Abstract
Background
This study evaluated the biomechanics of the proximal femoral nail antirotation-II (PFNA-II) in AO/OTA 31A2.2 intertrochanteric fractures based on the fracture reduction quality.
Methods
Unstable intertrochanteric fractures were created according to the AO classification and repaired by proximal femoral nail antirotation-II (PFNA-II) using one of three medial cortical support groups. The specimens were tested using cyclic axial loading. The following parameters were recorded: force and stiffness at failure, maximum vertical and horizontal displacement, neck-shaft angle, and location and patten of failure.
Results
In the cyclic loading test, the force at failure in the anatomical reduction (AR) group was greater than that of the positive medial cortical support (PMCS) group (984.22 ± 12.63 vs. 936.95 ± 16.78) N (P < 0.05) and negative medial cortical support (NMCS) group (918.04 ± 28.86) N (P < 0.05). The stiffness in the AR group was 4.77 and 31.9% higher than that in the PMCS group (P > 0.05) and NMCS group (P < 0.05). The maximum vertical displacement was the largest in the NMCS group. The maximum horizontal displacement in the NMCS group was 28.6 and 19.1% larger than that in the AR group (P > 0.05) and PMCS group (P < 0.05). The neck-shaft angle in the NMCS group was smaller than that in the anatomic reduction group (P < 0.05) and positive support group (P < 0.05).
Conclusion
For the unstable AO/OTA 31A2.2 intertrochanteric fracture, there were significant differences in their mechanical stability among AR, PMCS and NMCS. The NMCS is not recommended during the intraoperative reduction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of intertrochanteric fractures has increased significantly along with the accelerated aging of the population [1], and the morbidity is 1.32% among people over 85 years old [2]. In elderly patients, early operation within 24–48 h and function exercise can significantly reduce the complications and mortality [3]. For the intertrochanteric fracture patients without obvious operation contraindications, surgical treatment is still the first choice.
Compared with other surgical procedures, intramedullary nail fixation has obvious biomechanical advantages, due to its less invasiveness. It is suitable for most intertrochanteric fractures and more widely applied clinically. However, there are many hip muscles, and the mechanical structure is complex. To achieve anatomical reduction (AR), multiple reductions are often needed, and the operation time will be prolonged. In addition, the elderly patients often have other underlying chronic diseases, such as pneumonia and decreased cardiac function. To ensure the safety of the surgery, the operation time should be shortened as much as possible. A balance between the operation time, safety, reduction quality and biomechanics is needed. The reduction quality is one of most important factors affecting the stability of internal fixation of the intertrochanteric hip fracture [4]. If the stability is poor, the head-neck fragment will continue to telescope along the axis of the implant (lag screw/helical blade), resulting in the shortening of the proximal femur, and loss of the neck-shaft angle and varus. In these cases, the phenomenon of cut-in or cut-out and the functional influence will appear, and the hip function will be affected [5,6,7]. There are various criteria for assessing the reduction quality of intertrochanteric fractures, and the most widely used criteria were proposed by Baumgaertner et al. [8,9,10,11]. The Baumgaertner criteria define a displacement of any fragment of less than 4 mm (between 3 and 5 mm) as a good reduction quality, but the displacement direction of the fracture fragments is not considered at all. We were the first to test the effect of the displacement direction of the fracture fragments on stability from the perspective of biomechanics. The purpose of this study was to compare the biomechanical stability of different medial cortical support patterns after the proximal femoral nail antirotation-II (PFNA-II) fixation for unstable AO/OTA 31A2.2 intertrochanteric fractures. We aim to provide the theoretical basis for its clinical application to reduce postoperative complications and improve the outcome of the surgery.
Materials and Methods
Sample Preparation
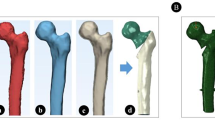
A total of 18 synthetic proximal osteoporotic femurs [12, 13] were divided into 3 different medial cortical support groups in intertrochanteric fracture models (AO/OTA 31A2.2) [14, 15], namely anatomical reduction (AR), positive medial cortical support (PMCS) and negative medial cortical support (NMCS).
