Abstract
Schizophrenia is associated with chronic low-grade inflammation, which has been linked to increased vascular risk and rates of cardiovascular disease. Levels of vascular endothelial growth factor (VEGF), intercellular adhesion molecule-1 (ICAM-1), and vascular cell adhesion molecule-1 (VCAM-1) have been related to aging and neurodegeneration, but their role in schizophrenia remains uncertain. Using a cross-sectional, case–control design, this study included 99 outpatients with schizophrenia and 99 healthy comparison subjects (HCs). Sociodemographic and clinical data were collected, and plasma levels of VEGF, ICAM-1, and VCAM-1 were assayed. A “vascular endothelial index” (VEI) was computed using logistic regression to create a composite measure that maximally differed between groups. General linear models were conducted to examine the possible role of demographic, physical, and lifestyle factors. A linear combination of ICAM-1 and VCAM-1 levels best distinguished the groups, with significantly higher levels of this composite VEI in persons with schizophrenia than HCs. Group differences in the VEI persisted after adjustment for BMI and cigarette smoking. Neither age nor gender was significantly related to the VEI. Schizophrenia patients with higher VEI had earlier age of disease onset, higher systolic and diastolic blood pressure, lower high-density lipoprotein cholesterol, higher insulin resistance, lower levels of mental well-being, and higher Framingham Coronary Heart Disease Risk scores. Schizophrenia is characterized by an elevation of vascular endothelial biomarkers, specifically cell adhesion molecules poised at the intersection between inflammatory response and vascular risk. Interventions aimed at reducing vascular risk may help reduce vascular endothelial abnormalities and prevent cardiovascular morbidity and mortality in schizophrenia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Schizophrenia is a complex neuropsychiatric disorder that affects approximately 1% of the world’s population. While the disease has traditionally been considered a brain disorder, schizophrenia involves not only psychiatric and cognitive pathology but also physiological abnormalities. Notably, cardiovascular disease (CVD) is more than twice as common in schizophrenia as in the general population and is likely a major source of medical morbidity [1, 2]. It has been suggested that an overactive inflammatory system may contribute to the gradual physiological “wear and tear” of several systemic processes in serious mental illnesses [3]. Specifically, a maladaptive and prolonged inflammatory response may play a key role in the development and maintenance of CVD in schizophrenia.
Schizophrenia is associated with a chronic low-grade inflammation, characterized by higher levels of pro-inflammatory interleukin (IL)-6, IL-1β, and tumor necrosis factor alpha (TNFα) [4] and lower levels of IL-2 [5] than in healthy comparison subjects (HCs). We have previously reported on elevated levels of IL-6, TNFα, and high-sensitivity C-reactive protein (hsCRP) in patients with schizophrenia compared to HCs in our study sample [6, 7]. Theoretical models have described inflammation both as an early risk factor for developing symptoms as well as a marker of worsening disease state [8, 9]. Inflammation is also linked to increased vascular risk and contributes to subsequent development of hypertension, atherosclerosis, and ischemic stroke [10,11,12,13]. Intracellular adhesion molecule-1 (ICAM-1), human vascular cellular adhesion molecule-1 (VCAM-1), and vascular endothelial growth factor (VEGF) are three vascular endothelial biomarkers poised at the intersection between inflammatory response and vascular risk [14]. An increase in circulating levels of pro-inflammatory cytokines triggers the production of ICAM-1 and VCAM-1 near the endothelial layer (EL) of the vessel wall; these markers are responsible for aiding leukocyte adhesion to the EL during normal immune response, but prolonged exposure can lead to pathological changes in the EL [15]. Specifically, increased adhesion of leukocytes can result in EL breakdown, ultimately promoting an atherosclerotic process characterized by the build-up of plaques and weakening of the vessel wall [16]. VEGF is a signal protein involved in angiogenesis [17]. Elevations in peripheral levels of VEGF are typically present when blood flow is inadequate, functioning to stimulate greater permeability in the EL and in the formation of new capillaries to restore oxygen supply. Chronic over-expression of VEGF is also associated with diabetes [18], CVD and stroke risk [19], and cancer [20]. Thus, chronic elevations in ICAM-1, VCAM-1 and VEGF may reflect poor endothelial health and have been linked to greater CVD risk.
Vascular endothelial health deteriorates with age, and advanced age is a major risk factor for the development of CVD [21, 22]. Studies have reported age-related changes in circulating levels of these biomarkers. Serum levels of ICAM-1 and VCAM-1 increase with age in healthy older adults without vascular risk factors [23, 24], older adults with hypercholesterolemia or heart disease [25], and those diagnosed with age-related neurodegenerative disorders (e.g., Alzheimer’s disease [26]). The increased physical comorbidity, mortality, and physiological changes in schizophrenia are suggestive of accelerated biological aging [27]. Elucidation of the role of vascular endothelial biomarkers in schizophrenia is important to understanding the aging process. Gender is another potentially important covariate. Studies have been largely mixed [28, 29], but one has suggested that estrogen might be a protective factor for mitigating vascular endothelial risk. Thus, more studies are needed to fully elucidate the nature of the relationships of vascular inflammation to age and gender.
In persons with schizophrenia, there have been reports of higher, lower, and no differences in ICAM-1, VCAM-1 or VEGF levels compared to HCs [30,31,32]. These inconsistent findings may reflect varying clinical characteristics of the samples studied [31, 33, 34]. A more thorough investigation of vascular endothelial biomarkers of inflammation in well-characterized patients with schizophrenia is warranted to disentangle potential contributions of clinical and medical co-morbid features of this disorder. Furthermore, it would be useful to understand the interplay between these biomarkers and how this may differ in people with and without schizophrenia. For this reason, an approach that creates a composite measure that summarizes the relative contribution of individual biomarkers to group differences can be informative and reduce the risk of false positives due to multiple group comparisons of individual biomarkers.
This study aimed to characterize group differences between people with schizophrenia and HCs on levels of VEGF, ICAM-1, and VCAM-1. We created a “vascular endothelial index” (VEI) based on the linear combination of markers that differed most between the two groups. We hypothesized that vascular endothelial levels would be elevated in schizophrenia relative to demographically comparable HCs. Additionally, we examined the relationship of age and gender to the VEI and the interactions between these demographic factors and diagnosis. We also explored whether adjusting for BMI and cigarette smoking, factors that correlate with vascular endothelial dysfunction [35,36,37] and are reported to be elevated in schizophrenia [38, 39], would reduce diagnostic group differences. Finally, we examined associations of the VEI with physical health and cognitive variables as well as disease-specific clinical factors in the schizophrenia group (e.g., symptom severity).
