Abstract
Background
In sepsis, the relationship between lymphocyte counts and patient outcomes is complex. Lymphocytopenia and lymphocytosis significantly influence survival, illustrating the dual functionality of lymphocytes in responding to infections. This study investigates this complex interaction, focusing on how variations in lymphocyte counts correlate with all-cause hospital mortality among sepsis patients.
Methods
This retrospective cohort study analyzed data from two extensive critical care databases: the Medical Information Mart for Intensive Care IV 2.0 (MIMIC-IV 2.0) from Beth Israel Deaconess Medical Center, Boston, Massachusetts, and the eICU Collaborative Research Database (eICU-CRD), which was Multi-center database from over 200 hospitals across the United States conducted by Philips eICU Research Institute. We included adult patients aged 18 years and older who met the Sepsis-3 criteria, characterized by documented or suspected infection and a Sequential Organ Failure Assessment (SOFA) score of 2 or higher. Sepsis patients were categorized into quartiles based on lymphocyte counts. The primary outcome was all-cause mortality in the hospital, with 90 and 60-day all-cause mortality as the secondary outcomes. Univariable and multivariable Cox proportional hazard regressions were utilized to assess lymphocyte counts' impact on hospital mortality. An adjusted restricted cubic spline (RCS) analysis was performed to elucidate this relationship further. Subgroup analyses were also conducted to explore the association across various comorbidity groups among sepsis and septic shock patients.
Results
Our study included 37,054 patients, with an observed in-hospital mortality rate of 16.6%. Univariable and multivariable Cox proportional hazard regression models showed that lymphocyte counts were independently associated with in-hospital mortality (HR = 1.04, P < 0.01; HR = 1.06, P < 0.01). RCS regression analysis revealed a U-shaped relationship between lymphocyte levels and hospital mortality risk in sepsis and septic shock patients (P for overall < 0.001, P for nonliner < 0.01; P for overall = 0.002, P for nonliner = 0.014). Subgroup analyses revealed that elevated lymphocyte counts correlated with increased hospital mortality among sepsis patients with liver disease and requiring renal replacement therapy (P for overall = 0.021, P for nonliner = 0.158; P for overall = 0.025, P for nonliner = 0.759). These findings suggest that lymphocytes may have enhanced prognostic value in specific subsets of critically ill sepsis patients.
Conclusion
Our findings demonstrate that lymphocyte counts are a significant independent predictor of hospital mortality in sepsis and septic shock patients. We observed a U-shaped association between lymphocyte levels and mortality risk, indicating that high and low counts are linked to increased mortality. This result highlights the complex role of lymphocytes in sepsis outcomes and suggests the need for further investigation into the underlying mechanisms and potential therapeutic approaches. Integrating lymphocyte count assessment into risk stratification algorithms and clinical decision support tools could enhance the early identification of high-risk sepsis patients.
Similar content being viewed by others
Introduction
Sepsis is a potentially fatal clinical syndrome triggered by various infectious syndromes and characterized by a dysregulated systemic inflammatory response. Despite substantial progress in medical interventions and an improved comprehension of its underlying pathophysiological mechanisms, sepsis remains a leading cause of intensive care unit (ICU) admissions. The persistent high incidence of sepsis-related ICU admissions highlights the urgent need for continued research to reduce its clinical burden [1,2,3]. Septic shock and sepsis rapidly advance inflammatory states marked by immunosuppression [4]. Lymphocytes, a critical subset of white blood cells (WBC), comprise 20–40% of the total WBC count [5]. Sepsis-induced lymphocyte apoptosis, associated with adverse outcomes, involves increased cell death and impaired lymphocyte proliferation, significantly reducing circulating lymphocyte percentages [6, 7]. Sepsis triggers the release of pro-apoptotic factors such as glucocorticoids, reactive oxygen species, and pro-inflammatory cytokines, which promote lymphocyte apoptosis [8]. The depletion of lymphocytes, mainly T, B, and natural killer cells, compromises innate and adaptive immune responses. [9, 10]. Sepsis-associated lymphopenia makes patients susceptible to secondary infections, often resulting in prolonged hospital stays and increased mortality rates [11, 12]. Recent studies have explored the relationship between lymphocyte counts and patient outcomes. Kazan et al. found that among COVID-19 patients admitted to the ICU, those with higher lymphocyte levels had better survival rates than individuals with decreased lymphocyte counts, while lower lymphocyte counts on the fifth day of hospitalization correlated with increased mortality [13]. Despite advances in sepsis research, our understanding of the relationship between lymphocyte counts and mortality risk in critically ill sepsis patients remains incomplete [14,15,16]. Furthermore, lymphocytosis is recognized as an indicator of poor clinical outcomes under specific conditions [17].
