Abstract
Background
The COVID-19 pandemic has led to a surge in the use of telemedicine as a means of delivering healthcare services remotely. Healthcare providers play a key role in the adoption and implementation of telemedicine for its effectiveness. Despite its benefits, there have been unclear concerns about its effectiveness and acceptance in the process of implementing telemedicine. The objective of the study was to assess health professionals’ perceptions towards the implementation of telemedicine during the COVID-19 pandemic.
Methods
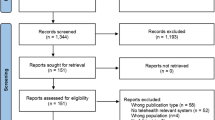
A cross-sectional study design was conducted among eight hundred forty-five study participants from December 2020 to February 2021. A pre-test was performed on 5% of the total sample size, and the quality of the data was ensured by checking its completeness and consistency. Descriptive statistics and bivariable and multivariable logistic regression were used. The Variables with a P-value equal to or less than 0.25 in bivariable logistic regression were entered into a multivariable logistic regression, and model fitness was assessed.
Result
The study revealed that 60.9% of professionals had a good perception toward telemedicine implementation, with an 87.2% response rate. Health professionals with IT support staff, ICT training, who use social media platforms regularly, and availability of computer or smartphone within/outside their health facility were 4.7, 3.3, 3.7, and 13.2 times more likely to have a positive association towards telemedicine implementation respectively.
Conclusion
More than half of the health professionals had a good perception of telemedicine. Social media use, ICT training, computer accessibility, and the presence of IT support staff were all found to have positive associations with the telemedicine perception. In the era of the COVID-19 pandemic, the government should take the initiative to strengthen opportunities for health professionals to learn and apply telemedicine in their medical practice by providing ICT training, IT infrastructure and support staff, improving computer access, and recommending health professionals’ positive use of social media in the health facility.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The COVID-19 pandemic severely harmed human ways of life around the world, and poses an unprecedented challenge in healthcare management. It is spread by droplets of saliva or discharge when an infected person coughs or sneezes [1,2,3].
The impacts of COVID-19 increased the burden on healthcare providers to respond to patient inquiries [4,5,6]. The global spread of COVID-19 hampered countries’ ability to address and respond to non-communicable diseases, as well as other routine activities [7,8,9,10]. To limit its communicability and improve provider preparedness, scholars recommend telemedicine as a preferable channel between health professionals and patients [11, 12]. Moreover, telemedicine overcomes the challenges in the control and prevention of the COVID-19 pandemic during the lockdown and restriction of face-to-face interactions. Health professionals were frightened by COVID-19, and generally, it was difficult to deliver health services during the pandemic [13,14,15].
Telemedicine has been implemented to promote medication adherence, resulting in fewer readmissions, lower morbidity and mortality, improved access to follow-up care, and high patient satisfaction [16,17,18,19]. Even though the patients benefited from increased access to health care, improved healthcare quality, and cost control in the developed countries [20], the perception of telemedicine among health professionals is not identified for long-term telemedicine implementation in resource-limited settings [21, 22].
The use of telemedicine to deliver healthcare services for chronic disease patients has been helpful during this pandemic. According to some studies, health professionals’ positive perceptions towards telemedicine are a critical factor in maximizing telemedicine adoption for communicable disease control and prevention [23, 24].
Social media platforms have been a way to engage with the public to provide insight into healthcare campaigns, a medium for sharing daily events [25], and health professionals have greatly participated in providing COVID-19 information [26,27,28]. The perceived use of social media by health professionals aids in the delivery of health care services to patients over long distances via telehealth [28, 29]. In the era of the COVID-19 pandemic, different social media platforms such as Facebook, Twitter, and Telegram were accurate reflections of how the disease spread and burden to communities [30]. Social media platforms became a main source of health information about day-to-day events and knowledge-sharing responses to the pandemic [31, 32].