Methods
Participants
Outpatients with schizophrenia (n = 79) or schizoaffective disorder (n = 55) and HCs (n = 113), all between the ages of 26 and 65 years, were included. The diagnoses of schizophrenia and schizoaffective disorder were made based on the Structured Clinical Interview for the DSM-IV-TR (SCID) [40]. Several papers have demonstrated similarities between schizoaffective disorder and schizophrenia [41, 42]. Additionally, the two patient subgroups did not differ significantly on mean age, duration or severity of mental illness, physical health (BMI, medical comorbidity) or cognition. Therefore, we combined them for subsequent analyses and refer to the group as “schizophrenia”. HCs completed the Mini-International Neuropsychiatric Interview (MINI) to rule out any history of major neuropsychiatric illnesses [43]. Methods have been previously reported in [6, 7, 44, 45]. Exclusion criteria were: (1) other current major DSM-IV-TR Axis I diagnoses; (2) alcohol or other substance (other than tobacco) abuse or dependence within 3 months prior to enrollment; (3) diagnosis of dementia, intellectual disability disorder, or a major neurological disorder; (4) any medical disability that interfered with a subject’s ability to complete the study procedures. All procedures were approved by the University of California, San Diego Human Research Protections Program. All participants provided written informed consent. For additional details regarding recruitment and subject selection criteria please see Joseph et al. [7].
Sociodemographic and clinical characteristics
Sociodemographic characteristics (i.e., age, education, gender, race/ethnicity, current smoking status) and illness-related factors (i.e., age of onset and duration of illness, daily antipsychotic medication dosages) were ascertained through participant interview and review of available research and medical records. Daily dosages of antipsychotic medication were converted to total World Health Organization-defined daily dose [46]. Body mass index (BMI) was based on assessment of height and weight (kg/m2).
Psychosocial and cognitive assessments
Positive and negative psychiatric symptoms were evaluated using interviewer-administered Scales for Assessment of Positive Symptoms and Negative Symptoms [SAPS and SANS, respectively; 47, 48]. Depression was assessed using the Patient Health Questionnaire [PHQ-9; 49]. Health-related quality of life and functioning was evaluated using the physical and mental health component scores from the Medical Outcomes Study 36-item Short Form [SF-36; 50]. Medical comorbidity was measured with the total score and severity index from the Cumulative Illness Rating Scale [CIRS; 51] and, specifically, vascular comorbidity was measured by the CIRS vascular score. Framingham coronary heart disease (CHD) and CVD risk scores were calculated using data collected in the CIRS. The Framingham 10-year CHD relative risk score was calculated using age, low density and high-density lipoprotein cholesterol (LDL, HDL), systolic and diastolic blood pressure, presence of diabetes, and current smoking according to Wilson et al. [52]. The Framingham 10-year CVD Risk was calculated using age, BMI, systolic blood pressure, current smoking, and diabetes according to D’Agostino et al. [53].
Cognition, specifically in the domain of executive function which has been shown to be impacted by inflammation in schizophrenia [54, 55], was assessed using the Delis–Kaplan Executive Function System [D-KEFS; 56]; specifically, the scores for Trail Making Test Letter-Number Switching, Color-Word Interference Inhibition Switching, and Letter Fluency were of interest. D-KEFS raw scores were converted into z scores relative to each measure’s mean, coded such that higher scores represented better performance, and averaged to create an Executive Functioning Composite score [57].
All assessments were performed by study staff members who underwent rigorous training and inter-rater reliability certification. Staff were trained in the administration of standardized assessments by shadowing senior raters and were observed while performing assessments.
Biomarker assays
Fasting blood was collected in ethylenediaminetetraacetic acid (EDTA)-treated vacutainers. Samples underwent refrigerated centrifugation at 3000 rpm, and plasma was stored at −80 °C until assay. Plasma levels of ICAM-1, VCAM-1, and VEGF were quantified using Meso Scale Discovery MULTI-SPOT® Assay System (MSD, Rockville, MD, USA) and analyzed on a SECTOR Imager 2400 instrument (MSD). Using MSD Discovery Workbench® analysis software (MSD), standard curves were formed by fitting ECL signal from calibrators to a four-parameter logistic model with a 1/y 2 weighting. Samples were run in duplicates, using V-PLEX Human Biomarker panels (Catalog # K151A0H-2). V-PLEX kits are fully validated according to fit-for-purpose principles and the FDA’s analytical validation guidelines according to the manufacturer (MSD). The laboratory technician who performed the assays was blind to the diagnostic group from which each sample was drawn. Intra-assay variability was less than 5% and inter-assay variability was less than 10% for all three assays. The lowest detected levels for each biomarker were: 1.19 ng/mL (ICAM-1), 2.88 ng/mL (VCAM-1), and 0.29 pg/mL (VEGF) [58]. No sample showed biomarker levels below the detection limits.
Statistical analysis
Statistical analyses were conducted using SPSS Statistics version 20.0 [59] and R [60]. Variables were inspected for violations of assumptions of normality, homogeneity of variance, and linearity for all variables required for parametric analyses. Values of all biomarkers were log10-transformed to approximate a normal distribution. An alpha level of p < 0.05 was used to determine statistical significance. Measures of sociodemographic, clinical, and physical health characteristics were analyzed using independent samples t tests and Chi-square statistics for continuous and discrete variables, respectively. Groups were comparable in mean age, but differed significantly on race/ethnicity distribution (p = 0.004) and nearly significantly on gender (p = 0.063). Therefore, we created a 1:1 gender- and race-matched sample (n = 99 in each group) using the case–control matching procedure in SPSS. The final schizophrenia sample included 55 patients diagnosed with schizophrenia and 44 with schizoaffective disorder. Analyses presented below are based on these two subgroups. Independent samples t tests were also used to compare levels of each vascular biomarker between diagnostic groups. Cohen’s d effect sizes were calculated for group differences, and effect sizes greater than 0.30 were interpreted as greater than a small effect. To understand how vascular biomarker levels in schizophrenia might relate to one another and jointly distinguish between those with and without the disorder, a VEI was created using backward stepwise logistic regression with group as the dependent variable. The index was calculated by creating a linear composite of the intercept and value of each significant predictor, weighted by parameter estimates from the logistic regression model. On average, the VEI will necessarily significantly differ between groups because it was designed to do so. The direction, composition, and weighting of biomarkers contributing to the VEI are of interest, however. Importantly, it reduces each individual’s set of biomarker levels to a single value that indicates the degree of abnormality of each participant’s weighted profile of vascular endothelial markers. Note that, since the VEI composite score was constructed from estimates of the logistic regression, the VEI outcomes are not stochastically independent. Variances of parameter estimates from the linear regression were adjusted to account for such dependency by taking into consideration the sampling variability of the estimated VEI composite score. Details about the methods used are available from the authors.
