Abstract
Background
Schwannomas originating from the intravertebral canal rarely extend into the paravertebral region or form large masses. There are few reports on such medical cases, and their clinical diagnosis and management are poorly understood. Here, we report a case of an intraspinal schwannoma with a giant extraspinal mass in a middle-aged Chinese woman and the clinical implications of the symptoms, diagnosis, and treatment of thoracic vertebral schwannoma.
Case presentation
A 59-year-old female patient who presented with sudden lower limb numbness and difficulty in walking was referred to our department. Magnetic resonance imaging (MRI) revealed a tumor compressing the T11-T12 spinal canal and extensively invading the left thoracic cavity to form a giant paravertebral mass. Schwannoma was diagnosed after intraoperative pathological examination, in which tumor cells were immunoreactive to S100 and Sox10 but negative for smooth muscle actin (SMH). Intraspinal mass resection through the posterior approach and extraspinal chest mass resection under video-assisted thoracoscopy through the left lateral approach were performed simultaneously, and instrumentation was used to maintain thoracic spinal stability.
Conclusion
In patients with large schwannomas, customized treatment plans are crucial. Tailoring the approach to an individual’s specific condition by considering factors such as tumor size and location is essential for optimal outcomes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Schwannomas are indolent and benign neoplasms originating from Schwann cells in the peripheral nervous system and are predominantly found in nerve tissues adjacent to the brain and spinal cord [1]. Although it is the most common form of intradural extramedullary (IDEM) tumor, the presence of a schwannoma with giant paravertebral mass invasion is extremely rare [2]. Typically, surgical excision, which has favorable postoperative outcomes, is the first-line treatment for schwannomas. However, early diagnosis and intervention of schwannomas pose a challenge because of their benign nature, and the likelihood of misdiagnosis as other tumors is high. Recently, our hospital successfully treated a related case. This is the hospital’s first instance of an intradural schwannoma accompanied by a large extradural mass compressing the thoracic cavity. The primary purpose of this report is to present the symptoms, radiological characteristics, surgical approach, and prognosis of this patient, with the secondary purpose being to provide guidance to medical professionals encountering similar situations in the future.
Case report
Patient information
A 59-year-old Chinese woman visited our hospital with sudden weakness and numbness in her lower limbs without any obvious symptoms, accompanied by limited activity and hypoesthesia. She had experienced mild discomfort in her lower limbs for five months. The patient was in good health and had no family history of malignant disease or exposure to risk factors.
Clinical findings
The basic physical examination findings were normal and revealed a body temperature of 36.5 °C, pulse of 79/min, respiratory rate of 20/min, blood pressure of 97/68 mmHg, and no significant abnormality in her thoracolumbar movements. However, a detailed neurological examination demonstrated muscle weakness and numbness in the lower limbs, with a muscle power score of 3/5 for the hip flexors, knee extensors, ankle dorsiflexors, and great toe extensors bilaterally. Sensory function showed decreased sensation to light touch and pinprick in the L2-S1 dermatomes bilaterally. Reflex examination revealed normal patellar and Achilles reflexes, but hyporeflexia of the anus was noted. Muscle tone in the lower limbs was normal, without spasticity or rigidity. Additionally, the Kernig and Lasegue signs were negative, and there were no signs of upper motor neuron involvement.
Diagnostic assessment
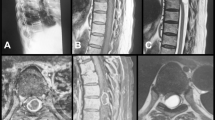
The initial radiological investigations commenced with a chest X-ray, which indicated the presence of an abnormal mass in the thoracic region. A computed tomography (CT) scan was subsequently performed to obtain a more detailed view of the mass and its extent. Comprehensive chest enhanced magnetic resonance imaging (MRI) revealed an intraspinal mass at the T11 level and a left thoracic cavity protrusion measuring approximately 10.2 × 7 × 3.8 cm originating from the T11-T12 level of the intravertebral foramen, along with pedicle destruction (Fig. 1). On the basis of these findings, differential diagnoses, including neurogenic tumors, metastatic disease, and infectious etiologies, were considered. Following this assessment, specific laboratory tests were conducted to evaluate tumor markers such as carcinoembryonic antigen (CEA), alpha-fetoprotein (AFP), and cancer antigen 125 (CA125). These tests yielded unremarkable results that helped narrow down the diagnosis to a likely benign schwannoma. The patient was subsequently transferred to the Orthopedic Division of the Spine Surgery Department for further treatment.
