Abstract
Background
Accumulating evidence suggests that serum vascular endothelial growth factor (VEGF) in many neurobiological processes potentially contributes to the pathophysiology of psychiatric disorders, particularly cognitive decline. The purpose of this study was to explore the differences in neurocognition, social cognition and VEGF among remitted first-episode schizophrenic patients, non-remitters and normal control subjects. Moreover, we investigated the association between serum VEGF levels and cognitive functions.
Method
65 remission (RS) and 45 nonremission patients (NRS) after first-episode schizophrenia, as well as 58 healthy controls (HC) were enrolled in this study. Social cognition was assessed using the Chinese Facial Emotion Test (CFET); neurocognition was measured with a test battery consisting of Hopkins Verbal Learning Test-Revised, Verbal Fluency Test, Trail Making Tests, Digit Span Tests (DST) and Stroop Tests. Blood samples were collected for VEGF measurements. Data was analyzed with SPSS 22.0 (Chicago, IL, USA).
Results
On nearly all neurocognitive tests (except for DST), RS performed significantly worse than HC but better than NRS (P < 0.05). NRS, but not RS, exhibited markedly poorer social cognition than HC (except for Happiness and Surprise subscales of the CFET) (P < 0.05). VEGF levels showed a gradient change among three groups (HC > RS > NRS).
Conclusion
Compared to HC, RS demonstrated poorer neurocognitive but intact social cognition functioning. These results indicate that VEGF levels decreased gradually with the severity of cognitive impairment in schizophrenia. VEGF may be involved in the pathological mechanism of cognitive performance in RS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Cognitive impairment, a core symptom of schizophrenia, is characterized by neurocognition and social cognition deficits [1, 2]. Recent neuropsychological studies have indicated that cognitive dysfunction occurs in unaffected first-degree relatives of individuals with schizophrenia [3,4,5], and almost all patients in remission after first-episode schizophrenia have experienced an improvement in cognitive function following treatment with atypical antipsychotics [6, 7]. In contrast, some scholars believe that impairment of cognition including working memory, attention and executive function is independent of psychiatric symptoms, and may be considered as specific and persistent trait markers of schizophrenia [8].
Schizophrenic patients also present with deficits in certain aspects of social cognition [9, 10]. Recent studies showed that social cognition deficit occurred during the early development of mental disorders and persisted until the improvement of clinical symptoms [5, 11, 12], suggesting that social cognition deficit may serve as a vulnerability marker of this disorder. It is noteworthy that these studies included patients with acute episodes, chronic episodes and minor remission. Therefore, it is not known whether this persists during clinical remission in patients with first-episode schizophrenia.
Vascular endothelial growth factor (VEGF) is not only a member of the prominent and well-characterized neurotrophin family, but also an angiogenetic factor [13]. VEGF can protect against brain cell loss, blood–brain barrier dysfunction, dendritic spine loss, spatial memory impairment and cognitive decline in response to injury [14, 15]. In addition, VEGF has been reported to regulate blood flow and induce vasopermeability of vascular endothelial cells [13], and VEGF deficiency contributes to alterations in cellular energy metabolism and blood flow in the regional brain. Therefore, we hypothesized that abnormal expression of VEGF may be involved in the pathological mechanisms underlying hypoperfusion or decreased blood flow observed in patients with schizophrenia.
Animals experiments revealed that VEGF reversibly modulated hippocampal synaptic plasticity and improved hippocampal activity related to learning and memory [13, 16, 17]. Furthermore, a recent study showed that VEGF was upregulated in the parietal cortex of patients with schizophrenia compared to controls, and the levels of VEGF in serum were related to prefrontal cortical volume of schizophrenia subjects [18]. Consistent with the animal experiments, human studies demonstrated that VEGF levels were associated with cognitive function in patients with Alzheimer’s disease [15, 19, 20]. These findings support the notion that VEGF is an important factor against cognitive decline in neuropsychiatric illnesses. However, the effect of VEGF on cognitive function in remitted first-episode schizophrenic patients still remains unclear.
