Abstract
Background
Polycystic ovary syndrome (PCOS) is a prevalent hormonal disorder affecting 5–15% of women of reproductive age, characterized by ovulatory dysfunction, hyperandrogenism, and polycystic ovarian morphology. PCOS is associated with metabolic disturbances such as dyslipidemia, insulin resistance (IR), and an increased risk of type 2 diabetes (T2DM) and cardiovascular disease.
Objective
The aim of this study is to apply new anthropometric indices [body adiposity index (BAI), visceral adiposity Index (VAI), lipid accumulation product (LAP), body roundness index (BRI), a body shape index (ABSI)] and new atherogenic indices [Castelli index-I, Castelli index-II, atherogenic risk of plasma (AIP), atherogenic coefficient (AC), lipoprotein combined index (LCI), triglycerides to high-density lipoprotein cholesterol (TG/HDL-C) ratio, metabolic score for insulin resistance (METS-IR), triglyceride glucose (TyG) index, triglyceride glucose-dody mass (TyG-BMI) index, triglyceride glucose-waist circumference (TyG-WC) index] metabolic score of insulin resistance to patients with PCOS.
Methods
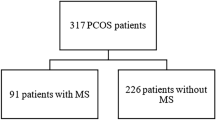
A retrospective analysis was conducted on 248 women diagnosed with PCOS based on the 2003 Rotterdam criteria. Anthropometric measurements, biochemical parameters, and atherogenic indices were collected from patient records. Statistical analyses were performed using Statistical Package for the Social Sciences software version 28.0.
Results
Significant correlations were found between fasting glucose and various anthropometric indices, such as Body mass index (BMI), waist-height ratio (WHtR), and BAI, indicating a link between adiposity and glucose metabolism in PCOS. Atherogenic indices like Castelli’s risk indices, AIP, and AC showed positive correlations with glucose and insulin levels, reinforcing their role in assessing cardiovascular risk. Novel indices such as METS-IR and TyG demonstrated strong correlations with both glucose and insulin profiles, highlighting their potential as reliable markers for IR and cardiometabolic risk.
Conclusion
The study underscores the importance of using a range of anthropometric and atherogenic indices for comprehensive metabolic assessment in women with PCOS. Indices like METS-IR and TyG offer valuable insights into insulin sensitivity and cardiovascular risk, potentially aiding in better management and prognosis of PCOS.
Similar content being viewed by others
Introduction
Polycystic ovary syndrome (PCOS) is a common and complex hormonal disorder affecting women of reproductive age, with a prevalence of approximately 5–15% [1]. It is characterized by ovulatory dysfunction, hyperandrogenism, and polycystic ovarian morphology. In addition, PCOS can lead to dyslipidemia, hyperinsulinemia, insulin resistance (IR), impaired glucose metabolism, type 2 diabetes (T2DM), metabolic syndrome, infertility, and oxidative stress disorders [2,3,4]. Women with PCOS have a higher risk of cardiovascular disease than other women. In particular, factors such as insulin resistance and metabolic syndrome can increase the risk of heart disease and stroke.
The pathogenesis of PCOS is complex and its etiology remains incompletely understood. Numerous studies have investigated the mechanisms of metabolic dysregulation (glucose and lipids) and inflammatory mechanisms in the pathogenesis of PCOS. IR is now a well-known feature of PCOS and, along with hypertension and dyslipidemia, increases the risk of cardiovascular and cerebrovascular events. These risk factors are further exacerbated by central obesity and metabolic syndrome, which are present in most women with PCOS [5, 6]. Almost 55% of women suffering from PCOS also have concurrent obesity [7]. Because the high IR in PCOS makes it easier to gain weight and obesity is frequently seen in these patients. Obesity can have a negative impact on PCOS, which can place additional burden on metabolic health.