We hypothesized that a non-linear relationship exists between lymphocyte counts and hospital mortality risk in critically ill sepsis patients. To investigate this, we analyzed the association between lymphocyte counts and all-cause hospital mortality in sepsis patients using data from two large intensive care databases: the Medical Information Mart for Intensive Care IV 2.0 (MIMIC-IV 2.0) and the eICU Collaborative Research Database 2.0 (eICU-CRD 2.0). We aimed to provide a comprehensive understanding of the prognostic significance of lymphocyte counts in sepsis. This research could inform clinical decision-making and improve risk stratification strategies in critical care settings.
Methods
Data source
This retrospective study utilized data from two comprehensive, publicly accessible critical care databases: the Medical Information Mart for Intensive Care IV 2.0 (MIMIC-IV 2.0) and the eICU Collaborative Research Database 2.0 (eICU-CRD 2.0).
The MIMIC-IV 2.0 is a publicly accessible database containing adult (≥ 18 years) medical data from Beth Israel Deaconess Medical Center in Boston, Massachusetts. It covers admissions to medical, surgical, coronary, and cardiac surgery intensive care units from 2008 to 2019. The database provides extensive information, including demographic data, vital sign measurements, comprehensive laboratory test results, detailed medication records, procedural information, ICD coding, and hospital length of stay [18].
The eICU-CRD 2.0, conducted by the Philips eICU Research Institute, is a multi-center database representing over 200 hospitals across the United States from 2014 to 2015. This telehealth archive focuses exclusively on adult ICU patients and includes continuous and intermittent vital signs, laboratory measurements, pharmaceutical records, detailed care plan information, admission diagnoses, and treatment information [19].
Participants
This study enrolled sepsis participants aged 18 or older from the MIMIC-IV 2.0 and eICU-CRD 2.0 databases. Inclusion criteria were as follows:1) Patients with confirmed infections and a Sequential Organ Failure Assessment (SOFA) score of 2 or greater, meeting the Sepsis-3.0 diagnostic criteria, were eligible for inclusion [4]. 2) Complete peripheral blood counts recorded within twenty-four hours of ICU admission.
Exclusion criteria were as follows: 1) ICU stay of less than twenty-four hours; 2) presence of immunodeficiency virus (HIV), rheumatism, malignancies, metastatic neoplasms, or hematological disorders including aplastic anemia; 3) the absence of lymphocyte data on the day of admission; 4) Only the first ICU admission was considered in cases of recurrent hospitalizations.
Data extraction
Clinical data were extracted using SQL queries from the MIMIC-IV 2.0 and eICU-CRD 2.0 databases. The extracted data, primarily from the first 24 h of ICU admission, included: 1) Laboratory assessments: Platelets, monocytes, neutrophil count, lymphocytes, WBC, blood glucose, hemoglobin, albumin, blood urea nitrogen (BUN), creatinine, sodium, potassium, alanine aminotransferase (ALT), aspartate aminotransferase (AST), high-density lipoprotein, low-density lipoprotein, total cholesterol, and triglycerides. 2) Demographic details and vital signs: sex, age, heart rate, systolic and diastolic, temperature, blood pressure, and SOFA score. 3) Blood gas analysis: Lactate, PH, PaO2fio2ratio, Fio2, Paco2, Pao2. 4) ICU-related data: Length of ICU stay and survival status at discharge. 5) Comorbidities and Treatments: congestive heart failure, myocardial infarction, renal disease, chronic pulmonary or liver disease, mechanical ventilatory support, and renal replacement therapy. Average values were employed for variables documented multiple times in the first twenty-four hours post-ICU admission.
