Abstract
Objectives
Adult-onset Still’s disease (AOSD) is a rare systemic inflammatory disorder. Diagnosing AOSD can be challenging, as disease presentation and clinical course are highly heterogeneous. For unclear reasons, a few patients develop life-threatening complications. Our objective was to determine whether these cases resulted from therapeutic delay or could represent a peculiar AOSD subset.
Methods
We conducted a multicentre retrospective study of 20 AOSD patients with organ failure requiring intensive care unit admission and 41 control AOSD patients without organ failure. Clinico-biological data at hospital admission were explored using supervised analyses and unsupervised dimension reduction analysis (factor analysis of mixed data, FAMD).
Results
Disease duration before admission was shorter in patients with life-threatening AOSD (median, 10 vs 20 days, p = 0.007). Disease duration before AOSD therapy initiation also tended to be shorter (median, 24 vs 32 days, p = 0.068). Despite this shorter disease duration, FAMD, hierarchical clustering and univariate analyses showed that these patients exhibited distinctive characteristics at first presentation, including younger age; higher frequency of splenomegaly, liver, cardiac and/or lung involvement; less frequent arthralgia; and higher ferritin level. In multivariate analysis, 3 parameters predicted life-threatening complications: lack of arthralgia, younger age and shorter time between fever onset and hospitalisation.
Conclusion
This study suggests that life-threatening complications of AOSD occur very early, in a peculiar subset, which we propose to name catastrophic adult-onset Still’s disease (CAOSD). Its exact burden may be underestimated and remains to be clarified through large multicentre cohorts. Further studies are needed to identify red flags and define the optimal therapeutic strategy.
Similar content being viewed by others
Introduction
Adult-onset Still’s disease (AOSD) is a rare systemic inflammatory disorder of unknown aetiology. AOSD typically affects previously healthy young adults and presents with high-grade fever, evanescent rash, sore throat, arthromyalgia, arthritis, serositis, discrete lymphadenopathy, hepato-splenomegaly, neutrophilic leukocytosis, hepatic cytolysis and high serum ferritin [1].
There is no single biological or pathological finding specific for AOSD. Thus, differential diagnosis can be broad (infection, malignancy, autoimmunity, etc.), depending on the patient’s presentation. AOSD is an experience-based diagnosis but several useful diagnostic criteria have been reported [2,3,4]. The modified Yamaguchi and Fautrel criteria provide high sensitivity and specificity [4]. Most studies on AOSD prognosis have focused on the long-term disease course, which can be monocyclic, polycyclic and/or complicated by a chronic erosive polyarthritis [5,6,7,8]. A few patients develop organ complications that can be life-threatening, but little is known about this subgroup of patients. In Europe and North America, the overall mortality rate is classically 0 to 3%, but two recent retrospective series from Korea and Italy reported a concerning disease-related mortality in AOSD (18.7% and 16%, respectively) [9, 10].
We recently reported the analysis of a multicentre series of patients requiring intensive care unit (ICU) admission due to AOSD-related organ failure [11]. Strikingly, these complications mostly occurred during the first AOSD flare, in patients admitted to hospital because of fever of unknown origin, who developed secondary histiocytic lympho-histiocytosis (sHLH), shock, cardiac failure, respiratory distress, coagulopathy, severe hepatitis, or even multiorgan failure (MOF) before the diagnosis of AOSD was eventually made. Thus, we propose to refer to these cases as catastrophic adult-onset Still disease (CAOSD). Most cases exhibited significant diagnostic and therapeutic inertia, and 2 had a fatal outcome.
The objectives of the present study were, firstly, to assess whether CAOSD is the consequence of therapeutic delay or could represent a peculiar disease subset and, secondly, to identify simple red flags, i.e. characteristics that could indicate a risk of life-threatening complications in AOSD.