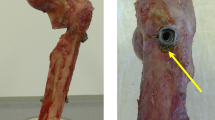
The fracture models were simulated according to the 2018 AO/OTA classification of 31A2.2 fracture models of intertrochanteric fractures. The intertrochanteric fractures were created using custom templates. According to the definition of lateral wall by Hsu [16], a horizontal line was drawn 3 cm below the innominate tubercle of the greater trochanter. At the intersection of this horizontal line and the lateral cortex, a 45° angle line was drawn intersecting the fracture line at point A with a lateral wall thickness of 2 cm. Another horizontal line was drawn at the lowest point of the lesser trochanter and the intersection of this line and the anteromedial wall of the femur was designated as B. The AO/OTA 31A2.2 fracture model was made by drawing a straight-line F across the two points of A/B and removing the large area of the lesser trochanter and part of the posterior wall (Fig. 1).
All fracture models were made by the same senior surgeon. PMCS is defined as the medial cortex of the head–neck fragment displaced and located slightly superomedially to the medial cortex of the femur shaft in the anteroposterior (AP) view. NMCS is the opposite of the PMCS, and is defined as the medial cortex of the head–neck fragment located lateral to the medial cortex of the femur shaft in the AP view. Every displacement is defined as a cortical distance of 3.64 mm. All the fractures were fixed using the PFNA-II (170 mm, diameter: 9 mm, titanium alloys; Double Medical Technology Inc., Xiamen, China). The lag screw was placed and fluoroscopy was used to ensure that the lag screw position was in the inferior third of the femoral neck in the PA view and in the center of the femoral neck in the lateral view, and the tip-to-apex distance (TAD) was between 20 and 25 mm [17,18,19]. All PFNA-II nails were statically locked with a distal locking screw.
Test Protocol
The model was place on the Instron 3365 testing machine (Instron, Norwood, MA, USA) with the distal part embedded. The position of the model was simulated with one leg standing (Fig. 2). The models were oriented at 15° of adduction in the coronal plane and aligned vertically in the sagittal plane [20, 21]. The femoral head was inserted proximally into an acetabulum-type cup and was free to rotate inside the cup.
A Axial stiffness mechanical test was taken under the Instron (Model 3365) testing machine (Instron, Norwood, MA, USA); B The data were collected by the GOM Inspect Professional Dynamic Capture 3D system (GOM GmbH, Braunschweig, Germany); C Screenshot of an optical view with vertical and horizontal axis of data acquisition
All three different medial cortical support groups were subjected to the cyclic loading test according to a previous study [13]. In the cyclic loading test, the number of cycles varies, but the commonly used 10,000 cycles protocol attempts to simulate the walking of a patient over a 6-week period until healing occurs. The upper load of 1400 N is considered to be the equivalent of the weight of a 70-kg person.
The test protocol included a preload of 200 N that was increased to the maximum force at a rate of 100 N at each cycle [22, 23] until failure or until a force of 1400 N is reached [24] at a displacement rate of 10 mm/min. The force at failure was defined as that at which there was a visible failure of the internal fixation (screw blade cutting out, screw blade withdrawing, screw blade broken or fracture reduction loss or new bone fracture), or a drop of the applied force or an inability to increase the force value with increasing standard travel.
The displacement and neck-shaft angle data were collected using the GOM Inspect Professional Dynamic Capture 3D system (GOM GmbH, Braunschweig, Germany) (Fig. 2). The load data were taken from the force gauge of the testing machine. The stiffness of the construct was calculated using the load/standard travel curve from the last three conditioning cycles.
After testing, the specimens were examined for the location of the fractures, distal screw migration or bending of the implant.
Statistical Analysis
The SPSS 23.0 statistical software (IBM Corp., Armonk, NY, USA) was used to analyze the data. One-way analysis of variance (ANOVA) was used to analyze the comparison among the data of multiple groups, and the least significant difference (LSD) post hoc test was used to compare the data of the two groups. Student tests were used to analyze the comparison between the two groups. The difference was considered statistically significant when the P value was less than 0.05.
Results
The detail results are shown in Table 1.
In the cyclic loading test, the force at failure of the AR group was 4.8 and 6.72% larger than that of the PMCS and NMCS groups, respectively (P < 0.05). However, there was no statistical difference between the PMCS and NMCS groups (P > 0.05), (Fig. 3).