To date, it is not clear whether neurocognition, social cognition and VEGF can be restored close to their normal levels in remitted first-episode schizophrenia, and whether VEGF represents a stable trait marker or a temporary state marker of the illness. Therefore, the purpose of this study was to explore neurocognition and social cognition as well as VEGF levels and their relationship with symptom remission in first-episode schizophrenia. We hypothesized that cognition and VEGF deficits were more pronounced in patients with non-remitted schizophrenia (NRS) as compared to healthy controls (HC) but not patients with remitted schizophrenia (RS), and that these abnormalities persisted even after remission of the patient’s psychiatric symptoms.
Methods
Subjects
A total of 110 patients with first-episode schizophrenia (65 RS and 45 NRS) and 58 normal controls were enrolled. Inclusion criteria for patients were: schizophrenia diagnosis (according to DSM-V); first episodes of schizophrenia; aged 18–55 years; All RS were from outpatient clinics and NRS were from both inpatient and outpatient clinics. All patients had been hospitalized at least once at Wutai Mountain Hospital in Yangzhou, Jiangsu Province, China. A total of 95 patients were treated with monotherapy of atypical antipsychotic drugs: clozapine (n = 25), olanzapine (n = 18), risperidone (n = 18), ziprasidone (n = 15), quetiapine (n = 12) and aripiprazole (n = 7); and 15 patients received a combination with other agents, remission: aripiprazole plus clozapine (n = 2), non-remission: risperidone plus quetiapine (n = 2), ziprasidone plus clozapine (n = 2), risperidone plus clozapine (n = 4), olanzapine plus aripiprazole (n = 3), quetiapine plus aripiprazole (n = 2). According to Andreasen [21], any patient who achieved at least a ‘mild or better’ score of eight items (three items on psychoticism, two on disorganization and three on negative symptoms) of the PANSS, and the score maintained for at least 6 months, was considered remitted. Exclusion criteria were: head trauma history, neurological disease, drug abuse, other mental illness related to cognitive manifestation. In addition, demographic and clinical variables such as age, sex, education period, age of illness onset, course of illness, and antipsychotic dose (converted to chlorpromazine equivalent) were collected.
The control group consisted of 58 healthy subjects who volunteered to participate in this trial. All control subjects were in good physical health with normal laboratory findings (renal function, thyroid function, liver function and electrocardiography) and had not a history of mental disorders, assessed by means of The Mini International Neuropsychiatric Interview (MINI) [22], or first-degree relatives with a history of mental disorders or brain disease (e.g. dementia and hypothyroidism) associated with cognitive ability. General information (age, sex, education period, number of smokers and body mass index) was matched between patients and controls.
All participants (or parents/legal guardians) provided signed informed consent prior to participation. The study was approved by the Ethics Committee of Yangzhou University.
Cognitive measurement
A battery of cognitive tests was administered to all subjects to measure neurocognitive performance: Hopkins Vocabulary Learning Test-Revised (HVLT-R), Verbal Fluency Test (VFT-animals and VFT-actions), Trail Making Tests (TMT-part A and TMT-part B) and Digit Span Tests (DST-Forward and DST-Backward), as well as Stroop Tests (words, colors and interference). Chinese Facial Emotion Test (CFET) was used for assessing social cognition, which includes six emotions (happiness, sadness, fear, disgust, anger, surprise) [23,24,25]. Cognitive assessment was performed by two experienced psychiatry specialists in the test laboratory and validated by an inter-rater correlation coefficient > 0.8. The administration of cognitive tests took 2 h on average. Higher test scores indicate better cognitive function (except for the TMT). Not all patients were able to complete all cognitive tests, 2 patients in the NRS group did not complete all cognitive tests (one did not complete DST-Backward, the other did not complete Stroop interference).
VEGF serum analysis
Blood samples were collected in anticoagulant-free tubes during the morning (between 08:00 and 09:00 h). Serum was then separated, sealed and stored at − 80 °C. VEGF levels were measured using a commercially available kit (DVE00; R&D Systems, Minneapolis, IN, USA) according to the manufacturer’s instructions. All tests were conducted in duplicate for each concentration. Calculation of VEGF was performed using a standard curve for recombinant human VEGF protein. The lower detection limit was 9 pg/mL. Intra- and inter-assay variances were below 5.1 and 6.2%, respectively. Sample collection and analyses were performed in a blinded manner.
