patients who had manifest treatment failure on IFX maintenance therapy and differed from those in the prior models, which were based on patients with moderately to severely active disease and naïve to IFX or patients in remission, respectively. Although differences in disease activity potentially could influence the pharmacokinetics of IFX, the estimates of the reported models were similar (Supplementary Material). Further, the use of a prior allows the parameter values to change with the information from the present data reducing the risk of biased parameter estimates.
In the fitted prior model, parameter estimates for central and peripheral volumes of distribution, the inter-compartmental clearance and their respective between-subject variability parameters did not deviate from the original prior estimates. This indicates that most information for these parameters was provided by the prior models rather than the available data; an expected result since no samples were available early after dose. Clearance and between-subject variability of clearance were estimated approximately to the mean of the two original priors. This could be a result of two equally strong priors and limited information in the data. However, when estimating clearance using one prior at the time, the values deviated from the prior similarly to when using both suggesting that the data do contain information for this parameter (data not shown). Considering the information content of the available data, covariate analysis was only performed on clearance. The impact of anti-IFX Abs was explored before any other covariate because it has been reported to have a large impact (4–6,13,21).
In general, the impact of anti-IFX Abs on drug clearance is intricate to predict, partly due to challenges related to quantification of anti-IFX Abs (22,32). For example, the commonly used bridging enzyme-linked immunosorbent assays cannot detect anti-drug Abs if the mAb is present in the sample (32). Consequently, the anti-IFX Ab status of a serum sample has often been defined as “anti-IFX Ab+,” “anti-IFX Ab−,” or “inconclusive” (11,12,53). This crude classification does not allow for proper characterization of the anti-IFX Ab response and may confound the results (22)—potentially explaining the wide range of reported increase of IFX clearance (1.3–2.7-fold) in anti-IFX Ab+ patients. Recently, newer assays have been developed aiming to deal with this unsatisfactory situation (32,40–42). The anti-IFX Ab samples in the present study were quantified by both HMSA and RGA, providing the “total” concentration (unbound and IFX-bound, neutralizing and non-neutralizing) and the “unbound neutralizing” anti-IFX Ab concentration, respectively (40,41), enabling a more sophisticated evaluation of the impact of anti-IFX Abs on IFX clearance.
Using a population modeling approach, different mathematical relationships as well as data from the two anti-IFX Ab assays were explored to identify the most appropriate prediction of increase in IFX clearance. Consistently for the two anti-IFX Ab assays, the anti-IFX Ab concentration more adequately predicted increased clearance as compared to the binary anti-IFX Ab+/Ab− classifications. Hence, the concentration of anti-IFX Abs appears to play an important role in how large the effect on IFX elimination will be. A similar trend was reported by Zhou et al. showing that higher anti-drug Ab titer correlated with lower concentrations of the mAb AMG317 (anti-drug Ab titer stratified into four groups) (54).
Comparison with respect to the data from the two different anti-IFX Ab assays identified the total anti-IFX Ab concentration as a more accurate descriptor of increased IFX clearance than the unbound neutralizing concentration. This was consistent for the three mathematical relationships. This suggests that quantification of total anti-IFX Ab concentration is important to optimally estimate the impact on IFX clearance and that measurements of unbound neutralizing anti-IFX Abs underestimate this effect. One explanation for this finding could be the lower detection rate of anti-IFX Abs when quantifying the unbound neutralizing concentration as compared to the total (Table I): fewer (high clearance) serum samples were identified as anti-IFX Ab+ (11 vs. 30). However, this randomized controlled study was relatively small, including a total of 152 plasma samples from 68 patients. Thus, the results need to be confirmed in a larger trial, preferably with denser samples for IFX and anti-IFX Ab concentrations. The size of the study could also explain why no additional covariate was found statistically significant. Figure 4 indicates that there is remaining unexplained variability in clearance also in the anti-IFX Ab negative population, which partly could be explained by other factors although not identified in the present analysis. It is important to note that serum albumin concentration, concomitant immunosuppressive medication, and sex may still be of importance as identified in other population pharmacokinetic studies of IFX in IBD (4–6,13,35).
