Abstract
Background
There are many adhesion barrier materials, cross-linked or non-cross-linked hyaluronic acid (HA), used during surgeries.
Purpose
This study investigates the efficacy of cross-linked and non-cross-linked HA in preventing Achilles tendon adhesions. We hypothesized that non-cross-linked HA may be more effective than cross-linked HA in preventing Achilles tendon adhesions following injury and repair.
Methods
Twenty male Sprague Dawley rats, totaling 40 legs, underwent Achilles tendon transection and repair. Following the surgery, they were treated simultaneously with cross-linked and non-cross-linked HA formulations. The rats were divided into four groups: a positive control group, a group treated with BMC non-cross-linked HA gel, a group treated with DEFEHERE cross-linked HA gel, and a group treated with ANIKA cross-linked HA gel. Four weeks after surgery, macroscopic evaluation of peritendinous adhesion and histological analysis were conducted to assess the effectiveness of the treatments.
Results
Non-cross-linked BMC HA demonstrated superior efficacy in preventing tendon adhesions compared to cross-linked HA and control groups. Histological analysis confirmed reduced adhesion severity in the non-cross-linked HA group (P < 0.05). The findings support the potential of non-cross-linked HA as a treatment to inhibit tendon adhesions. Further research, including clinical trials, is warranted to validate these results in human subjects.
Conclusions
Non-cross-linked BMC HA had significantly lower tendon adhesions parameters and better healing scores in histological analysis than cross-linked HA and control group did. Non-cross-linked HA holds promise as a potential treatment to inhibit the formation of such adhesions.
Similar content being viewed by others
Introduction
Achilles tendon disorders are commonly met clinical problems among athletics rendered surgical treatments [1,2,3,4]. Soft tissue and joint adhesions present significant clinical challenges, often manifesting as restricted joint mobility and pain [5]. These adhesions typically stem from histological abnormalities induced by joint inflammation, resulting in fibrosis and contraction of the joint capsule or surrounding soft tissues [6,7,8]. Trauma or surgical interventions commonly precipitate their development. Conventional treatments encompass oral analgesics, intra-articular injections of anti-inflammatory medications, and physical therapy. Moreover, there is emerging evidence suggesting that intra-articular viscosupplementation may alleviate postoperative pain and address adhesion-related conditions [9,10,11,12]. The commercial adhesion barrier materials are polymers, like polytetrafluoroethylene, polylactic acid, oxidized regenerated cellulose, and hyaluronic acid (HA) [13]. The hyaluronate is a non-sulfated glycosaminoglycan, which is one of the chief components of the extracellular matrix [14]. The hyaluronate modulates cell proliferation and migration and prevents inflammation [15]. Based on this property of hyaluronate, it has been used as an anti-adhesive agent in various surgeries, such as gynecological surgery, abdominal surgery, spine surgery, and tendon surgery, to prevent postoperative adhesion with promising results [16,17,18]. However, uncertainties persist regarding the optimal ratio of biological stimulants, the timing of treatment, the efficacy of various components such as cross-linked or non-cross-linked manufacturing, and doses of viscosupplements [19,20,21].
This study employs a rat model where different formulations of HA, both cross-linked and non-cross-linked, are administered to the sutured Achilles tendon following transection and repair. Subsequently, adhesion tissue scoring, and histological analysis are conducted to assess the efficacy of these HA formulations in preventing tendon adhesions. We hypothesized that non-cross-linked HA could be more effective than cross-linked HA in preventing tendon adhesion post-repair because it resolves quicker [18] and had less local effects than cross-linked HA. The findings from this investigation can potentially inform the development of clinical guidelines for preventing tendon adhesions.
Materials and methods
Experimental animal models
Animal Model: Male Sprague Dawley (SD) rats weighing between 220 and 260 g.
Number of Animals: 20 rats in total, with 10 legs assigned to each sample group. Each rat has one leg (left or right) treated with a different sample.
Gel Usage: 0.2 mL of HA gel extracted directly from the sample and applied per treatment.
Allocation of testing samples
Setup involves different groups of left and right sides Achilles tendons of male SD rats, treated with different samples, respectively:
4 groups are distributed as follows:
-
(A)
Positive Control: Wound adhesion without treatment.
-
(B)
BMC (BenQ Material Co., Taoyuan City, Taiwan) Sample: non-cross-linked HA gel.