Statistical analysis
The Kolmogorov–Smirnov test was performed to test normality of data. For normally distributed continuous variables, Student’s unpaired t-test or ANOVA was used for data comparisons between two or among more groups. Post-hoc analyses were done by multiple comparison tests with Bonferroni corrections. Not normally distributed variables were evaluated with Mann-Whitney or Kruskal–Wallis H tests. Analyses of categorical variables were carried out using a Chi-squared (χ2) test. Spearman’s correlation coefficients were used to analyze the correlation between VEGF and other parameters (demographic and clinical variables, cognitive performance) among the study groups. Partial correlation analysis was employed to explore the potential influence of confounding variables on cognitive performance. Differences of P < 0.05 were considered to be significant. Data were analyzed with SPSS 22.0 (Chicago, IL, USA).
Results
Socio-demographic variables, clinical characteristics and serum VEGF levels
There was no significant difference in age, sex, education period, number of smokers and body mass index among the three groups (P > 0.05). RS and NRS did not differ in the age of onset of schizophrenia and their family history of mental illness (P > 0.05). There were no significant differences in the sociodemographic and clinical characteristics and VEGF levels between in and outpatients (P > 0.05). However, NRS used a significantly higher antipsychotic drug dose (chlorpromazine equivalent) relative to RS patients (t = 3.298, df = 108, P = 0.001) (Table 1).
NRS patients had low baseline VEGF levels (351.6 ± 121.8) in the serum compared to control (438.6 ± 213.8) and RS patients (422.8 ± 130.5) (F [2, 165] = 4.014, P = 0.020), as shown in Table 1. No significant correlations were found between serum VEGF levels and socio-demographic or clinical data (age of onset, duration of illness, and family history of mental disorders) in either all samples or within each group.
RS remitted first-episode schizophrenia; NRS non-remitted first episode schizophrenia; HC healthy control; BMI body mass index; VEGF vascular endothelial growth factor; Significant differences (P < 0.05) were marked in bold.
Neurocognition in NRS, RS and HC groups
On nearly all neurocognitive tests (except for DST), RS performed significantly worse than HC but better than NRS (P < 0.05) (Table 2). These differences remained significant among the three groups after covarying for age, body mass index, education period, antipsychotic dose and combination therapy (P < 0.05).
Social cognition in NRS, RS and HC groups
In contrast to RS, NRS performed markedly poorer on all social cognition tests than controls (P < 0.05), with the exception of the Happiness and Surprise subscales of the CFET (Table 2), that is, correct identification of negative emotions (sadness, fear, disgust and anger) of CFET was lower in NRS than in RS (P < 0.05); the latter group did not differ from controls. This difference remained significant after covarying for antipsychotic dose.
Correlation among VEGF, neurocognition and social cognition performance
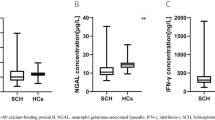
Serum VEGF levels showed a significant positive association with TMT-part B (r = 0.265, df = 58 P = 0.044) and CFET-Anger (r = 0.270, df = 58, P = 0.040) in HC. Additionally, VEGF levels were positively correlated to DST-Forward (r = 0.317, df = 65, P = 0.010) and CFET-Fear (r = 0.316, df = 65, P = 0.010) in RS (Table 3, Fig. 1). After controlling for demographic and psychopathological parameters using partial correlation analysis, the relationship between VEGF, neurocognition and social cognition performance was statistically significant only in RS, but not in HC. However, for NRS patients, no significant association between VEGF and any cognitive domain subscore was observed (all P > 0.05). Our results show a gradient among deficits in cognition across the groups (NRS > RS > HC) and VEGF levels among them also turns out that they share the different changing trend(HC > RS > NRS).
