Abstract
Background
Infertility remains a significant public health concern. An issue with controlled ovarian stimulation (COS) is the selection of an exogenous gonadotropin (Gn) regimen, which is mainly based on urinary follicle-stimulating hormone (uFSH), recombinant follicle-stimulating hormone alfa (rFSH-alfa), and human menopausal gonadotropin (HMG). In addition, most previous studies focused on the clinical pregnancy rates or live birth rates (LBR) per transfer cycle, but not on the cumulative live birth rate (CLBR) per started cycle. The CLBR, appears to be a more comprehensive and accurate universal measure of IVF treatment success. Therefore, this study aimed to compare the cumulative live birth rate (CLBR) between rFSH-alfa and uFSH regimens for ovarian stimulation.
Methods
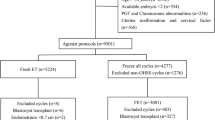
This retrospective cohort study included patients who underwent assisted reproductive technology (ART) with gonadotropin-releasing hormone (GnRH) agonist long protocol between March 2009 and December 2018. Patients were grouped according to the Gn regimen received (rFSH-alfa or uFSH). The main outcome was CLBR, which defined as the first live birth following the use of all fresh and frozen embryos derived from a single COS cycle.
Results
A total of 1078 cycles were analyzed (314 with rFSH-alfa and 764 with uFSH). The rFSH-alfa group was characterized by a higher number of retrieved oocytes (13.3 vs. 11.0) and transferable embryos (5.0 vs. 4.0), a higher fresh embryo transfer rate (35.0% vs. 26.3%), and a higher multiple birth rate among the fresh embryo transfer cycles (8.2% vs. 2.5%) (P < 0.05). There were no differences in pregnancy rate (32.7% vs. 33.8%) and LBR (25.5% vs. 26.9%) per transfer cycle (P > 0.05). No significant difference was found in clinical outcomes among the frozen embryo transfer cycles (P > 0.05). The CLBR per started cycle in the rFSH-alfa group was higher than in the uFSH group (53.5% vs. 43.1%, P < 0.05). After adjustment, rFSH-alfa was independently associated with a higher CLBR (OR = 1.56; 95%CI = 1.18–2.05; P = 0.0018).
Conclusions
rFSH-alfa and uFSH have similar pregnancy rates and LBR per transfer cycle, rFSH-alfa might achieve more transferrable blastocysts and higher CLBR per started cycle compared to uFSH.
Similar content being viewed by others
Introduction
Infertility remains a significant public health concern, affecting about 15% of all couples of reproductive age [1], with a global prevalence of about 50–70 million couples [2]. Since the first in vitro fertilization (IVF) in 1978, assisted reproductive technology (ART) with controlled ovarian stimulation (COS) has become an effective infertility treatment. An issue with COS is about the selection of an exogenous gonadotropin (Gn) regimen, which is mainly based on urinary follicle-stimulating hormone (uFSH), recombinant follicle-stimulating hormone alfa (rFSH-alfa), and human menopausal gonadotropin (HMG) [3]. The European Society of Human Reproduction and Embryology (ESHRE) published a guideline on COS in 2020, with recommendations on Gn [4]. Still, the consensus is based on previous evidence concluding that there is no difference between recombinant and urinary FSH, which is based only on clinical pregnancy rates or live birth rates (LBR) per transfer cycle, but not on the cumulative live birth rate (CLBR) per started cycle [4]. Indeed, there have been many studies comparing clinical pregnancy or LBR per transfer cycle between rFSH-alfa and uFSH [5,6,7,8], but no data related to the CLBR are available.
Outcomes traditionally used to evaluate results of in vitro fertilization, and embryo transfer (IVF-ET) treatment include the number of embryos obtained per IVF cycle, clinical pregnancy rate and LBR per transfer cycle (fresh or frozen cycle, respectively) [9]. Nevertheless, with the widespread use of embryo cryo-resuscitation technology to increase the LBR, the above outcomes are not sufficient to evaluate the clinician’s concern regarding the length of the treatment and relieve the patient’s concern about the number of hospital visits [10]. Therefore, the CLBR, which is defined as the first live birth following the use of all fresh and frozen embryos derived from a single COS cycle, appears to be a more comprehensive and accurate universal measure of IVF treatment success [10,11,12] for both fresh embryo transfer and subsequent frozen-thawed embryo transfer (FET) [13]. Therefore, more and more investigators in recent years have begun to use the CLBR to evaluate the therapeutic effect of IVF, and the recognition of CLBR as the universal outcome and even a “gold standard” continues to expand [10, 14,15,16].