Patients and methods
Study population and data collection
The CAOSD group included 20 patients from a recently reported multicentre case series [11]. These patients were admitted to an ICU between 1997 and 2014 due to AOSD. Inclusion criteria were (i) admission to ICU due to AOSD-related organ failure; (ii) AOSD diagnosis fulfilling the Yamaguchi [2] and/or Fautrel [3] criteria; (iii) exclusion of differential diagnoses, including infection, malignancy and other systemic immune-mediated disorders; (iv) age at AOSD diagnosis > 18 years; and (v) organ failure requiring organ supporting therapeutic intervention, including vasopressor agents, pericardial drainage, mechanical ventilation, renal replacement therapy (RRT) or plasmatherapy. Exclusion criteria were ICU admission without organ failure or for reasons other than AOSD. Key features of CAOSD are reported in Table 1. A control group was recruited, comprising 41 AOSD patients admitted to Nantes University Hospital during a similar period (2000–2015) for a first AOSD flare. Inclusion criteria were (i) AOSD diagnosis fulfilling the Yamaguchi [2] and/or Fautrel [3] criteria; (ii) exclusion of differential diagnoses, including infection, malignancy and other systemic immune-mediated disorders; (iii) age at AOSD diagnosis > 18 years; and (iv) absence of organ failure. For both groups, initial clinical data were extracted from charts and collected using a standardised form by one of the investigators (AW). This observational study was performed in accordance with the Declaration of Helsinki, European Union and French ethical regulations (reference methodology MR003: retrospective study of anonymised data with ethics approval waiver).
Statistical analyses
Time from first symptoms to hospital admission, time from admission to AOSD treatment initiation (i.e. NSAID or corticosteroids) and time from first symptoms to AOSD treatment initiation were compared between the 2 groups using the Mann–Whitney test. Survival curves were obtained using the Kaplan–Meier method (GraphPad Prism).
A factor analysis for mixed data (FAMD) was performed on patients’ initial data. FAMD is a principal component method which takes into account both qualitative and quantitative variables [12]. This algorithm of reduction of dimensionality sums up major variance/inertia of the variables and projects it on low-dimension planes, thus permitting easy visual interpretation of the data in a concise fashion. It also reduces the background noise of variables and permits downstream analysis, such as clustering. When missing data occurred, they were imputed by principal component analysis and multiple component analysis for quantitative and qualitative variables, respectively, in order to reduce interpolation bias [13]. Severity status was not included in axis construction. Hierarchical cluster analysis was performed on the FAMD coordinates on the first 5 dimensions, using an ascendant algorithm on the Euclidean distances between points and a Ward link. The optimal number of clusters was determined by the elbow method of the within-cluster sum of square with ascendant hierarchical clustering. Best number of clusters was further automatically confirmed by majority vote among 23 indices (NbClust package). All statistical analyses were performed within R-3.4.9 environment, using the FactoMineR, factoextra and missMDA packages [14, 15].
Univariate analyses were performed using the Mann–Whitney test and Fisher test, for quantitative and qualitative variables, respectively. A multiple logistic regression model was built, using variables with less than 10% of missing data. If variables with missing data were to be included, the prevalence of missing values had to be equally balanced between CAOSD and control cases. A backwise selection of variables was performed. Choice of the best multivariate model was based on maximisation of the Bayesian criterion information (BIC). Statistical testing was bilateral and was considered significant below 0.05.
Results
Catastrophic adult-onset Still disease is not due to therapeutic delay
We first hypothesised that life-threatening complications could occur in AOSD patients that experienced unusual therapeutic delay. First-line therapy was corticosteroids in all CAOSD cases. NSAID was only used in control cases (n = 8, of whom 6 eventually required corticosteroids). The timing of hospital admission and that of AOSD treatment initiation are shown in Fig. 1. We found that disease duration prior to initiation of therapy tended to be shorter in the CAOSD group when compared to the control group (median, 24 [IQR, 14–32] days vs 32 [IQR, 19–64], p = 0.068). The delay between hospital admission and initiation of therapy in the CAOSD group was similar to that in the control group (median, 14 days [IQR, 8–20] vs 13 [IQR, 6–25], p = 0.56), suggesting that life-threatening complications were not due to a lengthier diagnostic work-up. Interestingly, disease duration prior to hospital admission was significantly shorter in the CAOSD group (10 days [IQR, 5–13] vs 20 [IQR, 8–32], p = 0.007), suggesting that these patients had a more acute disease onset.