Discussion
To our knowledge, no published studies have simultaneously examined neurocognition, social cognition (facial emotion recognition) and VEGF levels in RS and NRS and HC. First of all, our results showed that RS have poorer neurocognitive function than HC, but perform better than NRS. This is in agreement with prior studies [8] demonstrating that neurocognition was impaired in RS even if the patient’s psychiatric symptoms were relieved. Moreover, Boden et al. [26] found that RS had better social behavior and subjective life satisfaction than NRS. In addition, Debrecen scholars have demonstrated cognitive impairment in the remission stage of patients with schizophrenia, suggesting that these deficits might be permanent [27, 28].
Interestingly, we also found that identification of the correct number of negative emotions (sadness, fear, anger, and disgust) was significantly lower in NRS than HC, while RS were not different from HC. This observation is consistent with previous findings [8, 29, 30] and may be explained by residual psychotic symptoms (e.g. paranoia and delusions) in NRS. Another possible explanation may be the effect of antipsychotic drugs on social cognition. Similarly, Balogh et al. [31, 32] suggested that social cognition dysfunctions are associated with acute episodes, particularly with positive psychiatric symptoms, and that these impairments are temporary. However, there is also inconsistent evidence. For example, Rodríguez-Sosa et al. [33] reported that social cognition deficit was still present in discharged patients with stable condition. These differences may be related to the heterogeneity of the sample (the unlike genetic background of different ethnicities), first-episode or relapse, anti-psychotic drug dose or illness severity. Most important of all, we included first-episode schizophrenic patients in the active stage or in clinical remission, which is our major difference. In short, our findings support impaired social cognition performance as a state of disease activity in schizophrenia. Further studies using larger sample sizes are needed to draw definitive conclusions.
In the current study, patients with first-episode schizophrenia presented with markedly impaired neurocognitive function, despite being in symptomatic remission. These results were different from social cognition measured by facial emotion recognition. However, some authors have pointed out that social cognition is associated with neurocognition [12, 34]. Conversely, Mehta et al. [35] investigated the specificity and severity of social cognition deficit in schizophrenic patients and found that Theory of Mind was not affected by cognitive ability. Therefore, social cognition and neurocognition may have distinct mechanisms.
Our most important findings are that VEGF levels are decreased in NRS patients compared to RS and HC. Furthermore, we previously reported a decrease in the VEGF in serum of subjects with schizophrenia that is restored in schizophrenia subjects treated with antipsychotic drugs or ECT [36,37,38]. These results are consistent with previous studies [39,40,41,42,43,44], supporting the hypothesis that levels of neurotrophic factor of the patients with schizophrenia was obviously abnormal. In addition, we found that VEGF was more strongly associated with neurocognitive deficits and social functioning in RS rather than NRS. However, the mechanism underlying this association remains unclear. There is compelling evidence VEGF may limit cognitive impairment, reduce dendritic spine loss and protect the blood-brain barrier [14, 17, 45,46,47]. Recent experimental evidence suggests that VEGF ameliorates cognitive and emotional deficits in an animal model of type 2 diabetes [48]. VEGF improves recovery of cognitive deficits by mediating the effect of hippocampal neurogenesis [49, 50], which links hippocampal activity with neurogenesis, learning and memory [16]. In addition, VEGF has been shown to exert robust neuroprotective effects by improving cognitive abilities in mice [51], and revert the cognitive impairment induced by a focal traumatic brain injury during the development of rats raised under environmental enrichment [52]. Human studies have found that VEGF levels were also associated with cognitive function in patients with Alzheimer’s disease [15, 19, 20]. VEGF may ameliorate cognitive impairment via improving neuronal viability and function [53], which may explain the relationship between cognitive function and VEGF in individuals with remitted schizophrenia.
Limitations
This study has some limitations. First, the sample size was relatively small. Second, the antipsychotic dose differed between RS and NRS patients. A potential effect of antipsychotic drugs on cognition cannot be excluded, although a meta-analysis showed that the second generation of antipsychotic drugs does not affect cognition in schizophrenia [54]. Third, our cross-sectional design may affect the precision and replication of the results. Finally, we only assessed one aspect of social cognition (facial emotion recognition), while other areas (psychological theory and attribution) were not evaluated. Notwithstanding these limitations, this study does suggest that VEGF is related to neurocognition and facial emotion recognition functioning in RS. Future clinical trials with additional neurocognition and social cognition tests are required to confirm our results.