Therapeutic intervention
After careful consideration of the patient’s condition and consultation with her family members, a surgical plan was devised to separately remove the intraspinal and thoracic components of the schwannomas. The initial approach involved a posterior midline incision to perform a T11 laminectomy for tumor exposure within the spinal canal. Dissection and retraction of the paraspinal muscles were performed to visualize the lamina, followed by execution of the laminectomy and opening of the dura mater, revealing a mass measuring 5.2 × 3.4 × 2.7 cm in size. The tumor, which had invaded the left thoracic cavity and caused epidural compression, underwent meticulous dissection and complete resection. To ensure thoracic spinal stability, pedicle screw fixation from T10 to T12 was meticulously performed under fluoroscopic guidance for precise placement. Subsequently, a lateral position was adopted for thoracoscopic surgery to excise any remaining tumor in the left chest cavity. Intraoperatively, under thoracoscopy guidance, an adherent solid cystic mass measuring 9 × 8 × 8 cm was observed adjacent to the inferior lobe of the left lung. Complete resection without inadvertent injury to surrounding structures was accomplished through meticulous separation using an ultrasound knife technique. The excised tumor specimen underwent pathological examination, including immunohistochemistry (IHC) staining for Sox10 and S100 markers, which confirmed its benign nature as a schwannoma exhibiting associated cystic changes (Fig. 2).
Follow-up and outcomes
Postoperative outcomes were favorable, with significant improvement in neurological status noted in terms of bilateral lower limb muscle strength returning to 4/5 and resolution of previously reported numbness symptoms. The follow-up MRI conducted two years post-discharge revealed no signs indicative of tumor recurrence, whereas the radiological findings confirmed stable placement and functionality of the instrumentation supporting thoracic spine integrity throughout the recovery period (Fig. 3). The patient’s vital signs remained stable during the postoperative phase without reporting any substantial pain or discomfort. Regular follow-ups were advised for monitoring potential recurrence or complications. All the diagnosis and treatment processes are shown in Fig. 4.
Histological examination results. (A) Gross findings of the removed schwannoma. The mass appeared grey-white, grey-red and irregular two masses, the smaller one is 5.2 × 3.4 × 2.7 cm in size, and the larger one is 10.2 × 7 × 3.8 cm in size. (B) Sectional cells exhibited oval or waved nuclei and deep staining. (C) Immunohistochemistry showed that the tumor cells were Sox10(+), S100(3+) and SMA(-)
Discussion and conclusion
Schwannoma are frequently encountered benign tumors in the spinal canal that originate from Schwann cells, which are responsible for producing a myelin sheath that insulates peripheral nerves [2]. Despite their non-malignant nature, early and precise diagnosis presents a formidable challenge. Consequently, symptoms often manifest only when the tumor compresses nerves or spinal cord, resulting in dyskinesia, sciatica, and paresthesia [3,4,5]. This particular case posed a diagnostic dilemma due to the rarity of extensive tumor invasion into both intraspinal and extraspinal regions—an uncommon occurrences that poses significant challenges in clinical practice.
Our case involved a 59-year-old female with an extensive schwannoma spanning both intraspinal and extraspinal regions, necessitating a two-stage surgical approach. Unlike previous cases documented in the literature that primarily focus on either spinal or thoracic involvement alone, our case is unique because the schwannoma extended significantly into both areas simultaneously. For instance, Samman et al. [1] reported a case of an 80-year-old male with a cystic schwannoma at the T6–T7 level who underwent laminectomy for solely intraspinal schwannoma. Chu and Trager [3] presented a similar case of an intraspinal tumor at T9 managed through posterior laminectomy and tumor resection confined to intraspinal surgery. Kalsi et al. [6] successfully managed seven paraspinal schwannomas through thoracotomy using different approaches, while Lan et al. [7]. describe a one-stage combined surgery involving hemilaminectomy and posterolateral thoracotomy for schwannoma resection, providing valuable insights into the surgical methods selection. Zhou et al. [5] described a large paravertebral schwannoma extending into the spinal canal that required two-stage surgery: posterior laminectomy followed by thoracotomy, which aligns closely with our surgical method but highlights variability in approaches. In contrast, our case utilized a combined posterior and thoracoscopic (minimally invasive) approach. Saleemi et al. [4] also presented a giant 10 cm × 15 cm × 12 cm schwannoma in the thoracic cavity and chose the same approach for resection as we did. This method offers significant advantages, including better visualization of the surgical field with less tissue disruption, reduced intraoperative blood loss, minimized postoperative pain due to smaller incisions, maximized tumor resection, lower risk of complications such as infections and respiratory issues, while facilitating faster recovery time. The comprehensive description of these studies is presented in Table 1. Studies by Safaee et al. [8] and Conti et al. [9], emphasizing the importance of meticulous preoperative planning and multidisciplinary collaboration in managing complex schwannomas align well with our approach involving detailed imaging, precise surgical techniques, and staged operations to ensure complete tumor resection while preserving neurological function. This case underscores the necessity of advanced imaging modalities and a comprehensive diagnostic workup in patients presenting ambiguous neurological symptoms. The success of our approach is reflected in the patient’s improved neurological status and the absence of tumor recurrence at the two-year follow-up, validating the efficacy of tailored sequential surgical strategies for complex schwannomas.
