Abstract
Background
Previous studies have reported that positive buttress is as effective as anatomical reduction in treating young femoral neck fractures, but whether this effect is related to the Pauwels classification remains unclear. The purpose of this study was to retrospectively analyze the clinical prognosis of positive buttress in young femoral neck fractures with different Pauwels classifications, as well as to assess its biomechanical properties.
Methods
A total of 170 young patients with femoral neck fractures who were treated with three cannulated screws were included in this study. Patients were divided into three groups based on their preoperative Pauwels classification. Each group was divided into three subgroups based on the reduction quality: positive buttress, negative buttress and anatomical reduction. The femoral neck shortening, the incidence of necrosis of the femoral head (AVN) and the Harris hip scores at the last follow-up were compared across the three reduction quality within each Pauwels classification. Subsequently, a volunteer was recruited, CT data of the hip was obtained, and finite element models representing different reduction quality under varying Pauwels classifications were established. The biomechanical properties of each model were then evaluated following the application of strains.
Results
In Pauwels type I, there were no significant differences in postoperative femoral neck shortening, incidence of AVN, or Harris score among the three types of reduction quality (P > 0.05). However, positive buttress provided superior biomechanical stability compared to negative buttress and anatomical reduction. In Pauwels type II, the incidence of AVN was similar between the positive buttress and the anatomical reduction groups, and both were significantly lower than that in the negative buttress (P < 0.05). The Harris score of the positive buttress was higher than that of the negative buttress, and there was no significant difference in the occurrence of femoral neck shortening between the three groups (P > 0.05). Finite element analysis showed that the biomechanical stability of positive buttress was equivalent to anatomical reduction, and both were better than negative buttress. In Pauwels type III, the incidence of AVN in the anatomical reduction group was lower than that in both the positive buttress and negative buttress (P < 0.05). There was no significant difference in the occurrence of AVN or femoral neck shortening between positive buttress and negative buttress (P > 0.05). There was also no difference in postoperative Harris scores between the three reduction qualities (P > 0.05). Both positive buttress and negative buttress exhibited identical biomechanical qualities and were inferior to anatomical reduction.
Conclusions
The biomechanical and clinical dominance of positive buttress correlates with Pauwels type. Specifically, Positive buttress is biomechanically stable in Pauwels types I and II. In Pauwels type III, positive buttress is not advantageous. As the Pauwels angle increases, the biomechanical benefit of the positive buttress is lost. Therefore, regardless of the Pauwels classification, negative buttress should be avoided after reduction of femoral neck fractures in young patients.
Similar content being viewed by others
Introduction
Femoral neck fracture is one of the most common fracture types, accounting for approximately 50% of all hip fractures [1]. Although femoral neck fractures are not very common in young people under the age of 65 [2, 3], due to the rapid development of society and the economy, high-energy injuries caused by car accidents and falls from heights are increasing, and the incidence of femoral neck fractures in young people is gradually increasing [4]. The incidence rates of postoperative AVN and nonunion can be as high as 11-86% and 16-59%, respectively, despite the incidence rate being lower in young patients compared to elderly sufferers [5, 6].
Younger patients have higher demands for joint functional activities due to the need to manage more daily work and recreational activities. Therefore, it is essential to preserve the original joint structure and function through reduction as much as feasible [7]. Anatomical reduction was once regarded as the gold standard for the treatment of femoral neck fractures in order to lower the risk of postoperative problems [5]. Many academics have suggested numerous closed reduction techniques, such as the Whitman, Leadbetter, and Deyerler approaches, to achieve precise anatomical reduction during surgery. However, there are still a few significantly displaced femoral neck fractures that cannot be reduced anatomically [8].
After the initial fracture internal fixation, roughly 20% of cases require a second operation due to the inability to achieve optimal reduction. The most common reasons of the second procedure include AVN and nonunion [9]. Studies have demonstrated that the occurrence of postoperative complications is closely related to the type of fracture, the precision of reduction, position of internal fixation, and degree of medial cortical bone damage [10, 11]. As a result, it is crucial to choose the proper reduction and internal fixation techniques in accordance with the specific clinical classification of femoral neck fractures.