At present, the rFSH-alfa and uFSH are widely used for COS in China [17, 18]. Still, there is a lack of comprehensive evidence comparing the efficacy of COS regimens using these two drugs in China. In addition, despite CLBR recently becoming the gold standard for evaluating the efficacy of COS, there is no large-scale study comparing the CLBRs between rFSH-alfa and uFSH protocols [18].
Therefore, this study aimed to compare the clinical outcomes, particularly CLBR, between rFSH-alfa and uFSH regimens for COS in a real-world setting. The results could provide additional evidence for selecting the most optimal treatment for COS.
Methods
Study design and patients
This retrospective study included patients who underwent ART with COS at the Center for Reproductive Medicine of Subei People’s Hospital of Jiangsu Province from March 2009 to December 2018. STROBE guideline was followed in our preparation. This study was approved by the ethics committee of the Reproductive Medicine of Subei People’s Hospital of Jiangsu Province. Due to the retrospective nature, the need for informed consent was waived by the committee.
The inclusion criteria were 1) underwent gonadotropin-releasing hormone (GnRH) agonist long protocol, including short-acting GnRH agonist long protocol and long-acting GnRH agonist long protocol, 2) received rFSH-alfa or uFSH for COS, 3) ≤2 previous stimulation cycles, and 4) antral follicle count (AFC) ≥5.
COS protocols
The depot GnRH agonist long protocol was used for COS. For the long-acting long protocol, a long-acting agonist analog was given on day 2–3 of menstruation for downregulation, with blood tests for FSH, luteinizing hormone (LH), and estradiol (E2) and a vaginal ultrasound 28–35 days after downregulation to check the status of downregulation. For the short-acting GnRH agonist long protocol, a short-acting agonist analog was given on day 21 of the previous menstrual cycle or 7 days after ovulation of the previous menstrual cycle. Blood was drawn for FSH, LH, and E2, and a vaginal ultrasound was performed on days 2–3 after the return of menstruation to check the status of downregulation. If pituitary down-regulation was confirmed, exogenous Gn was given to initiate COS. The FSH received by patients during the study period included rFSH-alfa (Gonal-F®, Merck Serono, Switzerland) or uFSH (Lizhu Pharmaceutical Trading Co., Zhuhai, China). The Gn initiation dose was 100–225 IU/d for patients with normal ovarian reserve function and 225–300 IU/d for patients with low reserve function. The drug dose was adjusted according to the growth rate of the follicles and hormone levels. During stimulation, the ovarian response was monitored by measuring serum E2, progesterone (P4), and LH and using serial transvaginal ultrasonographic examinations. Recombinant human choriogonadotropin (hCG) was administered until at least one follicle was observed with a diameter of ≥19 mm or two with diameters of ≥18 mm.
Oocyte retrieval occurred 36–40 h after hCG injection (trigger). IVF or ICSI were performed 4–6 h after in vitro culture of the oocyte. ICSI was performed in cases of males with severe oligospermia or azoospermia requiring testicular or epididymal puncture, previous IVF fertilization failure, fertilization rate < 20%, or normal fertilization rate < 30%; otherwise, IVF was performed. A pronucleus was observed 18–20 h after insemination. The Vitrolife serial sequential culture medium was used for embryo culture.
Embryo transfer, luteal support, and follow-up
For patients with high risk of ovarian hyperstimulation syndrome (OHSS), substandard endometrial thickness or morphology, or moderate to severe hydrosalpinx, frozen embryo transfer is recommended; otherwise, fresh embryo transfer will be utilized. Fresh embryo transfer was performed 48 or 72 h after oocyte retrieval using a Cook soft catheter, while FET was performed on the day of thawing or day 1 post-thawing. The greatest endometrial thickness in the uterus’s longitudinal plane in transvaginal ultrasound was measured from one endometrial-myometrium interphase to the corresponding interphase. The measurement recorded on the day of hCG administration was used as the referral value in this study. Pregnancy was first assessed by a positive hCG test 2 weeks after oocyte retrieval and confirmed by ultrasound visualization of an intrauterine gestational sac with an embryo with heartbeats at 6 weeks gestational age.