-
(C)
DEFEHERE (Scivision, Kaohsiung City, Taiwan), cross-linked HA gel.
-
(D)
ANIKA (ANIKA, Bedford, MA), cross-linked HA gel.
Power analysis indicated that a sample size of 8 was necessary for histology studies to detect a 10% difference in histology examination regarding fibrosis (⍺-error, 0.05; β-error, 0.2; drop-out rate, 20%), based on previous studies.
Duration of Experiment: 4 weeks.
This setup allows for a controlled examination of the efficacy of the gel treatment in preventing peri tendinous adhesion formation over the specified duration and within the chosen animal model.
Tendon injury model and treatment
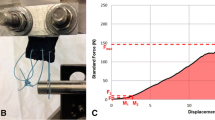
SD rats’ experimental procedures were approved by the Institutional Animal Care and Use Committee of the authors’ hospital. Rats were housed in ventilated micro isolator cages under a 12-h light and dark cycle with free access to food and water. For the tendon injury surgery, 8-week-old male SD rats were anesthetized by intraperitoneal injection of Zoletil 50 + Xylazine (20 mg/kg Z + 10 mg/kg X). Before surgery, the rats were randomly assigned by a technician who was not involved in the study to the control, non-cross-linked, and cross-linked HA Gel-treated groups. A longitudinal incision about 2 cm long was made at the posterior lower leg. The Achilles tendon was cut transversely and repaired using a 5–0 Prolene suture (Ethicon, Edinburgh, UK) with a modified Kessler suture technique. Then 0.2 mL of cross-linked and non-cross-linked HA gel were applied evenly on the tendon suture site following tendon repair. The skin incision was closed with 3–0 Dexon suture (Ethicon, Edinburgh, UK) subsequently. All steps of the procedure are listed in Fig. 1.
Surgical procedure and application of hyaluronic acid. A A longitudinal incision about 2 cm long was made at the posterior lower leg. B The subcutaneous tissue was dissected, and the tendon was cut using 11# scalpels. C The tendon was sutured with 5–0 Prolene suture by a modified Kessler suture technique. D Test articles will be applied evenly on the repaired tendons. E The skin incision was closed with 3–0 Dexon suture
In the experiment, the cages were labeled numerically and randomly to facilitate technicians' identification and operation. Four weeks after the tendon injury, the rats were euthanized, and the tendon tissues were collected for analysis. Only the laboratory director was aware of the group allocation at all experiment stages, including during the allocation, conduct, outcome assessment, and data analysis phases.
Gross evaluation of tendon healing and peritendinous adhesions
Macroscopic evaluation of peritendinous adhesion and maximal strength was performed by two independent researchers according to previously reported methods [22,23,24]. The severity of peritendinous adhesions, was scored as follows: grade 1, no adhesion formation; grade 2, adhesion could be separated by blunt dissection; grade 3, sharp dissection was needed to separate no more than 50% of adhesive tissues; grade 4, sharp dissection was required to separate 51–97.5% of adhesion tissues; and grade 5, sharp dissection was required to separate > 97.5% of adhesion tissues [23, 25] (Fig. 2).
The severity of peritendinous adhesions. Grade 1, no adhesion formation; Grade 2, adhesion could be separated by blunt dissection; Grade 3, sharp dissection was needed to separate no more than 50% of adhesive tissues; Grade 4, sharp dissection was required to separate 51–97.5% of adhesion tissues; and Grade 5, sharp dissection was required to separate > 97.5% of adhesion tissues
H&E and Masson staining
The cut sample were stored at − 80 °C or fixed in 4% paraformaldehyde and embedded in paraffin. Sections were cut at 5 mm thickness and H&E and Masson staining were performed according to standard procedures [22]. Histological evaluation was performed according to a previously reported system [23, 24]. Histologic adhesions were scored as follows: grade 1, no adhesions; grade 2, < 33% of the tendon surface; grade 3, 33–66% of the tendon surface; and grade 4, > 66% of the tendon surface [23, 24]. Histologic tendon healing was scored as follows: grade 1, good tendon continuity and smooth epitenon surface; grade 2, [26] intratendinous collagen bundles exhibited good repair, but the epitenon was interrupted by adhesions; grade 3, irregularly arranged and partly broken collagen bundles; and grade 4, failed healing [23, 24].