Conclusions
Our study showed that remitted first-episode schizophrenic patients had deficits in neurocognition but not social cognition, and that both were associated with VEGF serum levels. With the severity of cognitive impairments in schizophrenia, VEGF levels decreased gradually. Interestingly, VEGF may be involved in the mechanisms underlying cognitive function in remitted patients, although the mechanism about the association remains poorly understood. VEGF may serve as a sensitive monitor to estimate the degree of cognitive impairments and clinical prognosis in schizophrenia.
Availability of data and materials
The data that support the findings of this study contain sensitive personal information and thus are not publicly available as they are subject to secrecy. The datasets used during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CFET:
-
Chinese Facial Emotion Test
- DST:
-
Digit span tests
- HC:
-
Healthy control
- HVLT-R:
-
Hopkins Verbal Learning Test-Revised
- NRS:
-
Non-remitted first episode schizophrenia
- RS:
-
Remitted first-episode schizophrenia
- TMT:
-
Trail making tests
- VFT:
-
Verbal fluency tests
References
Wu JQ, Chen da C, Tan YL, Xiu MH, Yang FD, Soares JC, Zhang XY. Cognitive impairments in first-episode drug-naive and chronic medicated schizophrenia: MATRICS consensus cognitive battery in a Chinese Han population. Psychiatry Res 2016, 238:196–202.
Bora E. Developmental lag and course of cognitive deficits from the premorbid to postonset period in schizophrenia. Am J Psychiatry. 2014;171(3):369.
A Ü, Direk N, Koyuncu A, Keskin-Ergen Y, Yüksel Ç, Güler J, Karadayı G, Akturan E, Devrim-Üçok M. Cognitive deficits in clinical and familial high risk groups for psychosis are common as in first episode schizophrenia. Schizophr Res. 2013;151(1–3):265.
Eack SM, Mermon DE, Montrose DM, Miewald J, Gur RE, Gur RC, Sweeney JA, Keshavan MS. Social cognition deficits among individuals at familial high risk for schizophrenia. Schizophr Bull. 2010;36(6):1081–8.
Lee SY, Bang M, Kim KR, Lee MK, Park JY, Song YY, Lee E, An SK. Impaired facial emotion recognition in individuals at ultra-high risk for psychosis and with first-episode schizophrenia, and their associations with neurocognitive deficits and self-reported schizotypy. Schizophr Res. 2015;165(1):60–5.
Steen NE, Aas M, Simonsen C, Dieset I, Tesli M, Nerhus M, Gardsjord E, Mørch R, Agartz I, Melle I, et al. Serum levels of second generation antipsychotics are associated with cognitive function in psychotic disorders. World J Biol Psychiatry. 2016;18(6):471–82.
Yasuifurukori N, Kaneda A, Sugawara N, Tomita T, Kaneko S. Effect of adjunctive treatment with aripiprazole to atypical antipsychotics on cognitive function in schizophrenia patients. J Psychopharmacol. 2012;26(6):806.
Caldiroli A, Buoli M, Serati M, Cahn W, Altamura AC. General and social cognition in remitted first-episode schizophrenia patients: a comparative study. Eur Arch Psychiatry Clin Neurosci. 2016.
Bliksted V, Fagerlund B, Weed E, Frith C, Videbech P. Social cognition and neurocognitive deficits in first-episode schizophrenia. Schizophr Res. 2014;153(1–3):9–17.
Savla GN, Vella L, Armstrong CC, Penn DL, Twamley EW. Deficits in domains of social cognition in schizophrenia: a meta-analysis of the empirical evidence. Schizophr Bull. 2013;39(5):979.
Lee TY, Hong SB, Shin NY, Kwon JS. Social cognitive functioning in prodromal psychosis: a meta-analysis. Schizophr Res. 2015;164(3):28–34.
Bora E, Pantelis C. Theory of mind impairments in first-episode psychosis, individuals at ultra-high risk for psychosis and in first-degree relatives of schizophrenia: systematic review and meta-analysis. Schizophr Res. 2013;144(1–3):31–6.