Data collection and definition
Patients’ information through the electronic medical record (EMR) were retrospectively collected, including baseline data (age, body mass index [BMI], duration of infertility, primary causes of infertility, the previous number of IVF/ICSI cycles, and baseline endocrine information), COS treatment and laboratory embryo culture (Gn total dose, 2PN number, IVF/ICSI, number of transferable embryos, number of high-quality embryos, and number of embryo transfer cycles). Clinical outcomes, including CLBR per started cycle, LBR per transfer cycle, pregnancy rate per transfer cycle, abortion rate, and multiple birth rate, were calculated.
High-quality embryos were defined as grade I and II embryos, based on the size, regularity, refractive index of the cytoplasm, and the number of fragments. Grade I embryos: uniform cell size, regular shape, complete zona pellucida, uniform and clear cytoplasm without granular phenomenon, and fragmentation between 0 and 5%. Grade II embryos: slightly uneven cell size, slightly irregular shape, the cytoplasm may be granular, and fragmentation between 6 and 20%. Grade III embryos: obviously uneven cell size, obviously irregular shape, the cytoplasm may be granular, and fragmentation between 21 and 50%. Grade IV embryos: severely uneven cell size, severely granular cytoplasm, and fragmentation > 50%.
Live birth was defined as the final birth of at least one living child born after 28 weeks of gestation. CLBR was defined as the first live birth following the use of all fresh and frozen embryos derived from a single COS cycle. In cases when all embryos were used up in one embryo retrieval cycle, or if a live birth was not achieved for more than 2 years after ART started, we considered that this embryo retrieval cycle finally did not achieve a live birth. LBR per transfer cycle was calculated as the number of live birth cycles divided by number of transfer cycles. Miscarriage rate was calculated as the number of miscarriage cycles divided by number of clinical pregnancy cycles. Multiple birth rate was calculated as the number of multiple live birth cycles divided by transfer cycles. Clinical pregnancy was defined as a transvaginal ultrasound 4 weeks after transplantation or 2 weeks after a positive hCG blood test indicating a gestational sac in or outside the uterine cavity. Clinical pregnancy rate per transfer cycle was calculated as the number of clinical pregnancies divided by number of transfer cycles.
Statistical analysis
All statistical analyses were performed using Empower Stats (www.empowerstats.com, X&Y solutions, Inc. Boston, MA, USA) and R 3.6.1 (http://www.r-project.org). The continuous variables were tested for normality using the Kolmogorov-Smirnov test. The data complying with a normal distribution were presented as means ± standard deviations; otherwise, they were expressed as medians (25th–75th percentile). Categorical variables were expressed as the number of cases (percentage). The data between the two groups were compared and analyzed using non-parametric tests or the chi-square test, as appropriate. A logistic regression model was used to assess the relationship between FSH regimens and CLBR after adjusting for age, BMI, baseline FSH, and AFC. We selected confounders based on the associations reported with the outcomes of interest [6, 14,15,16]. A 1:2 propensity score matching (PSM) was also used to balance factors, including age, BMI, basic FSH, and AFC. Two-tailed P < 0.05 was considered statistically significant.
Results
General characteristics of the patients
This study included 1078 ART cycles with the GnRH agonist long protocol. Of them, 314 cycles were in the rFSH-alfa group, and 764 cycles were in the uFSH group, respectively. The patients in the uFSH group were 29.4 ± 3.8 years of age and had a mean BMI of 22.1 ± 3.6 kg/m2, while the patients in the rFSH-alfa group were 29.1 ± 3.6 years of age and had a mean BMI of 22.1 ± 3.6 kg/m2. The two groups were comparable for all baseline characteristics except AFC, which was slightly higher in the rFSH-alfa group (13.4 ± 4.4 vs. 12.3 ± 4.1, P < 0.001). The characteristics of the patients are shown in Table 1.
COS treatment and embryo culture
The overall Gn dose needed to achieve ovulation was significantly lower with rFSH-alfa than with uFSH (1912.3 ± 625.1 vs. 2334.5 ± 687.3 IU, P < 0.001). As shown in Table 2, the mean number of oocytes retrieved (13.0 vs. 10.0), 2PN oocytes (7.0 vs. 5.0), and transferable embryos (5.0 vs. 4.0) in the rFSH-alfa group were higher than in the uFSH group (all P < 0.05).
