Abstract
Introduction
Giant extradural thoracic schwannomas are very rare tumors in the pediatric age group and often occur together with neurofibromatosis. Giant schwannomas span across more than two vertebral segments and have an extraspinal extension of over 2.5 cm. In this case, we report on a 5-year-old boy with a purely extradural giant schwannoma without accompanying neurofibromatosis.
Clinical presentation.
A 5-year-old male patient was admitted to the orthopedics and traumatology outpatient clinic with complaints of difficulty in walking following waist and left leg pain after falling from a chair. Contrast-enhanced spinal MRI and cranial MRI showed an extradural spinal lesion measuring 22 × 18 × 35 mm that pushed the spinal cord to the right at the T10-12 level and extended into the left foramen at the T11-12 level. The patient was operated. The tumor was removed completely by performing bilateral laminoplasty at the T10-11–12 levels. Histopathology result reported schwannoma.
Conclusion
Giant schwannomas are slow-growing tumors that rarely occur in childhood. In these patients, spinal traumas can lead to serious neurological deficits. Early diagnosis and successful surgery can prevent permanent neurological damage.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Giant extradural thoracic schwannomas are very rare tumors in the pediatric age group. The most common age range is 40 to 70 years [1]. Pediatric spinal schwannomas constitute 2.5–4% of all pediatric spinal tumors [2]. Spinal schwannomas were classified by Sridhar et al. into five types according to their size and invasion area. According to this definition, giant schwannomas span across more than two vertebral segments and have an extraspinal extension of over 2.5 cm [3]. Seventy percent of spinal schwannomas arise from sensory nerves and rarely arise from motor nerves. Therefore, in the late stages of the disease, loss of strength begins as a result of pressure on the motor nerves [4]. Schwannomas and neurofibromatosis (NF 2) often occur together because they both derive from Schwann cells [4, 5].
Case presentation
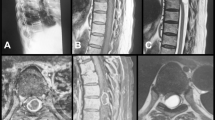
A 5-year-old male patient was admitted to the orthopedics and traumatology outpatient clinic with complaints of difficulty in walking following waist and left leg pain after falling from a chair 20 days ago. Since no orthopedic pathology was detected in the examination and tests, he was referred to the pediatric neurology department. Contrast-enhanced spinal MRI and cranial MRI showed an extradural spinal lesion measuring 22 × 18 × 35 mm that pushed the spinal cord to the right at the T10-12 level and extended into the left foramen at the T11-12 level. (Fig. 1A). Cranial MRI result came out to be normal. There was no evidence of lesion which may belong to neurofibromatosis. EMG results show that peripheral nerve motor sensory transmission and responses were normal. In the neurological examination, left lower extremity deep tendon reflexes were hyperactive, muscle strength examination was found iliopsoas muscle 3/5, quadriceps femoralis muscle 4/5, biceps femoralis muscle 3/5, tibialis anterior muscle 3/5, gastrocnemius muscle 3/5 on the left side. No “café au lait spot” was seen during the examination.
Preoperative and postoperative magnetic resonance imaging (MRI). The contrast-enhanced T1-weighted sagittal (A), T2-weighted sagittal (B), and axial T2-weighted (C) images demonstrate compression of the spinal cord by a lesion showing homogeneous contrast enhancement at the T10-12 vertebral level. The axial T2-weighted image (C) showing that the lesion extends into the neural foramen (dumbbell shape). The postoperative contrast-enhanced T1-weighted sagittal (D), T2-weighted sagittal (E), and contrast-enhanced T1-weighted axial (F) images showing that the lesion has been completely resected
The patient who was planned to have a surgical operation was transferred to the neurosurgery department. Following the recommendation of the pediatric neurology department, a pulse dose of 30 mg/kg/day methylprednisolone for 5 days was followed by a single dose of methylprednisolone, 1 mg/kg/day divided into four doses for 4 days administered. 