Clinical trials and observational data support switching to a different TNFα inhibitor in order to restore response in patients with treatment failure in the presence of anti-IFX Abs and low IFX concentration (15–20). Several studies have investigated the lower effective concentration threshold for IFX in Crohn’s disease, identifying that a minimal concentration (C min) above 0.5–4.2 μg/mL is associated with response or remission (53,55–57). The present analysis shows that all anti-IFX Ab+ patients in this dataset, irrespectively of their anti-IFX Ab concentration, would be in the risk zone of having C min below these values (Fig. 6). Thus, the model supports the need of a treatment intervention for these patients. It also explains why a switch to another TNF-inhibitor for patients with insufficient effect in the presence of anti-IFX Abs has been shown to be rational from an efficacy, safety, and economic point of view (14,21,58).
The improved characterization of the impact of anti-IFX Ab on IFX clearance provided in this analysis may serve as a stepping stone to explore impact of other sources of variability in the anti-IFX Ab response, such as differences in binding characteristics to the TNFα inhibitor, immunoglobulin (sub)type, or transiency of anti-IFX response. Separate characterization of these mechanisms could in the future extend to more sophisticated recommendations on how to change the therapy for an anti-IFX Ab+ patient in clinical practice.
CONCLUSION
By combining data from a randomized clinical trial with prior knowledge of the pharmacokinetics of IFX, this analysis shows that the magnitude of increase in IFX clearance imposed by anti-IFX Abs closely relates to the concentration of the anti-IFX Abs. However, irrespectively of their concentration, anti-IFX Abs lead to sub-therapeutic IFX concentrations, which support the need of treatment intervention in these patients. Furthermore, quantification of total anti-IFX Ab concentration more accurately identified high clearance individuals in this study as compared to the unbound neutralizing anti-IFX Ab concentration. The developed model can serve as a basis for investigations to further refine recommendations for treatment of anti-IFX Ab+ patients.
Abbreviations
- Ab:
-
Antibody
- Anti-IFX Abs (+/−):
-
Anti-infliximab antibodies (positive/negative)
- IFX:
-
Infliximab
- IBD:
-
Inflammatory bowel disease
- HMSA:
-
Homogenous mobility shift assay
- (>/<) LLOQ:
-
(Above/below) lower limit of quantification
- mAb:
-
Monoclonal antibody
- RGA:
-
Reporter gene assay
- TNFα:
-
Tumor necrosis factor α
References
Dirks NL, Meibohm B. Population pharmacokinetics of therapeutic monoclonal antibodies. Clin Pharmacokinet. 2010;49:633–59. doi:10.2165/11535960-000000000-0000.
Tabrizi MA, Tseng CML, Roskos LK. Elimination mechanisms of therapeutic monoclonal antibodies. Drug Discov Today. 2006;11:81–8. doi:10.1016/S1359-6446(05)03638-X.
Ordás I, Mould DR, Feagan BG, Sandborn WJ. Anti-TNF monoclonal antibodies in inflammatory bowel disease: pharmacokinetics-based dosing paradigms. Clin Pharmacol Ther. 2012;91:635–46. doi:10.1038/clpt.2011.328.
Fasanmade AA, Adedokun OJ, Ford J, Hernandez D, Johanns J, Hu C, et al. Population pharmacokinetic analysis of infliximab in patients with ulcerative colitis. Eur J Clin Pharmacol. 2009;65(12):1211–28. doi:10.1007/s00228-009-0718-4.
Fasanmade AA, Adedokun OJ, Blank M, Zhou H, Davis HM. Pharmacokinetic properties of infliximab in children and adults with Crohn’s disease: a retrospective analysis of data from 2 phase III clinical trials. Clin Ther. 2011;33:946–64. doi:10.1016/j.clinthera.2011.06.002.