Timing of hospital admission and treatment initiation in catastrophic (black curve) versus uncomplicated (grey dotted curve) AOSD. Disease duration prior to hospital admission was significantly shorter in the catastrophic AOSD group (upper panel). Delay between hospital admission and initiation of AOSD therapy was similar in both groups (middle panel). Disease duration prior to initiation of AOSD therapy tended to be shorter in catastrophic AOSD patients (lower panel)
Multi-dimensional reduction analysis suggests that CAOSD is a distinct disease subset
Having shown that CAOSD does not result from therapeutic delay, we wanted to determine whether these patients could represent a distinct subset even at the time of hospital admission. All clinical and laboratory variables recorded on admission in both groups, i.e. before patients with CAOSD had developed organ failure, were submitted to FAMD.
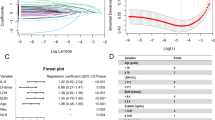
The first five dimensions of FAMD accounted for 47% of the total inertia of the described/dimension-reduced data frame. The first two axes embodied 15.3% and 10.7% of this inertia, respectively (Fig. 2A). An ascendant hierarchical clustering on FAMD coordinates was performed (Fig. 2B). Two clusters were identified, by visual inspection of inertia gain and by automatic selection. Clustering accuracy to distinguish controls and cases, based on FAMD coordinates, was 80%, with a sensitivity of 75% and a specificity of 83% (OR = 13, 95% CI = 3.4–66, p = 2.8E−5). As clearly shown on the first plan of FAMD (Dim1∩Dim2), the two groups of patients were separated, mostly spanning the first axis (Fig. 2A). As detailed in Fig. 3, the variables contributing mostly to the first dimension were C-reactive protein (CRP), blood leukocyte count, splenomegaly, myocarditis and lung infiltrate on one side and age, arthralgia and delay between first symptoms and hospital admission on the other. Overall, these findings are consistent with the hypothesis that even before organ failure CAOSD represents a distinct AOSD subset.
Unsupervised dimension reduction analysis and hierarchical clustering. A Factor analysis on mixed data separates 2 groups along axis 1, with strong concordance with patient severity status (catastrophic AOSD, blue; control cases, red; star, mean point of the group). B Hierarchical clustering identifies 2 clusters. Cluster 2 (black circles) strongly overlaps with catastrophic AOSD cases
Factor analysis on mixed data (FAMD): axis construction. Contribution of quantitative (left panel) and qualitative (right panel) variables to FAMD axis construction. Adenopath., adenopathy; AKI, acute kidney injury; CAOSD, catastrophic adult-onset Still’s disease; Dim, dimension; Eff., effusion; Hepatomeg., hepatomegaly; infil., infiltrate; Splenomeg., splenomegaly
Young age, early referral and lack of arthralgia as potential red flags for life-threatening complications
In order to determine which key parameters could help identify patients at risk of life-threatening complications, univariate and multivariate statistical analyses were performed to compare CAOSD and uncomplicated cases. CAOSD patients were significantly younger than patients with uncomplicated AOSD and had less arthralgia and arthritis; more frequent hepato-splenomegaly, pulmonary and/or cardiological involvement; and a higher heart rate (Table 2); their CRP and ferritin levels were higher. There were no differences between the two groups in terms of rash, sore throat, serositis, blood cell count or liver enzyme levels. As expected, univariate analyses were in strong agreement with FAMD results.
Twenty-three variables were included in the multiple logistic regression analysis. Final key variables were arthralgia, age at diagnosis and time from first symptoms to hospitalisation. Due to a significant interaction between age and time from first symptoms to hospitalisation (ρ = 0.44, p = 6E−4, Pearson), 2 models were built (Table 2), associating arthralgia with either time to hospitalisation (model 1) or age at diagnosis (model 2). Both analyses confirmed that arthralgia was less prevalent in CAOSD than in uncomplicated cases. In the first multivariate model, CAOSD patients were significantly younger than uncomplicated cases. In the second multivariate model, time from first symptoms to hospitalisation was shorter for CAOSD than for uncomplicated AOSD.
Discussion
AOSD is a rare systemic inflammatory disorder of unknown aetiology [16]. Most studies on the prognosis of AOSD focused on the long-term risk of systemic relapse and/or chronic polyarthritis [5,6,7,8]. SJIA and AOSD are currently considered the same diseases at different ages [1]. In the past decade, AOSD has been shown to be a potentially life-threatening disease [9, 10, 17, 18]. As with SJIA, the complication that has attracted most attention is sHLH [9, 10, 19,20,21]. A variety of organ complications can occur, such as myocarditis, cardiac tamponade, respiratory failure and non-cardiogenic shock [1, 17]. We recently reported a multicentre series of 20 patients that required ICU admission due to AOSD complication-related organ failure, and reviewed 79 published cases [11]. Strikingly, complications mostly occurred at disease onset, resulting in a considerable diagnostic delay, with sepsis as the key misleading working hypothesis.