Statistical analysis
All experiments were performed at least three times, and the data are described as the means ± standard error of mean (SEM). Statistical analyses were performed using the two-tailed Student’s t-test. Two or more groups were compared using a one-way analysis of variance (ANOVA). All the statistical analyses were conducted using the SPSS 19.0 software (SPSS Inc., Chicago, IL, USA). A P-value < 0.05 was considered statistically significant.
Results
In vivo animal study
Four weeks post-surgery, the repair sites underwent exploration to assess tendon healing and peritendinous adhesions through gross observation. Dense adhesion formations were observed around the tendons in the untreated control (Fig. 3A) and ANIKA-treated group (Fig. 3B), necessitating sharp dissection to separate the large fibrous tissue bundles connecting the tendon and surrounding tissue. In contrast, the DEFEHERE-treated group exhibited small bundles of fibrous tissue bridging the tendon and surrounding tissue (Fig. 3C), with minimal adhesion noted in the BMC-treated group between the repaired tendon and peritendinous tissue throughout the experiment (Fig. 3D).
The statistics regarding tendon adhesions observed through gross observation in the four groups are depicted in Fig. 4. Representative histological sections of tendons treated with each intervention were compared with the control group. In most specimens, severe adhesions between the tendon and surrounding tissues were evident in the untreated control and ANIKA-treated group, necessitating sharp dissection and peeling to separate more than 60% of the large fibrous tissue connecting the tendon and surrounding tissue. In contrast, loose fibrous tissue bridging the repaired tendon and surrounding tissue were observed in the DEFEHERE-treated group. Interestingly, in the BMC-treated group, few peritendinous adhesions were detected in most tendons (Fig. 4D). Histological analysis revealed that parameters for tendon adhesions were significantly lower in the BMC-treated group compared to the other groups (all P < 0.05). Turkey’s multiple comparison tests indicated a statistically significant difference between the BMC group and the control group (P < 0.01), as well as between the DEFEHERE group and the control group (P < 0.05). However, no statistical differences were detected when comparing the BMC and DEFEHERE groups (Fig. 4E). Histologic tendon healing score was score revealed better healing in BMC and DEFEHERE groups when comparted with control group (both P < 0.05, Fig. 4F).
Evaluation of the rat tendon model in untreated control, cross-linked, and non-crosslinked hyaluronic acid gel groups. A Gross evaluation of tendon healing and peritendinous adhesions of the 4 groups before histological exams. B H&E stain, C Masson staining of untreated repair site, repair site wrapped with cross-linked and non-crosslinked hyaluronic acid gel. White arrows indicate the interface without peritendinous adhesions, while black arrowheads indicate peritendinous adhesions between materials and tendon (T). 28 days after surgery, the repaired tendon was evaluated by macroscopic evaluation of tendon adhesions D, the histologic quality of adhesion grade E, and tendon scale F. (n = 10 for each group). Data are expressed as means ± SEM. *P < 0.05; **P < 0.01, Tendon (T) is indicated in the figures, and adhesion tissue is pointed using black arrows
White arrows indicate the interface without peritendinous adhesions, while black arrowheads indicate peritendinous adhesions between materials and tendon (T). 28 days after surgery, the repaired tendon was evaluated by macroscopic evaluation of tendon adhesions (D), the histologic quality of adhesion grade (E), and tendon scale (F). (n = 10 for each group). Data are expressed as means ± SEM. *P < 0.05; **P < 0.01, Tendon (T) is indicated in the figures, and adhesion tissue is pointed using black arrows.
Discussion
In this study, our hypothesis was confirmed that non-cross-linked BMC HA was more effective than cross-linked ANIKA HA and the control group in preventing tendon adhesion post-repair. HA has consistently shown promise in reducing tendon adhesion formation, particularly following tendon repair after injury [27,28,29,30]. Previous studies using a rat model of Achilles tendon repair have demonstrated that HA treatment significantly decreases adhesion scores compared to control groups, as assessed by macroscopic and histological evaluations [31]. Additionally, HA has been found to promote tendon healing and reduce post-operative adhesion formation across various tendon types, including the rotator cuff, epicondylitis, Achilles, and patellar tendinopathy [9].