Clinical outcomes in the uFSH group and rFSH-alfa group
The clinical outcomes were analyzed and compared between the two groups and between the fresh and frozen embryo transfer subgroups in each group, as shown in Table 3. The CBLR was higher with rFSH-alfa than with uFSH (53.5% vs. 43.1%, P = 0.002). The fresh embryo transfer rate (35.0% vs. 26.3%) and the multiple birth rate in the fresh embryo transfer cycles (8.2% vs. 2.5%) in the rFSH-alfa group were higher than in the uFSH group (all P < 0.05). In the fresh transfer subgroup, there were no differences in the pregnancy rate (32.7% vs. 33.8%), the abortion rate (11.1% vs. 11.8%), and LBR (77.8% vs. 79.4%) among the groups in the fresh embryo transfer cycles (all P > 0.05). For the FET cycles, there were no differences in the clinical pregnancy rate (47.7% vs. 48.7%), abortion rate (13.6% vs. 16.3%), LBR (40.1% vs. 39.1%), and multiple birth rate (7.9% vs. 7.5%) between the two groups (all P > 0.05).
Univariable and multivariable analysis for CLBR before and after PSM
The univariable analyses showed that rFSH-alfa (OR = 1.52, 95%CI: 1.17–1.98, P = 0.0018), age (OR = 0.94, 95%CI: 0.91–0.97, P < 0.0001), and AFC (OR = 1.04, 95%CI: 1.01–1.07, P = 0.0031) were associated with higher CLBR in the total study population. The multivariable analysis showed that rFSH-alfa (OR = 1.56, 95%CI: 1.18–2.05, P = 0.018) and age (OR = 0.94, 95%CI: 0.91–0.98, P = 0.0013) were independently associated with a higher CLBR (Table 4). After PSM, it was also found that the CLBR in the rFSH-alfa group was higher than in the uFSH group (53.5% vs. 43.1%, P = 0.0004) (Table S1).
Discussion
This study aimed to compare the clinical outcomes, particularly CLBR, between rFSH-alfa and uFSH regimens for ovarian stimulation in a real-world setting. Our main finding is that after adjusting potential confounders (age, BMI, and AFC), rFSH-alfa was independently associated with a higher CLBR compared with uFSH (OR = 1.56, 95%CI: 1.18–2.05, P = 0.001). To the best of our knowledge, this is the first real-world study that used CLBR as a main outcome on a relatively large sample size and reported significant differences between rFSH-alfa and uFSH.
In addition, we found that the mean number of oocytes retrieved (13.3 vs. 11.0), 2PN oocytes (7.0 vs. 5.0), and transferable embryos (5.0 vs. 4.0) in the rFSH-alfa group were higher than in the uFSH group. There were no differences in the incidence of OHSS (7% vs. 4.7%), pregnancy rate (32.7% vs. 33.8%), abortion rate (11.1% vs. 11.8%), and LBR (77.8% vs. 79.4%) among the groups both in the fresh and frozen embryo transfer cycles.
COS is an important part of assisted reproduction, and FSH is commonly used clinically to enhance recruitment and development of ovarian follicles. Ongoing issues with uFSH derived from urine donations include batch-to-batch variability and a finite donor supply [19]. Indeed, batch-to-batch variability can lead to imprecise dosage [20, 21], and the precise dosage of FSH is critical in COS [4]. Hazard issues with urinary products have also been suggested [21], including impurities [22]. The development of rFSH-alfa has mostly solved related problems. Previous studies have already reported that the pregnancy rates were higher for rFSH but failed to demonstrate differences in LBR [5,6,7,8]. Therefore, many physicians generally consider that for normal responders, a good single transfer cycle LBR can be obtained regardless of the Gn selected and that the selection of Gn is not that important. However, our study found that rFSH-alfa group showed higher oocyte retrieval with fewer FET cycle cancellations (10.0% in the rFSH-alfa group and 18.5% in the uFSH group) in young responders with good responses. Therefore, even in young patients with good responses, rFSH-alfa for COS may bring clear clinical benefits, and the flexible dose adjustment characteristics of rFSH-alfa should be considered to allow for a more individualized Gn initiation and dose adjustment. In our study, the LBR per transfer cycle also showed no difference between rFSH-alfa and uFSH, but the CLBR was higher in the rFSH-alfa group than in the uFSH group, together with the number of retrieved oocytes (13.3 vs. 11.0) and the number of mature oocytes (7.6 vs. 6.0). Those findings are in line with a large real-world study, reporting that the CLBR of a single ovulation induction cycle increases significantly with the number of obtained oocytes [23] and confirming that rFSH-alfa might be beneficial for the clinical outcomes of COS for ART.