The main objective of the present study was to determine if CAOSD is a consequence of therapeutic delay or could represent a peculiar disease subset. We found that CAOSD patients tended to have a shorter delay between disease onset and AOSD treatment initiation, which was mainly due to a faster referral to the hospital. Both supervised and unsupervised statistical analyses demonstrated that even before organ failure occurred, these AOSD cases that would subsequently become life-threatening had peculiar characteristics, including a younger age and a shorter interval between disease onset and hospital admission. Furthermore, these CAOSD patients exhibited a peculiar phenotype, with more frequent cardio-pulmonary manifestations, hepato-splenomegaly, higher inflammatory markers and less frequent arthralgia and/or arthritis, when compared to other AOSD patients. Interestingly, these findings are reminiscent of how the heterogeneity of AOSD and SJIA has been delineated in recent years, by opposing arthritis on one side to systemic features and/or macrophage activation on the other [22, 23]. Several pro-inflammatory cytokines play a key role in SJIA/AOSD, including TNF-α, IFN-γ, IL-1, IL-6, IL-17 and IL-18. Ten years ago, Gattorno et al. showed that children with SJIA that responded to IL-1 receptor antagonist (anakinra) had less arthritis and higher neutrophilic leucocytosis than others [24]. In 2014, Ichida et al. reported that non-arthritic AOSD patients had more frequent splenomegaly, higher ferritin levels and higher IL-18 level and occasionally suffered organ complications (serositis, acute respiratory distress, sHLH, disseminated intravascular coagulation), which were not seen in arthritic patients [25]. More recently, Shimizu et al. described 2 cytokine profiles in SJIA: the IL-6-dominant subset had more arthritis, whereas the IL-18-dominant one was more susceptible to sHLH [26]. The same group subsequently made similar observations in patients with AOSD, where IL-18-dominant patients had higher ferritin levels but a lower frequency of arthritis as compared to IL-6-dominant patients [27]. A recent study demonstrated how arthritic versus systemic manifestation of AOSD predicted response to IL-6 and IL-1 blockade, respectively [28].
Overall, our data suggest that CAOSD patients, i.e. AOSD patients who develop life-threatening complications at disease onset, represent a distinct clinical subset characterised by a more rapid and more severe systemic inflammatory response syndrome. This life-threatening cytokine storm might be driven mostly by IL-1 and IL-18. Hyperferritinaemia, hepato-splenomegaly and haemophagocytosis also point to macrophage activation as a key driving force of CAOSD. Our finding that these patients are significantly younger suggests that some genetic susceptibility may play a role.
Importantly, the overwhelming majority of patients who developed life-threatening manifestations did so before the diagnosis of AOSD was made [11]. AOSD is a well-known cause of sHLH, an entity most intensivists are more familiar with. However, key manifestations of most malignancy, immunodeficiency and/or infection-related sHLH include cytopenias. By contrast, despite several features are reminiscent of macrophage activation (fever, hyperferritinaemia, hepato-splenomegaly, coagulopathy and haemophagocytosis), CAOSD present with marked neutrophilic leukocytosis with or without moderate anaemia and/or thrombocytopenia, which likely contribute to misguide clinician [11]. Thus, the main area of improvement is to increase awareness of this peculiar entity among non-specialists (hospitalists, intensivists, respiratory physicians, cardiologists, etc.), who have to be aware of CAOSD being a sepsis mimicker in critically ill adult patients with fever of unknown origin (FUO). Despite the diversity of organ complications that CAOSD patients may present with, the overall picture of AOSD, including the simple clues to its diagnosis, remains the classical ones (salmon rash, sore throat, neutrophil leukocytosis, hyperferritinaemia, etc.). Early recognition of those may avoid pointless investigations, diagnostic delay and deaths of young adult patients.