The stiffness at failure of the AR group was 4.77 and 31.9% higher than that in the PMCS group (P > 0.05) and NMCS group (P < 0.05), (Fig. 3). The vertical displacement of the NMCS group was 8.32 and 5.4% larger than that of the AR and PMCS groups, respectively (P < 0.05), (Figs. 4, 5). The horizontal displacement of the NMCS group was 28.64 and 19.12% larger than that of the AR and PMCS groups, respectively (P < 0.05) (Fig. 4). The neck-shaft angle of the AR group was 0.6 and 1.7% larger than that of the PMCS and NMCS groups, respectively (P < 0.05) (Fig. 4). However, there was no statistical difference between the AR group and PMCS in the stiffness at failure, the maximum vertical and horizontal displacement, and the neck-shaft angle (P > 0.05).
The vertical displacement of NMCS group was 8.32% and 5.4% larger than that of AR and PMCS groups, respectively. The horizontal displacement of NMCS group was 28.64% and 19.12%larger than that of AM and PMCS groups, respectively. The neck-shaft angle of AR group was 0.6% and 1.7% larger than that of PMCS and NMCS groups, respectively.**Significant (P < 0.05)
The breakage of the head–neck fragment occurred in seven cases, split fracture at the zone of the distal screw in two cases, and breakage in the distal femur area in eight cases, and one case of breakage in both the zone of the distal screw and distal femur area.
Discussion
The results of this study revealed that although the AR, PMCS, and NMCS are all methods that achieve good reduction quality according to the Baumgaertner criteria, there are significant differences in their mechanical stability. The PMCS method is not inferior to the AR method, and both are superior to the NMCS method. The Baumgaertner criteria only consider the displacement distance of the fracture fragments, but we should also consider and add the displacement direction of the fracture fragment to these criteria. All the forces at failure in the AR, PMCS and NMCS groups were less than 1400 N, which is consistent with the results obtained by Ceynowa [13]. Accordingly, whether early weight-bearing is needed after the treatment of unstable AO/OTA 31A2.2 intertrochanteric fractures should be carefully considered.
In 1980, Kaufer first described five factors that affect the stability of internal fixation of the intertrochanteric hip fracture, namely bone quality, fracture geometry, reduction quality, implant type and implant placement [4]. For implant type selection, compared with extramedullary fixation, intramedullary fixation has many advantages, such as central fixation with better biomechanics to reduce the risk of collapse and less invasive procedure [17,18,19]. As a result, the intramedullary nail is much more widely used. Before intramedullary nail insertion, the reduction of the fracture should be the most important procedure. AR is the goal of all fracture treatments. However, sometimes, it is not easy to achieve AR in intertrochanteric fractures in a short time during the surgery, which will undoubtedly increase the operation time and the risk of complications. Since the elderly patients often suffer from some chronic medical condition, the incidence of perioperative complications and mortality is high. To reduce the operation time and the incidence of intraoperative complications, we had to compromise the reduction quality to ensure the safety of the operation. At present, in clinical practice, we most commonly use the Baumgaertner criteria to evaluate the reduction quality in intertrochanteric fractures. According to the proposed criteria, the reduction quality of the intertrochanteric fractures is divided into three grades: good, acceptable, and bad. Less than 4 mm displacement of any fragments is considered as good reduction quality, but the displacement direction of the fracture fragment is not considered. However, it seems that the displacement direction of the fracture fragment after reduction also affects the stability and clinical outcomes [25,26,27]. Therefore, in this study, we further divided the reduction quality into AR, PMCS and NMCS and found that the biomechanical performance of these three kinds of reduction models with “good” reduction quality was quite different.
In the cyclic loading test, the stiffness in the PMCS and AR groups was much higher than that in the NMCS group, and there was a statistically significant difference. Stiffness refers to the ability of a component to resist deformation. The change in the reduction quality can alter the whole stiffness. The ability to resist deformation in the AR and PMCS groups is higher than that in the NMCS group. The reason is that when the experimental model is loaded, the head and neck fracture fragment will have a slight tendency of varus deformity, the medial cortex of the distal intertrochanteric fracture can support the proximal cortical fragment to resist deformation in the PMCS and AR groups. For the negative cortical support reduction model, the medial cortical support is absent. The lack of this kind of support reduces its ability to resist varus deformity. The head–neck fragment was under more force, as a result the breakage of the head-neck fragment was found the most in the PMCS group. Different reduction quality had different location and patten of failure. The varus deformity of the head and neck fracture fragments also implies a decrease of the neck-shaft angle. The changes in the neck-shaft angle were also the largest in the NMCS group. On the other hand, the NMCS group had the largest vertical and horizonal displacement in each cycle. When the load of the sine wave load increases, the head and neck fracture fragment moves down more in the negative cortical support group than that in the positive cortical support group and the AR group, as a result the spiral blade may cut more bone of the femoral head and neck fracture fragment. Therefore, the screw blade in the NMCS is more likely to destroy the normal bone of the femoral head as mentioned by Ceynowa [13], especially in patients with osteoporosis. Thus, the shortening and varus deformity of the proximal femur will result in a poor mechanical environment in the intertrochanteric fracture site, increased stress of the internal fixation device, increased incidence of the internal fixation failure (cut-out, cut-in), fracture non-union and other complications [27, 28].