Data extraction was performed by our research team member Guyu Zhang, who has extensive experience working with these databases and obtained approval certification number (55,849,941). Before data extraction, all team members underwent training on the structure and content of the MIMIC-IV 2.0 and eICU-CRD 2.0 databases.
Outcome measures
The primary endpoint was all-cause hospital mortality. Secondary outcomes included 60-day and 90-day all-cause hospital mortality, allowing for assessment of both short-term and intermediate-term mortality risks associated with lymphocyte levels.
Statistical analysis
Clinical data were extracted using SQL queries. Continuous variables were presented as mean ± standard deviation for normally distributed data or median and interquartile range for non-normally distributed data. Continuous variables were analyzed using either the Student's t-test for normally distributed data or the Mann–Whitney U test for non-normally distributed data. We employed the Chi-square test or Fisher's exact test as appropriate for categorical variables, presented as proportions.
To explore the independent prognostic significance of lymphocytes on hospital mortality, we performed univariable and multivariable analyses using Cox proportional hazard models facilitated by the 'survival' package in R. Results were reported as hazard ratios (HR) with 95% confidence intervals (CI). Spearman correlation analyses using the R package ‘ggpur’ were performed to prevent overfitting due to multicollinearity. Clinically relevant and prognosis-associated variables such as WBC, gender, age, albumin, creatinine, potassium, temperature, first-day sofa score, and respiratory rate were included in the restricted cubic spline (RCS) model to investigate the associations between lymphocytes and hospital mortality by R package 'rms'. Patients were categorized into quartiles based on lymphocyte counts. Kaplan–Meier survival analysis was conducted to evaluate the incidence rate of hospital mortality across lymphocyte level groups, with group discrepancies assessed by log-rank tests using the R package 'Survminer'. Analyses were further stratified according to diabetes, congestive heart failure, renal disease, liver disease, cerebrovascular disease, invasive ventilation, renal replacement therapy, and chronic pulmonary disease to verify the robustness of the prognostic effect of lymphocytes on hospital mortality. Interactions between lymphocytes and stratification variables were examined using likelihood ratio tests.
Variables with more than 30% missing data, such as lactate, PaO2/FiO2 ratio, pH, FiO2, PaCO2, PaO2, high-density lipoprotein, low-density lipoprotein, total cholesterol, and triglycerides, were excluded from the analysis (Figure S1). The remaining 33 predictor variables, identified at ICU admission, were included. Missing values among these selected variables were imputed using predictive mean matching (PMM) through the 'mice' package. Data analysis was performed with R software, version 4.1.3 (Beijing, China), and statistical significance was established at a two-tailed P-value threshold of < 0.05 for all analyses conducted in the study.
Results
Demographics and clinical characteristics
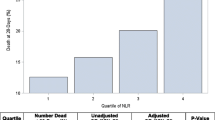
Based on the inclusion criteria, our study included 37,054 sepsis patients (Fig. 1). Table 1 reveals that in the survival group, levels of white blood cells (WBC), neutrophils, monocytes, platelet count, blood urea nitrogen (BUN), creatinine, glucose, potassium, alanine aminotransferase (ALT), aspartate aminotransferase (AST), heart rate, respiratory rate, and age were significantly lower compared to those in the non-survival group. Conversely, levels of lymphocytes, albumin, calcium, and hemoglobin were higher in the survival group. Comorbidities were less prevalent in the survival group than in the non-survival group. Specifically, we observed lower rates of congestive heart failure (24.3% vs. 29.8%, P < 0.001), chronic pulmonary disease (22.5% vs. 24.1%, P < 0.008), myocardial infarction (10.3% vs. 13.5%, P < 0.001), renal diseases (19.9% vs. 25.3%, P < 0.001), liver disease (7.49% vs. 15.7%, P < 0.001), and cerebrovascular disease (12.6% vs 16.3%, P < 0.001). The non-survival group had a higher need for invasive ventilation (55.1% vs 74.6%, P < 0.001) and renal treatment (19.9% vs 25.3%, P < 0.001). Patients were categorized into four groups based on their lymphocyte count during the first twenty-four hours of admission, using quartile for classification (Q1: 0.05–0.81; Q2: 0.81–1.3; Q3: 1.3–2; Q4: 2–8). As shown in Table 2, the third quartile (Q3) group exhibited the highest survival rate (87.6%, P < 0.001). Furthermore, the incidence rate of myocardial infarction was not statistically significant across different groups. A similar pattern was observed in patients with septic shock (TableS1).