Although, Sharing health information to provide health care services across distance and time has been proposed as a potential solution to the current health care crisis, as it aids in scaling up the health care system and providing health care services to rural and remote areas for disease control and prevention [33].
The potential impact of telemedicine on healthcare delivery is well-known [3]. However, it has failed to sustain and integrate with the healthcare system, particularly in developing countries [34]. To deliver convenient healthcare services to the patient, the healthcare facility needs advanced medical instruments and healthcare services, but some of these are expensive and concentrated in a limited facility [35]. Especially in Ethiopia, the accessibility of healthcare services is costly and risky in the era of the COVID-19 pandemic [34, 36]. Assessing the perception of telemedicine among health professionals is significantly important as a baseline study and full implementation telemedicine system and helps the Ethiopian health system concerning healthcare digitization. Therefore, this study aimed to assess perceptions of health professionals towards telemedicine implementation and associated factors in Ethiopia during the COVID-19 Pandemic.
Methods and materials
Study design, setting, and period
An institutional-based cross-sectional study design study was conducted at a governmental health facility among health professionals in Addis Ababa started from December 2020 to February 2021. The study area has a population of more than 4 million. It has ten sub-cities, the capital city of the country, and the AU, and has more than 80 government health facilities in the city and 50 private health facilities. The total number of health professionals in the city is more than 20,000.
Source and study populations
All health professionals who were working at a governmental health facility were the source population. The health professionals who were working in the selected governmental health facility found in Addis Ababa were the study population.
Inclusion and exclusion criteria
Health professionals working at government health facilities in Addis Ababa and available during data collection time were included in the study. Health professionals who were seriously ill, unable to respond and positive for COVID-19 were excluded from the study.
Sample size determination and sampling procedures
The sample size was determined by using the single population proportion formula of 50% of health professionals to determine the perception of telemedicine since there was no previous study done in the same population among health professionals. By considering a 10% non-response rate and stratified the health professionals to their respective departments, so the design effect two and the total sample size was 845 study participants. Were
-
✓ n1 = was the calculated sample size , Z = Confidence interval [95%]
-
✓ P = (Proportion of perception of Telemedicine health professionals =50%
-
✓ 1-p = proportion of No perception of Telemedicine health professionals
-
✓ d = marginal error [5%] and design effect =2
$$\mathrm{n}1=\frac{{\left(Z\alpha /2\right)}^{2} \mathrm{p}\left(1-\mathrm{p}\right)}{{d}^{2}} =\frac{{\left(1.96\right)}^{2} *0.5 * \left(1-0.5\right)}{{\left(0.05\right)}^{2}} \boldsymbol{=384*2+768*0.1=845}$$
Study participants were selected from ten hospitals, two health centers from each sub-city in the Addis Ababa Administration, and a proportionate allocation from each hospital in the Administration, while health professionals were selected using simple random sampling techniques by a lottery method after being stratified according to their respective professions.
Operational definition
Health professional
Employees with at least a diploma certificate in the health professions who provide healthcare services in the study settings were defined as health professionals [37].
Telemedicine system
Using video conferencing, store-and-forward imaging, and wireless communications to diagnose or treat a patient, as well as providing remote patient monitoring services, electronic information, and telecommunication technologies are used to support long-distance clinical health and public health care, patients, and health professionals to prevent and control COVID-19 pandemics [38, 39].
Telemedicine
Use teleconsultation, Tele-education, teleradiology, mobile data dissemination, and other telemedicine components with interactive video conferencing online, storing and forwarding, remote patient monitoring applications and other audio platforms to diagnose or treat a patient, patient monitoring services, or consult with other health care providers to prevent and control COVID-19 pandemics, [40, 41].
Good perception telemedicine
Study participants who scored above the median in the five-point Likert scale of perception questions were categorized as having a good perception of the implementation of telemedicine, while those who scored below the median were categorized as having a poor perception [42].