Many studies have shown that women with PCOS have significantly higher levels of triglyceride to high-density lipoprotein (HDL) cholesterol ratio, indicating an important association with IR and cardiometabolic risk factors [8, 9]. Lipid indices are highly correlated with impaired insulin metabolism and hyperandrogenemia [10, 11]. A study by Zheng et al. indicated that new metabolic lipid indices (TyG index - triglyceride glucose index; TyG-BMI index - triglyceride-body mass index; TyG-WC index - triglyceride-waist circumference index) are useful in the early identification of prediabetes risk [12]. Given that adipose tissues secrete adipokines, inflammatory cytokines, and reactive oxygen species, leading to various metabolic disorders, such indices may be better predictors of IR than the triglyceride glucose (TyG) index alone [13, 14]. Additionally, a new non-insulin-based score, METS-IR (Metabolic Score for Insulin Resistance), may be useful in assessing insulin sensitivity and detecting IR in patients at risk of developing T2DM [15]. Therefore, METS-IR, along with the lipoprotein combined index (LCI), a new risk determinant for coronary artery disease (CAD), are promising scores for evaluating cardiometabolic risk in women with PCOS [16].
Adiposity plays a significant role in the prevention and management of PCOS. Anthropometric indices such as waist-hip ratio (WHR), waist-height ratio (WHtR), visceral adiposity index (VAI), body adiposity index (BAI), lipid accumulation product (LAP), body roundness index (BRI), and a body shape index (ABSI) may serve as indicators of adipose tissue abnormalities and cardiovascular disease risk in patients with PCOS [17, 18].
The aim of this study is to apply new anthropometric indices (BAI, VAI, LAP, BRI, ABSI) and new atherogenic indices [Castelli index-I, Castelli index-II, atherogenic risk of plasma (AIP), atherogenic coefficient (AC), lipoprotein combined index (LCI), triglycerides to HDL-Cholesterol ratio (TG/HDL-C ratio), metabolic score of insulin resistance (METS-IR), triglyceride glucose index (TyG index), triglyceride glucose-body mass index (TyG-BMI index), triglyceride glucose-waist circumference index (TyG-WC index)] to patients with PCOS. Additionally, an attempt was made to evaluate the significance of atherogenic indices in PCOS patients’ assessments.
Material method
Study group
This study was conducted retrospectively at Mardin Training and Research Hospital, reviewing patient records from 2022 to 2023. A total of 248 women diagnosed with PCOS according to the 2003 Rotterdam criteria were included in the study. The sample size was calculated using the formula recommended in a paper by Hajian-Tilaki [19].
2003 Rotterdam Criteria.
-
1)
Oligo-ovulation or anovulation.
-
2)
Clinical and/or biochemical hyperandrogenism.
-
3)
Polycystic ovaries seen on ultrasound (12 or more follicles 2–9 mm in size).
PCOS was diagnosed if at least two of these three criteria were met.
Exclusion Criteria: The exclusion criteria were as follows: refusal to participate in the study; pregnancy; hemolyzed samples; use of hormonal contraceptives, glucocorticosteroids, oral steroids, lipid-lowering medications, or drugs affecting glucose metabolism; previously diagnosed and treated diabetes; decompensated thyroid disorders; diseases associated with androgen excess (congenital or late-onset congenital adrenal hyperplasia, hyperprolactinemia, Cushing’s disease/syndrome, androgen-secreting tumors, idiopathic hirsutism); depressive disorders and treatment for depression.
Laboratory measurements and indices
Patient records from 2022 to 2023 were retrospectively reviewed. Demographic data (height, weight, waist circumference, hip circumference) and laboratory results (fasting glucose, fasting insulin, HDL-C, triglycerides, LDL-C (low-density lipoprotein cholesterol)) were collected from patient records. For this study, no additional blood was drawn from patients beyond what was required for their diagnosis and follow-up.
-
The value of the Homeostatic Model Assessment for Insulin Resistance (HOMA-IR) index was calculated using the following formula:
HOMA-IR = fasting insulin (mU/L) × fasting glucose (mmol/L) / 22.5 [20].
-
The value of METS-IR (Metabolic Score for Insulin Resistance) was calculated as follows:
METS-IR = (In ((2 x fasting glucose) (mU/L) + TG (mg/dL) x Body mass index)/(ln (HDL-C) (mg/dL)) [21].
-
The TyG index was calculated using the following formula:
ln[fasting glucose (mg/dL) x TG (mg/dL)/2] [20].
-
The TyG-BMI index is defined as follows:
ln[fasting glucose (mg/dL) x fasting triglycerides (mg/dL)/2] x BMI [22].