In 2013, Gotfried proposed a new reduction method, introducing the concepts of “positive buttress” and “negative buttress”. The research predicted that positive buttress could reduce the incidence of postoperative complications, and further noted that this method is simple to operate, economical and practical [12]. Negative buttress can easily result in displacement of the reduced femoral head, subsequently leading to coxa varus, and a high internal fixation failure rate. Many scholars also concur with this viewpoint, and have confirmed in the research that the clinical efficacy of positive buttress and anatomical reduction is equivalent, indicating that there is no need to pursue anatomical reduction [13, 14]. However, as the Pauwels angle increases, the shear force also increases, thereby reducing the stability of the fracture end [8]. To the best of our knowledge, there are no studies demonstrating whether the clinical efficacy and biomechanical stability of positive buttress are related to the Pauwels angle. Therefore, we hypothesize that the preponderance of positive buttress is associated with Pauwels classification. This study was divided into clinical research and biomechanical research components. Patients were categorized using the Pauwels classification, and finite element analysis was conducted alongside an evaluation of the clinical effectiveness of positive buttress in each classification.
Method
Clinical study design
Clinical data from patients who underwent cannulated screw fixation for femoral neck fractures at the First Affiliated Hospital of the Guangzhou University of Traditional Chinese Medicine between January 2015 to December 2020 were retrospectively analyzed. Inclusion criteria: (1) Age ≤ 65 years. (2) Clinical and imaging diagnosis confirmed femoral neck fracture. (3) Three parallel cannulated screw were used for pressure fixation. (4) There was no serious hip disease before the fracture and the hip mobility was basically normal. exclusion criteria: (1) Pathological femoral neck fracture. (2) Combined fractures elsewhere. (3) Patients with cognitive dysfunction and mental disorders. (4) Follow-up time was less than 1 year. (5) The presence of comorbidities such as hemiplegia that affect the evaluation of efficacy. (6) Postoperative X-ray films indicated that the Garden alignment index was grade III or grade IV. All included patients provided informed consent to participate in this study. This study was approved by the Hospital Ethics Committee (NO.JY2020259).
Subgroup
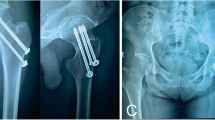
Based on the Pauwels angle measured before operation, the patients were categorized into three groups: Group A (Pauwels angle < 30°), Group B (Pauwels angle > 30° and < 50°), and Group C (Pauwels angle > 50°). Furthermore, each of these groups was subdivided into three categories based on the reduction quality: anatomical reduction group, positive buttress group, and negative buttress group. Anatomic reduction group: There was no displacement between the inner and upper margins of the distal fracture end and the inner and lower edges of the proximal fracture end. positive buttress group: the inner and lower edges of the distal fracture end protruded medially to the inner and upper edges of the proximal femoral neck fracture end. negative buttress group: the distal femoral neck fracture end protruded medially toward the inner and lower borders of the proximal fracture end. As seen in Fig. 1, groups A1, B1, and C1 are anatomical reduction. Groups A2, B2, and C2 are positive buttress. Groups A3, B3, and C3 are negative buttress.
Surgical methods
All surgeries were performed by the same senior physician. After successful anesthesia, routine disinfection and draping, the patients were positioned and held in a supine position on the orthopedic traction bed. Initially, the hip of the affected limb was flexed at 90°. Subsequently, axial traction was applied while simultaneously internally rotating and adducting the hip to achieve closed reduction.
If the closed reduction was satisfactory, a skin incision of about 2 cm could be made at 3–4 cm below the greater trochanter, followed by incision of the fascia. Under the fluoroscopy of the C-arm X-ray, one guide pin was inserted initially, and then the other two guide pins were inserted through the parallel guide. The three guide pins were distributed in an inverted triangle shape and should be dispersed as much as possible to avoid concentration. Then three cannulated screws (Diameter: 6.5 mm, Thread lengths of the screw: 16 mm) were inserted along the guide pin for fixation. The specific length of each cannulated screw was determined by intraoperative measurement.
Postoperative management
Patients should not bear weight within 3 months after surgery, and X-ray and MRI should be regularly reviewed to evaluate fracture healing and complications. Partial weight-bearing was recommended after fracture healing, and full weight-bearing activities were allowed after 6 months. Outpatient follow-up should be conducted in the first month after surgery and every three months thereafter. Hip X-rays and MR examinations were taken at each follow-up until AVN occurs or until 3 years after surgery.
Finite element analysis
A 29-year-old male health volunteer (Height is 171 cm, weight is 68 kg)was included. CT data of the volunteer’s hip were obtained using Multi-slice spiral CT without contrast agent, the slice thickness was set to 0.5 mm, the slice distance to 5 mm, and the resolution of each slice was 1024 × 1024 pixels. The image was saved in DICOM format.