Data collection tool and procedures
A structured administrative questionnaire adapted and modified from various literatures was used to collect the data. The questionnaire was prepared in English and included socio-demographic characteristics of the respondents, basic computer skills and internet use, Knowledge on healthcare digitization, and organizational-related questions. Data were collected using 18 a five-point Likert-scale questionnaire, ranging from 1 to 5, i.e., “1” for strongly disagree, “2” for strongly disagree, “3” for neutral, “4” for agree, and “5” for strongly agree. A minimum of “18” and a maximum of “90” can be scored to assess the study participant’s perception of telemedicine during the COVID-19 Pandemic [43,44,45]. It was pre-tested for reliability before the conduct of the actual data collection. Four Health informatics professionals collected the data after receiving one-day training on the research’s objective, purpose, and how to conduct the data collection and were guided by a supervisor. Both the data collectors and study participants used COVID-19 protective equipment like masks and sanitizers, keeping a 2-m distance.
Data quality assurance
The content validity of the questionnaire was checked, and the reliability was calculated using Cronbach’s alpha coefficient (α = 0.79). Before the actual data collection, modifications were made based on the pre-test. The data collectors and the supervisor were selected and trained before participating in the actual data collection process. Creating awareness of the purpose of the study, their rights, and confidentiality issues, sufficient time was given to respondents to read and fill in materials carefully. There was continuous supervision up to the end of data collection. After collecting the data, the supervisor and the investigator checked its consistency and completeness. We used a backup system to minimize data duplication and data loss.
Data processing and analysis
Data was edited and cleaned, then exported to SPSS- 26 for further analysis and to generate descriptive statistics of the collected data to describe variables in the study using statistical measurements. A binary logistic regression was used to analyze the association between the independent variable and the dependent variable (good or poor perception of telemedicine). Then, if the P-Value was 0.2, multivariable logistic regression analysis was carried out to assess the perception of telemedicine. A significant association was interpreted using an odds ratio, a 95% confidence interval, and a p-value less than 0.05. The Hosmer–Lemeshow test was used to test model fitness, and model multicollinearity was checked using variance inflation factors (VIF).
Result
Socio-demographic characteristics
Seven hundred thirty-seven (87.2% response rate) of the study participants were given written consent to respond to all the questionnaires. Among the study participants, 507 (62.8%) respondents were male. The mean age of the participants was 31.32 + 7.33 SD years, and the majority of the respondents were within the age group of 20–29 years. In terms of educational status, most of the respondents had bachelor’s degrees (51.6%). Regarding the professions of the respondents, 150 (20.4%) were medical doctors and 155 (21.0%) were nurses. The average working experience was 3 + 1.2 SD years, in terms of respondents age, 341( 46.3%) were between the ages of 1 and 5, with 701 (95.1%) using computers, PCs, or smartphones to perform various internet tasks (42.8%) (Table 1).
Basic computer skills and internet use
More than two-third of the 457 (62.0%) respondents had taken basic ICT training, 701 (95.1%) used their computer, laptop, or Smartphone for work, and 321 (43.6%) of study participants searched for information online to provide advice. During the COVID-19 pandemic, 584 (29.4%) of study participants were asked for online advice by patients. 238 (32.3%) of the participants in the study communicated with patients via e-mail or social media (24.3%) (Table 2).
Knowledge on healthcare digitization
More than half of the participants (497, or 67.4%) were familiar with health care digitations or E-health. The internet was the source of information for those who knew about e-health. 505 (23.6%) and 306 (60.59%) of study participants had visited telemedicine-related websites on the Internet. During the COVID-19 pandemic, 555 (75.3%) of respondents shared information with their friends, consulate healthcare providers, and patients. Although 627 (85.1%) respondents were aware of the factors that impede the use of telemedicine services in the health facility, 576 (25.56%) study participants stated that a lack of telemedicine awareness and 524 (23.25%) a lack of E-health professionals were factors that hampered the implementation and use of telemedicine systems (Fig. 1) (Table 3).