Dotan I, Ron Y, Yanai H, Becker S, Fishman S, Yahav L, et al. Patient factors that increase infliximab clearance and shorten half-life in inflammatory bowel disease. Inflamm Bowel Dis. 2014;20:2247–59. doi:10.1097/MIB.0000000000000212.
Nanda KS, Cheifetz AS, Moss AC. Impact of antibodies to infliximab on clinical outcomes and serum infliximab levels in patients with inflammatory bowel disease (IBD): a meta-analysis. Am J Gastroenterol. 2013;108:40–7. doi:10.1038/ajg.2012.363.
De Groot AS, Scott DW. Immunogenicity of protein therapeutics. Trends Immunol. 2007;28:482–90. doi:10.1016/j.it.2007.07.011.
Niebecker R, Kloft C. Safety of therapeutic monoclonal antibodies. Curr Drug Saf. 2010;5:275–86. doi:10.2174/157488610792246055.
Baert F, Noman M, Vermeire S, Van Assche G, D’Haens G, Carbonez A, et al. Influence of immunogenicity on the long-term efficacy of infliximab in Crohn’s disease. N Engl J Med. 2003;348:601–8. doi:10.1056/NEJMoa020888.
Maser EA, Villela R, Silverberg MS, Greenberg GR. Association of trough serum infliximab to clinical outcome after scheduled maintenance treatment for Crohn’s disease. Clin Gastroenterol Hepatol. 2006;4:1248–54. doi:10.1016/j.cgh.2006.06.025.
Seow CH, Newman A, Irwin SP, Steinhart AH, Silverberg MS, Greenberg GR. Trough serum infliximab: a predictive factor of clinical outcome for infliximab treatment in acute ulcerative colitis. Gut. 2010;59:49–54. doi:10.1136/gut.2009.183095.
Dreesen E, Vande Casteele N, Tops S, Vermeire S, Gils A. Anti-drug antibodies, low serum albumin and high C-reactive protein increase infliximab clearance in patients with inflammatory bowel disease: a population pharmacokinetic study of the TAXIT trial. PAGE 25. 2016 Abstr 5873. www.page-meeting.org/?abstract=5873 Accessed 01 Jul 2016.
Steenholdt C, Svenson M, Bendtzen K, Thomsen OØ, Brynskov J, Ainsworth MA. Severe infusion reactions to infliximab: aetiology, immunogenicity and risk factors in patients with inflammatory bowel disease. Aliment Pharmacol. 2011;34:51–8. doi:10.1111/j.1365-2036.2011.04682.x.
Bendtzen K, Ainsworth MA, Steenholdt C, Thomsen OØ, Brynskov J. Individual medicine in inflammatory bowel disease: monitoring bioavailability, pharmacokinetics and immunogenicity of anti-tumour necrosis factor-alpha antibodies. Scand J Gastroenterol. 2009;44:774–81. doi:10.1080/00365520802699278.
Afif W, Loftus EV, Faubion WA, Kane SV, Bruining DH, Hanson KA, et al. Clinical utility of measuring infliximab and human anti-chimeric antibody concentrations in patients with inflammatory bowel disease. Am J Gastroenterol. 2010;105:1133–9. doi:10.1038/ajg.2010.9.
Velayos F, Kahn J, Sandborn W, Feagan B. A test-based strategy is more cost effective than empiric dose escalation for patients with Crohn’s disease who lose responsiveness to infliximab. Clin Gastroenterol Hepatol. 2013;11:654–66. doi:10.1016/j.cgh.2012.12.035.
Steenholdt C, Brynskov J, Thomsen OØ, Munck LK, Fallingborg J, Christensen LA, et al. Individualised therapy is more cost-effective than dose intensification in patients with Crohn’s disease who lose response to anti-TNF treatment: a randomised, controlled trial. Gut. 2014;63:919–27. doi:10.1136/gutjnl-2013-305279.