Lymphocyte counts and hospital mortality risk
A univariable Cox regression analysis was conducted to identify variables influencing hospital mortality. As shown in Table 3, WBC, neutrophils, monocytes, gender, age, albumin, creatinine, potassium, temperature, respiratory rate, and the first-day sofa score were significantly associated with hospital mortality. Conversely, ALT, AST, heart rate, blood pressure components, platelets, glucose, and sodium were found to have limited clinical significance,with hazard ratios close to 1. We conducted a correlation analysis to address potential collinearity among the remaining continuous variables. Figure 2A demonstrates strong correlations among WBC, neutrophils, and monocytes. Based on these findings, WBC was selected as the adjusted variable. A multivariable Cox regression analysis was then utilized to assess the independent prognostic significance of lymphocytes (Table 3). After adjusting for WBC, gender, age, albumin, creatinine, potassium, temperature, respiratory rate, and the first-day sofa score, the RCS model revealed a U-shaped relationship between lymphocytes and hospital mortality (Fig. 2B). The optimal lymphocyte level associated with the lowest in-hospital mortality was identified as 1.85 × 109/L, within the Q3 interval. Both lower and higher lymphocyte counts were significantly associated with increased hospital mortality rates. This pattern remained consistent in patients with and without septic shock (Fig. 3).
Survival outcomes and subgroup analyses
The Kaplan–Meier survival analysis curve was employed to illustrate the hospital mortality rates at 60 and 90 days, revealing significant differences across various groups. The second (Q2) and third (Q3) quartile groups demonstrated longer median survival time of 50.5 and 57.6 days, respectively, compared to the first quartile (Q1) group (P < 0.05). In contrast, the Q1 and fourth quartile (Q4) groups exhibit similar median survival times of 40.5 and 41 days, respectively, with no significant difference (P > 0.05) (Fig. 4A). This pattern remained consistent for 60-day hospital mortality (Fig. 4B) and septic patients (FigureS2). As shown in Fig. 5, the subgroup analysis further elucidated the relationship between lymphocyte counts and hospital mortality across various patient subgroups. A U-shaped relationship was observed in patients receiving invasive ventilation therapy and those with congestive heart failure, diabetes, or renal disease(Fig. 5A-D), indicating that low and high lymphocyte counts were associated with increased mortality in these groups. In contrast, no significant relationship between lymphocyte counts and hospital mortality was found in patients with cerebrovascular or chronic pulmonary disease (Fig. 5G-H). Patients with liver disease and undergoing renal replacement therapy exhibited a linear correlation between lymphocyte counts and hospital mortality (P for overall = 0.021, P for nonliner = 0.158, P for overall = 0.025, P for nonliner = 0.759) (Fig. 5E-F). Notably, significant interactions were observed in the third (Q3) quartile groups of patients with liver disease (P for interaction < 0.01) and undergoing renal replacement therapy (P for interaction < 0.01), suggesting the relationship between lymphocyte counts and mortality may differ in these specific patients (Fig. 6).
Kaplan–Meier survival analysis curves for all-cause mortality in sepsis patients. Footnote lymphocyte count quartiles: Q1 (0.05–0.81), Q2 (0.81–1.3), Q3 (1.3–2), Q4 (2–8). Kaplan–Meier curves showing cumulative probability of all-cause mortality according to groups at ninety days (a), and sixty days (b)
For patients with septic shock, a similar pattern was observed among those receiving invasive ventilation therapy and those with congestive heart failure or diabetes. However, no significant relationship was found between lymphocyte counts and hospital mortality in patients with cerebrovascular disease, chronic pulmonary disease, liver, or renal replacement therapy (Figure S3-4).