Organizational factors for telemedicine implementation
According to the finding, majority of the study participants 514 (69.7%) had sufficient computers for their work; 525 (71.2%) of the participants had internet access within their health facility, and 241 (45.90%) had both Wi-Fi and broadband types of internet access. Similarly, 555 (75.3%) of the health professionals had an information-sharing culture with other healthcare providers or patients, 461 (62.6%) of the study participants had attended training for E-health or health information revolution, and also 498 (67.6%) study participants had IT, support staff, in their health facility (Table 4).
Factors associated with the perception of health professionals towards telemedicine implementation
Computer accessibility, health professionals’ ICT training, frequency of use of social media, and having IT support staff in their health facility, were all significantly associated with the perception of telemedicine implementation among health professionals for the control and prevention of COVID-19. Participants in the study who had sufficient computers were 13.2 times more likely to have a good perception of using telemedicine than those who did not have enough computers in their organization (AOR = 13.21, 95% CI: [5.07–24.05]).
Health professionals in facilities with IT-supporting staff were 4.7 times more likely to have a good perception of telemedicine systems for COVID-19 control and prevention than those in facilities without IT-supporting staff (AOR = 4.42, 95%CI: [CI: 2.958–7.52]). Health professionals certified in ICT were strongly associated with the perception of telemedicine implementation for the control and prevention of COVID-19. Health professionals who had received certification in related ICT areas were 3.26 times more likely to be perceived positively than those who had not (AOR = 3.263, 95% CI: [1.72–6.18]). Another factor influencing health professionals’ perception of telemedicine was their use of social media/Gmail platforms. Health professionals who used social media regularly were 3.7 times more likely to be perceived positively than those who did not (AOR = 3.224, 95% CI: [1.805–7.88]) (Others4, Dongle internet from telecoms, Table 5).
Discussion
In low-income settings, telemedicine helps users to diagnose and treat patients remotely and offers many advantages to the healthcare system, ranging from immediate access to high-quality healthcare services to reducing healthcare expenses [46]. Providing adequate information about telemedicine technologies to health professionals aids in improving their perceptions.
According to the findings of this study, 60.9% (95% CI: [60.7, 67.4]) of health professionals had a good perception of telemedicine. Perception of e-health is important for the implementation of telemedicine to improve healthcare delivery in rural and remote areas. Currently, the Ministry of Health is focusing on healthcare digitization as one of its top priorities, even though we have limited resources and technological infrastructure to dedicate to the healthcare system [47]. The study is high as compared with the previous cross-section study conducted in Addis Ababa [48]. This could be due to the time lapse between the study’s completion and the Ethiopian government’s increased emphasis on ICT to support the health system.
The finding is also lower than the study conducted in Iran [49]. User motivation and support can help technology become a reality, allowing the system to scale up and the value of health professionals to e-Health to increase [50]. Furthermore, this study differs from a study conducted in Australia [45] that would improve dental practice by improving communication with colleagues and referring new patients. It could be a difference in infrastructure between developing and developed countries.
A study conducted in Saudi Arabia [43] found a high level of perception toward telemedicine when compared with this research finding. It could be due to differences in infrastructure and e-health literacy between the two countries. More than half of the participants were aware of the benefits of telemedicine services. Some scholars indicate that telemedicine can decrease the risk of infection in the hospital, provide adequate treatment and follow-up of patients, and provide a suitable approach for providing remote mental health services [51]. When the participants were aware of the types of telemedicine services available to deliver healthcare services by using telemedicine applications [52]. For both clients and healthcare workers, telemedicine provides continuous access to critical healthcare services in the era of COVID-19 [53].