Steenholdt C, Brynskov J, Thomsen OØ, Munck L, Fallingborg J, Christensen L, et al. Individualized therapy is a long-term cost-effective method compared to dose intensification in Crohn’s disease patients failing infliximab. Dig Dis Sci. 2015;60:2762–70. doi:10.1007/s10620-015-3581-4.
Yanai H, Lichtenstein L, Assa A, Mazor Y, Weiss B, Levine A, et al. Levels of drug and antidrug antibodies are associated with outcome of interventions after loss of response to infliximab or adalimumab. Clin Gastroenterol Hepatol. 2015;13:522–30. doi:10.1016/j.cgh.2014.07.029.
Steenholdt C, Bendtzen K, Brynskov J, Ainsworth MA. Optimizing treatment with TNF-inhibitors in inflammatory bowel disease by monitoring drug levels and anti-drug antibodies. Inflamm Bowel Dis. 2016. doi: 10.1097/MIB.0000000000000772.
Shankar G, Arkin S, Cocea L, Devanarayan V, Kirshner S, Kromminga A, et al. Assessment and reporting of the clinical immunogenicity of therapeutic proteins and peptides-harmonized terminology and tactical recommendations. AAPS J. 2014;16:658–73. doi:10.1208/s12248-014-9599-2.
Ungar B, Chowers Y, Yavzori M, Picard O, Fudim E, Har-Noy O, et al. The temporal evolution of antidrug antibodies in patients with inflammatory bowel disease treated with infliximab. Gut. 2014;63:1258–64. doi:10.1136/gutjnl-2013-305259.
Steenholdt C, Al-khalaf M, Brynskov J, Bendtzen K, Thomsen OØ, Ainsworth MA. Clinical implications of variations in anti-infliximab antibody levels in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2012;18:2209–17. doi:10.1002/ibd.22910.
Steenholdt C, Frederiksen MT, Bendtzen K, Ainsworth MA, Thomsen OØ, Brynskov J. Time course and clinical implications of development of antibodies against adalimumab in patients with inflammatory bowel disease. J Clin Gastroenterol. 2015;50:483–9. doi:10.1097/MCG.0000000000000375.
Steenholdt C, Bendtzen K, Brynskov J, Thomsen OØ, Munck LK, Christensen LA, et al. Changes in serum trough levels of infliximab during treatment intensification but not in anti-infliximab antibody detection are associated with clinical outcomes after therapeutic failure in Crohn’s disease. J Crohn’s Colitis. 2015;9:238–45. doi:10.1093/ecco-jcc/jjv004.
Vande Casteele N, Gils A, Singh S, Ohrmund L, Hauenstein S, Rutgeerts P, et al. Antibody response to infliximab and its impact on pharmacokinetics can be transient. Am J Gastroenterol. 2013;108:962–71. doi:10.1038/ajg.2013.12.
Steenholdt C. Transient and persistent antibodies against TNF-inhibitors in IBD. Am J Gastroenterol. 2015;110:1623–4. doi:10.1038/ajg.2015.325.
Chirmule N, Jawa V, Meibohm B. Immunogenicity to therapeutic proteins: impact on PK/PD and efficacy. AAPS J. 2012;14:296–302. doi:10.1208/s12248-012-9340-y.
U.S. Food and Drug Administration, Center for Drug Evaluation and Research and Center for Biologics Evaluation and Research. Guidance for industry: immunogenicity assessment for therapeutic protein products. 2014. http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM338856.pdf. Accessed 01 Jul 2016.
Butler JE, Feldbush TL, McGivern PL, Stewart N. The enzyme-linked immunosorbent assay (ELISA): a measure of antibody concentration or affinity? Mol Immunol. 1978;15:131–6. doi:10.1016/0161-5890(78)90053-6.