The exact burden of CAOSD remains unclear in recently published series and discrepancies between them suggest that CAOSD may be underdiagnosed in FUO patients presenting with life-threatening complications. In a large retrospective series from an Italian rheumatological network including 245 AOSD patients, no data were available regarding organ manifestations or deaths, and only 7 patients (2.6%) were considered to have sHLH [2]. In a recent nationwide Japanese series, none of the 169 patients had a fatal outcome [29, 30]. In another French series, patients were seen mainly in internal medicine departments and as many as 33% presented with organ complications (with a heterogeneous spectrum, in line with our own observations [7]). Two recent retrospective AOSD series reported an unexpectedly high mortality rate, which suggests better recognition of CAOSD, but that therapeutic management still needs to be improved. Ahn et al. studied 64 Korean patients diagnosed with AOSD at a Seoul Hospital over a 10-year period, of whom 36 (56%) were classified as having sHLH and 12 (18.7%) died [9]. Death occurred within 3 months in all cases (within 1 month in 10 cases), due to AOSD-related multiorgan failure in 8 cases, and superimposed infection in 4. In a recent Italian series of 119 AOSD patients, 19 (16%) patients died due to AOSD: 12 deaths were attributed to AOSD-related sHLH, 5 to AOSD-related MOF and 2 to infection [10]. To date, limited data are available to define the optimum therapeutic strategy beyond corticosteroids. Most published experience reports the promising efficacy of cyclosporin and IL-1 receptor antagonist (anakinra). Intravenous immunoglobulins are an appealing immunomodulatory strategy when infection is a key concern. Unfortunately, they have limited efficacy and may even delay the recourse to more potent therapies [9, 11]. Further studies are needed to clarify the benefit/risk of sHLH-targeting chemotherapy (etoposide) [31], pleiotropic immunosuppressants (e.g. cyclophosphamide) and IL-6 targeted therapies [32] Other candidate drugs will hopefully appear in the near future [32, 33].
Our study has several limitations, owing to its retrospective nature and the rarity of AOSD. Unfortunately, the methodology of case–control collection and the rarity of CAOSD in our single-centre AOSD cohort (5/46, 11%) did not allow us to build a scoring system to predict CAOSD. Thus, the potential red flags we point at should be taken with caution. Another limitation of our study is that we focused on data gathered at first presentation. However, AOSD early clinico-biological course is heterogeneous. Further studies are needed to determine if the dynamics of blood cell counts, liver tests and ferritin levels can predict short-term outcome. Comparing a multicentre case series to a single-centre control group may be a source of bias. However, cases were collected from centres that were very similar to ours (internal medicine department of non-tertiary university or non-teaching hospitals) and 5 were from our own cohort. Further multicentre matched case–controlled studies are warranted to identify red flags for CAOSD.
Conclusion
There is growing evidence that AOSD can lead to life-threatening complications, mainly before the diagnosis is made. Our study shows that these complications are not the consequence of therapeutic delay but occur in a peculiar subset of patients. It should be popularised that AOSD is a great mimicker in FUO patient entering the ICU. Prospective AOSD cohort studies and interdisciplinary approaches may help to quantify the exact burden of CAOSD. Dedicated studies are needed to identify robust red flags and clarify the optimal therapeutic strategy.
Availability of data and materials
The datasets analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AOSD:
-
Adult-onset Still’s disease
- AKI:
-
Acute kidney injury
- ALAT:
-
Alanine aminotransferase
- ASAT:
-
Aspartate aminotransferase
- BIC:
-
Bayesian criterion information
- CAOSD:
-
Catastrophic adult-onset Still’s disease
- CI:
-
Confidence interval
- CRP:
-
C-reactive protein
- FAMD:
-
Factor analysis for mixed data
- FUO:
-
Fever of unknown origin
- ICU:
-
Intensive care unit
- IL:
-
Interleukin
- IQR :
-
Interquartile range
- MOF:
-
Multiorgan failure
- NSAID:
-
Non-steroidal anti-inflammatory drug
- sHLH:
-
Reactive haemophagocytic syndrome
- SJIA:
-
Systemic juvenile idiopathic arthritis
- TNF:
-
Tumour necrosis factor
- IFN:
-
Interferon
References
Feist E, Mitrovic S, Fautrel B. Mechanisms, biomarkers and targets for adult-onset Still’s disease. Nat Rev Rheumatol. 2018;14:603–18.