This study is consistent with a study conducted in Europe, which found that the availability of technology, access to the internet, and a lack of telemedicine training are the most significant factors influencing healthcare provider perception [54]. Besides that, as found in a study conducted in Indonesia, study participants’ lack of internet connectivity was a significant barrier to using telemedicine [44]. A telemedicine training intervention carried out among nursing staff in India demonstrates an effective method of increasing telemedicine awareness and adoption [55]. The pandemic has had a positive impact on the perception of physicians and other stakeholders toward telemedicine and the adoption of this new technology is changing due to the present conduction of COVID-19 [56]. Health professionals who had received ICT training had a positive perception of telemedicine, and the digitization era could help improve their perception.
Another study conducted in developing countries found that many healthcare providers are unable to resolve technical issues caused related to computer systems and ICT networks. As a result, for the telemedicine system to function properly and smoothly, trained and expert personnel are required to establish stable and continuous communication during teleconsultation [57]. It could be due to a lack of technical support, training, or government concern.
According to this finding, frequent use of social media determined whether health professionals were likely to be perceived positively towards telemedicine implementation [25]. The scholars indicated that the COVID-19 medical guidelines have been distributed through social media communication channels such as Facebook, YouTube, or Telegram [58], where health professionals frequently exchange information and disseminate knowledge regarding how to control and minimize the spread of the virus [59].
During lockdown measures at health facilities, physicians have conducted free medical consultations through social media, and researchers disseminate articles published by international authoritative magazines [60]. Sometimes the doctors establish a non-contact doctor-to-patient interactive network platform based on mobile Internet, including social media management, which was used as an important information channel for preventing and responding to the COVID-19 epidemic [61, 62]. Therefore, to scale up and implement the telemedicine system within healthcare facilities, health professionals need ICT training, technical support, and improved internet access to motivate users to use telemedicine.
Conclusion
More than half of the health professionals had a good perception of telemedicine during the COVID-19 pandemic. The telemedicine concept is more popular among health professionals and has the potential to be fully integrated into the healthcare system. The use of social media, ICT training, computer accessibility, and the availability of IT support staff were all found to be significantly associated with the telemedicine system.
The government should take the initiative to strengthen opportunities for health professionals to learn and apply telemedicine in their medical practice by providing ICT training, and IT support staff, improving computer access, and recommending health professionals' positive use of social media in the health facility to promote the evidence-based use of telemedicine in the era of the COVID-19 pandemic and future outbreaks in health facilities.
Strengths and limitations of the study
This study has the following strengths. The sample size was large which help to generalize the result. The result of this study will be used as a baseline for other researcher and helps the scalability of health sectors to digital health transformation.
However, the study was not supported by a qualitative study, as we employed a simple random sampling method that may be affected by the sample frame and its lower precision. The study was conducted only in an urban environment, where there is a higher likelihood of perception towards telemedicine.
Availability of data and materials
All major data have been analyzed and presented in the manuscript.
Abbreviations
- BSC:
-
Bachelor of Science
- E-Health:
-
Electronic Health
- Epi-info:
-
Epidemiological Information
- ETB:
-
Ethiopian Birr
- FMOH:
-
Federal Ministry of Health
- GP:
-
General Practitioners
- HI:
-
Health Informatics
- HIT:
-
Health Information Technician
- HP:
-
Health professionals
- MPH:
-
Master of Public Health
- ICT:
-
Information communication technology
- IT:
-
Information technology
- SPSS:
-
Statistical Package for Social Science
- WHO:
-
World Health Organization
References
Ezhilan M, Suresh I, Nesakumar N. SARS-CoV, MERS-CoV and SARS-CoV-2: a diagnostic challenge. Measurement. 2021;168:108335.
Hassel J, Schütze S, Hagenlocher M. COVID-19 Pandemic.
Lone SA, Ahmad A. COVID-19 pandemic–an African perspective. Emerg Microbes Infect. 2020;9(1):1300–8.
Bauchner H, Sharfstein J. A bold response to the COVID-19 pandemic: medical students, national service, and public health. JAMA. 2020;323(18):1790–1.