2 mg/kg/day for the next 6 days and 1 mg/kg/day for the following next 3 days administered as a single dose per day. The patient was operated on during the pulse steroid treatment period. Laminectomy of the T10, T11, and T12 vertebrae was performed using an ultrasonic bone scalpel to minimize bone loss. The laminae of these three levels were removed in their entirety along with the spinous processes. After laminectomy and excision of the ligamentum flavum at the T10, T11, and T12 vertebral levels, the lesion was visualized. The lesion was dissected from the dura while preserving the capsule. Subsequently, the capsule of the lesion was opened linearly and the mass was debulked by removing it in pieces. Then, the majority of the mass was dissected and removed from the surrounding tissue and dura, and the foraminal extension of the lesion was visualized laterally. The foraminal part was then completely excised. Upon total excision of the mass, no intradural extension of the mass was observed. Therefore, the dura was not opened. During the laminoplasty phase, the laminae were fixed with silk sutures. The frozen result was confirmed schwannoma (Fig. 2). Postoperative muscle strength examination at 8 h: left iliopsoas muscle 4/5, left quadriceps femoralis muscle 3/5, left biceps femoralis muscle 3/5, left tibialis anterior muscle 4/5, left extensor hallucis longus muscle 4/5. The patient was transferred to the ward after 2 days of intensive care follow-up and mobilized with thoracolumbar orthosis. The patient was discharged with pre-discharge neurological motor muscle strength examination as left quadriceps femoralis muscle 4/5 and left gastrocnemius muscle 4/5 with no sciatica on the left leg. The patient’s pathology result was confirmed as WHO grade I schwannoma. (Fig. 3). During the physical examination at the 3-month postoperative follow-up, it was observed that the neurological deficit had completely recovered. A contrast-enhanced lumbar and thoracic spine MRI was performed in the second month of the patient’s 3-month follow-up. No residual or recurrence was detected. (Fig. 1D-F).
A Intraoperative photograph showing the structure of the tumor located extradurally after the capsule has been opened. B The second photograph showing the part of the tumor extending into the neural foramen. Purple arrow, schwannoma with the capsule opened; blue arrow, capsule of the tumor; yellow arrow, tumor segment extending into the foramen; green arrow, spinal cord
Discussion
Spinal cord tumors account for 1–10% of all pediatric nervous system tumors. Only 2.5 to 4% of pediatric spine tumors consist of schwannomas. They are 70–80% intradural in location. Shaped like a dumbbell mass, both intradural and extradural placement are seen in 15% [2]. However, the literature informs that schwannomas are most common in the cervical segment of the spine (63%), less frequently (26%) in the thoracic segment [6].
In multiple case reports and literature review study published in 2021, it was reported that there were six cases of giant extradural schwannomas in the pediatric age group without accompanying fibromatosis [7,8,9,10,11,12]. No new case report has been published from 2021 to the present.
Spinal schwannomas and neurofibromatosis are two closely related diseases. Neurofibromatosis is known to occur in the brain, spinal cord, and peripheral nerves. It is a multiple tumor-related genetic disease. These tumors originate from Schwann cells. The most common type is NF1, also spinal neurofibromas are more common in this type. In a series of 21 pediatric spinal schwannoma cases, it was found that six patients were associated with neurofibromatosis [2]. Additionally, in 1998, a study was conducted with 128 patients who present the recurrence rate of NF2 spinal schwannoma cases after resection was reported to be higher than in NF1 cases [13]. In our case, there was no finding of neurofibromatosis detected in the patient’s scans performed after the diagnosis of schwannoma.
Schwannomas are generally benign tumors with slow growth pattern. Upon reaching critical mass, they may present with different clinical presentations depending on their anatomic location and spinal level. The most common presentations of spinal schwannomas are as follows: non-radicular pain (65.6%), radiculopathy (28.1%), sensory deficit or paresthesia (37.5%), motor weakness (18.8%), bowel or bladder dysfunction (3.1%) [14]. However, unlike the adult age group, the presenting symptoms in the pediatric patient group are progressive motor deficits (86%), localized pain (67%), and blade disturbances (29%) [2]. These presenting complaints are generally non-traumatic originated and are rarely post-traumatic related. However, pediatric patient in our case report presented post-traumatic sciatica, motor deficits, and walking difficulties.
The recommended treatment for giant spinal schwannomas is total excision. Surgical approach choice depending on the location and size of the mass is important at this stage. In pediatric patients, instrumentation should be avoided as much as possible. To prevent the development of postoperative kyphosis, laminoplasty is recommended over laminectomy [9, 10]. In our case, we chose to perform laminoplasty over laminectomy. Our patient was mobilized with a thoracolumbar orthosis on postoperative day 1. There was no evidence of kyphosis or significant angle changes seen in the X-ray on the 3rd month of the outpatient clinic.