rFSH-alfa is produced by inserting the FSH DNA into a Chinese hamster ovary cell line and has no detectable LH activity and very high specific bioactivity for FSH (> 10,000 IU/mg protein) [24, 25]. Highly purified human urinary Gn products are extracted from postmenopausal urine, and for each 75 IU of FSH, the LH content varies from < 1 to 75 IU, and the LH might influence the outcomes of COS or at least complicate the precise control of COS [24, 26]. FSH possesses different isoforms (more or less acidic, glycosylated, and sialylated isoforms), and the extraction conditions of FSH (e.g., pH) from the urine can affect the isoforms being present in the resulting uFSH preparations since the isoforms have different subunit assembly, intracellular sorting, metabolic clearance, and regulation of potency at the cell level [27]. LH activity promotes folliculogenesis in LH deficiency patients [28, 29], but how to precisely dose uFSH to optimize the outcomes of COS when it is unknown which LH content will be found in the next uFSH vial is a major issue. This variability potentially leads to variation in clinical effectiveness, caused not only by the normal problems associated with isolation and purification of hormones from the urine of postmenopausal women but also by the evidence that the bioactive content of uFSH varies considerably from batch to batch [26]. Studies that compared uFSH with rFSH-alfa noted increased ovarian recruitment of follicles in the rFSH-alfa group [30], more efficient ovarian response, and better quality of oocytes [31]. In our study, we also noted that the fresh embryo transfer rate (35.0% vs. 26.3% in the rFSH-alfa group were higher than in the uFSH group (P < 0.05).
Another recent large (> 28,000 women) real-world study demonstrated significantly higher rates of CLBR, cumulative ongoing pregnancy, and cumulative clinical pregnancy with r-hFSH-alfa compared to human menopausal gonadotropin [32]. The relatively large sample size using PSM in our study allowed us to statistically validate previous trends, in particular, that the overall FSH dose needed to achieve ovulation is significantly lower for rFSH-alfa [5, 33], and there is no evidence of a difference in the OHSS rate [34] noted by other studies.
This study has certain limitations. First, there is a risk of selection bias due to the retrospective nature of the study. In order to reduce this effect, we used multivariable analyses and PSM to ensure higher reliability of the obtained outcome. Second, we did not collect the medical costs of two groups in the study. Future studies are warranted to provide more comprehensive evidence for clinical decision-making. Third, we only compared the CLBR between rFSH-alfa and uFSH in patients received agonist long protocol. The different FSH in antagonist protocol will need to be studied in the future. Finally, our study is single-center research. Despite the large sample size, it might not represent other regions or nationalities.
Conclusions
In conclusion, this study reports that despite rFSH-alfa and uFSH having similar pregnancy rates and LBR in both fresh embryo transfer cycle and FET cycle, rFSH-alfa achieved more transferrable blastocysts and higher CLBR compared with uFSH. Those results contribute to the discussion on the use of exogenous Gn regimens in COS and might help in optimizing COS strategies for clinical practice.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- IVF:
-
In vitro fertilization
- ART:
-
Assisted reproductive technology
- COS:
-
Controlled ovarian stimulation
- Gn:
-
Gonadotropin
- uFSH:
-
Urinary follicle-stimulating hormone
- rFSH-alfa:
-
Recombinant follicle-stimulating hormone alfa
- HMG:
-
Human menopausal gonadotropin
- LBR:
-
Live birth rates
- CLBR:
-
Cumulative live birth rate
- FET:
-
Frozen-thawed embryo transfer
- AFC:
-
Antral follicle count
- LH:
-
Luteinizing hormone
References
Vander Borght M, Wyns C. Fertility and infertility: definition and epidemiology. Clin Biochem. 2018;62:2–10.
Szamatowicz M, Szamatowicz J. Proven and unproven methods for diagnosis and treatment of infertility. Adv Med Sci. 2020;65:93–6.
Farquhar C, Marjoribanks J. Assisted reproductive technology: an overview of Cochrane reviews. Cochrane Database Syst Rev. 2018;8:CD010537.