Uy J, et al. The impact of COVID-19 on hospital admissions for twelve high-burden diseases and five common procedures in the Philippines: A National Health Insurance Database Study 2019–2020. Lancet Reg Health-West Pac. 2022;18:100310.
Mehraeen E, et al. Technology in the era of COVID-19: a systematic review of current evidence. 2022;22(4):51–60.
Akalu Y, Ayelign B, Molla MD. Knowledge, attitude and practice towards COVID-19 among chronic disease patients at Addis Zemen Hospital, Northwest Ethiopia. Infect Drug Resist. 2020;13:1949.
Yadav UN, et al. A syndemic perspective on the management of non-communicable diseases amid the COVID-19 pandemic in low-and middle-income countries. Front Public Health. 2020;8:508.
Posai V, et al. Assessment of the health-promoting behaviors of hospitalized patients with non-communicable diseases during the second wave of COVID-19. J Multidiscip Healthc. 2021;14:2185.
Mehraeen E, et al. Telemedicine technologies and applications in the era of COVID-19 pandemic: A systematic review. 2023;29(2):14604582231167431.
Albarrak AI, et al. Assessment of physician’s knowledge, perception and willingness of telemedicine in Riyadh region, Saudi Arabia. J Infect Public Health. 2021;14(1):97–102.
Almeida F, Santos JD, Monteiro JA. The challenges and opportunities in the digitalization of companies in a post-COVID-19 World. IEEE Eng Manage Rev. 2020;48(3):97–103.
Boehm K, et al. Telemedicine online visits in urology during the COVID-19 pandemic—potential, risk factors, and patients’ perspective. Eur Urol. 2020.
Ghai B, Malhotra N, Bajwa SJS. Telemedicine for chronic pain management during COVID-19 pandemic. Indian J Anaesth. 2020;64(6):456.
Anthony Jnr B. Integrating telemedicine to support digital health care for the management of COVID-19 pandemic. Int J Healthc Manag. 2021;14(1):280–9.
Kim E, Gellis ZD, Hoak V. Telehealth utilization for chronic illness and depression among home health agencies: A pilot survey. Home Health Care Serv Q. 2015;34(3–4):220–31.
Kooy MJ, et al. Patients’ general satisfaction with telephone counseling by pharmacists and effects on satisfaction with information and beliefs about medicines: Results from a cluster randomized trial. Patient Educ Couns. 2015;98(6):797–804.
Mburu S, Oboko R. A model for predicting utilization of mHealth interventions in low-resource settings: case of maternal and newborn care in Kenya. BMC Med Inform Decis Mak. 2018;18(1):67–67.
Moss HE, Lai KE, Ko MW. Survey of telehealth adoption by neuro-ophthalmologists during the COVID-19 pandemic: benefits, barriers, and utility. J Neuroophthalmol. 2020;40(3):346–55.
Novara G, et al. Telehealth in urology: a systematic review of the literature. How much can telemedicine be useful during and after the COVID-19 pandemic? Eur Urol. 2020.
Lennon MR, et al. Readiness for delivering digital health at scale: lessons from a longitudinal qualitative evaluation of a national digital health innovation program in the United Kingdom. J Med Internet Res. 2017;19(2):e6900.
Zimmerling A, Chen X. Innovation and possible long-term impact driven by COVID-19: Manufacturing, personal protective equipment and digital technologies. Technol Soc. 2021;65:101541.
Rodriguez JA, Clark CR, Bates DW. Digital health equity as a necessity in the 21st century cures act era. JAMA. 2020;323(23):2381–2.
Ye Q, Zhou J, Wu H. Using information technology to manage the COVID-19 pandemic: development of a technical framework based on practical experience in China. JMIR Med Inform. 2020;8(6):e19515.
Shamsabadi A, et al. Social media application in education during the COVID-19 pandemic; pros and cons: A systematic review. 2023.