Discussion
Sepsis is a life-threatening condition that triggers systemic organ dysfunction and an exaggerated immune response to infection, leading to metabolic disturbances and severe immunosuppression [20]. Lymphocytes, crucial for adaptive and innate immune systems, are essential for an effective defense against sepsis [21]. Studies by Cillion's [22] and Ceccato's [23] have demonstrated that lymphocytopenia can independently predict ICU mortality. The underlying pathophysiological mechanism may involve early-stage impairment of B lymphocytes during sepsis onset, resulting in decreased IgM levels of natural antibodies against bacterial infection [24]. Furthermore, T lymphocytes, when continuously exposed to antigens, upregulate the expression of checkpoint inhibitors like CTLA-4, PD-1, LAG-3, and TIM-3, which weakens the host's capacity to mount a robust cellular immune response to subsequent infections [25, 26]. Clinical observational studies have shown a strong correlation between sepsis-induced lymphopenia and poor prognosis [27,28,29]. Persistent lymphopenia on the fourth day after sepsis diagnosis has emerged as a reliable biomarker for predicting 28-day and 1-year survival [30]. Lower lymphocyte counts and sustained lymphopenia are associated with elevated risks of ICU-acquired infections and 28-day mortality [31]. Our findings reveal a U-shaped relationship between lymphocyte count and hospital mortality risk in sepsis patients. The potential mechanisms behind this relationship may involve a delicate balance between the protective and harmful effects of lymphocytes in sepsis. Low lymphocyte counts likely signify impaired immune function and an inability to effectively respond to infections, while high counts could suggest uncontrolled inflammation causing organ damage [32, 33]. While lymphocytopenia has been considered a predictor of poor outcomes in sepsis, our study suggests that lymphocytosis also warrants equal attention. Recognizing both extremes in lymphocyte counts as indicators of poor prognosis represents a significant advancement in the field, pointing toward a more balanced approach to evaluating immune status beyond the simplistic association of low lymphocyte counts with higher mortality risk. The subgroup analyses reveal a linear association between higher lymphocyte counts and improved prognosis in sepsis patients with liver disease or requiring renal replacement therapy, highlighting the importance of robust cell-mediated immunity for survival in these cohorts [34]. In contrast, no significant association was found between lymphocyte counts and outcomes in patients with chronic pulmonary disease or cerebrovascular disease, suggesting disease-specific differences in the prognostic value of lymphopenia that merit further investigation.
Importantly, our study also explored the relationship between lymphocyte counts and outcomes in septic shock patients. Subgroup analysis revealed that septic shock patients exhibited similar patterns to those observed in the overall sepsis cohort. Specifically, we found a U-shaped association between lymphocyte counts and hospital mortality in septic shock patients with congestive heart failure, diabetes, renal disease, and receiving invasive ventilation therapy (Figure S3-4). This finding suggests that the complex interplay between lymphocyte levels and mortality risk persists even in the more severe septic shock. However, it's noteworthy that no significant relationship was found between lymphocyte counts and hospital mortality in septic shock patients undergoing renal replacement therapy. This divergence from the overall sepsis cohort could indicate that in septic shock, the impact of extreme organ dysfunction might outweigh the prognostic value of lymphocyte counts in specific subgroups. Alternatively, It may suggest that the immune dysregulation in septic shock is more complex than in sepsis conditions.
Our study underscores the role of lymphocytes as a potent biomarker for risk stratification and prognosis in sepsis and septic shock. The complex interplay between alterations in lymphocyte distribution, functionality, and inflammatory response underlines the need for personalized management approaches tailored to specific sepsis phenotypes. These findings have significant clinical implications, indicating that regular monitoring of lymphocyte counts could be a crucial aspect of sepsis management. Such monitoring can inform therapeutic decisions and enhance patient risk assessment, potentially improving outcomes.
