Abstract
Background
A minimally invasive treatment for vertebral compression fractures is vertebroplasty. In spite of its relative safety, complications have been reported. It is a relatively uncommon complication among these that patients experience massive cement pulmonary embolism. Polymethyl methacrylate (PMMA) can cause embolization in the pulmonary arteries. One of the most common cements used in vertebroplasty is PMMA, a type of acrylic cement. Pulmonary cement embolism can occur if cement leaks into the perivertebral veins and then the pulmonary arteries (Barbero et al., Radiol Med 113:101–13, 2008). Occasionally, the patient will show no symptoms at all, while other times they will experience dyspnea, chest pain, or acute respiratory distress syndrome. A 54-year-old male who underwent vertebroplasty developed pulmonary cement embolism is the patient in our case report.
Case presentation
A 54-year-old male had complaints of breathlessness for 1 week and left lower limb and lower back pain associated with swelling of the lower limbs for 20 days. The patient is an operated case of osteoporotic compression fractures of D6, D11, L1, L3, and L5 vertebroplasty 3 years back. Subsequently, computed tomography pulmonary angiography was performed and diagnosed with partial embolization of the distal peripheral branches of the bilateral pulmonary arteries by the vertebroplasty material.
Conclusion
Vertebroplasty and kyphoplasty are the most prevalent procedures used to inject bone cement (PMMA) into the vertebral column in order to treat osteoporosis. With vertebroplasty, the possibility of embolization increases. In vertebral osteoporosis, the primary advantage is a reduction in pain and vertebral body collapse. Pulmonary cement embolization causes chest discomfort and shortness of breath. Sometimes, acute respiratory distress syndrome is present (Yoo et al., Spine (Phila Pa 1976) 29:E294–7, 2004). After the operation, these symptoms rarely arise. Symptoms often appear weeks, months, or years after the surgery (Habib et al., Heart Lung 41:509-11, 2012). Through this case report, we discuss the complication following vertebroplasty and their management guidelines.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Vertebroplasty and kyphoplasty, two percutaneous methods that use vertebral cement to treat vertebral fracture pain, particularly osteoporotic fractures, have grown in popularity [1]. Percutaneous vertebroplasty risks include pulmonary cement embolism. More than 70% of patients leak extravertebral cement material (PMMA) into the epidural space and perivertebral tissue, but most have no symptoms and can only be detected by advanced imaging studies like HRCT or CT angiography. The perivertebral veins carry PMMA cement into the pulmonary vasculature, causing pulmonary cement embolism. We report the case of a 54-year-old male who presented with breathlessness and lower limb pain—diagnosed with pulmonary cement embolism—and also perform a short review of literature.
Case presentation
This is a case report of 54-year-old male who presented with breathlessness for 1 week and left lower limb pain associated with swelling for 20 days. The patient was operated for osteoporotic compression fractures involving D6, D11, L1, L3, and L5 vertebrae 3 years back. At the time of procedure of the D6 vertebra, there was leakage of cement into the spinal canal leading to left lower limb paralysis 3 years back, and subsequently, he recovered.
General examination revealed a heart rate, blood pressure, oxygen saturation, and blood sugar levels within normal range. On local examination of the bilateral lower limbs, there is diffuse swelling in the left lower leg region with redness on the anterior part of distal leg region. On palpation, diffuse tenderness was noted. On respiratory assessment, bilateral vesicular breath sounds were heard. On routine hematological investigations, total leucocyte count is mildly increased (13,400), and platelet count, prothrombin time, and INR are within normal range.
Chest radiograph PA revealed multiple linear radiodensities involving bilateral lung fields. Vertebroplasty cement is noted along the thoracic vertebral levels (Fig. 1).
Computed tomography whole spine and magnetic resonance lower thoracic and lumbosacral spine were performed which revealed vertebroplasty cement in multiple levels extending in the anterior and bilateral antero-lateral epidural space from the D10-11 to the L5-S1 intervertebral levels without causing any significant compression of the spinal cord/traversing nerve roots, along the bilateral (R > L) neural foramen, D12-L1, L1-2, L2-3, and L3-4, and right neural foramen of the L5-S1 levels abutting the exiting nerve roots. It is also noted extending inferiorly along the prevertebral space at the level of the L3 vertebra and L3-4 inter-vertebral level abutting the aorta posteriorly and extending in the left paravertebral region at the D11 vertebral level.
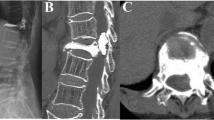
There is evidence of marked loss of the D6 vertebral height with posterior displacement vertebroplasty cement in the anterior and posterior spinal subarachnoid/epidural space opposite the D6 vertebra and D6-D7 intervertebral disc causing significant compression of the thoracic spinal cord with resultant myelomalacia (from the D5-6 to D9-10 intervertebral levels). Additionally, there is marked loss of the height of the D11 vertebral body with horizontal fracture and posterior cortex of the D11 vertebra abutting the spinal cord without any significant compression. There was fracture of the anterior column and inferior endplate of the D12 vertebra with anterior vacuum phenomenon and marrow edema (Figs. 2 and 3).