We extracted the initial femur model using mimics and Geomagic-Studio software. The cancellous bone and cortical bone of femur were isolated for modeling. Using the segmentation tool in SolidWorks software, Pauwels I, Pauwels II, and Pauwels III femoral neck fracture models were created. Then, through the translation command, the proximal end of the fracture was translated upward by 2 mm along the fracture line to obtain a positive buttress model, and translated downward 2 mm to obtain a negative buttress model. The anatomical reduction model did not move the fracture end. We built cannulated screw according to real clinical implant geometric data. Finally, The fracture model with three cannulated screws were assembled to form the final analytical model.
Biomechanical analysis was performed using ANSYS software, and the elastic modulus and Poisson’s ratio of each material in the model were set according to Table 1. The number of nodes, elements and mesh size of the models were list in Table 2. Cancellous bone and cortical bone, cannulated screw and femur were set as binding contact. The fracture ends were brought to frictional contact with a 0.2 coefficient of friction. The degrees of freedom of the distal femur on the X-axis, Y-axis, and Z-axis were set to 0 and a simplified model of single-legged standing was adopted. A vertical downward stress of 700 N was applied to the weight-bearing area of the femoral head (Fig. 2).
Assessment variables
A retrospective study was conducted to compare the femoral neck shortening amount at the final postoperative follow-up among subgroups A, B, and C below (using the exposed screw measurement method: neck shortening length = measured value of the exposed length of the screw rod × The actual thickness of the cannulated screw cap/the measured value of the screw cap thickness. The cannulated screw with the longest exposed part was selected for measurement. Mild: 0–5 mm, moderate: 5–10 mm, severe: more than 10 mm). Additionally, the incidence of hip varus, nonunion, re-fracture, AVN, and the Harris hip score at the last follow-up after surgery were also compared among the subgroups.
Finite element analysis was used to compared the maximum displacement of the model (MDM), the maximum stress of the screw (MSS), the maximum displacement of the fracture (MDF), and the average stress of the cortex at the fracture (ASCF). The ASCF was obtained by calculating the average stress of the stress values of 5 points at roughly the same position in the inner and lower bone cortex of the fracture site in different models.
Statistical analysis
SPSS 29.0 was utilized to analyze and process the research data. Count data and ordinal data were represented by frequency. The χ2 test or Fisher’s exact test was used for the comparison of enumeration data between groups, and the Kruskal-Wallis test was used for the comparison of multi-group grade data. Measurement data were expressed as \(\bar{x}\pm\:s\). If the data conformed to normal distribution and homogeneity of variance, one-way ANOVA test was used for multiple group comparisons, and LSD method was employed for multiple comparisons between groups. If the data did not meet the assumptions of normal distribution or homogeneity of variances, the rank sum test was utilized. P<0.05 means the difference is statistically significant.
Results
Among the subgroups A1, A2, A3 within group A, B1, B2, B3 within group B, and C1, C2, C3 within group C, there were no significant difference in baseline characteristics such as sex, age, injured side, follow-up time, Garden classification, smoking status, alcohol status, and Time from injury to surgery. None of the included patients experienced postoperative nonunion, refracture, or hip varus (Tables 3, 5 and 7).
Clinical prognosis and biomechanical comparison of three reduction qualities in Pauwels I
Compared with groups A1, A2, and A3, there were no statistical significance in the incidence of postoperative AVN(p > 0.05), femoral neck shortening (p > 0.05), and postoperative Harris score (p > 0.05) (Table 3).
In the analysis of the MDM, the anatomical reduction was 0.47 mm, the positive buttress was the smallest of the three, 0.39 mm, and the negative buttress was 0.49 mm. The overall maximum displacement of the three models was located at the top of the femoral head. The MSS with positive buttress (33.26 MPa) was also the smallest among the three, 44.78 MPa for the anatomical reduction model, and 47.6 MPa for the negative buttress model, all of which occur at the fracture line of the upper anterior screw. The MDF of the models was arranged from small to large in order of positive buttress (0.24 mm), negative buttress (0.29 mm), and anatomical reduction (0.30 mm). In the comparison of ASCF, positive buttress was the smallest (6.26 MPa), followed by anatomical reduction was 8.71 MPa, and negative buttress was the largest (10.55 MPa) (Table 4; Fig. 3).