Subsequently, we examined the differential relationships of age and gender, which have been established in the literature as potentially impacting vascular endothelial levels, on the VEI between the schizophrenia and HC groups. General linear models were conducted with age and gender (and their respective interactions) as covariates. Additionally, to consider the potential confounding role of physical and lifestyle factors, BMI and cigarette smoking (and their respective interactions) were also included as covariates in the same model, given that they were significantly different between schizophrenia and HC groups and are highly relevant to vascular inflammation.
Clinical, physical health, and cognitive correlates of VEI were examined in each group, including illness-specific variables in the schizophrenia group, using Pearson’s r correlations. Additionally, we examined the relationship of the VEI with other physiological biomarkers of inflammation (e.g., chemokines, cytokines) and oxidative stress (e.g., F2 isoprostanes) found to be abnormal in patients with schizophrenia on which our group has previously reported. These include pro-inflammatory cytokines IL-6 and TNFα [6], chemokines Eotaxin-1 (CCL11) and macrophage-derived chemokine (MDC/CCL22), combined into a single “chemokine index” [44], hsCRP [7], and F2 isoprostanes [45].
Results
Sample characteristics
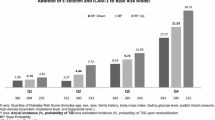
Sociodemographic, psychiatric, and physical health characteristics for the schizophrenia and HC groups are presented in Table 1. Our gender- and race-matched schizophrenia and HC groups did not differ on age. As expected, persons with schizophrenia had lower levels of educational attainment, worse psychiatric symptoms, higher depression levels, lower levels of physical and mental well-being, poorer executive functioning, higher rates of smoking, greater medical co-morbidity, higher BMI, and greater risk for developing coronary heart disease and cardiovascular disease. Additionally, gender differences were observed in both groups on measures of cardiovascular health, including HDL, LDL, triglycerides, and HDL-triglycerides ratio (Supplemental Table 1). Plasma ICAM-1 levels were significantly higher in the schizophrenia group compared to the HCs, with a borderline-medium effect size. No group differences were observed for VEGF or VCAM-1.
Vascular endothelial index
VEGF, ICAM-1, and VCAM-1 were entered in backward model selection into a logistic regression with group membership as the dependent variable. The final model was significant, χ 2(2) = 15.4, p < 0.001, Nagelkerke R 2 = 0.10, with ICAM-1 entered on the first step and VCAM-1 entered on the second step. Levels of ICAM-1 (Wald test = 13.6, p < 0.001) and VCAM-1 (Wald test = 10.4, p = 0.001) were both significantly related to group membership. The VEI was calculated from model parameter estimates using the following equation: − 2.047 + [5.183 × log10(ICAM-1)] + [− 4.370 × log10(VCAM-1)]. Note that, ICAM-1 has a slightly stronger weight than VCAM-1, and the VEI reflects the balance of these two biomarkers with a positive sign for ICAM-1 and negative weighting for VCAM-1. As expected, VEI was significantly different in the schizophrenia group than HCs with a medium effect size (p < 0.001, Cohen’s d = 0.57). The direction of this difference is that the composite VEI is higher in schizophrenia participants than HCs.
Relationship to age and gender and role of other potential confounds
A general linear model of the VEI testing the differential effects of age and group and accounting for BMI and cigarette smoking revealed an expected main effect of group, z = 2.06, p = 0.038, and a main effect of BMI, z = 2.62, p = 0.01. Even after adjusting for BMI and smoking, the VEI remained higher in patients with schizophrenia (0.078 ± 0.08) compared to HCs (−0.107 ± 0.06). Moreover, regardless of group, individuals with higher BMI had higher values on the VEI (β = 0.33, p < 0.001). The main effects of age, z = 0.61, p = 0.540, gender, z = −0.47, p = 0.640, and smoking, z = 1.76, p = 0.078, were not significant; none of the interactions with group were significant (ps > 0.10).
Psychiatric, physical health, and cognitive correlates
Table 2 displays correlations of the VEI with psychiatric, physical health, and cognitive measures as well as other biomarker variables for each group. Schizophrenia patients with higher (more abnormal) VEI were younger and had higher systolic and diastolic blood pressure, lower HDL cholesterol, higher insulin and insulin resistance, higher levels of leukocytes, greater depression, lower levels of self-reported mental well-being, and higher Framingham CHD and CVD risk scores. Among the HCs, VEI was higher in non-Caucasians and those with higher BMI, worse medical comorbidity, higher systolic/diastolic blood pressure, greater triglycerides to HDL cholesterol ratio, higher levels of glycated hemoglobin, higher insulin and insulin resistance, higher Framingham CHD risk scores, higher leukocyte levels, and poorer executive functioning. Earlier age of onset was related to higher VEI in schizophrenia, but duration of illness, antipsychotic exposure, and severity of psychotic symptoms were not.
Relationship with other biomarkers
We also examined the relationship between the VEI and other physiological biomarkers of inflammation [6, 7, 44] and oxidative stress [45]. Higher VEI was associated with elevated IL-6 and hsCRP levels in schizophrenia and only hsCRP in HCs (Table 2). Correlations were followed up with general linear models to assess group differences in VEI, independent of additional biomarkers. The main effect of group remained significant after adjusting for IL-6, z = 2.48, p = 0.013 (overall model fit: R 2 = 0.12). The main effect of IL-6, z = 1.30, p = 0.19, and group × IL-6 interaction were not significant, z = 1.01, p = 0.31.