Neavel C, Watkins SC, Chavez M. Youth, social media, and telehealth: How COVID-19 changed our interactions. Pediatr Ann. 2022;51(4):e161–6.
Farsi D. Social media and health care, part I: literature review of social media use by health care providers. J Med Internet Res. 2021;23(4):e23205.
Machado RA, et al. Social media and telemedicine for oral diagnosis and counselling in the COVID-19 era. 2020;105:104685.
Li H, et al. The establishment and practice of pharmacy care service based on Internet social media: telemedicine in response to the COVID-19 pandemic. 2021;12:707442.
Massaad E, Cherfan P. Social media data analytics on telehealth during the COVID-19 pandemic. Cureus. 2020;12(4):e7838.
Zhao S, et al. The opportunities and challenges of telemedicine during COVID-19 pandemic. 2021;13(2):291–298.
Peine A, et al. Telemedicine in Germany during the COVID-19 pandemic: multi-professional national survey. 2020;22(8): e19745.
Brown NA. The telemedicine information exchange: an online resource. Comput Biol Med. 1998;28(5):509–18.
Dodoo JE, Al-Samarraie H, Alzahrani AI. Telemedicine use in sub-Saharan Africa: barriers and policy recommendations for Covid-19 and beyond. Int J Med Informatics. 2021;151:104467.
Mann DM, et al. COVID-19 transforms health care through telemedicine: evidence from the field. J Am Med Inform Assoc. 2020;27(7):1132–5.
Abdela SG, et al. Essential healthcare services in the face of COVID-19 prevention: experiences from a referral hospital in Ethiopia. Am J Trop Med Hyg. 2020;103(3):1198.
Biruk K, Abetu E. Knowledge and attitude of health professionals toward telemedicine in resource-limited settings: a cross-sectional study in North West Ethiopia. J Healthc Eng. 2018;2018:2389268.
Fisk M, Livingstone A, Pit SW. Telehealth in the Context of COVID-19: Changing Perspectives in Australia, the United Kingdom, and the United States. J Med Internet Res. 2020;22(6):e19264.
Lonergan PE, et al. Rapid utilization of telehealth in a comprehensive cancer center as a response to COVID-19: Cross-sectional analysis. 2020;22(7):e19322.
Albarrak AI, et al. Assessment of physician’s knowledge, perception and willingness of telemedicine in Riyadh region, Saudi Arabia. 2019.
Bisrat A. Knowledge and perception of health care providers towards telemedicine applications & benefits: a survey from Tikur Anbessa & Nekemete Hospitals. 2010. Addis Ababa University.
Ayatollahi H, Sarabi FZP, Langarizadeh M. Clinicians’ knowledge and perception of telemedicine technology. Perspect Health Inf Manag. 2015;12(Fall):1c.
Albarrak AI, et al. Assessment of physician’s knowledge, perception and willingness of telemedicine in Riyadh region, Saudi Arabia. J Infect Public Health. 2019.
Armfield NR, Donovan T, Smith AC. Clinicians’ perceptions of telemedicine for remote neonatal consultation. Stud Health Technol Inform. 2010;161:1–9.
Estai M, Kruger E, Tennant M. Perceptions of Australian dental practitioners about using telemedicine in dental practice. Br Dent J. 2016;220(1):25–9.
Haleem A, et al. Telemedicine for healthcare: Capabilities, features, barriers, and applications. Sensors International. 2021;2:100117.
Getachew E, Woldeamanuel Y, Manyazewal T. Digital health interventions in the clinical care and treatment of tuberculosis and hiv in central Ethiopia: An initial provider perceptions and acceptability study using the unified theory of acceptance and use of technology model. Int J Mycobacteriol. 2022;11(1):1.
Gebre AB. Knowledge and perception of health care providers towards telemedicine applications & benefits: A survey from Tikur Anbessa & Nekemete Hospitals. 2010. Addis Ababa University.