This study investigated the impact of BMC, a non-cross-linked HA, on preventing peritendinous adhesion formation in a rat experimental model. Peritendinous adhesions are significant postoperative complications commonly observed after tendon repair in orthopedic surgery [32]. While the concept of utilizing a mechanical barrier to prevent adhesion formation is not new, [33] the effectiveness of various materials, both biological and synthetic, has been inconsistent over past decades [34, 35]. Biological barriers may introduce issues such as donor site morbidity and increased surgical complexity. At the same time, certain synthetic materials have failed due to eliciting a strong inflammatory reaction or facilitating adhesion ingrowth around their edges [26, 36, 37]. Additionally, some materials hindered nutrient diffusion to the healing tendon, ultimately resulting in tendon necrosis [38].
Cross-linked HA has demonstrated efficacy in alleviating knee pain associated with osteoarthritis. Studies have shown that a single injection of cross-linked HA can be safe and effective for at least 52 weeks, with some patients experiencing pain relief and improved joint function up to 39 weeks post-treatment [39, 40]. On the other hand, non-cross-linked HA has not been extensively investigated for its potential to reduce adhesion formation. In a study comparing the efficacy of a cross-linked hyaluronan solution with non-cross-linked HA, both forms of HA demonstrated effectiveness as resorbable biomaterials for reducing postoperative adhesions after laparotomy [41]. However, in contrast, a separate study found that non-cross-linked HA failed to show efficacy in reducing adhesions within the utilized models [42]. Previous literature has presented inconclusive evidence regarding the comparative effectiveness of cross-linked versus non-cross-linked HA. Therefore, our study's design has the potential to provide a definitive insight into the effectiveness of non-cross-linked HA as an anti-adhesion agent.
Conclusion
Non-cross-linked BMC HA had significantly lower tendon adhesions parameters and better healing scores in histological analysis than cross-linked HA and control group did. Non-cross-linked HA holds promise as a potential treatment to inhibit the formation of such adhesions.
Availability of data and materials
The data details can be found in the Chang Gung Memorial Hospital Database. The point of contact is the corresponding author (Joe Chih-Hao Chiu MD, PhD).
References
Maffulli N, Irwin AS, Kenward MG, Smith F, Porter RW. Achilles tendon rupture and sciatica: a possible correlation. Br J Sports Med. 1998;32(2):174.
Gajhede-Knudsen M, Ekstrand J, Magnusson H, Maffulli N. Recurrence of Achilles tendon injuries in elite male football players is more common after early return to play: an 11-year follow-up of the UEFA Champions League injury study. Br J Sports Med. 2013;47(12):763–8.
Godoy-Santos AL, Bruschini H, Cury J, Srougi M, de Cesar-Netto C, Fonseca LF, Maffulli N. Fluoroquinolones and the risk of achilles tendon disorders: update on a neglected complication. Urology. 2018;113:20–5.
Maffulli N. Current concepts in the management of subcutaneous tears of the Achilles tendon. Bulletin (Hospital for Joint Diseases (New York, NY)). 1998;57(3):152–8.
Temiz A, Ozturk C, Bakunov A, Kara K, Kaleli T. A new material for prevention of peritendinous fibrotic adhesions after tendon repair: oxidised regenerated cellulose (Interceed), an absorbable adhesion barrier. Int Orthop. 2008;32(3):389–94.
Gelberman RH, Woo SL, Amiel D, Horibe S, Lee D. Influences of flexor sheath continuity and early motion on tendon healing in dogs. J Hand Surg Am. 1990;15(1):69–77.
Ruzzini L, Longo UG, Campi S, Maffulli N, Onetti Muda A, Denaro V. Adhesion and collagen production of human tenocytes seeded on degradable poly (urethane urea). Knee Surg Sports Traumatol Arthrosc. 2013;21:1834–40.
Gougoulias N, Maffulli N. Peritendinous adhesions that form after the repair of lacerated digital flexor tendons cause stiffness and functional impairment. J Bone Jt Surg Am. 2011;93(2):e7–e7.
Oliva F, Marsilio E, Asparago G, Frizziero A, Berardi AC, Maffulli N. The impact of hyaluronic acid on tendon physiology and its clinical application in tendinopathies. Cells. 2021;10(11):3081.
Khanna A, Gougoulias N, Maffulli N. Modalities in prevention of flexor tendon adhesion in the hand: What have we achieved so far? Acta Orthop Belg. 2009;75(4):433.
Khanna A, Friel M, Gougoulias N, Longo UG, Maffulli N. Prevention of adhesions in surgery of the flexor tendons of the hand: what is the evidence? Br Med Bull. 2009;90(1):85–109.