In conclusion, the management of this giant intraspinal and extraspinal schwannoma underscores the significance of individualized treatment plans that take into account tumor dimensions, location, and patient-specific factors. Future research should prioritize the refinement of surgical techniques and postoperative care to further enhance outcomes in similar cases. The insights gained from comparing diverse surgical approaches and their respective outcomes will continue to advance our comprehension and management of intricate schwannomas.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- SMH:
-
Smooth muscle actin
- IDEM:
-
Intradural extramedullary
- VATS:
-
Video-assisted thoracoscopy
- IHC:
-
Immunohistochemistry
References
Samman AM, Bardeesi AM, Alzahrani MT. Thoracic cystic schwannoma: case report and review of literature. Spinal Cord Ser Cases. 2021;7(1):7.
Donner TR, Voorhies RM, Kline DG. Neural sheath tumors of major nerves. J Neurosurg. 1994;81(3):362–73.
Chu EC, Trager RJ. Thoracic Schwannoma as an unusual cause of sciatic Pain in the Chiropractic Office: a Case Report. Am J Case Rep. 2022;23:e938448.
Saleemi MS, Abdelwahab AOY, Abdelwahab MOY, George KJ. A case of a giant thoracic schwannoma. Surg Neurol Int. 2022;13:188.
Zhou Y, Liu CZ, Zhang SY, Wang HY, Nath Varma S, Cao LQ, Hou TT, Li X, Yao BJ. Giant schwannoma of thoracic vertebra: a case report. World J Clin Cases. 2021;9(36):11448–56.
Kalsi P, Zaidman N, Jain A, Casey ATH, Prezerakos G, Russo VM. Surgical Management of Giant thoracic paraspinal Schwannomas. World Neurosurg. 2021;149:e1155–65.
Lan ZG, Chen HF, Huang SQ, Pu Q. One-stage removal of a giant thoracic paraspinal shamrock-shaped schwannoma via modified hemilaminectomy and posterolateral thoracotomy. Spine Journal: Official J North Am Spine Soc. 2012;12(6):e8–11.
Safaee MM, Lyon R, Barbaro NM, Chou D, Mummaneni PV, Weinstein PR, Chin CT, Tihan T, Ames CP. Neurological outcomes and surgical complications in 221 spinal nerve sheath tumors. J Neurosurg Spine. 2017;26(1):103–11.
Conti P, Pansini G, Mouchaty H, Capuano C, Conti R. Spinal neurinomas: retrospective analysis and long-term outcome of 179 consecutively operated cases and review of the literature. Surg Neurol. 2004;61(1):34–43. discussion 44.
Acknowledgements
We acknowledge the assistance of the Editage editorial service for enhancing the manuscript.
Funding
The authors are grateful for the financial supports from the Natural Science Foundation of Jiangxi Province (grant no. 20171ACB21057, 20202BABL206034).
Author information
Authors and Affiliations
Contributions
Case diagnosis and treatment: P.D, Z.P. and Q.X. Literature review and research background: X.F., J.H., H.Y. Manuscript writing: X.F. Manuscript revision, supervision, and discussion: P.D., Q.X., X.F.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the institutional Ethics Committee of our hospital (IRB approval number: IIT2024458).
Consent for publication
The patient was informed of the study aims and provided written consent for the publication of her personal and clinical details, along with any identifying images.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Feng, X., Huang, J., Yu, H. et al. Resection of a giant intraspinal and extraspinal schwannoma with cystic change using a two-step surgery: a case report. BMC Musculoskelet Disord 25, 715 (2024). https://doi.org/10.1186/s12891-024-07821-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-024-07821-3