Vincent FB, Morand EF, Murphy K, Mackay F, Mariette X, Marcelli C. Antidrug antibodies (ADAb) to tumour necrosis factor (TNF)-specific neutralising agents in chronic inflammatory diseases: a real issue, a clinical perspective. Ann Rheum Dis. 2013;72:165–78. doi:10.1136/annrheumdis-2012-202545.
Xu Z, Seitz K, Fasanmade A, Ford J, Williamson P, Xu W, et al. Population pharmacokinetics of infliximab in patients with ankylosing spondylitis. J Clin Pharmacol. 2008;48:681–95. doi:10.1177/0091270008316886.
Ternant D, Aubourg A, Magdelaine-Beuzelin C, Degenne D, Watier H, Picon L, et al. Infliximab pharmacokinetics in inflammatory bowel disease patients. Ther Drug Monit. 2008;30:523–9. doi:10.1097/FTD.0b013e318180e300.
Buurman DJ, Maurer JM, Keizer RJ, Kosterink JG, Dijkstra G. Population pharmacokinetics of infliximab in patients with inflammatory bowel disease: potential implications for dosing in clinical practice. Aliment Pharmacol Ther. 2015;42:529–39. doi:10.1111/apt.1329.
Gobburu JV. Pharmacometrics 2020. J Clin Pharmacol. 2010;50:151S–7. doi:10.1177/009127001037697.
Ternant D, Berkane Z, Picon L, Gouilleux-Gruart V, Colombel JF, Allez M, et al. Assessment of the influence of inflammation and FCGR3A genotype on infliximab pharmacokinetics and time to relapse in patients with Crohn’s disease. Clin Pharmacokinet. 2015;54:551–62. doi:10.1007/s40262-014-0225-3.
Gisleskog PO, Karlsson MO, Beal SL. Use of prior information to stabilize a population data analysis. J Pharmacokinet Pharmacodyn. 2002;29:473–505. doi:10.1023/A:1022972420004.
Beal S, Sheiner LB, Boeckmann A, Bauer RJ. NONMEM user’s guides (1989–2009). Ellicott City: Icon Development Solutions; 2009.
Lallemand C, Kavrochorianou N, Steenholdt C, Bendtzen K, Ainsworth MA, Meritet J-F, et al. Reporter gene assay for the quantification of the activity and neutralizing antibody response to TNFα antagonists. J Immunol Methods. 2011;373:229–39. doi:10.1016/j.jim.2011.08.022.
Wang SL, Ohrmund L, Hauenstein S, Salbato J, Reddy R, Monk P, et al. Development and validation of a homogeneous mobility shift assay for the measurement of infliximab and antibodies-to-infliximab levels in patient serum. J Immunol Methods. 2012;382:177–88. doi:10.1016/j.jim.2012.06.002.
Steenholdt C, Bendtzen K, Brynskov J, Thomsen OØ, Ainsworth MA. Clinical implications of measuring drug and anti-drug antibodies by different assays when optimizing infliximab treatment failure in Crohn’s disease: post hoc analysis of a randomized controlled trial. Am J Gastroenterol. 2014;109:1055–64. doi:10.1038/ajg.2014.106.
Edlund H, Melin J, Parra-Guillen ZP, Kloft C. Pharmacokinetics and pharmacokinetic—pharmacodynamic relationships of monoclonal antibodies in children. Clin Pharmacokinet. 2015;54:35–80. doi:10.1007/s40262-014-0208-4.
Ahn JE, Karlsson MO, Dunne A, Ludden TM. Likelihood based approaches to handling data below the quantification limit using NONMEM VI. J Pharmacokinet Pharmacodyn. 2008;35:401–21. doi:10.1007/s10928-008-9094-4.
Bergstrand M, Karlsson MO. Handling data below the limit of quantification in mixed effect models. AAPS J. 2009;11:371–80. doi:10.1208/s12248-009-9112-5.
Holford N. The Visual predictive check—superiority to standard diagnostic (Rorschach) plots. PAGE 14 2005 Abstr 738. www.page-meeting.org/?abstract=738.