In the general linear model including hsCRP, the main effect of group remained significant, z = 2.12, p = 0.034 (overall model fit: R 2 = 0.21). The main effect of hsCRP was also significant F(1,190) = 2.92, p = 0.004, with higher levels of hsCRP associated with higher VEI. The group × hsCRP interaction was not significant, z = −1.83, p = 0.067.
Discussion
Partially consistent with our hypothesis, when considered individually, plasma levels of ICAM-1 were higher in schizophrenia compared to HCs, but VEGF and VCAM-1 levels were not. When considered together in a logistic regression analysis to distinguish between those with and without schizophrenia, however, levels of both ICAM-1 and VCAM-1 were related to group membership with slightly stronger weighting for ICAM-1 and negative weighting of VCAM-1. The weighted linear combination of these two biomarkers, which we call the VEI, was elevated in schizophrenia. We sought to explore the relationship of age and gender with vascular endothelial levels, and neither age nor gender was significantly related to the VEI, nor were their interactions with group. In terms of the role of potential confounds, group differences did not appear to be explained by group differences in BMI or smoking.
The existing literature presents inconsistent findings for ICAM-1 and VCAM-1 [31, 34, 61, 62], with some reporting higher levels of ICAM-1 compared to HCs [33, 34], and others showing lower levels or no group differences. Discrepancies amongst investigations may reflect the heterogeneous nature of schizophrenia, particularly at different stages of the disorder. Recently, Stefanović [34] observed that ICAM-1 levels in schizophrenia were comparable to those of HCs in early stages of the disorder but elevated in late stages. Decreased ICAM-1 expression may reflect reduced activation of the immune system during acute phases of schizophrenia [63,64,65], while increased expression during late stages may indicate immune over-activation [32, 34]. The latter interpretation is consistent with the body of literature suggesting that schizophrenia is associated with a chronic pro-inflammatory state [66, 67]. Although VCAM-1 levels were not significantly higher in the schizophrenia group compared with HCs, it, together with ICAM-1, was a significant predictor of group membership, suggesting that the interrelation between adhesion molecules is important. Consequently, examining these markers together may be more informative than individually. Finally, in contrast with previous studies [30, 68], we did not observe group differences in VEGF between schizophrenia and HC.
In general, we did not find an effect of age or gender on the VEI, which was surprising given that previous studies reported that vascular endothelial function seemed to deteriorate with age [21] and women had lower levels of ICAM-1 and VCAM-1 [28, 29, 33, 69]. Interpretation of our negative finding regarding age is limited by several factors including the cross-sectional study design, non-linear aging trajectories, and cohort and sampling effects. In fact, when simple correlations were explored, individuals with schizophrenia who had higher VEI tended to be younger with earlier age of onset, indicating that vascular inflammation may have a greater presence earlier in life in those with the disorder. In line with previous models, vascular inflammation may be both an early risk factor for developing symptoms [9] as well as a marker of worsening disease state [8]. BMI and cigarette smoking are strongly related to vascular risk in the extant literature [35, 70]. In our study, even after adjusting for BMI, the schizophrenia group exhibited higher VEI, suggesting that group differences were not solely due to the schizophrenia group having higher BMI than HCs, although it may be impacted by BMI in both groups. Similarly, adjusting for smoking did not mitigate the group effect, suggesting that group differences were not solely due to schizophrenia group having a larger proportion of smokers than HCs.
As expected, the VEI was positively associated with markers of vascular health in both patients with schizophrenia and HCs, including systolic and diastolic blood pressure, insulin resistance, and an increased Framingham CHD risk score indicating elevated risk for developing coronary heart disease. Although some of these vascular health measures (e.g., systolic and diastolic blood pressure) were within normal limits, the observed positive associations with the VEI suggest that this index may be a more sensitive marker (than the clinical measures), which may help identify individuals who could develop CVD, such as hypertension, at a later point in time and be a longitudinal marker of vascular health. The association between higher VEI and greater physical/medical comorbidity is not surprising, given the role of vascular endothelial proteins in regulating vasculature as well as in the development of atherosclerosis [71,72,73]. Vascular endothelial dysfunction has been described in the literature, often in the context of aging, as a major risk factor for the development of CVD [21, 22]. Furthermore, there is evidence that prolonged stressful life experiences interfere with appropriate regulation of immune response [74], which may lead to chronic stress-induced endothelial dysfunction. ICAM-1 and VCAM-1 are important cell adhesion molecules positioned at the nexus between inflammatory response and vascular risk. Several prior studies by our group, using the same cohort of participants, have revealed elevations in inflammatory biomarkers upstream of ICAM-1 and VCAM-1 [6, 7, 44], and not surprisingly, VEI was associated with leukocytes and hsCRP in both groups and IL-6 in schizophrenia. That the main group effect remained significant with the addition of hsCRP and IL-6 to the model may indicate that inflammation does not completely account for VEI’s ability to differentiate the groups. Additionally, elevated F2-isoprostanes, indicating higher levels of oxidative stress, have been reported in this sample [45], although its relationship with the VEI was not significant. Overall, our results suggest that schizophrenia is characterized by dysfunction of important vascular endothelial biomarkers, which may be related to immune dysfunction and oxidative stress in this population. A large body of the literature suggests that schizophrenia is associated with a chronic pro-inflammatory state [66, 67] and increased oxidative stress-induced cellular damage [45, 75], which may lead to downstream endothelial dysfunction and cardiovascular disease [76, 77]. Results suggest that interventions aimed at reducing inflammation and vascular risk may help reduce vascular endothelial abnormalities and prevent cardiovascular morbidity and mortality as well as, potentially, cognitive dysfunction in schizophrenia.
A novel aspect and particular strength of this study is the investigation of the relationship between vascular endothelial markers and cognition. Previous studies have demonstrated alterations in serum levels of ICAM-1 and VCAM-1 in clinical populations in which cognitive impairment is a key feature [e.g., Alzheimer’s disease; 26], yet very few have investigated direct associations between these biomarkers and cognitive performance. Some have reported worse general cognition with higher ICAM-1 and VCAM-1 [78, 79], while others have found no association [80]. Our finding that greater VEI was associated with poorer executive functioning in the HCs suggests that vascular inflammation may influence cognition, particularly on tasks of executive function, among individuals who are psychiatrically healthy. The lack of relationship between VEI and executive function in schizophrenia may indicate that cognitive impairment and elevated markers of vascular inflammation are present simultaneously, yet somewhat independently, in individuals with schizophrenia. Our findings suggest a need for more targeted investigations to better determine how vascular inflammation may contribute to cognitive impairment.