Yamaguchi M, Ohta A, Tsunematsu T, Kasukawa R, Mizushima Y, Kashiwagi H, et al. Preliminary criteria for classification of adult Still’s disease. J Rheumatol. 1992;19:424–30.
Fautrel B, Zing E, Golmard JL, Le Moel G, Bissery A, Rioux C, et al. Medicine (Baltimore). 2002;81:194–200.
Hamidou MA, Denis M, Barbarot S, Boutoille D, Belizna C, Le Moël G. Usefulness of glycosylated ferritin in atypical presentations of adult onset Still’s disease. Ann Rheum Dis. 2004;63:605.
Wouters JM, van de Putte LB. Adult-onset Still’s disease; clinical and laboratory features, treatment and progress of 45 cases. Q J Med. 1986;61:1055–65.
Pouchot J, Sampalis JS, Beaudet F, Carette S, Décary F, Salusinsky-Sternbach M, et al. Adult Still’s disease: manifestations, disease course, and outcome in 62 patients. Medicine (Baltimore). 1991;70:118–36.
Gerfaud-Valentin M, Maucort-Boulch D, Hot A, Iwaz J, Ninet J, Durieu I, et al. Adult-onset Still disease: manifestations, treatment, outcome, and prognostic factors in 57 patients. Medicine (Baltimore). 2014;93:91–9.
Franchini S, Dagna L, Salvo F, Aiello P, Baldissera E, Sabbadini MG. Efficacy of traditional and biologic agents in different clinical phenotypes of adult-onset Still’s disease. Arthritis Rheum. 2010;62:2530–5.
Ahn SS, Yoo B-W, Jung SM, Lee SW, Park YB, Song JJ. Application of the 2016 EULAR/ACR/PRINTO classification criteria for macrophage activation syndrome in patients with adult-onset Still disease. J Rheumatol. 2017;44:996–1003.
Ruscitti P, Iacono D, Ciccia F, Emmi G, Cipriani P, Grembiale RD, et al. Macrophage activation syndrome in patients affected by adult-onset Still disease: analysis of survival rates and predictive factors in the Gruppo Italiano di Ricerca in Reumatologia Clinica e Sperimentale Cohort. J Rheumatol. 2018;45:864–72.
Néel A, Wahbi A, Tessoulin B, Boileau J, Carpentier D, Decaux O, et al. Diagnostic and management of life-threatening adult-onset Still disease: a French nationwide multicenter study and systematic literature review. Crit Care. 2018;22:88.
Pagès J. Multiple factor analysis by example using R. 1st ed. Boca Raton: Chapman and Hall/CRC Press; 2014. https://doi.org/10.1201/b17700.
missMDA: a package for handling missing values in multivariate data analysis | Josse | Journal of Statistical Software. [cited 2017 Sep 23]; Available from: https://www.jstatsoft.org/article/view/v070i01
Lê S, Josse J, Husson F. FactoMineR: an R package for multivariate analysis. J Stat Softw. 2008;25(1):1–18.
Josse J, Husson F. missMDA: a package for handling missing values in multivariate data analysis. J Stat Softw. 2016;70(1):1–31.
Bywaters EG. Still’s disease in the adult. Ann Rheum Dis. 1971;30:121–33.
Efthimiou P, Kadavath S, Mehta B. Life-threatening complications of adult-onset Still’s disease. Clin Rheumatol. 2014;33:305–14.
Efthimiou P, Paik PK, Bielory L. Diagnosis and management of adult onset Still’s disease. Ann Rheum Dis. 2006;65:564–72.
Lenert A, Yao Q. Macrophage activation syndrome complicating adult onset Still’s disease: a single center case series and comparison with literature. Semin Arthritis Rheum. 2016;45:711–6.
Hot A, Toh ML, Coppéré B, Perard L, Madoux MH, Mausservey C, et al. Reactive hemophagocytic syndrome in adult-onset Still disease: clinical features and long-term outcome: a case-control study of 8 patients. Medicine (Baltimore). 2010;89:37–46.
Bae CB, Jung JY, Kim HA, Suh CH. Reactive hemophagocytic syndrome in adult-onset Still disease: clinical features, predictive factors, and prognosis in 21 patients. Medicine (Baltimore). 2015;94:e451.