In this study, we only considered the effect of the medial cortical support in the coronal plane. We believe that there should be similar differences in mechanical stability in the sagittal plane. In the unstable intertrochanteric fractures, the posterior medial side of the intertrochanteric region is mostly comminuted and displaced, while the anterior medial region is mostly thicker with a simple fracture line. Therefore, the cortical support reduction of the “anteromedial corner” proposed by Professor Chang is extremely important [27]. The stability of the fracture reduction should be determined from both the AP and lateral views to avoid intertrochanteric fracture reduction without cortical support reduction. The head and neck fragments will slide excessively to the medullary cavity which will affect the stability of the fracture site under axial compression, leading to varus or internal fixation failure. In addition, the AR model in our study is hand-made and idealized. However, due to the resolution of the fluoroscopy machine, a cortical displacement of less than 2 mm cannot be distinguished by the naked eye. It is difficult to distinguish the accurate AR, slight PMCS and slight NMCS during the surgery. Thus, during the surgery, the surgeon should make a much more careful evaluation.
This study has several limitations. First, no lateral bending stiffness tests and torsional stiffness tests were performed. Second, in the current treatment, InterTAN, PFNA-II, Gamma3 are all widely used as intramedullary fixation devices, but we only used the PFNA-II to perform the biomechanical test. In the future, the stability of the positive cortical support reduction model can be compared using different implants.
Conclusion
For the unstable AO/OTA 31A2.2 intertrochanteric fracture fixed using PFNA-II, the mechanical stability of the PMCS is not inferior to AR, but significantly superior to the NMCS. If we have to shorten the operation time and reduce the operation risk, the PMCS, after the reduction of intertrochanteric fracture is also an acceptable option. In addition, we should refine the evaluation criteria of the reduction quality and appraise the relative position of the medial cortex of the fracture fragment after reduction to provide an optimal mechanical environment for early functional exercise and fracture healing.
References
Radaideh, A. M., Qudah, H. A., Audat, Z. A., Jahmani, R. A., Yousef, I. R., & Saleh, A. (2018). Functional and radiological results of proximal femoral nail antirotation (PFNA) osteosynthesis in the treatment of unstable pertrochanteric fractures. Journal of Clinical Medicine, 7(4), 78. https://doi.org/10.3390/jcm7040078
Füchtmeier, B., Gebhard, F., & Lenich, A. (2011). Komplikationen bei pertrochantären Frakturen [Complications after pertrochanteric fractures]. Der Unfallchirurg, 114(6), 479–484. https://doi.org/10.1007/s00113-011-1974-13
Uzoigwe, C. E., Burnand, H. G., Cheesman, C. L., Aghedo, D. O., Faizi, M., & Middleton, R. G. (2013). Early and ultra-early surgery in hip fracture patients improves survival. Injury, 44(6), 726–729. https://doi.org/10.1016/j.injury.2012.08.025
Kaufer, H. (1980). Mechanics of the treatment of hip injuries. Clinical Orthopaedics and Related Research, 146, 53–61.