Finally, higher VEI was associated with increased depression and decreased self-report ratings of mental well-being in the schizophrenia group, which is consistent with existing research indicating elevated levels of ICAM-1, VCAM-1, and VEGF in major depression [81], including late-life depression [82]. This finding further supports the “vascular depression” hypothesis [83], which postulates that cerebrovascular disease may predispose, precipitate, or exacerbate depressive syndromes. It also suggests that vascular inflammation may be an important predictor of depression in individuals with schizophrenia, especially as they age, and has important implications for the management of late-life depression in this population [84].
Several limitations to our study must be acknowledged. First, the cross-sectional design limits our ability to make causal inferences about the role of vascular inflammation in schizophrenia. Prospective longitudinal studies are required to determine whether vascular inflammation is a key pathophysiological feature of the disease. Multiple comparisons conducted in this study inflate the risk of Type I errors. Finally, the patient sample in this analysis primarily consisted of chronic stable outpatients presenting with mild to moderate symptoms, which limits the generalizability of these findings to patients with a more severe disease course or who are acutely ill. Future studies should aim to replicate these findings in an inpatient or antipsychotic-free sample. Finally, amino acids leucine, isoleucine, valine, tyrosine, and phenylalanine have been shown to be predictors of future development of diabetes [85]. These data were not available in this sample of participants, and should be included in future studies of vascular dysfunction in schizophrenia.
In summary, schizophrenia is characterized by an abnormal profile of vascular endothelial biomarkers, and the degree of abnormality is related to increased inflammatory response and poorer vascular health. These factors are important mediators between inflammation and vascular dysfunction and may be one of the mechanisms underlying increased CVD in this population. Future studies should explore the longitudinal trajectory of cell adhesion molecules to determine their contribution to the aging process in schizophrenia. Treatments aimed at normalizing endothelial dysfunction may reduce vascular risk and cardiovascular morbidity and mortality in schizophrenia.
References
Osby U, Westman J, Hallgren J, Gissler M (2016) Mortality trends in cardiovascular causes in schizophrenia, bipolar and unipolar mood disorder in Sweden 1987–2010. Eur J Pub Health 26(5):867–871. doi:10.1093/eurpub/ckv245
Fan Z, Wu Y, Shen J, Ji T, Zhan R (2013) Schizophrenia and the risk of cardiovascular diseases: a meta-analysis of thirteen cohort studies. J Psychiatr Res 47(11):1549–1556. doi:10.1016/j.jpsychires.2013.07.011
Grande I, Magalhães PV, Kunz M, Vieta E, Kapczinski F (2012) Mediators of allostasis and systemic toxicity in bipolar disorder. Physiol Behav 106(1):46–50. doi:10.1016/j.physbeh.2011.10.029
Tomasik J, Rahmoune H, Guest PC, Bahn S (2016) Neuroimmune biomarkers in schizophrenia. Schizophr Res 176(1):3–13. doi:10.1016/j.schres.2014.07.025
Mahendran R, Mahendran R, Chan YH (2004) Interleukin-2 levels in chronic schizophrenia patients. Ann Acad Med Singapore 33(3):320–323
Lee EE, Hong S, Martin AS, Eyler LT, Jeste DV (2016) Inflammation in schizophrenia: cytokine levels and their relationships to demographic and clinical variables. Am J Geriatr Psychiatry 25(1):50–61
Joseph J, Depp C, Martin AS, Daly RE, Glorioso DK, Palmer BW, Jeste DV (2015) Associations of high sensitivity C-reactive protein levels in schizophrenia and comparison groups. Schizophr Res 168(1–2):456–460. doi:10.1016/j.schres.2015.08.019
Khansari N, Shakiba Y, Mahmoudi M (2009) Chronic inflammation and oxidative stress as a major cause of age-related diseases and cancer. Recent Pat Inflamm Allergy Drug Discov 3(1):73–80
Willerson JT, Ridker PM (2004) Inflammation as a cardiovascular risk factor. Circulation 109(21 Suppl 1):II2–II10. doi:10.1161/01.CIR.0000129535.04194.38
Libby P, Ridker PM, Hansson GK (2011) Progress and challenges in translating the biology of atherosclerosis. Nature 473(7347):317–325. doi:10.1038/nature10146
Hotamisligil GS (2006) Inflammation and metabolic disorders. Nature 444(7121):860–867. doi:10.1038/nature05485
Zhou Y, Han W, Gong D, Man C, Fan Y (2016) Hs-CRP in stroke: a meta-analysis. Clin Chim Acta 453:21–27. doi:10.1016/j.cca.2015.11.027
Legein B, Temmerman L, Biessen EA, Lutgens E (2013) Inflammation and immune system interactions in atherosclerosis. Cell Mol Life Sci 70(20):3847–3869. doi:10.1007/s00018-013-1289-1
Hall JR, Wiechmann AR, Johnson LA, Edwards M, Barber RC, Winter AS, Singh M, O’Bryant SE (2013) Biomarkers of vascular risk, systemic inflammation, and microvascular pathology and neuropsychiatric symptoms in Alzheimer’s disease. J Alzheimer’s Dis 35(2):363–371. doi:10.3233/JAD-122359
Liao JK (2013) Linking endothelial dysfunction with endothelial cell activation. J Clin Investig 123(2):540–541. doi:10.1172/JCI66843
Davies MJ, Gordon JL, Gearing AJ, Pigott R, Woolf N, Katz D, Kyriakopoulos A (1993) The expression of the adhesion molecules ICAM-1, VCAM-1, PECAM, and E-selectin in human atherosclerosis. J Pathol 171(3):223–229. doi:10.1002/path.1711710311