Johns DB, Rodgers KE, Donahue WD, Kiorpes TC. Reduction of adhesion formation by postoperative administration of ionically cross-linked hyaluronic acid. Fertil Steril. 1997;68(1):37–42.
Chen P-C, Chen Y-P, Wu C-C, Tseng C-C, Yang C-Y, Hung Y-W, Wen Z-H. A resorbable hyaluronic acid hydrogel to prevent adhesion in porcine model under laparotomy pelvic surgery. J Appl Biomater Funct Mater. 2021;19:2280800020983233.
Gupta RC, Lall R, Srivastava A, Sinha A. Hyaluronic acid: molecular mechanisms and therapeutic trajectory. Front Vet Sci. 2019;18:10. https://doi.org/10.3389/fvets.2019.00192.
Bär A, Van Ommen B, Timonen M. Metabolic disposition in rats of regular and enzymatically depolymerized sodium carboxymethylcellulose. Food Chem Toxicol. 1995;33(11):901–7.
Park H, Baek S, Kang H, Lee D. Biomaterials to prevent post-operative adhesion. Materials. 2020;13(14):3056.
Kumar S, Wong PF, Leaper DJ. Intra-peritoneal prophylactic agents for preventing adhesions and adhesive intestinal obstruction after non-gynaecological abdominal surgery. Cochrane Database Syst Rev. 2009. https://doi.org/10.1002/14651858.CD005080.pub2.
Mineda K, Feng J, Ishimine H, Takada H, Doi K, Kuno S, Kinoshita K, Kanayama K, Kato H, Mashiko T. Therapeutic potential of human adipose-derived stem/stromal cell microspheroids prepared by three-dimensional culture in non-cross-linked hyaluronic acid gel. Stem Cells Transl Med. 2015;4(12):1511–22.
Miller JA, Ferguson RL, Powers DL, Burns JW, Shalaby SW. Efficacy of hyaluronic acid/nonsteroidal anti-inflammatory drug systems in preventing postsurgical tendon adhesions. J Biomed Mater Res. 1997;38(1):25–33.
McGonagle L, Jones MD, Dowson D, Theobald PS. The bio-tribological properties of anti-adhesive agents commonly used during tendon repair. J Orthop Res. 2012;30(5):775–80.
Sikes KJ, Renner K, Li J, Grande-Allen KJ, Connell JP, Cali V, Midura RJ, Sandy JD, Plaas A, Wang VM. Knockout of hyaluronan synthase 1, but not 3, impairs formation of the retrocalcaneal bursa. J Orthop Res. 2018;36(10):2622–32.
Li L, Huang W, Li K, Zhang K, Lin C, Han R, Lu C, Wang Y, Chen H, Sun F, et al. Metformin attenuates gefitinib-induced exacerbation of pulmonary fibrosis by inhibition of TGF-β signaling pathway. Oncotarget. 2015;6(41):43605–19.
Jiang S, Zhao X, Chen S, Pan G, Song J, He N, Li F, Cui W, Fan C. Down-regulating ERK1/2 and SMAD2/3 phosphorylation by physical barrier of celecoxib-loaded electrospun fibrous membranes prevents tendon adhesions. Biomaterials. 2014;35(37):9920–9.
Yao Z, Wang W, Ning J, Zhang X, Zheng W, Qian Y, Fan C. Hydroxycamptothecin inhibits peritendinous adhesion via the endoplasmic reticulum stress-dependent apoptosis. Front Pharmacol. 2019;10:967.
Zheng W, Song J, Zhang Y, Chen S, Ruan H, Fan C. Metformin prevents peritendinous fibrosis by inhibiting transforming growth factor-β signaling. Oncotarget. 2017;8(60):101784–94.
Rossi LA, Pasqualini I, Huespe I, Brandariz R, Fieiras C, Tanoira I, Ranalletta M. A 2-year follow-up may not be enough to accurately evaluate recurrences after arthroscopic Bankart repair: a long-term assessment of 272 patients with a mean follow-up of 10.5 years. Am J Sports Med. 2023;51(2):316–22.
Balazs EA, Laurent TC, Jeanloz RW. Nomenclature of hyaluronic acid. Biochem J. 1986;235(3):903.