A Vertebroplasty cement in multiple levels extending from the D10-11 to the L5-S1 intervertebral levels. B Axial image showing vertebroplasty cement at D11 vertebra extending in the anterior and bilateral antero-lateral epidural space. Marked loss of the height of the T11 vertebral body with horizontal fracture and posterior cortex of the T11 vertebra is abutting the spinal cord
A Sagittal image of whole spine shows marked loss of the D6 vertebral height with posterior displacement vertebroplasty cement in the anterior and posterior spinal subarachnoid/epidural space opposite D6 vertebra and D6-D7 intervertebral disc. Additionally, there is marked loss of the height of the D11 vertebral body with horizontal fracture and posterior cortex of the D11 vertebra and fracture of T12 vertebra. B Axial image of D11 vertebra shows horizontal fracture and posterior cortex fracture
Subsequently, computed tomography pulmonary angiography was advised on CT 128 slice scanner. The scan revealed prominent multiple discrete hyper densities of CT attenuation of more than 1300 HU (attenuation similar to the vertebroplasty cement material) which is seen along the distal peripheral segmental branches of the bilateral pulmonary arteries showing no opacification in post-contrast study. However, the majority of the subsegmental arteries show normal contrast opacification distal to the above-mentioned hyper-densities suggesting partial embolization of the distal peripheral branches of the bilateral pulmonary arteries by the vertebroplasty material which can be most likely due to absorption of the extruded vertebroplasty material from the spinal epidural space (Figs. 4 and 5).
A–D Axial images of CT pulmonary angiography. E, F Sagittal images of CT pulmonary angiography. The images show prominent multiple discrete hyper-densities of CT attenuation more than 1300 HU (attenuation similar to the vertebroplasty cement material) along the distal peripheral segmental branches of the bilateral pulmonary arteries showing no opacification in post-contrast study
Discussion
In 1987, Galibert et al. first described vertebroplasty. Vertebroplasty is a minimally invasive procedure that is most commonly used for treating vertebral compression fractures [2]. It is a type of cement called PMMA, and it is injected percutaneously into the vertebral bodies [3]. Given its inertness, dependability, and lack of toxicity, PMMA, an artificial cement, is frequently used in vertebroplasty procedures [4]. Transpedicular needle placement under fluoroscopic guidance is used to reach the vertebral body marrow space before PMMA injection. Real-time imaging helps position bone needles and distribute PMMA evenly without extravasation. This synthetic cement helps to stabilize the vertebral body, which in turn relieves pain in most cases. It is important that the cement in the front two thirds of the vertebral body be evenly distributed and provides support for the structure [5]. Higher cement volumes lead to stronger post-procedural vertebral bodies but increase cement extravasation. In order to achieve the bone-strengthening qualities while preventing cement extravasation sequela, the primary difficulty of vertebroplasty is to administer the precise amount of cement in the exact anatomical site.
Vertebroplasty does have a few extremely unusual hazards despite its well-established safety and universally acknowledged effectiveness.
According to the literature, complications happen between 1 and 10% of the time [6, 7]. Major consequences are uncommon, although the majority of complications are local, including fractures, infection, discomfort, aggravation, bleeding at the puncture site, temporary radiculopathy, and cement leaking. Less than 1% of individuals with osteoporotic vertebral collapse experience major adverse events, with cement extravasation being the most frequent consequence, accounting for 30–65% of those patients’ difficulties [8, 9]. Serious consequences may result from cement spills. For instance, spinal extravasation can cause damage to the intervertebral disc, paravertebral soft tissue, and the spinal cord. Cardiac and pulmonary cement embolization may result from venous extravasation into the epidural and spinal veins.
This case report demonstrates a rare but possibly serious PMMA vertebroplasty complication—cement pulmonary embolism. Accidental needle placement into the basivertebral vein causes extravasation. The cement enters the inferior vena cava, vena radicularis magna, azygos vein, and auxiliary hemiazygos vein through the right heart chambers [10]. Overfilling the vertebral body (9–15 mL), high injection pressure, utilizing low-viscosity PMMA with insufficient polymerization, and several injection levels aggravate cement venous migration [11]. PMMA embolus causes vertebral collapse, cortical damage, and enhanced vascularity. In addition, it is important to consider the operator’s experience, abnormal vascular anatomy, and the absence of biplane fluoroscopy.