Hoeben A, Landuyt B, Highley MS, Wildiers H, Van Oosterom AT, De Bruijn EA (2004) Vascular endothelial growth factor and angiogenesis. Pharmacol Rev 56(4):549–580. doi:10.1124/pr.56.4.3
Kakizawa H, Itoh M, Itoh Y, Imamura S, Ishiwata Y, Matsumoto T, Yamamoto K, Kato T, Ono Y, Nagata M (2004) The relationship between glycemic control and plasma vascular endothelial growth factor and endothelin-1 concentration in diabetic patients. Metabolism 53(5):550–555
Shoamanesh A, Preis SR, Beiser AS, Kase CS, Wolf PA, Vasan RS, Benjamin EJ, Seshadri S, Romero JR (2016) Circulating biomarkers and incident ischemic stroke in the Framingham Offspring Study. Neurology. doi:10.1212/wnl.0000000000003115
Harmey JH (2004) VEGF and cancer. Springer, Berlim
Brandes RP, Fleming I, Busse R (2005) Endothelial aging. Cardiovasc Res 66(2):286–294. doi:10.1016/j.cardiores.2004.12.027
Seals DR, Jablonski KL, Donato AJ (2011) Aging and vascular endothelial function in humans. Clin Sci 120(9):357–375. doi:10.1042/CS20100476
Richter V, Rassoul F, Purschwitz K, Hentschel B, Reuter W, Kuntze T (2003) Circulating vascular cell adhesion molecules VCAM-1, ICAM-1, and E-selectin in dependence on aging. Gerontology 49(5):293–300. doi:10.1159/000071710
Miguel-Hidalgo JJ, Nithuairisg S, Stockmeier C, Rajkowska G (2007) Distribution of ICAM-1 immunoreactivity during aging in the human orbitofrontal cortex. Brain Behav Immun 21(1):100–111
Morisaki N, Saito I, Tamura K, Tashiro J, Masuda M, Kanzaki T, Watanabe S, Masuda Y, Saito Y (1997) New indices of ischemic heart disease and aging: studies on the serum levels of soluble intercellular adhesion molecule-1 (ICAM-1) and soluble vascular cell adhesion molecule-1 (VCAM-1) in patients with hypercholesterolemia and ischemic heart disease. Atherosclerosis 131(1):43–48. doi:10.1016/S0021-9150(97)06083-8
Ewers M, Mielke MM, Hampel H (2010) Blood-based biomarkers of microvascular pathology in Alzheimer’s disease. Exp Gerontol 45(1):75–79. doi:10.1016/j.exger.2009.09.005
Kirkpatrick B, Messias E, Harvey PD, Fernandez-Egea E, Bowie CR (2008) Is schizophrenia a syndrome of accelerated aging? Schizophr Bull 34(6):1024–1032. doi:10.1093/schbul/sbm140
Demerath E, Towne B, Blangero J, Siervogel RM (2001) The relationship of soluble ICAM-1, VCAM-1, P-selectin and E-selectin to cardiovascular disease risk factors in healthy men and women. Ann Hum Biol 28(6):664–678
Chen Y, Osika W, Dangardt F, Gan LM, Strandvik B, Friberg P (2010) High levels of soluble intercellular adhesion molecule-1, insulin resistance and saturated fatty acids are associated with endothelial dysfunction in healthy adolescents. Atherosclerosis 211(2):638–642. doi:10.1016/j.atherosclerosis.2010.03.013
Pillai A, Howell KR, Ahmed AO, Weinberg D, Allen KM, Bruggemann J, Lenroot R, Liu D, Galletly C, Weickert CS, Weickert TW (2016) Association of serum VEGF levels with prefrontal cortex volume in schizophrenia. Mol Psychiatry 21(5):686–692. doi:10.1038/mp.2015.96
Schwarz MJ, Riedel M, Ackenheil M, Müller N (1999) Levels of soluble adhesion molecules in schizophrenia: relation to psychopathology. In: Müller N (ed) Psychiatry, psychoimmunology, and viruses. Springer Vienna, Vienna, pp 121–130. doi:10.1007/978-3-7091-6404-4_13
Schwarz MJ, Riedel M, Ackenheil M, Müller N (2000) Decreased levels of soluble intercellular adhesion molecule-1 (sICAM-1) in unmedicated and medicated schizophrenic patients. Biol Psychiatry 47(1):29–33. doi:10.1016/S0006-3223(99)00206-1
Beumer W, Drexhage RC, De Wit H, Versnel MA, Drexhage HA, Cohen D (2012) Increased level of serum cytokines, chemokines and adipokines in patients with schizophrenia is associated with disease and metabolic syndrome. Psychoneuroendocrinology 37(12):1901–1911. doi:10.1016/j.psyneuen.2012.04.001
Stefanović MP, Petronijević N, Dunjić-Kostić B, Velimirović M, Nikolić T, Jurišić V, Lačković M, Damjanović A, Totić-Poznanović S, Jovanović AA, Ivković M (2016) Role of sICAM-1 and sVCAM-1 as biomarkers in early and late stages of schizophrenia. J Psychiatr Res 73:45–52. doi:10.1016/j.jpsychires.2015.11.002
Al Suwaidi J, Higano ST, Holmes DR Jr, Lennon R, Lerman A (2001) Obesity is independently associated with coronary endothelial dysfunction in patients with normal or mildly diseased coronary arteries. J Am Coll Cardiol 37(6):1523–1528
Schumacher A, Seljeflot I, Sommervoll L, Christensen B, Otterstad J, Arnesen H (2002) Increased levels of markers of vascular inflammation in patients with coronary heart disease. Scand J Clin Lab Invest 62(1):59–68
Steinberg HO, Chaker H, Leaming R, Johnson A, Brechtel G, Baron AD (1996) Obesity/insulin resistance is associated with endothelial dysfunction. Implications for the syndrome of insulin resistance. J Clin Investig 97(11):2601–2610
Coodin S (2001) Body mass index in persons with schizophrenia. Can j Psychiatry Revue 46(6):549–555
de Leon J (1996) Smoking and vulnerability for schizophrenia. Schizophr Bull 22(3):405–409
First M, Spitzer RL, Gibbon M, Williams JB (2002) Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition With Psychotic Screen (SCID-I/PW/PSY SCREEN) New York: Biometrics Research, New York State Psychiatric Institute; 2002; Biometrics Research. New York State Psychiatric Institute, New York
Amann BL, Canales-Rodriguez EJ, Madre M, Radua J, Monte G, Alonso-Lana S, Landin-Romero R, Moreno-Alcazar A, Bonnin CM, Sarro S, Ortiz-Gil J, Gomar JJ, Moro N, Fernandez-Corcuera P, Goikolea JM, Blanch J, Salvador R, Vieta E, McKenna PJ, Pomarol-Clotet E (2016) Brain structural changes in schizoaffective disorder compared to schizophrenia and bipolar disorder. Acta Psychiatr Scand 133(1):23–33. doi:10.1111/acps.12440