-
TyG-WC is defined as:
ln[fasting glucose (mg/dL) x TG (mg/dL)/2] x WC [22].
-
LCI was calculated using the following formula:
((TC, Total Cholesterol, (mg/dL) × TG (mg/dL) × LDL-C (mg/dL))/HDL-C (mg/dL)) [23].
-
Castelli risk index-I was calculated according to the formula = (TC/HDL-C) [10].
-
Castelli risk index-II was calculated according to the formula = (LDL-C/HDL-C) [10].
-
Atherogenic coefficient (AC) was calculated according to the formula = ((TC-HDL-C)/HDL-C) [10].
-
The atherogenic index (AIP) of plasma was calculated according to the formula = (log(TG/HDL-C)) [10].
-
The ratio of triglyceride to HDL-cholesterol was calculated according to the formula = (TG/HDL-C) [10].
Anthropometric parameters were measured using standard methods. These measurements included body weight [kg], height [cm], waist circumference [cm], and hip circumference [cm].
-
Body mass index (BMI) is calculated according to the following formula: BMI = body weight [kg]/height [m]2 [24].
-
Waist-to-hip ratio (WHR) was calculated according to the following formula: WHR = waist circumference [cm]/hip circumference [cm] [25].
-
Waist-height ratio (WHtR) was calculated according to the following formula: WHtR = waist circumference [cm]/height [cm] [25].
-
Body adiposity index (BAI) was calculated according to the following formula: BAI = ((hip circumference [cm]/height [m]1.5)-18) [26].
-
Visceral Adiposity Index (VAI) was calculated according to the following formula: VAI = [waist circumference [cm]/(36.58 + (1.89 × BMI))] × (triglyceride concentration [triglyceride]/0.81) × (1.52/ HDL concentration [mg/dL]) [20].
-
Lipid Accumulation Product (LAP) was calculated according to the following formula: LAP = (waist circumference [cm] – 58) × (triglyceride concentration [triglyceride]) [20].
-
Body Roundness Index (BRI) was calculated according to the following formula: BRI = 365.2 − 365.5 × √(1 − (((WC/2π)2)/[(0.5 × height)]2) [27].
-
A Body Shape Index (ABSI) was calculated according to the following formula: ABSI = WC[m]/[(BMI)2/3) × (height [m])1/2)] [27].
Statistical analysis
The data obtained in the study will be analyzed using SPSS software version 28.0. The Shapiro-Wilk test was used to assess the distribution of the data. Continuous variables are expressed as mean ± standard deviation (for normally distributed data) or median and interquartile range (for non-normally distributed data). For normally distributed data, the Student’s t-test will be used, while the Mann-Whitney U test will be used for non-parametric data. Correlation between variables will be evaluated using the Pearson correlation coefficient (for normally distributed data) and Spearman’s rank correlation coefficient (for non-normally distributed data). A p-value of less than 0.05 will be considered statistically significant.
Result
The anthropometric measurements, biochemical parameters, and atherogenic index results of women diagnosed with PCOS are presented in Table 1.
The relationships between anthropometric measurements, atherogenic indices, and glucose profile in the study group are presented in Table 2.
Upon examining Table 2, a low positive correlation was found between fasting glucose (mmol/L) and weight, waist circumference, hip circumference, BMI, WHR, WHtR, BAI, VAI, LAP, BRI, Castelli’s risk index-I, Castelli’s risk index-II, AIP, AC, LCI, TG/HDL-C, and TyG index; a moderate positive correlation was found between fasting glucose and METS-IR, TyG-BMI, and TyG-waist circumference index (p < 0.001, p < 0.01, p < 0.05), with no significant relationship observed between fasting glucose and ABSI (p > 0.05).
60 min glucose (mg/dL) showed a low positive correlation with weight, WHR, VAI, LAP, Castelli’s risk index-I, Castelli’s risk index-II, AIP, AC, LCI, and TG/HDL-C; and a moderate positive correlation with waist circumference, hip circumference, BMI, WHtR, BAI, BRI, METS-IR, TyG index, TyG-BMI, and TyG-waist circumference index (p < 0.001, p < 0.01), with no significant relationship observed with ABSI (p > 0.05).