Hascall VC, Majors AK, De La Motte CA, Evanko SP, Wang A, Drazba JA, Strong SA, Wight TN. Intracellular hyaluronan: a new frontier for inflammation? Biochim Biophys Acta. 2004;1673(1–2):3–12.
Kogan G, Soltés L, Stern R, Gemeiner P. Hyaluronic acid: a natural biopolymer with a broad range of biomedical and industrial applications. Biotechnol Lett. 2007;29(1):17–25.
Sawaguchi N, Majima T, Iwasaki N, Funakoshi T, Shimode K, Onodera T, Minami A. Extracellular matrix modulates expression of cell-surface proteoglycan genes in fibroblasts. Connect Tissue Res. 2006;47(3):141–8.
Ahn KH, Park ES, Choi CY, Cha HG, Hwang Y, Nam SM. Hyaluronic acid treatment improves healing of the tenorrhaphy site by suppressing adhesions through extracellular matrix remodeling in a rat model. Polymers (Basel). 2021;13(6):928.
Zhou H, Lu H. Advances in the development of anti-adhesive biomaterials for tendon repair treatment. Tissue Eng Regen Med. 2021;18(1):1–14.
Pinnaratip R, Bhuiyan MSA, Meyers K, Rajachar RM, Lee BP. Multifunctional biomedical adhesives. Adv Healthc Mater. 2019;8(11): e1801568.
Shah NV, Meislin R. Current state and use of biological adhesives in orthopedic surgery. Orthopedics. 2013;36(12):945–56.
Park CH, Woo KM. Fibrin-based biomaterial applications in tissue engineering and regenerative medicine. Adv Exp Med Biol. 2018;1064:253–61.
Park H, Baek S, Kang H, Lee D. Biomaterials to prevent post-operative adhesion. Materials (Basel). 2020;13(14):3056.
Tan AR, Ifkovits JL, Baker BM, Brey DM, Mauck RL, Burdick JA. Electrospinning of photocrosslinked and degradable fibrous scaffolds. J Biomed Mater Res A. 2008;87(4):1034–43.
Yalcin E, Cavusoglu K. Glutaraldehyde cross-linked agarose carriers: design, characterization and insulin release behaviour. Turk J Biochem. 2008;33:148–53.
Petterson SC, Plancher KD. Single intra-articular injection of lightly cross-linked hyaluronic acid reduces knee pain in symptomatic knee osteoarthritis: a multicenter, double-blind, randomized, placebo-controlled trial. Knee Surg Sports Traumatol Arthrosc. 2019;27(6):1992–2002.
Ko PY, Li CY, Li CL, Kuo LC, Su WR, Jou IM, Wu PT. Single injection of cross-linked hyaluronate in knee osteoarthritis: a 52-week double-blind randomized controlled trial. Pharmaceutics. 2022;14(9):1783.
Koçak I, Unlü C, Akçan Y, Yakin K. Reduction of adhesion formation with cross-linked hyaluronic acid after peritoneal surgery in rats. Fertil Steril. 1999;72(5):873–8.
Johns DB, Rodgers KE, Donahue WD, Kiorpes TC, diZerega GS. Reduction of adhesion formation by postoperative administration of ionically cross-linked hyaluronic acid. Fertil Steril. 1997;68(1):37–42.
Acknowledgements
The authors gratefully thank Taiwan Minister of Science and Technology and Linkou Chang Gung Memorial Hospital for financial support of this study (Grant: MOST 111-2628-B-182A-016, NSTC112-2628-B-182A-002, SMRPG3N0011, CMRPG5K0092, CMRPG3M2032)
Funding
The authors gratefully thank Taiwan Minister of Science and Technology and Linkou Chang Gung Memorial Hospital for financial support of this study (Grant: MOST 111-2628-B-182A-016, NSTC112-2628-B-182A-002, SMRPG3N0011, CMRPG5K0092, CMRPG3M2032).
Author information
Authors and Affiliations
Contributions
CH wrote the paper. PC and CY performed the study. YC prepared the pictures. JC revised the whole manuscript and apply for the grant.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
2021101301.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Hsu, CH., Chen, P., Yang, CP. et al. The results of preventing postoperative achilles tendon adhesion using cross-linked and non-cross-linked hyaluronic acid, a study with rat model. J Orthop Surg Res 19, 457 (2024). https://doi.org/10.1186/s13018-024-04952-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-024-04952-0