Bretherton, C. P., & Parker, M. J. (2016). Femoral medialization, fixation failures, and functional outcome in trochanteric hip fractures treated with either a sliding hip screw or an intramedullary nail from within a randomized trial. Journal of Orthopaedic Trauma, 30(12), 642–646. https://doi.org/10.1097/BOT.0000000000000689
Weil, Y. A., Khoury, A., Zuaiter, I., Safran, O., Liebergall, M., & Mosheiff, R. (2012). Femoral neck shortening and varus collapse after navigated fixation of intracapsular femoral neck fractures. Journal of Orthopaedic Trauma, 26(1), 19–23. https://doi.org/10.1097/BOT.0b013e318214f321
Stern, L. C., Gorczyca, J. T., Kates, S., Ketz, J., Soles, G., & Humphrey, C. A. (2017). Radiographic review of helical blade versus lag screw fixation for cephalomedullary nailing of low-energy peritrochanteric femur fractures: There is a difference in cutout. Journal of Orthopaedic Trauma, 31(6), 305–310. https://doi.org/10.1097/BOT.0000000000000853
Carr, J. B. (2007). The anterior and medial reduction of intertrochanteric fractures: A simple method to obtain a stable reduction. Journal of Orthopaedic Trauma, 21(7), 485–489. https://doi.org/10.1097/BOT.0b013e31804797cf
Davis, T. R., Sher, J. L., Horsman, A., Simpson, M., Porter, B. B., & Checketts, R. G. (1990). Intertrochanteric femoral fractures. Mechanical failure after internal fixation. The Journal of Bone and Joint Surgery. British Volume, 72(1), 26–31. https://doi.org/10.1302/0301-620X.72B1.2298790
Biber, R., Berger, J., & Bail, H. J. (2016). The art of trochanteric fracture reduction. Injury, 47(Suppl 7), S3–S6. https://doi.org/10.1016/S0020-1383(16)30845-2
Baumgaertner, M. R., Curtin, S. L., Lindskog, D. M., & Keggi, J. M. (1995). The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. The Journal of Bone and Joint Surgery. American Volume, 77(7), 1058–1064. https://doi.org/10.2106/00004623-199507000-00012
Ozkan, K., Türkmen, İ, Sahin, A., Yildiz, Y., Erturk, S., & Soylemez, M. S. (2015). A biomechanical comparison of proximal femoral nails and locking proximal anatomic femoral plates in femoral fracture fixation: A study on synthetic bones. Indian journal of orthopaedics, 49(3), 347–351. https://doi.org/10.4103/0019-5413.156220
Ceynowa, M., Zerdzicki, K., Klosowski, P., Pankowski, R., Rocławski, M., & Mazurek, T. (2020). The early failure of the gamma nail and the dynamic hip screw in femurs with a wide medullary canal. A biomechanical study of intertrochanteric fractures. Clinical Biomechanics (Bristol, Avon), 71, 201–207. https://doi.org/10.1016/j.clinbiomech.2019.11.006
Cauley, J. A., Cawthon, P. M., Peters, K. E., Cummings, S. R., Ensrud, K. E., Bauer, D. C., Taylor, B. C., Shikany, J. M., Hoffman, A. R., Lane, N. E., Kado, D. M., Stefanick, M. L., Orwoll, E. S., & Osteoporotic Fractures in Men (MrOS) Study Research Group. (2016). Risk factors for hip fracture in older men: The osteoporotic fractures in men study (MrOS). Journal of Bone and Mineral Research: The Official Journal of the American Society for Bone and Mineral Research, 31(10), 1810–1819. https://doi.org/10.1002/jbmr.2836
Meinberg, E. G., Agel, J., Roberts, C. S., Karam, M. D., & Kellam, J. F. (2018). Fracture and dislocation classification compendium-2018. Journal of Orthopaedic Trauma, 32(Suppl 1), S1–S170. https://doi.org/10.1097/BOT.0000000000001063
Hsu, C. E., Shih, C. M., Wang, C. C., & Huang, K. C. (2013). Lateral femoral wall thickness. A reliable predictor of post-operative lateral wall fracture in intertrochanteric fractures. The Bone & Joint Journal, 95-B(8), 1134–1138. https://doi.org/10.1302/0301-620X.95B8.31495
Kaplan, K., Miyamoto, R., Levine, B. R., Egol, K. A., & Zuckerman, J. D. (2008). Surgical management of hip fractures: an evidence-based review of the literature. II: intertrochanteric fractures. The Journal of the American Academy of Orthopaedic Surgeons, 16(11), 665–673. https://doi.org/10.5435/00124635-200811000-00007