120 min glucose (mg/dL) demonstrated a low positive correlation with WHR, VAI, Castelli’s risk index-I, Castelli’s risk index-II, AIP, AC, TG/HDL-C, and TyG index; and a moderate positive correlation with weight, waist circumference, hip circumference, BMI, WHtR, BAI, LAP, BRI, LCI, METS-IR, TyG-BMI, and TyG-waist circumference index (p < 0.001, p < 0.01, p < 0.05), with no significant relationship observed with ABSI (p > 0.05).
The relationships between anthropometric measurements, atherogenic indices, and insulin profile in the study group are presented in Table 3.
Upon examining Table 3, a low positive correlation was found between fasting insulin (mU/L) and WHR, LAP, Castelli’s risk index-I, Castelli’s risk index-II, AC and LCI; a moderate positive correlation was found between fasting insulin and weight, waist circumference, hip circumference, BMI, WHtR, BAI, BRI, METS-IR TyG-BMI and TyG-waist circumference index (p < 0.001, p < 0.01, p < 0.05). No significant relationship was observed with VAI, ABSI, AIP, TG/HDL-C, TyG Index (p > 0.05).
60 min insulin (mU/L) showed a low positive correlation with WHR, VAI, Castelli’s risk index-I, Castelli’s risk index-II, AIP, AC, TG/HDL-C, and TyG index; and a moderate positive correlation with weight, waist circumference, hip circumference, BMI, WHtR, BAI, LAP, BRI, LCI, METS-IR, TyG-BMI, and TyG-waist circumference index (p < 0.001, p < 0.01, p < 0.05). No significant relationship was observed with ABSI (p > 0.05).
The relationships between anthropometric measurements, atherogenic indices, and hemoglobin A1c (HbA1c) and HOMA-IR index in the study group are presented in Table 4.
Upon examining Table 4, a low positive correlation was found between HbA1c (%) and waist circumference, hip circumference, BMI, WHR, WHtR, BAI, LAP, BRI, Castelli’s risk index-I, Castelli’s risk index-II, AC, LCI, TG/HDL-C, METS-IR, TyG index, TyG-BMI, and TyG-waist circumference index; a moderate positive correlation was found with weight; and a low negative correlation was found with ABSI (p < 0.001, p < 0.01, p < 0.05). No significant relationship was observed with VAI, AIP, and TG/HDL-C (p > 0.05).
For the HOMA-IR index, a low positive correlation was found with hip circumference, BAI, LAP, Castelli’s risk index-I, Castelli’s risk index-II, AIP, AC, LCI, TG/HDL-C, TyG index, and TyG-waist circumference index; a moderate positive correlation was found with weight, waist circumference, BMI, WHtR, BRI, and METS-IR (p < 0.001, p < 0.01, p < 0.05). No significant relationship was observed with WHR, VAI, and ABSI (p > 0.05).
Discussion
The findings of this study provide valuable insights into the relationships between various anthropometric, biochemical, and atherogenic indices and their relevance to glucose and insulin profiles in women with PCOS. This study reinforces the importance of comprehensive metabolic assessment in managing PCOS and highlights the potential utility of newer indices like METS-IR, TyG, and LCI in clinical practice.
Anthropometric indices and glucose profile
The positive correlations between fasting glucose and anthropometric indices such as BMI, WHtR, and BAI indicate that central and overall adiposity are significant contributors to glucose dysregulation in PCOS patients. This aligns with previous studies that have shown a strong link between obesity and impaired glucose metabolism in PCOS [1, 5]. The lack of significant correlation with ABSI suggests that this index may not be as sensitive in detecting metabolic disturbances associated with PCOS compared to other measures of adiposity.