Evans JD, Heaton RK, Paulsen JS, McAdams LA, Heaton SC, Jeste DV (1999) Schizoaffective disorder: a form of schizophrenia or affective disorder? J Clin Psychiatry 60(12):874–882
Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC (1998) The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 59:22–33
Hong S, Lee EE, Martin AS, Soontornniyomkij B, Soontornniyomkij V, Achim CL, Reuter C, Irwin MR, Eyler LT, Jeste DV (2016) Abnormalities in chemokine levels in schizophrenia and their clinical correlates. Schizophr Res. doi:10.1016/j.schres.2016.09.019
Lee EE, Eyler LT, Wolkowitz OM, Martin AS, Reuter C, Kraemer H, Jeste DV (2016) Elevated plasma F2-isoprostane levels in schizophrenia. Schizophr Res. doi:10.1016/j.schres.2016.06.011
WHO Collaborating Centre for Drug Statistics Methodology (2009) Guidelines for ATC classification and DDD assignment 2010
Andreasen NC (1983) Scale for the assessment of negative symptoms (SANS). University of Iowa, Iowa City
Andreasen NC (1984) Scale for the assessment of positive symptoms (SAPS). University of Iowa, Iowa City
Kroenke K, Spitzer RL (2002) The PHQ-9: a new depression diagnostic and severity measure. Psychiatr Ann 32(9):509–515
Ware Jr JE, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Medical care 30(6):473–483
Parmelee PA, Thuras PD, Katz IR, Lawton MP (1995) Validation of the cumulative illness rating scale in a geriatric residential population. J Am Geriatr Soc 43(2):130–137
Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB (1998) Prediction of coronary heart disease using risk factor categories. Circulation 97(18):1837–1847
D’Agostino RB Sr, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, Kannel WB (2008) General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation 117(6):743–753. doi:10.1161/CIRCULATIONAHA.107.699579
Frydecka D, Misiak B, Pawlak-Adamska E, Karabon L, Tomkiewicz A, Sedlaczek P, Kiejna A, Beszlej JA (2015) Interleukin-6: the missing element of the neurocognitive deterioration in schizophrenia? The focus on genetic underpinnings, cognitive impairment and clinical manifestation. Eur Arch Psychiatry Clin Neurosci 265(6):449–459. doi:10.1007/s00406-014-0533-5
Bulzacka E, Boyer L, Schurhoff F, Godin O, Berna F, Brunel L, Andrianarisoa M, Aouizerate B, Capdevielle D, Chereau-Boudet I, Chesnoy-Servanin G, Danion JM, Dubertret C, Dubreucq J, Faget C, Gabayet F, Le Gloahec T, Llorca PM, Mallet J, Misdrahi D, Rey R, Richieri R, Passerieux C, Roux P, Yazbek H, Leboyer M, Fond G (2016) Chronic peripheral inflammation is associated with cognitive impairment in schizophrenia: results from the multicentric FACE-SZ dataset. Schizophr Bull 42(5):1290–1302. doi:10.1093/schbul/sbw029
Delis DC, Kaplan E, Kramer JH (2001) The Delis–Kaplan executive function system: examiner’s manual. Psychol Corp, San Antonio
Gibbons LE, Carle AC, Mackin RS, Harvey D, Mukherjee S, Insel P, Curtis SM, Mungas D, Crane PK, Alzheimer’s Disease Neuroimaging I (2012) A composite score for executive functioning, validated in Alzheimer’s Disease Neuroimaging Initiative (ADNI) participants with baseline mild cognitive impairment. Brain Imaging Behav 6(4):517–527. doi:10.1007/s11682-012-9176-1
Calvier L, Legchenko E, Grimm L, Sallmon H, Hatch A, Plouffe BD, Schroeder C, Bauersachs J, Murthy SK, Hansmann G (2016) Galectin-3 and aldosterone as potential tandem biomarkers in pulmonary arterial hypertension. Heart 102(5):390–396. doi:10.1136/heartjnl-2015-308365
IBM Corporation (2011) IBM SPSS Statistics for Macintosh, Version 20.0. IBM Corporation, Armonk, NY
Core Team R (2008) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna
Thomas AJ, Davis S, Ferrier IN, Kalaria RN, O’Brien JT (2004) Elevation of cell adhesion molecule immunoreactivity in the anterior cingulate cortex in bipolar disorder. Biol Psychiatry 55(6):652–655. doi:10.1016/j.biopsych.2003.10.015
Kavzoglu SO, Hariri AG (2013) Intracellular adhesion molecule (ICAM-1), vascular cell adhesion molecule (VCAM-1) and E-selectin levels in first episode schizophrenic patients. Bull Clin Psychopharmacol 23(3):204–214
Arolt V, Rothermundt M, Wandinger KP, Kirchner H (2000) Decreased in vitro production of interferon-gamma and interleukin-2 in whole blood of patients with schizophrenia during treatment. Mol Psychiatry 5(2):150–158
Muller N, Ackenheil M, Hofschuster E, Mempel W, Eckstein R (1991) Cellular immunity in schizophrenic patients before and during neuroleptic treatment. Psychiatry Res 37(2):147–160
Steiner J, Jacobs R, Panteli B, Brauner M, Schiltz K, Bahn S, Herberth M, Westphal S, Gos T, Walter M, Bernstein HG, Myint AM, Bogerts B (2010) Acute schizophrenia is accompanied by reduced T cell and increased B cell immunity. Eur Arch Psychiatry Clin Neurosci 260(7):509–518. doi:10.1007/s00406-010-0098-x
Na KS, Jung HY, Kim YK (2014) The role of pro-inflammatory cytokines in the neuroinflammation and neurogenesis of schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry 48:277–286. doi:10.1016/j.pnpbp.2012.10.022
Monji A, Kato TA, Mizoguchi Y, Horikawa H, Seki Y, Kasai M, Yamauchi Y, Yamada S, Kanba S (2013) Neuroinflammation in schizophrenia especially focused on the role of microglia. Prog Neuropsychopharmacol Biol Psychiatry 42:115–121. doi:10.1016/j.pnpbp.2011.12.002