This study's retrospective design and reliance on observational databases inherently introduce potential confounding factors. While our findings underscore the significance of lymphocytes in influencing mortality rates in sepsis patients, these results should be interpreted with caution and verified through prospective trials that meticulously control pertinent clinical variables. Our analysis is constrained by the limitations inherent in the MIMIC-IV 2.0 and eICU-CRD 2.0 databases. Notably, the inadequate documentation of specific critical data, such as inflammatory biomarkers and the dynamic changes in lymphocyte counts over time, precludes their comprehensive analysis. It is essential to acknowledge that, given the observational nature of our study, the association identified between lymphocyte counts and mortality does not imply causation. Future research is needed through prospective studies or randomized controlled trials to elucidate this relationship. Subsequent research should evaluate the implications of sustained lymphopenia during the ICU rather than focusing solely on initial lymphocyte counts. This approach could provide a more comprehensive understanding of the dynamic role of lymphocytes in sepsis progression and outcomes.
Conclusion
Our findings demonstrate a U-shaped association between lymphocyte counts and hospital mortality risk in sepsis patients, with the lowest risk observed at moderately elevated levels around 1.85 × 109/L. Both lymphocyte deficiency and extreme lymphocytosis are associated with a poorer prognosis, underscoring the delicate balance between impaired immunity and hyperinflammation in influencing outcomes. This finding suggests that an optimal range of lymphocyte counts may be crucial for better patient outcomes.
Availability of data and materials
All the data available in our articles has been saved in the MIMIC-IV 2.0 (https://mimic.mit.edu/) and eICU-CRD 2.0 (https://eicu-crd.mit.edu/) database, which is freely accessible for analysis and downloading. Access to the MIMIC-IV 2.0 and eICU-CRD 2.0 databases required passing a qualifying test and obtaining approval (certification number: 55849941).The associated code and the extracted data will be available from the corresponding author on reasonable request.
Data availability
No datasets were generated or analysed during the current study.
References
Denstaedt SJ, Singer BH, Standiford TJ. Sepsis and nosocomial infection: patient characteristics, mechanisms, and modulation. Front Immunol. 2018;9:2446.
Gameiro J, Fonseca JA, Jorge S, Gouveia J, Lopes JA. Neutrophil, lymphocyte and platelet ratio as a predictor of mortality in septic-acute kidney injury patients. Nefrologia (Engl Ed). 2020;40(4):461–8.
Hajj J, Blaine N, Salavaci J, Jacoby D. The, “centrality of sepsis”: a review on incidence, mortality, and cost of care. Healthcare (Basel). 2018;6(3):90.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801–10.
de Pablo R, Monserrat J, Prieto A, Alvarez-Mon M. Role of circulating lymphocytes in patients with sepsis. Biomed Res Int. 2014;2014:671870.
Girardot T, Rimmelé T, Venet F, Monneret G. Apoptosis-induced lymphopenia in sepsis and other severe injuries. Apoptosis. 2017;22(2):295–305.
Jiang W, Zhong W, Deng Y, Chen C, Wang Q, Zhou M, Li X, Sun C, Zeng H. Evaluation of a combination “lymphocyte apoptosis model” to predict survival of sepsis patients in an intensive care unit. BMC Anesthesiol. 2018;18(1):89.
Bantel H, Schulze-Osthoff K. Cell death in sepsis: a matter of how, when, and where. Crit Care. 2009;13(4):173.
Liu D, Huang SY, Sun JH, Zhang HC, Cai QL, Gao C, Li L, Cao J, Xu F, Zhou Y, et al. Sepsis-induced immunosuppression: mechanisms, diagnosis and current treatment options. Mil Med Res. 2022;9(1):56.
Cao C, Yu M, Chai Y. Pathological alteration and therapeutic implications of sepsis-induced immune cell apoptosis. Cell Death Dis. 2019;10(10):782.
Finfer S, Venkatesh B, Hotchkiss RS, Sasson SC. Lymphopenia in sepsis-an acquired immunodeficiency. Immunol Cell Biol. 2022;101(6):35–544.