Atherogenic indices and cardiometabolic risk
Depending on the population being investigated and the particular cardiovascular risk assessment recommendations being followed, cut off values for atherogenic indices may change. Nonetheless, it is acknowledged that having high values for these indices increases the risk of cardiovascular illnesses [28]. Therefore, in PCOS patients, there are no established cutoff values for atherogenic indices, nor, although some research on these patients indicates that their lipid profiles alter and their cardiovascular risk factors rise [16, 17]. In the current study, atherogenic indices such as Castelli’s risk index-I and II, AIP, and AC showed positive correlations with both fasting glucose and insulin levels, reinforcing their role in assessing cardiovascular risk in PCOS patients. These findings are consistent with the understanding that dyslipidemia is a common feature in PCOS and contributes to the heightened cardiovascular risk [2, 3]. In the studies of Zheng et al. and Ahn et al., the novel indices, particularly the TyG index and its derivatives (TyG-BMI, TyG-WC), demonstrated robust correlations with glucose and insulin parameters, underscoring their utility as predictors of insulin resistance and cardiometabolic risk [12, 20]. Contrary to these studies in the literature, in general, all the relationships between anthropometric indices and atherogenic indices with glucose and insulin profiles were weak or moderate in the current study. Not a single one was strong.
Compared to conventional endocrinological testing, we think that atherogenic index values can offer patients with PCOS more useful information. Thus, additional research on these subject encounters to be done. Early diagnosis can be accomplished and patient risk values for cardiovascular diseases can be ascertained if the cutoff values of the atherogenic indices in PCOS patients can be established for each group.
Insulin resistance and metabolic indices
The significant correlations between METS-IR and both glucose and insulin profiles highlight its potential as a reliable marker for insulin resistance in PCOS. In parallel, in the study of Bello-Chavolla et al., it was stated that METS-IR, which combines both metabolic and anthropometric parameters, provides a comprehensive evaluation of insulin sensitivity [15]. This result is particularly valuable in PCOS, because insulin resistance plays a central role in the pathophysiology contributing to the risk of developing T2DM and cardiovascular disease [6, 13].
Clinical implications
The results of this study suggest that incorporating a range of anthropometric and atherogenic indices into routine clinical assessment could enhance the identification and management of metabolic and cardiovascular risks in women with PCOS. Indices such as the TyG and METS-IR, which are simple to calculate and do not require complex testing, could be particularly useful in resource-limited settings.
Limitations and future research
This study has several limitations, including its retrospective design and reliance on existing patient records, which may introduce selection bias and limit the generalizability of the findings. This study also did not take into account other potential risk factors for cardiovascular diseases, such as diet and physical activity. Furthermore, just one group in one area was included in the study, and more investigation is required to confirm these results in groups with greater diversity. Prospective cohort studies with larger sample sizes and longitudinal follow-up can be conducted to determine the predictive value of these indices for long-term metabolic and cardiovascular outcomes in PCOS. Spearman’s rank correlation test was used in this study, and it should be noted that this method cannot predict causality.
Conclusion
In conclusion, this study highlights the significant relationships between various metabolic indices and glucose and insulin profiles in women with PCOS. The findings support the use of newer indices such as METS-IR, TyG, and LCI as effective tools for assessing metabolic and cardiovascular risk in PCOS. Incorporating these indices into clinical practice could improve the management and prognosis of PCOS, ultimately leading to better health outcomes for affected women.
Data availability
The datasets used in this study are available from the corresponding author upon request.
Abbreviations
- ABSI:
-
A Body Shape Index
- AC:
-
Atherogenic Coefficient
- AIP:
-
Atherogenic Risk of Plasma
- BAI:
-
Body Adiposity Index
- BMI:
-
Body Mass Index
- BRI:
-
Body Roundness Index
- CAD:
-
Coronary Artery Disease
- HbA1c:
-
Hemoglobin A1c
- HDL:
-
High-Density Lipoprotein
- HOMA-IR:
-
Homeostatic Model Assessment for Insulin Resistance
- IR:
-
Insulin Resistance
- LAP:
-
Lipid Accumulation Product
- LCI:
-
Lipoprotein Combined Index
- LDL:
-
Low-Density Lipoprotein
- METS-IR:
-
Metabolic Score for Insulin Resistance
- OGTT:
-
Oral Glucose Tolerance Test
- PCOS:
-
Polycystic Ovary Syndrome
- SPSS:
-
Statistical Package for the Social Sciences
- T2DM:
-
Type 2 Diabetes Mellitus
- TC:
-
Total Cholesterol
- TG/HDL-C:
-
Triglycerides to High-Density Lipoprotein Cholesterol Ratio
- TyG:
-
Triglyceride Glucose Index
- TyG-BMI:
-
Triglyceride Glucose-Body Mass Index
- TyG-WC:
-
Triglyceride Glucose-Waist Circumference Index
- VAI:
-
Visceral Adiposity Index
- WC:
-
Waist Circumference
- WHR:
-
Waist-to-Hip Ratio
- WHtR:
-
Waist-Height Ratio
References
March WA, Moore VM, Willson KJ, Phillips DI, Norman RJ, Davies MJ. The prevalence of polycystic ovary syndrome in a community sample assessed under contrasting diagnostic criteria. Hum Reprod. 2010;25(2):544–51.