Clinical prognosis and biomechanical comparison of three reduction qualities in Pauwels II
There was a statistical difference in the incidence of postoperative AVN between groups B1, B2, and B3 (p< 0.05). However, the difference between group B1 and group B2 was not statistically significant (p = 0.467, > 0.05). The AVN rate of group B1 was lower than that of group B3 (p = 0.008, < 0.05). The AVN rate of group B2 was lower than that of group B3 (p = 0.038, < 0.05). Additionally, the Harris score at the last follow-up showed statistical significance across the three groups (p < 0.05). Both group B1 and group B3 did not differ significantly from one another (p = 0.059, > 0.05) or between group B1 and group B2 (p = 0.429, > 0.05). Group B2 performed superior than group B3 (p = 0.008, < 0.05). Incidences of femoral neck shortening were similar in all three groups (p > 0.05), with no discernible difference (Table 5).
The MDM of anatomical reduction, positive buttress, and negative buttress were 0.46 mm, 0.39 mm, and 0.53 mm respectively, all located at the top of the femoral head. The MSS with positive buttress was equivalent to that of anatomical reduction, which were 41.27 MPa and 42.76 MPa respectively. The stress of the negative buttress was the largest (53.26 MPa), which was significantly greater than the other two. The MSF for anatomical reduction, positive buttress, and negative buttress were 0.29 mm, 0.24 mm, and 0.32 mm respectively. In the comparison of the ASCF, Positive buttress (6.46 MPa) was equivalent to anatomical reduction (6.69 MPa). The negative buttress was the largest among the three at 10.07Mpa (Table 6; Fig. 4).
Clinical prognosis and biomechanical comparison of three reduction qualities in Pauwels III
Compared with groups C1, C2 and C3, the incidence of postoperative AVN was statistically different (p < 0.05). The AVN rate of group C1 was lower than that of group C2 (p = 0.036, < 0.05); the AVN rate of group C1 was lower than that of group C3 (p = 0.039, < 0.05). There was no significant difference between C2 group and C3 group (p = 0.567, > 0.05). The incidence of femoral neck shortening among the three reduction qualities was also statistically different (p < 0.05). There was a difference between the C1 group and the C3 group, with the incidence of femoral neck shortening in the C1 group being Lower than C3 group (p = 0.029, < 0.05), but there was no significant difference between the C1 group and the C2 group (p = 0.09, > 0.05), C2 group and C3 group, either (p = 0.252, p > 0.05). However, there was no significant statistical significance in the last follow-up Harris score among the three groups (p > 0.05) (Table 7).
The MDM of anatomical reduction, positive buttress, and negative buttress were 0.47 mm, 0.55 mm, and 0.56 mm respectively. Positive buttress was comparable to negative buttress, both higher than anatomical reduction. The MSS with positive buttress was equivalent to that of negative buttress, which were 53.66 MPa and 51.59 MPa respectively, and the anatomical reduction was 47.85 MPa, which was the smallest among the three. The MDF in anatomical reduction, positive buttress, and negative buttress were 0.3 mm, 0.36 mm, and 0.35 mm respectively. The anatomical reduction was lower than the other two. In the comparison of the ASCF, the anatomical reduction stress (5.83 MPa) was the lowest among the three. The positive buttress was 7.29 MPa, and the negative buttress was 6.24Mpa (Table 8; Fig. 5).
Discussion
This study first conducted a retrospective cohort study and found that anatomical reduction, positive buttress, and negative buttress had equivalent clinical effects in Pauwels type I. The positive buttress and anatomical reduction in Pauwels type II had the same clinical efficacy, which could reduce the incidence of postoperative AVN and improve postoperative hip function. Conversely, negative buttress were less effective. In Pauwels type III, there was no obvious advantage for positive buttress. Subsequently, finite element analysis was conducted on different models, which further proved that in Pauwels I, the biomechanical stability of the positive buttress was significantly better than that of anatomical reduction and negative buttress, with the negative buttress having the worst stability. In Pauwels II, the stability of positive buttress and anatomical reduction was equivalent, but both were better than negative buttress. In Pauwels III, anatomical reduction was superior to both positive and negative buttress. But positive and negative buttress were equivalent. Therefore, it could be speculated that the biomechanical benefit of positive buttress is related to the Pauwels type, and is gradually lost with the increase of the Pauwels angle.