Jamilloux Y, Gerfaud-Valentin M, Martinon F, Belot A, Henry T, Sève P. Pathogenesis of adult-onset Still’s disease: new insights from the juvenile counterpart. Immunol Res. 2015;61:53–62.
Colafrancesco S, Priori R, Valesini G. Presentation and diagnosis of adult-onset Still’s disease: the implications of current and emerging markers in overcoming the diagnostic challenge. Expert Rev Clin Immunol. 2015;11:749–61.
Gattorno M, Piccini A, Lasigliè D, Tassi S, Brisca G, Carta S, et al. The pattern of response to anti-interleukin-1 treatment distinguishes two subsets of patients with systemic-onset juvenile idiopathic arthritis. Arthritis Rheum. 2008;58:1505–15.
Ichida H, Kawaguchi Y, Sugiura T, Takagi K, Katsumata Y, Gono T, et al. Clinical manifestations of Adult-onset Still’s disease presenting with erosive arthritis: association with low levels of ferritin and Interleukin-18. Arthritis Care Res. 2014;66:642–6.
Shimizu M, Nakagishi Y, Yachie A. Distinct subsets of patients with systemic juvenile idiopathic arthritis based on their cytokine profiles. Cytokine. 2013;61:345–8.
Inoue N, Shimizu M, Tsunoda S, Kawano M, Matsumura M, Yachie A. Cytokine profile in adult-onset Still’s disease: comparison with systemic juvenile idiopathic arthritis. Clin Immunol. 2016;169:8–13.
Vercruysse F, Barnetche T, Lazaro E, Shipley E, Lifermann F, Balageas A, et al. Adult-onset Still’s disease biological treatment strategy may depend on the phenotypic dichotomy. Arthritis Res Ther. 2019;21:53.
Sfriso P, Priori R, Valesini G, Rossi S, Montecucco CM, D’Ascanio A, et al. Adult-onset Still’s disease: an Italian multicentre retrospective observational study of manifestations and treatments in 245 patients. Clin Rheumatol. 2016;35:1683–9.
Asanuma YF, Mimura T, Tsuboi H, Noma H, Miyoshi F, Yamamoto K, et al. Nationwide epidemiological survey of 169 patients with adult Still’s disease in Japan. Mod Rheumatol. 2015;25:393–400.
La Rosée P, Horne A, Hines M, von Bahr GT, Machowicz R, Berliner N, et al. Recommendations for the management of hemophagocytic lymphohistiocytosis in adults. Blood. 2019;133:2465–77.
Ruscitti P, Ursini F, Cipriani P, De Sarro G, Giacomelli R. Biologic drugs in adult onset Still’s disease: a systematic review and meta-analysis of observational studies. Expert Rev Clin Immunol. 2017;13:1089–97.
Gabay C, Fautrel B, Rech J, Spertini F, Feist E, Kötter I, et al. Open-label, multicentre, dose-escalating phase II clinical trial on the safety and efficacy of tadekinig alfa (IL-18BP) in adult-onset Still’s disease. Ann Rheum Dis. 2018;77:840–7.
Acknowledgements
The authors thank all the additional investigators for their participation in the study:
Ygal Benhamou, Rouen; Odile Beyne-Rauzy, Toulouse; Philippe de Faucal, Nantes; Christophe Guitton, Le Mans; Patrick Jego, Rennes; and Laurent Sailler, Toulouse.
Funding
None
Author information
Authors and Affiliations
Contributions
AW, CB, MH and AN have contributed to the conception and the design of the work. AW, JB, DC, OD, LF, GG, PG, CG, HM, AM, JP and JMZ contributed to the acquisition and interpretation of the data. BT and AN performed the statistical analysis. AW and AN have drafted the manuscript. BT, SGL and MH have revised the manuscript. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This observational study was performed in accordance with the Declaration of Helsinki, European Union and French ethical regulations (reference methodology MR003: retrospective study of anonymised data with ethics approval waiver).
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wahbi, A., Tessoulin, B., Bretonnière, C. et al. Catastrophic adult-onset Still’s disease as a distinct life-threatening clinical subset: case–control study with dimension reduction analysis. Arthritis Res Ther 23, 256 (2021). https://doi.org/10.1186/s13075-021-02631-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13075-021-02631-7