Although most PCEs are asymptomatic, dyspnea is the most prevalent symptom [12]. Moreover, tachypnea, tachycardia, cyanosis, chest pain, coughing up blood, hemoptysis, and sweating have all been reported as causes of death after vertebroplasty [13]. High-density artery marks on a chest X-ray suggest PCE. X-rays may show tubular or branching emboli. Most clinicians prefer CT scans for their greater detail. Cement emboli have radio densities over 1000 HU on CT scans, distinguishing them from thrombotic emboli [14]. Patients who have symptomatic emboli or numerous emboli can benefit from echocardiography as an aid in the diagnosis of pulmonary hypertension. The tests that evaluate respiratory function may reveal decreased CO2 lung diffusion in some patients. Despite the potential severity of pulmonary consequences, cement pulmonary emboli have no clear management guidelines, and the few available treatment options lack any supporting scientific data.
Conclusions
Despite the fear of pulmonary PMMA emboli, most patients are safe, asymptomatic, and only need clinical follow-up. Overall mortality from a PMMA embolus is less than 1% [15]. However, long-term effects like “benign” small peripheral emboli causing persistent pulmonary hypertension are unknown. The location, size, and severity of the embolus and symptoms determine the treatment options for symptomatic patients. For central and peripheral emboli, heparinization and warfarin are recommended similar to thromboembolism therapy. Surgery and embolectomy are only recommended in exceptional cases of large central pulmonary emboli.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- PMMA:
-
Polymethyl methacrylate
References
Boonen S, Wahl DA, Nauroy L, Brandi ML, Bouxsein ML, Goldhahn J et al (2011) Balloon kyphoplasty and vertebroplasty in the management of vertebral compression fractures. Osteoporos Int 22:2915–2934
Galibert P, Deramond H, Rosat P, Le Gars D (1987) Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty. Neurochirurgie 33(2):166–168
Winking M, Stahl J-P, Oertel M, Schnettler R, Böker D-K (2003) PMMA vertebroplasty in patients with malignant vertebral destruction of the thoracic and lumbar spine. Ger Med Sci 1:Doc08
Mousa WF, Kobayashi M, Shinzato S, Kamimura M, Neo M, Yoshihara S, Nakamura T (2000) Biological and mechanical properties of PMMA-based bioactive bone cements. Biomaterials 21(21):2137–2146
Kandarpa K, Machan L, Durham JD (2016) Handbook of interventional radiologic procedures Wolters Kluwer. Philadelphia 5:1445–1460
Khan M, Terk M (2009) Cement pulmonary embolus complicating percutaneous vertebroplasty. Radiol Case Rep 4:282
Cotton A, Boutry N, Cortet B et al (1998) Percutaneous vertebroplasty: state of the art. Radiographics 18:311–322
Nussbaum DA, Gailloud P, Murphy K (2004) A review of complications associated with vertebroplasty and kyphoplasty as reported to the Food and Drug Administration medical device related web site. J Vasc Interv Radiol 15:1185–1192
Righini M, Sekoranja L, Le Gal G et al (2006) Pulmonary cement embolism after vertebroplasty. Thromb Haemost 95:388–389
Abdul-Jalil Y, Bartels J, Alberti O et al (2007) Delayed presentation of pulmonary polymethylmethacrylate emboli after percutaneous vertebroplasty. Spine 32:E589–E593
Giraldo WA, Riazuelo JR, Rivera JI et al (2013) Cement pulmonary embolism after vertebroplasty. Reumatol Clin 9:239–242
Toru U, Coskun T, Acat M, Onaran H, Gul S, Cetinkaya E (2014) Pulmonary cement embolism following percutaneous vertebroplasty. Case Rep Pulmonol 2014:851573
Krueger A, Bliemel C, Zettl R, Ruchholtz S (2009) Management of pulmonary cement embolism after percutaneous vertebroplasty and kyphoplasty: a systematic review of the literature. Eur Spine J 18(9):1257–1265
Botia Gonzalez CM, Hernandez Sanchez L, Plasencia Martinez JM (2017) Cement pulmonary embolism. Am J Med Sci 353(5):507
Gangi A, Guth S, Imbert JP et al (2003) Percutaneous vertebroplasty: indications, technique, and results. Radiographics 23:e10
Acknowledgements
Not applicable.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
T.K and M. K diagnosed and helped H.K. in writing and drafting the article and finalizing it. H. K and A.D. drafted and wrote the article. T. K, M. K, and V. S critically revised the article with important conceptual and editorial input. All authors have read and approved the manuscript.
Authors’ information
Not applicable.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical clearance was waived by the Institutional Review Board, in view of the article being a case report. The board recommended only patient consent.
Consent for publication
Informed, full, free, and voluntary verbal and written consent was provided by the patient for the entire process of publication and sharing of images and data.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kalekar, T., Kumar, M.K., Dahiya, A. et al. Pulmonary cement embolism: a complication following vertebroplasty - a case report with brief review of literature. Egypt J Bronchol 17, 28 (2023). https://doi.org/10.1186/s43168-023-00202-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43168-023-00202-9