For patients with unstable or displaced femoral neck fractures under the age of 65, previous studies have suggested that “anatomical reduction” is a key factor to promote fracture healing and avoid postoperative complications [15,16,17]. But Gotfried suggested that “positive buttress” may also achieve the same clinical effect. In his study, 18 patients achieved positive buttress after closed reduction, and 5 of them were followed up for more than 1 year. None of the patients had complications such as internal fixation failure, nonunion, or femoral head necrosis [12]. The conclusion is not sufficiently reliable due to the limited sample size and inconsistent internal fixation. However, subsequent studies have validated this theory [18,19,20].
Zhao et al. [13] retrospectively analyzed the data of 225 young patients with femoral neck fractures, all patients were fixed with three parallel cannulated screws, and 78 patients achieved positive buttress. The study found that the postoperative Harris scores of the positive buttress group and anatomical reduction group were higher than that of the negative buttress group, and the incidence of AVN was higher in the negative buttress group. The finite element study also indicated that the fracture displacement of the negative buttress group was greater than that of the positive buttress group. One shortcoming of their study is that patients were not analyzed separately based on their Pauwels classification. Their findings are consistent with some of the results of our study. In the Pauwels type I and II, the positive buttress is better than the negative buttress in terms of biomechanical stability. However, in Pauwels type III, our study found no significant differences in postoperative hip function, femoral neck shortening and incidence of AVN between the positive and negative buttress group. Fan et al. [21] conducted a finite element analysis and constructed positive buttress models with Pauwels angles of 30° and 50° respectively. The study concluded that at a Pauwels angle of 30°, the positive buttress is more stable than the negative buttress and this advantage weakens when the Pauwels angle is 50°. This conclusion is consistent with our research, but they lacked further verification of clinical research, and did not analyze the case of Pauwels angle of 70°.
There may be several reasons why positive buttress is more stable than negative buttress. Under the applied force, the proximal fragment has a propensity to deform in varus. In the positive buttress group, the distal medial cortex can support the proximal end to resist deformation. In contrast, negative buttress lacks support from the medial cortex, resulting in poorer stability [22]. In addition, due to the obvious thickening of the medial cortex of the femoral neck, an arch bridge structure is formed. When a positive buttress is obtained, the arch bridge support function of the distal medial cortex can effectively resist the longitudinal shear force between the fracture fragments, thereby making the fracture end more stable [23, 24]. In our study, we discovered that the MDM and the MDF in Pauwels type I and type II in the positive buttress group were lower than those in the negative buttress group, demonstrating the more stable biomechanical properties of the positive buttress. However, in Pauwels type III, the performance of the positive buttress group was equivalent to that of the negative buttress group. This may be related to the increased shear force at the fracture end as the increase of the Pauwels angle. These findings were consistent with the results of some clinical studies. An interesting fact is that in Pauwels type I, we found that the clinical efficacy of the three reduction qualities was equivalent. This may be due to insufficient shear force. Our research conclusions are also consistent with a previous finite element study, which suggests that damage to load-bearing structures at different implant placements does not affect the overall final fixation stability. Therefore, there is no need to reintroduce implants at ideal locations, as this can reduce the radiation dose to the patient during the surgery. However, that study did not consider the potential impact of Pauwels classification on the results [25]. Therefore, we recommend that it is not necessary to pursue anatomical reduction when dealing with Pauwels type I and Pauwels type II femoral neck fractures in young adults, but striving for anatomical reduction is still the preferred standard for Pauwels type III.
Currently, questions remain regarding whether the amount of displacement of the distal medial cortex of the positive strut relative to the proximal medial cortex is related to its mechanical properties. Wang et al. [26] studied the effect of moving the distal end of the positively supported fracture upward by 2 mm, 3 mm, and 4 mm along the fracture direction, to evaluate whether its biomechanical advantages were related to the degree of displacement. Finally, it was found that in the positive buttress model with a displacement of 3 mm, the relative displacement between the fracture fragments was the smallest when a load was applied. Therefore, it is believed that the upward displacement of the proximal end of the positive buttress fracture should be controlled within 3 mm in order to better exert the biomechanical advantages. However, it has not yet been confirmed by clinical studies. In this study, the finite element model of positive buttress and negative buttress obtained by translating the distal end of the fracture along the fracture line by 2 mm is within the ideal range. Based on the current limited knowledge, we recommend that the displacement should be controlled to 3 mm to maximize the performance of the positive buttress.