Licht T, Goshen I, Avital A, Kreisel T, Zubedat S, Eavri R, Segal M, Yirmiya R, Keshet E. Reversible modulations of neuronal plasticity by VEGF. Proc Natl Acad Sci U S A. 2011;108(12):5081–6.
Taylor SL, Trudeau D, Arnold B, Wang J, Gerrow K, Summerfeldt K, Holmes A, Zamani A, Brocardo PS, Brown CE. VEGF can protect against blood brain barrier dysfunction, dendritic spine loss and spatial memory impairment in an experimental model of diabetes. Neurobiol Dis. 2015;78:1–11.
Hohman TJ, Bell SP, Jefferson AL. Alzheimer's disease neuroimaging I. the role of vascular endothelial growth factor in neurodegeneration and cognitive decline: exploring interactions with biomarkers of Alzheimer disease. JAMA Neurol. 2015;72(5):520–9.
Cao L, Jiao X, Zuzga DS, Liu Y, Fong DM, Young D, During MJ. VEGF links hippocampal activity with neurogenesis, learning and memory. Nat Genet. 2004;36(8):827–35.
Blumberg HP, Wang F, Chepenik LG, Kalmar JH, Edmiston E, Duman RS, Gelernter J. Influence of vascular endothelial growth factor variation on human hippocampus morphology. Biol Psychiatry. 2008;64(10):901–3.
Pillai A, Howell KR, Ahmed AO, Weinberg D, Allen KM, Bruggemann J, Lenroot R, Liu D, Galletly C, Weickert CS, et al. Association of serum VEGF levels with prefrontal cortex volume in schizophrenia. Mol Psychiatry. 2016;21(5):686–92.
Tang H, Mao X, Xie L, Greenberg DA, Jin K. Expression level of vascular endothelial growth factor in hippocampus is associated with cognitive impairment in patients with Alzheimer's disease. Neurobiol Aging. 2013;34(5):1412–5.
Chiappelli M, Borroni B, Archetti S, Calabrese E, Corsi MM, Franceschi M, Padovani A, Licastro F. VEGF gene and phenotype relation with Alzheimer's disease and mild cognitive impairment. Rejuvenation Res. 2006;9(4):485–93.
Andreasen NC, Jr CW, Kane JM, Lasser RA, Marder SR, Weinberger DR. Remission in schizophrenia: proposed criteria and rationale for consensus. Am J Psychiat. 2005;162(3):441–9.
Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998, 59 Suppl 20:22–33; quiz 34-57.
Oral E, Canpolat S, Yildirim S, Gulec M, Aliyev E, Aydin N. Cognitive functions and serum levels of brain-derived neurotrophic factor in patients with major depressive disorder. Brain Res Bull. 2012;88(5):454–9.
Tang XW, Yu M, Duan WW, Zhang XR, Sha WW, Wang X, Zhang XB. Facial emotion recognition and alexithymia in Chinese male patients with deficit schizophrenia. Psychiatry Res. 2016;246:353–9.
Miotto EC, Campanholo KR, Rodrigues MM, Serrao VT, Lucia MC, Scaff M. Hopkins verbal learning test-revised and brief visuospatial memory test-revised: preliminary normative data for the Brazilian population. Arq Neuropsiquiatr. 2012;70(12):962.
Bodén R, Sundström J, Lindström E, Lindström L. Association between symptomatic remission and functional outcome in first-episode schizophrenia. Schizophr Res. 2009;107(2–3):232–7.
Bobes J, Ciudad A, Álvarez E, San L, Polavieja P, Gilaberte I. Recovery from schizophrenia: results from a 1-year follow-up observational study of patients in symptomatic remission. Schizophr Res. 2009;115(1):58–66.
Balogh N, Égerházi A, Berecz R. Neurocognitive changes in patients with schizophrenia during relapse and early remission. Eur J Psychiatry. 2015;29(3):199–209.
Mier D, Kirsch P. Social-cognitive deficits in schizophrenia. Curr Top Behav Neurosci. 2016;30:397–409.
Goghari VM, Sponheim SR. More pronounced deficits in facial emotion recognition for schizophrenia than bipolar disorder. Compr Psychiatry. 2013;54(4):388–97.