Keizer RJ, Karlsson MO, Hooker A. Modeling and simulation workbench for NONMEM: tutorial on Pirana, PsN, and Xpose. CPT Pharmacometrics Syst Pharmacol. 2013;2:e50. doi:10.1038/psp.2013.24.
R Core Team. A language and environment for statistical computing. Vienna, Austria; 2015. http://www.r-project.org/.
Wickham H. ggplot2: elegant graphics for data analysis. New York: Springer; 2009.
Wählby U, Jonsson EN, Karlsson MO. Comparison of stepwise covariate model building strategies in population pharmacokinetic-pharmacodynamic analysis. AAPS PharmSci. 2002;4:68–79. doi:10.1208/ps040427.
Garces S, Demengeot J, Benito-Garcia E. The immunogenicity of anti-TNF therapy in immune-mediated inflammatory diseases: a systematic review of the literature with a meta-analysis. Ann Rheum Dis. 2013;72:1947–55. doi:10.1136/annrheumdis-2012-202220.
Ben-Horin S, Yavzori M, Katz L, Kopylov U, Picard O, Fudim E, et al. The immunogenic part of infliximab is the F(ab′)2, but measuring antibodies to the intact infliximab molecule is more clinically useful. Gut. 2011;60:41–8. doi:10.1136/gut.2009.201533.
Reinisch W, Colombel JF, Sandborn WJ, Mantzaris GJ, Kornbluth A, Adedokun OJ, et al. Factors associated with short- and long-term outcomes of therapy for Crohn’s disease. Clin Gastroenterol Hepatol. 2015;13:539–47. doi:10.1016/j.cgh.2014.09.031.
Zhou L, Hoofring SA, Wu Y, Vu T, Ma P, Swanson SJ, et al. Stratification of antibody-positive subjects by antibody level reveals an impact of immunogenicity on pharmacokinetics. AAPS J. 2012;15:30–40. doi:10.1208/s12248-012-9408-8.
Vande Casteele N, Khanna R, Levesque BG, Stitt L, Zou GY, Singh S, et al. The relationship between infliximab concentrations, antibodies to infliximab and disease activity in Crohn’s disease. Gut. 2014. doi:10.1136/gutjnl-2014-307883.
Levesque BG, Greenberg GR, Zou G, Sandborn WJ, Singh S, Hauenstein S, et al. A prospective cohort study to determine the relationship between serum infliximab concentration and efficacy in patients with luminal Crohn’s disease. Aliment Pharmacol Ther. 2014;39:1126–35. doi:10.1111/apt.12733.
Steenholdt C, Bendtzen K, Brynskov J, Thomsen OØ, Ainsworth MA. Cut-off levels and diagnostic accuracy of infliximab trough levels and anti-infliximab antibodies in Crohn’s disease. Scand J Gastroenterol. 2011;46:310–8. doi:10.3109/00365521.2010.536254.
Feuerstein JD, Cullen G, Cheifetz AS. Immune-mediated reactions to anti-tumor necrosis factors in inflammatory bowel disease. Inflamm Bowel Dis. 2015;21:1176–86. doi:10.1097/MIB.0000000000000279.
Acknowledgments
The authors would like to thank Eurodiagnostica (Malmö, Sweden) and Prometheus Laboratories Inc. (San Diego, CA, USA).
Author information
Authors and Affiliations
Corresponding author
Additional information
Helena Edlund and Casper Steenholdt contributed equally to this work.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 657 kb)
Rights and permissions
About this article
Cite this article
Edlund, H., Steenholdt, C., Ainsworth, M.A. et al. Magnitude of Increased Infliximab Clearance Imposed by Anti-infliximab Antibodies in Crohn’s Disease Is Determined by Their Concentration. AAPS J 19, 223–233 (2017). https://doi.org/10.1208/s12248-016-9989-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1208/s12248-016-9989-8