Ovarian Stimulation T, Bosch E, Broer S, Griesinger G, Grynberg M, Humaidan P, et al. ESHRE guideline: ovarian stimulation for IVF/ICSI (dagger). Hum Reprod Open. 2020;2020:hoaa009.
Revelli A, Poso F, Gennarelli G, Moffa F, Grassi G, Massobrio M. Recombinant versus highly-purified, urinary follicle-stimulating hormone (r-FSH vs. HP-uFSH) in ovulation induction: a prospective, randomized study with cost-minimization analysis. Reprod Biol Endocrinol. 2006;4:38.
Pan W, Tu H, Jin L, Hu C, Xiong J, Pan W, et al. Comparison of recombinant and urinary follicle-stimulating hormones over 2000 gonadotropin-releasing hormone antagonist cycles: a retrospective study. Sci Rep. 2019;9:5329.
Liu X, Hao C, Wang J. Efficacy of highly purified urinary FSH versus recombinant FSH in Chinese women over 37 years undergoing assisted reproductive techniques. Int J Fertil Steril. 2015;8:385–92.
Weiss NS, Kostova E, Nahuis M, Mol BWJ, van der Veen F, van Wely M. Gonadotrophins for ovulation induction in women with polycystic ovary syndrome. Cochrane Database Syst Rev. 2019;1:CD010290.
Kamath MS, Mascarenhas M, Franik S, Liu E, Sunkara SK. Clinical adjuncts in in vitro fertilization: a growing list. Fertil Steril. 2019;112:978–86.
Maheshwari A, McLernon D, Bhattacharya S. Cumulative live birth rate: time for a consensus? Hum Reprod. 2015;30:2703–7.
Heijnen EM, Macklon NS, Fauser BC. What is the most relevant standard of success in assisted reproduction? The next step to improving outcomes of IVF: consider the whole treatment. Hum Reprod. 2004;19:1936–8.
pang T, li R. [cumulative live birth rate: a new index for evaluating the efficacy of assisted reproductive technology] (article in chinese). Chinese. J Reprod Contracept. 2019;39:657–9.
Tan SL, Royston P, Campbell S, Jacobs HS, Betts J, Mason B, et al. Cumulative conception and livebirth rates after in-vitro fertilisation. Lancet. 1992;339:1390–4.
De Neubourg D, Bogaerts K, Blockeel C, Coetsier T, Delvigne A, Devreker F, et al. How do cumulative live birth rates and cumulative multiple live birth rates over complete courses of assisted reproductive technology treatment per woman compare among registries? Hum Reprod. 2016;31:93–9.
McLernon DJ, Maheshwari A, Lee AJ, Bhattacharya S. Cumulative live birth rates after one or more complete cycles of IVF: a population-based study of linked cycle data from 178,898 women. Hum Reprod. 2016;31:572–81.
Malizia BA, Hacker MR, Penzias AS. Cumulative live-birth rates after in vitro fertilization. N Engl J Med. 2009;360:236–43.
Ye H, Huang GN, Cao YX, Zhong Y, Huang YH, Zhu GJ, et al. Effect of domestic highly purified urinary follicle stimulating hormone on outcomes of in vitro fertilization-embryo transfer in controlled ovarian stimulation. Zhonghua Fu Chan Ke Za Zhi. 2013;48:838–42.
Bordewijk EM, Mol F, van der Veen F. Van Wely M. required amount of rFSH, HP-hMG and HP-FSH to reach a live birth: a systematic review and meta-analysis. Hum Reprod Open. 2019;2019:hoz008.
Lunenfeld B, Bilger W, Longobardi S, Alam V, D'Hooghe T, Sunkara SK. The development of gonadotropins for clinical use in the treatment of infertility. Front Endocrinol (Lausanne). 2019;10:429.
Yeko T, Pasqualini SR, Alam V, Tredway D. Cumulative ovulation and pregnancy rates according to recombinant human follicle stimulating hormone (r-hFSH) dosing: comparison of a new formulation of follitropin alfa in vials versus the standard formulation of follitropin alfa in ampules. Fertil Steril. 2004;82:S119.
Wikland M, Hugues JN, Howles C. Improving the consistency of ovarian stimulation: follitropin alfa filled-by-mass. Reprod BioMed Online. 2006;12:663–8.