Guastella AJ, Hermens DF, Van ZA, Naismith SL, Lee RS, Cacciotti-Saija C, Scott EM, Hickie IB. Social cognitive performance as a marker of positive psychotic symptoms in young people seeking help for mental health problems. Schizophr Res. 2013;149(1–3):77–82.
Balogh N, Egerházi A, Berecz R, Csukly G. Investigating the state-like and trait-like characters of social cognition in schizophrenia: a short term follow-up study. Schizophr Res. 2014;159(2–3):499.
Rodríguez Sosa JT, Gil Santiago H, Trujillo Cubas A, Winter Navarro M, León Pérez P, Guerra Cazorla LM, Martín Jiménez JM. Social cognition in patients with schizophrenia, their unaffected first degree relatives and healthy controls. Comparison between groups and analysis of associated clinical and sociodemographic variables. Revista De Psiquiatria Y Salud Mental. 2013;6(4):160–7.
Fernandezgonzalo S, Jodar M, Pousa E, Turon M, Garcia R, Rambla CH, Palao D. Selective effect of neurocognition on different theory of mind domains in first-episode psychosis. J Nerv Ment Dis. 2014;202(8):576–82.
Mehta UM, Thirthalli J, Subbakrishna DK, Gangadhar BN, Eack SM, Keshavan MS. Social and neuro-cognition as distinct cognitive factors in schizophrenia: a systematic review. Schizophr Res. 2013;148(1–3):3–11.
Ye F, Zhan Q, Xiao W, Tang X, Li J, Dong H, Sha W, Zhang X. Altered serum levels of vascular endothelial growth factor in first-episode drug-naive and chronic medicated schizophrenia. Psychiatry Res. 2018;264:361–5.
Xiao W, Zhan Q, Ye F, Tang X, Li J, Dong H, Sha W, Zhang X. Elevated serum vascular endothelial growth factor in treatment-resistant schizophrenia treated with electroconvulsive therapy: positive association with therapeutic effects. World J Biol Psychiatry. 2018;20(2):150–8.
Xiao W, Zhan Q, Ye F, Tang X, Li J, Dong H, Sha W, Zhang X. Baseline serum vascular endothelial growth factor levels predict treatment response to antipsychotic medication in patients with schizophrenia. Eur Neuropsychopharmacol. 2018;28(5):603–9.
Frydecka D, Krzystek-Korpacka M, Lubeiro A, Stramecki F, Stanczykiewicz B, Beszlej JA, Piotrowski P, Kotowicz K, Szewczuk-Boguslawska M, Pawlak-Adamska E, et al. Profiling inflammatory signatures of schizophrenia: a cross-sectional and meta-analysis study. Brain Behav Immun. 2018;71:28–36.
Nguyen TT, Dev SI, Chen G, Liou SC, Martin AS, Irwin MR, Carroll JE, Tu X, Jeste DV, Eyler LT. Abnormal levels of vascular endothelial biomarkers in schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2018;268(8):849–60.
Mohammadi A, Rashidi E, Amooeian VG. Brain, blood, cerebrospinal fluid, and serum biomarkers in schizophrenia. Psychiatry Res. 2018;265:25–38.
Misiak B, Stramecki F, Stanczykiewicz B, Frydecka D, Lubeiro A. Vascular endothelial growth factor in patients with schizophrenia: a systematic review and meta-analysis. Prog Neuro-Psychopharmacol Biol Psychiatry. 2018;86:24–9.
Krivoy A, Hochman E, Sendt KV, Hollander S, Vilner Y, Selakovic M, Weizman A, Taler M. Association between serum levels of glutamate and neurotrophic factors and response to clozapine treatment. Schizophr Res. 2018;192:226–31.
Józwiak-Bebenista M, Jasinska-Stroschein M, Kowalczyk E. Involvement of vascular endothelial growth factor (VEGF) and mitogen-activated protein kinases (MAPK) in the mechanism of neuroleptic drugs. Pharmacol Rep. 2018;70(5):1032–9.