Liu Q, Xie Y-j, Qu L-h, Zhang M-x. Mo Z-c. Dyslipidemia involvement in the development of polycystic ovary syndrome. Taiwan J Obstet Gynecol. 2019;58(4):447–53.
Lathia T, Joshi A, Behl A, Dhingra A, Kalra B, Dua C, et al. A practitioner’s Toolkit for Polycystic Ovary Syndrome Counselling. Indian J Endocrinol Metabol. 2022;26(1):17–25.
Sachdeva G, Gainder S, Suri V, Sachdeva N, Chopra S. Comparison of the different PCOS phenotypes based on clinical metabolic, and hormonal profile, and their response to clomiphene. Indian J Endocrinol Metabol. 2019;23(3):326–31.
Tao L-C, Xu J-n, Wang T-t, Hua F, Li J-J. Triglyceride-glucose index as a marker in cardiovascular diseases: landscape and limitations. Cardiovasc Diabetol. 2022;21(1):68.
Guo F, Gong Z, Fernando T, Zhang L, Zhu X, Shi Y. The lipid profiles in different characteristics of women with PCOS and the interaction between dyslipidemia and metabolic disorder states: a retrospective study in Chinese population. Front Endocrinol. 2022;13:892125.
Aggarwal S, Pandey K. Early identification of PCOS with commonly known diseases: obesity, diabetes, high blood pressure and heart disease using machine learning techniques. Expert Syst Appl. 2023;217:119532.
Ulutaş F, Cander S, Gül ÖÖ. The association between triglycerides/high-density lipoprotein cholesterol ratio, insulin resistance, and serum androgen levels in patients with polycystic ovary syndrome. Eur Res J. 2022;8(2):275–81.
Song DK, Lee H, Sung Y-A, Oh J-Y. Triglycerides to high-density lipoprotein cholesterol ratio can predict impaired glucose tolerance in young women with polycystic ovary syndrome. Yonsei Med J. 2016;57(6):1404–11.
Kamoru AA, Japhet OM, Adetunji AD, Musa MA, Hammed OO, Akinlawon AA, et al. Castelli risk index, atherogenic index of plasma, and atherogenic coefficient: emerging risk predictors of cardiovascular disease in HIV-treated patients. Saudi J Med Pharm Sci. 2017;4929:1101–10.
Liu Z, He H, Dai Y, Yang L, Liao S, An Z, Li S. Comparison of the diagnostic value between triglyceride-glucose index and triglyceride to high-density lipoprotein cholesterol ratio in metabolic-associated fatty liver disease patients: a retrospective cross-sectional study. Lipids Health Dis. 2022;21(1):55.
Zheng S, Shi S, Ren X, Han T, Li Y, Chen Y, et al. Triglyceride glucose-waist circumference, a novel and effective predictor of diabetes in first-degree relatives of type 2 diabetes patients: cross-sectional and prospective cohort study. J Translational Med. 2016;14:1–10.
Lee J, Kim B, Kim W, Ahn C, Choi HY, Kim JG, et al. Lipid indices as simple and clinically useful surrogate markers for insulin resistance in the US population. Sci Rep. 2021;11(1):2366.
Klöting N, Fasshauer M, Dietrich A, Kovacs P, Schön MR, Kern M, et al. Insulin-sensitive obesity. Am J Physiology-Endocrinology Metabolism. 2010;299(3):E506–15.
Bello-Chavolla OY, Almeda-Valdes P, Gomez-Velasco D, Viveros-Ruiz T, Cruz-Bautista I, Romo-Romo A, et al. METS-IR, a novel score to evaluate insulin sensitivity, is predictive of visceral adiposity and incident type 2 diabetes. Eur J Endocrinol. 2018;178(5):533–44.