This study has some shortcomings. Firstly, although the Pauwels classification is the first biomechanical-based classification method for femoral neck fractures, it is still widely used clinically [27]. However, its disadvantage is that the image may be affected by the shooting angle [6]. Our study did not conduct unified quality control on the photographing angle, which may lead to inaccurate classification judgments. In addition, when performing finite element analysis, the influence of surrounding muscle strength on the results was not considered in order to simplify calculations. This may be slightly different from the physiological state of the human body. Since only one finite element model was created, it may not be representative of 170 patients with femoral neck fractures. Additionally, the loads applied to the model are not physiological. Last but not least, this study was retrospective, had a limited sample size, and neglected to take into account the effects of variables that can influence the prognosis of femoral neck fractures, such as the interval between injury and surgery and the time required to bear weight on the ground. In the future, studies with larger samples can be carried out to address these issues.
Conclusion
In conclusion, The results of our study suggest that there is no need to pursue anatomical reduction during closed reduction of Pauwels type I and Pauwels type II femoral neck fractures in young people. Positive buttress may also achieve a good prognosis. Since the advantage of positive buttress is gradually lost with the increase of Pauwels angle, anatomical reduction in Pauwels type III is the optimal treatment choice. But in any case, we should avoid negative buttress.
Data availability
The data used to support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- AVN:
-
Necrosis of the femoral head
- MDM:
-
The maximum displacement of the model
- MSS:
-
The maximum stress of the screw
- MDF:
-
The maximum displacement of the fracture
- ASCF:
-
The average stress of the cortex at the fracture
References
Abrahamsen B, van Staa T, Ariely R, Olson M, Cooper C. Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int. 2009;20(10):1633–50.
Robinson CM, Court-Brown CM, McQueen MM, Christie J. Hip fractures in adults younger than 50 years of age. Epidemiology and results. Clin Orthop Relat Res. 1995;(312):238–46.
Duckworth AD, Bennet SJ, Aderinto J, Keating JF. Fixation of intracapsular fractures of the femoral neck in young patients: risk factors for failure. J bone Joint Surg Br Volume. 2011;93(6):811–6.
Wan L, Zhang X, Wu D, Li Z, Yuan D, Li J, et al. Application of Robot Positioning for Cannulated Screw Internal Fixation in the treatment of femoral Neck fracture: Retrospective Study. JMIR Med Inf. 2021;9(1):e24164.
Haidukewych GJ, Rothwell WS, Jacofsky DJ, Torchia ME, Berry DJ. Operative treatment of femoral neck fractures in patients between the ages of fifteen and fifty years. J bone Joint Surg Am Volume. 2004;86(8):1711–6.
Collinge CA, Mir H, Reddix R. Fracture morphology of high shear angle vertical femoral neck fractures in young adult patients. J Orthop Trauma. 2014;28(5):270–5.
Malchau H, Herberts P, Eisler T, Garellick G, Söderman P. The Swedish total hip replacement Register. J bone Joint Surg Am Volume. 2002;84–A(Suppl 2):2–20.
Florschutz AV, Langford JR, Haidukewych GJ, Koval KJ. Femoral neck fractures: current management. J Orthop Trauma. 2015;29(3):121–9.
Slobogean GP, Sprague SA, Scott T, Bhandari M. Complications following young femoral neck fractures. Injury. 2015;46(3):484–91.
Liporace F, Gaines R, Collinge C, Haidukewych GJ. Results of internal fixation of Pauwels type-3 vertical femoral neck fractures. J bone Joint Surg Am Volume. 2008;90(8):1654–9.
Ly TV, Swiontkowski MF. Treatment of femoral neck fractures in young adults. Instr Course Lect. 2009;58:69–81.
Gotfried Y, Kovalenko S, Fuchs D. Nonanatomical reduction of displaced subcapital femoral fractures (gotfried reduction). J Orthop Trauma. 2013;27(11):e254–9.
Zhao G, Liu M, Li B, Sun H, Wei B. Clinical observation and finite element analysis of cannulated screw internal fixation in the treatment of femoral neck fracture based on different reduction quality. J Orthop Surg Res. 2021;16(1):450.
Huang K, Fang X, Li G, Yue J. Assessing the effect of Gotfried reduction with positive buttress pattern in the young femoral neck fracture. J Orthop Surg Res. 2020;15(1):511.
Wang Y, Ma JX, Yin T, Han Z, Cui SS, Liu ZP, et al. Correlation between reduction quality of femoral Neck fracture and AVNBased on Biomechanics. Orthop Surg. 2019;11(2):318–24.