Liu B, Du H, Zhang J, Jiang J, Zhang X, He F, Niu B. Developing a new sepsis screening tool based on lymphocyte count, international normalized ratio and procalcitonin (LIP score). Sci Rep. 2022;12(1):20002.
Dizen Kazan E, Orhan S, Korkmaz D, Sari A, Kazan S. The effect of lymphocyte blood levels on mortality of COVID-19 patients under intensive care unit follow-up. Eur Rev Med Pharmacol Sci. 2022;26(19):7290–6.
Shi Y, Yang C, Chen L, Cheng M, Xie W. Predictive value of neutrophil-to-lymphocyte and platelet ratio in in-hospital mortality in septic patients. Heliyon. 2022;8(11): e11498.
Russell CD, Parajuli A, Gale HJ, Bulteel NS, Schuetz P, de Jager CPC, Loonen AJM, Merekoulias GI, Baillie JK. The utility of peripheral blood leucocyte ratios as biomarkers in infectious diseases: A systematic review and meta-analysis. J Infect. 2019;78(5):339–48.
Huang Z, Fu Z, Huang W, Huang K. Prognostic value of neutrophil-to-lymphocyte ratio in sepsis: A meta-analysis. Am J Emerg Med. 2020;38(3):641–7.
Martinez-Camacho A, Khaoustov V, Adam E, Lewis D, Tavakoli-Tabasi S, Yoffe B. Lymphocytosis as a predictor of poor response to treatment of hepatitis C. Clin Res Hepatol Gastroenterol. 2011;35(1):34–40.
Johnson AEW, Bulgarelli L, Shen L, Gayles A, Shammout A, Horng S, Pollard TJ, Hao S, Moody B, Gow B, et al. MIMIC-IV, a freely accessible electronic health record dataset. Sci Data. 2023;10(1):1.
Pollard TJ, Johnson AEW, Raffa JD, Celi LA, Mark RG, Badawi O. The eICU Collaborative research database, a freely available multi-center database for critical care research. Sci Data. 2018;5: 180178.
Venet F, Monneret G. Advances in the understanding and treatment of sepsis-induced immunosuppression. Nat Rev Nephrol. 2018;14(2):121–37.
Hsieh YC, Athar M, Chaudry IH. When apoptosis meets autophagy: deciding cell fate after trauma and sepsis. Trends Mol Med. 2009;15(3):129–38.
Cilloniz C, Peroni HJ, Gabarrús A, García-Vidal C, Pericàs JM, Bermejo-Martin J, Torres A. Lymphopenia is associated with poor outcomes of patients with community-acquired pneumonia and sepsis. Open Forum Infect Dis. 2021;8(6):ofab169.
Ceccato A, Panagiotarakou M, Ranzani OT, Martin-Fernandez M, Almansa-Mora R, Gabarrus A, Bueno L, Cilloniz C, Liapikou A, Ferrer M, et al. Lymphocytopenia as a predictor of mortality in patients with ICU-acquired pneumonia. J Clin Med. 2019;8(6):843.
Rauch PJ, Chudnovskiy A, Robbins CS, Weber GF, Etzrodt M, Hilgendorf I, Tiglao E, Figueiredo JL, Iwamoto Y, Theurl I, et al. Innate response activator B cells protect against microbial sepsis. Science. 2012;335(6068):597–601.
Hotchkiss RS, Colston E, Yende S, Angus DC, Moldawer LL, Crouser ED, Martin GS, Coopersmith CM, Brakenridge S, Mayr FB, et al. Immune checkpoint inhibition in sepsis: a phase 1b randomized, placebo-controlled, single ascending dose study of antiprogrammed cell death-ligand 1 antibody (BMS-936559). Crit Care Med. 2019;47(5):632–42.
McBride MA, Patil TK, Bohannon JK, Hernandez A, Sherwood ER, Patil NK. Immune Checkpoints: Novel Therapeutic Targets to Attenuate Sepsis-Induced Immunosuppression. Front Immunol. 2020;11: 624272.
Vahedi HSM, Bagheri A, Jahanshir A, Seyedhosseini J, Vahidi E. Association of lymphopenia with short term outcomes of sepsis patients; a brief report. Arch Acad Emerg Med. 2019;7(1):e14.