Lispi M, Bassett R, Crisci C, Mancinelli M, Martelli F, Ceccarelli D, et al. Comparative assessment of the consistency and quality of a highly purified FSH extracted from human urine (urofollitropin) and a recombinant human FSH (follitropin alpha). Reprod BioMed Online. 2006;13:179–93.
Ji J, Liu Y, Tong XH, Luo L, Ma J, Chen Z. The optimum number of oocytes in IVF treatment: an analysis of 2455 cycles in China. Hum Reprod. 2013;28:2728–34.
Baker VL, Fujimoto VY, Kettel LM, Adamson GD, Hoehler F, Jones CE, et al. Clinical efficacy of highly purified urinary FSH versus recombinant FSH in volunteers undergoing controlled ovarian stimulation for in vitro fertilization: a randomized, multicenter, investigator-blind trial. Fertil Steril. 2009;91:1005–11.
Bassett RM, Driebergen R. Continued improvements in the quality and consistency of follitropin alfa, recombinant human FSH. Reprod BioMed Online. 2005;10:169–77.
Daya S, Gunby J. Recombinant versus urinary follicle stimulating hormone for ovarian stimulation in assisted reproduction cycles. Cochrane Database Syst Rev. 2000:CD002810.
Barrios-De-Tomasi J, Timossi C, Merchant H, Quintanar A, Avalos JM, Andersen CY, et al. Assessment of the in vitro and in vivo biological activities of the human follicle-stimulating isohormones. Mol Cell Endocrinol. 2002;186:189–98.
Filicori M, Cognigni GE, Taraborrelli S, Spettoli D, Ciampaglia W, de Fatis CT, et al. Luteinizing hormone activity supplementation enhances follicle-stimulating hormone efficacy and improves ovulation induction outcome. J Clin Endocrinol Metab. 1999;84:2659–63.
De Placido G, Alviggi C, Mollo A, Strina I, Ranieri A, Alviggi E, et al. Effects of recombinant LH (rLH) supplementation during controlled ovarian hyperstimulation (COH) in normogonadotrophic women with an initial inadequate response to recombinant FSH (rFSH) after pituitary downregulation. Clin Endocrinol. 2004;60:637–43.
Gholami H, Vicari E, Molis M, La Vignera S, Papaleo E, Cappiello F. Pregnancy outcome following in vitro fertilization-embryo transfer (IVF-ET) in women aged < 37, undergoing ovulation induction with human FSH compared with recombinant FSH: a randomised controlled study. Eur Rev Med Pharmacol Sci. 2010;14:97–102.
Cheon KW, Byun HK, Yang KM, Song IO, Choi KH, Yoo KJ. Efficacy of recombinant human follicle-stimulating hormone in improving oocyte quality in assisted reproductive techniques. J Reprod Med. 2004;49:733–8.
Buhler KF, Fischer R, Verpillat P, Allignol A, Guedes S, Boutmy E, et al. Comparative effectiveness of recombinant human follicle-stimulating hormone alfa (r-hFSH-alfa) versus highly purified urinary human menopausal gonadotropin (hMG HP) in assisted reproductive technology (ART) treatments: a non-interventional study in Germany. Reprod Biol Endocrinol. 2021;19:90.
Hugues JN, Bry-Gauillard H, Bstandig B, Uzan M, Cedrin-Durnerin I. Comparison of recombinant and urinary follicle-stimulating hormone preparations in short-term gonadotropin releasing hormone agonist protocol for in vitro fertilization-embryo transfer. J Assist Reprod Genet. 2001;18:191–6.
van Wely M, Kwan I, Burt AL, Thomas J, Vail A, Van der Veen F, et al. Recombinant versus urinary gonadotrophin for ovarian stimulation in assisted reproductive technology cycles. Cochrane Database Syst Rev. 2011:CD005354.
Acknowledgements
Not applicable
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
All authors participated in the design of the study, CY collected and analyzed the patient data, prepared the first draft of the paper, and actively participated in the entire process of editing. ND revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethics committee of the Reproductive Medicine of Subei People’s Hospital of Jiangsu Province. Due to the retrospective nature, the need for informed consent was waived by the committee.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yang, C., Dong, N., Li, F. et al. The cumulative live birth rate of recombinant follicle-stimulating hormone alfa verse urinary human follicle-stimulating hormone for ovarian stimulation in assisted reproductive technology cycles. J Ovarian Res 15, 74 (2022). https://doi.org/10.1186/s13048-022-01009-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13048-022-01009-w