Anglen, J. O., & Weinstein, J. N. (2008). Nail or plate fixation of intertrochanteric hip fractures: changing pattern of practice. A review of the American Board of Orthopaedic Surgery Database. The Journal of Bone and Joint Surgery. American volume, 90(4), 700–707. https://doi.org/10.2106/JBJS.G.00517
Haidukewych, G. J., Israel, T. A., & Berry, D. J. (2001). Reverse obliquity fractures of the intertrochanteric region of the femur. The Journal of Bone and Joint Surgery. American Volume, 83(5), 643–650. https://doi.org/10.2106/00004623-200105000-00001
Rybicki, E. F., Simonen, F. A., & Weis, E. B., Jr. (1972). On the mathematical analysis of stress in the human femur. Journal of biomechanics, 5(2), 203–215. https://doi.org/10.1016/0021-9290(72)90056-5
Zdero, R., Walker, R., Waddell, J. P., & Schemitsch, E. H. (2008). Biomechanical evaluation of periprosthetic femoral fracture fixation. The Journal of Bone and Joint Surgery. American Volume, 90(5), 1068–1077. https://doi.org/10.2106/JBJS.F.01561
Kaiser, W., Burmester, J., Hausmann, H., Gulielmos, V., Hätzel, M., & Merker, H. J. (1997). Vergleichende Stabilitätsprüfungen von DHS- und gamma-Nagel-Osteosynthesen bei instabilen pertrochantären Femurosteotomien [Comparative stability evaluation of dynamic hip screw and gamma-nail osteosyntheses in unstable pertrochanteric femoral osteotomies]. Langenbecks Archiv fur Chirurgie, 382(2), 100–106. https://doi.org/10.1007/BF02465097
Kukla, C., Pichl, W., Prokesch, R., Jacyniak, W., Heinze, G., Gatterer, R., & Heinz, T. (2001). Femoral neck fracture after removal of the standard gamma interlocking nail: A cadaveric study to determine factors influencing the biomechanical properties of the proximal femur. Journal of Biomechanics, 34(12), 1519–1526. https://doi.org/10.1016/s0021-9290(01)00157-9
Aminian, A., Gao, F., Fedoriw, W. W., Zhang, L. Q., Kalainov, D. M., & Merk, B. R. (2007). Vertically oriented femoral neck fractures: Mechanical analysis of four fixation techniques. Journal of Orthopaedic Trauma, 21(8), 544–548. https://doi.org/10.1097/BOT.0b013e31814b822e
Kozono, N., Ikemura, S., Yamashita, A., Harada, T., Watanabe, T., & Shirasawa, K. (2014). Direct reduction may need to be considered to avoid postoperative subtype P in patients with an unstable trochanteric fracture: A retrospective study using a multivariate analysis. Archives of Orthopaedic and Trauma Surgery, 134(12), 1649–1654. https://doi.org/10.1007/s00402-014-2089-2
Tsukada, S., Okumura, G., & Matsueda, M. (2012). Postoperative stability on lateral radiographs in the surgical treatment of pertrochanteric hip fractures. Archives of Orthopaedic and Trauma Surgery, 132(6), 839–846. https://doi.org/10.1007/s00402-012-1484-9
Chang, S. M., Zhang, Y. Q., Ma, Z., Li, Q., Dargel, J., & Eysel, P. (2015). Fracture reduction with positive medial cortical support: A key element in stability reconstruction for the unstable pertrochanteric hip fractures. Archives of Orthopaedic and Trauma Surgery, 135(6), 811–818. https://doi.org/10.1007/s00402-015-2206-x
Gotfried, Y., Kovalenko, S., & Fuchs, D. (2013). Nonanatomical reduction of displaced subcapital femoral fractures (Gotfried reduction). Journal of Orthopaedic Trauma, 27(11), e254–e259. https://doi.org/10.1097/BOT.0b013e31828f8ffc
Funding
There is no funding to support this research.
Author information
Authors and Affiliations
Contributions
Conceptualization: LL, ZQ, KZ. Test and data statistics: ZQ. Writing—original draft: LL. Writing—review and editing: KZ.
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflicts of interest to disclose. The authors alone are responsible for the content and writing of the paper. The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical Standard Statement
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed Consent
For this type of study, informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ling, L., Qu, Z. & Zhou, K. Effect of Fracture Reduction with Different Medial Cortical Support on Stability After Cephalomedullary Nail Fixation of Unstable Pertrochanteric Fractures: A Biomechanical Analysis. JOIO 56, 34–40 (2022). https://doi.org/10.1007/s43465-021-00443-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-021-00443-0