Jais A, Solas M, Backes H, Chaurasia B, Kleinridders A, Theurich S, Mauer J, Steculorum SM, Hampel B, Goldau J, et al. Myeloid-cell-derived VEGF maintains brain glucose uptake and limits cognitive impairment in obesity. Cell. 2016;165(4):882–95.
Ng T, Cheung YT, Ng QS, Ho HK, Chan A. Vascular endothelial growth factor inhibitors and cognitive impairment: evidence and controversies. Expert Opin Drug Saf. 2014;13(1):83–92.
Maass A, Duzel S, Brigadski T, Goerke M, Becke A, Sobieray U, Neumann K, Lovden M, Lindenberger U, Backman L, et al. Relationships of peripheral IGF-1, VEGF and BDNF levels to exercise-related changes in memory, hippocampal perfusion and volumes in older adults. NeuroImage. 2016;131:142–54.
Zhao Q, Niu Y, Matsumoto K, Tsuneyama K, Tanaka K, Miyata T, Yokozawa T. Chotosan ameliorates cognitive and emotional deficits in an animal model of type 2 diabetes: possible involvement of cholinergic and VEGF/PDGF mechanisms in the brain. BMC Complement Altern Med. 2012;12:188.
During MJ, Cao L. VEGF, a mediator of the effect of experience on hippocampal neurogenesis. Curr Alzheimer Res. 2006;3(1):29–33.
Wang Y, Galvan V, Gorostiza O, Ataie M, Jin K, Greenberg DA. Vascular endothelial growth factor improves recovery of sensorimotor and cognitive deficits after focal cerebral ischemia in the rat. Brain Res. 2006;1115(1):186–93.
Plaschke K, Staub J, Ernst E, Marti HH. VEGF overexpression improves mice cognitive abilities after unilateral common carotid artery occlusion. Exp Neurol. 2008;214(2):285–92.
Ortuzar N, Rico-Barrio I, Bengoetxea H, Argandona EG, Lafuente JV. VEGF reverts the cognitive impairment induced by a focal traumatic brain injury during the development of rats raised under environmental enrichment. Behav Brain Res. 2013;246:36–46.
Yang J, Yao Y, Chen T, Zhang T. VEGF ameliorates cognitive impairment in in vivo and in vitro ischemia via improving neuronal viability and function. NeuroMolecular Med. 2014;16(2):376–88.
Nielsen RE, Levander S, Kjaersdam TG, Jensen SO, ØC T, Leucht S. Second-generation antipsychotic effect on cognition in patients with schizophrenia--a meta-analysis of randomized clinical trials. Acta Psychiatr Scand. 2015;131(3):185–96.
Acknowledgements
We thank the psychiatric inpatient unit of Wu Tai Shan Hospital of Yangzhou, China, we are grateful to the funding of this study. We also express our thanks to our colleagues, who assisted in subject recruitment in this study.
Funding
The work was supported by Scientific research foundation of Jiangsu Provincial 333 Project (BRA2015541, BRA2016555), Medical scientific research project of Jiangsu Provincial Commission of Health and Family Planning (No. H2018041), Medical youth talent projects in Jiangsu Province (No. QNRC2016314), and Postgraduate Research & Practice Innovation Program of Jiangsu Province (No. KYCX18_1497). The funding body had no further role in study design and collection, analysis, interpretation of data or in writing the manuscript.
Author information
Authors and Affiliations
Contributions
YQZ, WHX and XBZ were responsible for study design, statistical analysis, and manuscript preparation. YQZ, WHX, KYC, XWT, FY, QQZ were responsible for recruiting the subjects and collected clinical data and performing the clinical rating. XBZ, XWT were providing the funding for the study. All authors contributed to manuscript preparation and approved its final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Ethics Review Committee of Yangzhou WuTaiShan Hospital approved the study (NO. 201602). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed written consent was obtained from all participants prior to the commencement of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Zhao, Y., Xiao, W., Chen, K. et al. Neurocognition and social cognition in remitted first-episode schizophrenia: correlation with VEGF serum levels. BMC Psychiatry 19, 403 (2019). https://doi.org/10.1186/s12888-019-2397-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-019-2397-8