Jabczyk M, Nowak J, Jagielski P, Hudzik B, Kulik-Kupka K, Włodarczyk A, et al. Metabolic deregulations in patients with polycystic ovary syndrome. Metabolites. 2023;13(2):302.
Naghshband Z, Kumar L, Mandappa S, Murthy ASN, Malini SS. Visceral adiposity index and lipid accumulation product as diagnostic markers of metabolic syndrome in south indians with polycystic ovary syndrome. J Hum Reproductive Sci. 2021;14(3):234–43.
Gönülalan G, Saçkan F. The importance of new anthropometric measurements in detecting cardio metabolic risk and insulin resistance in patients with polycystic ovary syndrome: single center experience. Türkiye Diyabet ve Obezite Dergisi. 2021;5(1):25–32.
Hajian-Tilaki K. Sample size estimation in diagnostic test studies of biomedical informatics. J Biomed Inform. 2014;48:193–204.
Ahn N, Baumeister SE, Amann U, Rathmann W, Peters A, Huth C, et al. Visceral adiposity index (VAI), lipid accumulation product (LAP), and product of triglycerides and glucose (TyG) to discriminate prediabetes and diabetes. Sci Rep. 2019;9(1):9693.
Yoon J, Jung D, Lee Y, Park B. The metabolic score for insulin resistance (METS-IR) as a predictor of incident ischemic heart disease: a longitudinal study among Korean without diabetes. J Personalized Med. 2021;11(8):742.
Khamseh ME, Malek M, Abbasi R, Taheri H, Lahouti M, Alaei-Shahmiri F. Triglyceride glucose index and related parameters (triglyceride glucose-body mass index and triglyceride glucose-waist circumference) identify nonalcoholic fatty liver and liver fibrosis in individuals with overweight/obesity. Metab Syndr Relat Disord. 2021;19(3):167–73.
Si Y, Liu J, Han C, Wang R, Liu T, Sun L. The correlation of retinol-binding protein-4 and lipoprotein combine index with the prevalence and diagnosis of acute coronary syndrome. Heart Vessels. 2020;35:1494–501.
Weir CB, Jan A. BMI classification percentile and cut off points. 2019.
Consultation WE. Waist circumference and waist-hip ratio. Report of a WHO Expert Consultation Geneva. World Health Organ. 2008;2008:8–11.
Bergman RN, Stefanovski D, Buchanan TA, Sumner AE, Reynolds JC, Sebring NG, et al. A better index of body adiposity. Obesity. 2011;19(5):1083–9.
Głuszek S, Ciesla E, Głuszek-Osuch M, Kozieł D, Kiebzak W, Wypchło Ł, Suliga E. Anthropometric indices and cut-off points in the diagnosis of metabolic disorders. PLoS ONE. 2020;15(6):e0235121.
Kim SH, Cho YK, Kim Y-J, Jung CH, Lee WJ, Park J-Y, et al. Association of the atherogenic index of plasma with cardiovascular risk beyond the traditional risk factors: a nationwide population-based cohort study. Cardiovasc Diabetol. 2022;21(1):81.
Acknowledgements
None.
Funding
No specific funding for this research.
Author information
Authors and Affiliations
Contributions
Study conception and design: EU Designed and prepared the text messages: EU, OT, MI and MAPerformed the analysis: EUWrote the Manuscript: EU and MA Collected the data: OT, ES and DFAll of the authors reviewed the results and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The objectives of the study were explained in detail to the study participants. The collection of demographic information and the data obtained from all patients participating in this research were done after obtaining informed consent and willingness to participate in the study. Also, all the information remained confidential and the results were published anonymously and only statistically. Ethical approval for the study was obtained from the Ethics Committee of Mardin Artuklu University (Decision number: 2024/3–21). The authors confirm that all experiments were performed following the relevant Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Uysal, E., Tammo, O., Soylemez, E. et al. Significance of measuring anthropometric and atherogenic indices in patients with polycystic ovary syndrome. BMC Endocr Disord 24, 160 (2024). https://doi.org/10.1186/s12902-024-01701-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-024-01701-6