Conclusion
Diagnosis of spinal extradural schwannoma without accompanying neurofibromatosis in childhood is a challenging pathology. The main reasons for this are its rarity in the pediatric age group and being a slow-growing benign tumor. In patients with giant schwannomas, even minor spinal traumas prior to the diagnosis can lead to serious neurological deficits. It is important to keep this in mind in such cases.
References
Takahashi T, Hirai T, Yoshii T et al (2023) Risk factors for recurrence and regrowth of spinal schwannoma. J Orthop Sci 28:554–559. https://doi.org/10.1016/j.jos.2022.03.003
Kulkarni A, Srinivas D, Somanna S et al (2012) Pediatric spinal schwannomas: an institutional study. J Pediatr Neurosci 7:1–3. https://doi.org/10.4103/1817-1745.97608
Sridhar K, Ramamurthi R, Vasudevan MC, Ramamurthi B (2001) Giant invasive spinal schwannomas: definition and surgical management. J Neurosurg 94:210–215. https://doi.org/10.3171/spi.2001.94.2.0210
Hsu W, Jallo GI (2013) Pediatric spinal tumors. Handb Clin Neurol 112:959–965. https://doi.org/10.1016/B978-0-444-52910-7.00016-7
Öğrenci A, Koban O, Şentürk S, Yaman O, Sasani M, Dalbayrak S (2017) Giant spinal schwannomas Clin Surg 2:1593
Yazol M, Derinkuyu BE, Boyunaga O (2023) Three different faces of schwannoma in pediatric patients. Curr Med Imaging 20:1–5. https://doi.org/10.2174/1573405620666230414115555
Shaikh ST, Thareja V, Mohanty CB, Deopujari CE (2021) Giant extradural spinal schwannoma in a non-neurofibromatosis child-case report and review of literature. Childs Nerv Syst 37:1327–1331. https://doi.org/10.1007/s00381-020-04801-5
Kataria R, Kurmi DJ, Mehta J, Sinha VD (2012) Giant lumbosacral schwannoma in a child. J Pediatr Neurosci 7:126–128. https://doi.org/10.4103/1817-1745.102576
Gill M, Maheshwari V, Narang A (2017) Extradural spinal schwannoma in a 5 year old non NF child: a rare entity. Romanian Neurosurg 222–225. https://doi.org/10.1515/romneu-2017-0036
Srinivas M, Sridevi H, Dikshitha K (2016) Extradural spinal schwannoma at cervical spine in 12 year old child. Int J Med Res Health Sci 5:179–181
Pokharel A, Rao TS, Basnet P et al (2019) Extradural cervical spinal schwannoma in a child: a case report and review of the literature. J Med Case Reports 13:230. https://doi.org/10.1186/s13256-019-2108-6
Agrawal A, Reddy VU, Santhi V, Sandeep Y (2019) Giant lumbar dumbbell extradural schwannoma in a child. Asian J Neurosurg 14:535–537. https://doi.org/10.4103/ajns.AJNS_132_18
Klekamp J, Samii M (1998) Surgery of spinal nerve sheath tumors with special reference to neurofibromatosis. Neurosurgery 42:279. https://doi.org/10.1097/00006123-199802000-00042
Sowash M, Barzilai O, Kahn S et al (2017) Clinical outcomes following resection of giant spinal schwannomas: a case series of 32 patients. J Neurosurg Spine 26:494–500. https://doi.org/10.3171/2016.9.SPINE16778
Acknowledgements
The authors would like to thank all the staffs of the Department of Neurosurgery at Bolu Abant Izzet Baysal University for their contributions to the patient’s treatment process.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Caner Çiçek, Yaşar Dağıstan, and Yağız Akyüz. The first draft of the manuscript was written by Caner Çiçek, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Ethical approval was waived by the local Ethics Committee of Bolu Abant İzzet Baysal University in view of the retrospective nature of the study, and all the procedures being performed were part of the routine care.
Consent for publication
The participant’s parents have consented to the submission of the case report to the journal.
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Çiçek, C., Dağıstan, Y. & Akyüz, Y. Extradural giant thoracic schwannoma in a pediatric patient; a case report. Childs Nerv Syst (2024). https://doi.org/10.1007/s00381-024-06494-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00381-024-06494-6