Slobogean GP, Stockton DJ, Zeng B, Wang D, Ma BT, Pollak AN. Femoral Neck fractures in adults treated with internal fixation: a prospective Multicenter Chinese Cohort. J Am Acad Orthop Surg. 2017;25(4):297–303.
Stacey SC, Renninger CH, Hak D, Mauffrey C. Tips and tricks for ORIF of displaced femoral neck fractures in the young adult patient. Eur J Orthop Surg Traumatology: Orthopedie Traumatologie. 2016;26(4):355–63.
Jiang Q, Liu Y, Bai X, Deng Y, Cao Y, Yu C, et al. Nonanatomical reduction of femoral neck fractures in young patients treated with femoral neck system: a retrospective cohort study. BMC Musculoskelet Disord. 2023;24(1):412.
Zhu J, Li Y, Zhang Y, Cheng X. Clinical Outcome and Biomechanical Analysis of Dynamic Hip Screw Combined with Derotation Screw in Treating Displaced Femoral Neck Fractures Based on Different Reduction Qualities in Young Patients (≤ 65 Years of Age). BioMed research international. 2022; 2022:9505667.
Zhong Z, Lan X, Xiang Z, Duan X. Femoral neck system and cannulated compression screws in the treatment of non-anatomical reduction Pauwels type-III femoral neck fractures: a finite element analysis. Clin Biomech (Bristol Avon). 2023;108:106060.
Fan Z, Chen P, Yu X, Li X, Su H, Chen H, et al. Biomechanical study of femoral neck system for young patients with nonanatomically reduced femoral neck fractures: a finite element. BMC Musculoskelet Disord. 2023;24(1):54.
Ling L, Qu Z, Zhou K. Effect of fracture reduction with different medial cortical support on Stability after Cephalomedullary nail fixation of unstable Pertrochanteric fractures: a biomechanical analysis. Indian J Orthop. 2022;56(1):34–40.
Sjöholm P, Otten V, Wolf O, Gordon M, Karsten G, Sköldenberg O, et al. Posterior and anterior tilt increases the risk of failure after internal fixation of Garden I and II femoral neck fracture. Acta Orthop. 2019;90(6):537–41.
Wang G, Wang B, Wu X, Yang H. Gotfried positive reduction promotes the repair of femoral neck fracture potentially via enhancing osteogenesis and angiogenesis. Volume 123. Biomedicine & pharmacotherapy = Biomedecine & pharmacotherapie; 2020. p. 109801.
Bartoska R, Baca V, Horak Z, Hrubina M, Skala-Rosenbaum J, Marvan J, et al. The importance of intramedullary hip nail positioning during implantation for stable pertrochanteric fractures: biomechanical analysis. Surg Radiol Anat. 2016;38(5):577–85.
Wang G, Wang B, Tang Y, Yang HL. A quantitative biomechanical study of positive buttress techniques for femoral neck fractures: a finite element analysis. Chin Med J. 2019;132(21):2588–93.
Bartonícek J. Pauwels’ classification of femoral neck fractures: correct interpretation of the original. J Orthop Trauma. 2001;15(5):358–60.
Acknowledgements
Not applicable.
Funding
This work was supported by the Beijing Municipal Science and Technology Project (Z191100006619024), the Beijing Municipal Natural Science Foundation of China (7172244) and the hospital-level research project of Shunyi Hospital of Beijing Traditional Chinese Medical Hospital (SYYJLC-202401) .
Author information
Authors and Affiliations
Contributions
BLX and XHC: Research Design and Paper Writing; CZ and SYW: Collection and organization of data; ZXB: Finite Element Analysis Modeling; SXD: Data Statistical Analysis; ZYG: Analysis and visualization of results; QWZ and WDS: Research Quality Assessment.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was conducted in agreement with the Declaration of Helsinki and its later amendments or comparable ethical standards and had been approved by the ethics board of The First Affiliated Hospital of Guangzhou University of Chinese Medicine (NO.JY2020259).
Consent for publication
Written informed consent for publication was obtained from all participants.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xiong, B., Cao, X., Zhang, C. et al. Nonanatomical reduction of femoral neck fractures in young patients with different Pauwels classifications: a retrospective study and finite element analysis. BMC Musculoskelet Disord 25, 686 (2024). https://doi.org/10.1186/s12891-024-07802-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-024-07802-6