Lee BH, Hong JP, Hwang JA, Ham BJ, Na KS, Kim WJ, Trigo J, Kim YK (2015) Alterations in plasma vascular endothelial growth factor levels in patients with schizophrenia before and after treatment. Psychiatry Res 228(1):95–99. doi:10.1016/j.psychres.2015.04.020
Muller V, Szabo A, Viklicky O, Gaul I, Portl S, Philipp T, Heemann UW (1999) Sex hormones and gender-related differences: their influence on chronic renal allograft rejection. Kidney Int 55(5):2011–2020. doi:10.1046/j.1523-1755.1999.00441.x
Noguchi T (1999) Soluble intercellular adhesion molecule-1 and vascular cell adhesion molecule-1 concentrations, and leukocyte count in smokers. Environ Health Prev Med 4(2):71–74. doi:10.1007/bf02931997
Pueyo ME, Gonzalez W, Nicoletti A, Savoie F, Arnal JF, Michel JB (2000) Angiotensin II stimulates endothelial vascular cell adhesion molecule-1 via nuclear factor-kappaB activation induced by intracellular oxidative stress. Arterioscler Thromb Vasc Biol 20(3):645–651
O’Brien KD, McDonald TO, Chait A, Allen MD, Alpers CE (1996) Neovascular expression of E-selectin, intercellular adhesion molecule-1, and vascular cell adhesion molecule-1 in human atherosclerosis and their relation to intimal leukocyte content. Circulation 93(4):672–682
van der Wal AC, Das PK, Tigges AJ, Becker AE (1992) Adhesion molecules on the endothelium and mononuclear cells in human atherosclerotic lesions. Am J Pathol 141(6):1427–1433
Cohen S, Janicki-Deverts D, Doyle WJ, Miller GE, Frank E, Rabin BS, Turner RB (2012) Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk. Proc Natl Acad Sci USA 109(16):5995–5999. doi:10.1073/pnas.1118355109
Okusaga OO (2014) Accelerated aging in schizophrenia patients: the potential role of oxidative stress. Aging Dis 5(4):256–262. doi:10.14336/AD.2014.0500256
Madamanchi NR, Vendrov A, Runge MS (2005) Oxidative stress and vascular disease. Arterioscler Thromb Vasc Biol 25(1):29–38. doi:10.1161/01.ATV.0000150649.39934.13
Pearson TA, Mensah GA, Alexander RW, Anderson JL, Cannon RO 3rd, Criqui M, Fadl YY, Fortmann SP, Hong Y, Myers GL, Rifai N, Smith SC Jr, Taubert K, Tracy RP, Vinicor F (2003) Markers of inflammation and cardiovascular disease: application to clinical and public health practice: a statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation 107(3):499–511
Dimopoulos N, Piperi C, Salonicioti A, Mitropoulos P, Kallai E, Liappas I, Lea RW, Kalofoutis A (2006) Indices of low-grade chronic inflammation correlate with early cognitive deterioration in an elderly Greek population. Neurosci Lett 398(1–2):118–123. doi:10.1016/j.neulet.2005.12.064
Rafnsson SB, Deary IJ, Smith FB, Whiteman MC, Rumley A, Lowe GD, Fowkes FG (2007) Cognitive decline and markers of inflammation and hemostasis: the Edinburgh Artery Study. J Am Geriatr Soc 55(5):700–707. doi:10.1111/j.1532-5415.2007.01158.x
Elwan O, Madkour O, Elwan F, Mostafa M, Abbas Helmy A, Abdel-Naseer M, Abdel Shafy S, El Faiuomy N (2003) Brain aging in normal Egyptians: cognition, education, personality, genetic and immunological study. J Neurol Sci 211(1–2):15–22
Iga J, Ueno S, Yamauchi K, Numata S, Tayoshi-Shibuya S, Kinouchi S, Nakataki M, Song H, Hokoishi K, Tanabe H, Sano A, Ohmori T (2007) Gene expression and association analysis of vascular endothelial growth factor in major depressive disorder. Prog Neuropsychopharmacol Biol Psychiatry 31(3):658–663. doi:10.1016/j.pnpbp.2006.12.011
Dimopoulos N, Piperi C, Salonicioti A, Mitsonis C, Liappas I, Lea RW, Kalofoutis A (2006) Elevation of plasma concentration of adhesion molecules in late-life depression. Int J Geriatr Psychiatry 21(10):965–971. doi:10.1002/gps.1592
Alexopoulos GS, Meyers BS, Young RC, Campbell S, Silbersweig D, Charlson M (1997) ‘Vascular depression’ hypothesis. Arch Gen Psychiatry 54(10):915–922
Taylor WD, Aizenstein HJ, Alexopoulos GS (2013) The vascular depression hypothesis: mechanisms linking vascular disease with depression. Mol Psychiatry 18(9):963–974. doi:10.1038/mp.2013.20
Wang TJ, Larson MG, Vasan RS, Cheng S, Rhee EP, McCabe E, Lewis GD, Fox CS, Jacques PF, Fernandez C, O’Donnell CJ, Carr SA, Mootha VK, Florez JC, Souza A, Melander O, Clish CB, Gerszten RE (2011) Metabolite profiles and the risk of developing diabetes. Nat Med 17(4):448–453. doi:10.1038/nm.2307
Acknowledgements
This study was supported in part by National Institutes of Health Grant 5R01MH094151-04 (Jeste), UL1 RR031980 for the UCSD Clinical and Translational Research Institute, the VA Desert-Pacific Mental Illness Research Education and Clinical Center and Office of Academic Affiliations (Nguyen, Eyler), and UC San Diego Stein Institute for Research on Aging. We thank Benchawanna Soontornniyomkij, Ph.D., for her help with the assays of the vascular biomarkers, and Rebecca Daly for her major contributions to data management for the project. Parts of these results were presented at the annual conference of the American College of Neuropsychopharmacology in Hollywood, FL, on December 7, 2016.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Additional information
Dilip V. Jeste and Lisa T. Eyler: Co-senior authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nguyen, T.T., Dev, S.I., Chen, G. et al. Abnormal levels of vascular endothelial biomarkers in schizophrenia. Eur Arch Psychiatry Clin Neurosci 268, 849–860 (2018). https://doi.org/10.1007/s00406-017-0842-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-017-0842-6