Ranjbar H, et al. Iranian clinical nurses’ and midwives’ attitudes and awareness towards telenursing and telehealth: a cross-sectional study. Sultan Qaboos Univ Med J. 2021;21(1):e50.
Hastall MR, Dockweiler C, Mühlhaus J. Achieving end user acceptance: Building blocks for an evidence-based user-centered framework for health technology development and assessment. in International Conference on Universal Access in Human-Computer Interaction. Springer; 2017.
Elhadi M, et al. Telemedicine awareness, knowledge, attitude, and skills of health care workers in a low-resource country during the COVID-19 pandemic: cross-sectional study. J Med Internet Res. 2021;23(2):e20812.
Wernhart A, Gahbauer S, Haluza D. eHealth and telemedicine: Practices and beliefs among healthcare professionals and medical students at a medical university. PLoS One. 2019;14(2):e0213067.
Oyediran KA, Makinde OA, Adelakin O. The role of telemedicine in addressing access to sexual and reproductive health services in sub-Saharan Africa during the COVID-19 pandemic. Afr J Reprod Health. 2020;24(2):49–55.
Hassan A, et al. Global survey on telemedicine utilization for movement disorders during the COVID-19 pandemic. Mov Disord. 2020;35(10):1701–11.
Khan I, Dhanalakshami M, Naveena J. Effectiveness of SIM on knowledge Regarding telemedicine among the staff nurses. Int J Nurs. 2015;1(2):1–15.
Sharma M, et al. Tele-ophthalmology: Need of the hour. Indian J Ophthalmol. 2020;68(7):1328.
Bali S. Barriers to development of telemedicine in developing countries, in Telehealth. IntechOpen; 2018.
Hazza J, Lahrech A. Health care professionals’ social media behavior and the underlying factors of social media adoption and use: quantitative study. J Med Internet Res. 2018;20(11):e12035.
Mulrennan S, Colt H. Medical information and social media in the time of COVID-19. Respirology. 2020;25(6):578.
Neely S, Eldredge C, Sanders R. Health information seeking behaviors on social media during the COVID-19 pandemic among American social networking site users: survey study. J Med Internet Res. 2021;23(6):e29802.
Merchant RM, Lurie N. Social media and emergency preparedness in response to novel coronavirus. JAMA. 2020;323(20):2011–2.
Merchant RM. Evaluating the potential role of social media in preventive health care. JAMA. 2020;323(5):411–2.
Acknowledgements
We would like to acknowledge the Ethiopia Ministry of Health, Ethiopia Midwife Association, Addis Ababa administration health bearua, and head of health facility administrators for their permission, data collectors, and study participants for their support in the process of data collection.
Guarantor declaration statement
Not applicable.
Funding
The funding body has no role in the design of the study and collection, analysis, interpretation of the data, writing the manuscript, and publication as well.
Author information
Authors and Affiliations
Contributions
BT substantially contributed to the conception and design, analysis, and interpretation of the study. MB, AW, SB, AS, MK, and HM were involved in the analysis and participated in the write-up of the article. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical clearance was obtained from the Ethiopian midwife association's ethical review committee on behalf of MOH, and support letters from the Addis Ababa health bureau and MOH were obtained with approval number EMwA-IRB/001–2020. Written informed consent was obtained from each study participant after telling the objective of the study. All methods were performed in accordance with the relevant guidelines and regulations. The data collection procedure was anonymous.
Consent for publication
Not applicable.
Competing interests
All authors reported no conflicts of interest in this work. The authors followed all ethical principles of scholarship in the preparation, data collection, and analysis; the authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Assaye, B.T., Belachew, M., Worku, A. et al. Perception towards the implementation of telemedicine during COVID-19 pandemic: a cross-sectional study. BMC Health Serv Res 23, 967 (2023). https://doi.org/10.1186/s12913-023-09927-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-023-09927-1