Grondman I, de Nooijer AH, Antonakos N, Janssen NAF, Mouktaroudi M, Leventogiannis K, Medici M, Smit JWA, van Herwaarden AE, Joosten LAB, et al. The Association of TSH and Thyroid Hormones With Lymphopenia in Bacterial Sepsis and COVID-19. J Clin Endocrinol Metab. 2021;106(7):1994–2009.
Jensen IJ, Sjaastad FV, Griffith TS, Badovinac VP. Sepsis-induced T cell immunoparalysis: the ins and outs of impaired T cell immunity. J Immunol. 2018;200(5):1543–53.
Drewry AM, Samra N, Skrupky LP, Fuller BM, Compton SM, Hotchkiss RS. Persistent lymphopenia after diagnosis of sepsis predicts mortality. Shock. 2014;42(5):383–91.
Adrie C, Lugosi M, Sonneville R, Souweine B, Ruckly S, Cartier JC, Garrouste-Orgeas M, Schwebel C, Timsit JF. Persistent lymphopenia is a risk factor for ICU-acquired infections and for death in ICU patients with sustained hypotension at admission. Ann Intensive Care. 2017;7(1):30.
Buonacera A, Stancanelli B, Colaci M, Malatino L. Neutrophil to lymphocyte ratio: an emerging marker of the relationships between the immune system and diseases. Int J Mol Sci. 2022;23(7):3636.
Aygun U, Yagin FH, Yagin B, Yasar S, Colak C, Ozkan AS, Ardigò LP. Assessment of Sepsis Risk at Admission to the Emergency Department: Clinical Interpretable Prediction Model. Diagnostics (Basel). 2024;14(5):457.
Li G, Li B, Song B, Liu D, Sun Y, Ju H, Xu X, Mao J, Zhou F. Uplift modeling to predict individual treatment effects of renal replacement therapy in sepsis-associated acute kidney injury patients. Sci Rep. 2023;14(1):5833.
Acknowledgements
We express our sincere gratitude to all the participants from the Emergency Medicine Clinical Research Center at Beijing Chao-Yang Hospital, Capital Medical University, for their invaluable contributions to this study.
Funding
High-Level Public Health Technical Talent Building Program (Discipline Leader-01–01).
Author information
Authors and Affiliations
Contributions
GZ was instrumental in collecting and analyzing data, as well as drafting the manuscript. TW, LA, FS, and CCH were pivotal in data extraction and played a significant role in the study's design. XSW and RS dedicated their efforts to conducting literature research. ZT, who oversaw the entire project, contributed by reviewing and designing the study, in addition to providing supervision. All authors actively participated in the development of the article and gave their approval for the final version to be submitted.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in strict compliance with the ethical principles outlined in the 1964 Declaration of Helsinki and its subsequent updates, or equivalent ethical standards. In line with local laws and institutional guidelines, ethical review and approval for research involving human participants were deemed not necessary. Similarly, the requirement for written informed consent from participants was waived under national regulations and institutional policies.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
12245_2024_682_MOESM2_ESM.tif
Supplementary Material 2: Figure S2 Kaplan–Meier survival analysis curves for all-cause mortality in septic shock patients. Footnote lymphocyte count quartiles: Q1 (0.05–0.81), Q2 (0.81–1.3), Q3 (1.3–2), Q4 (2–8). Kaplan–Meier curves showing cumulative probability of all-cause mortality according to groups at ninety days (a), and sixty days (b)
12245_2024_682_MOESM3_ESM.tif
Supplementary Material 3: Figure S3 Restricted cubic spline curve for different subgroups among septic shock patients (A) Invasive ventilation therapy (B) Congestive heart failure (C) Diabetes (D) Renal disease (E) Liver disease (F) Renal replacement therapy (G) Cerebral disease (H) Chronic pulmonary disease.
12245_2024_682_MOESM4_ESM.tiff
Supplementary Material 4: Figure S4 Forest plot for the primary outcome in different subgroup among patients with septic shock. HR, hazard ratio; CI, confidence interval
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, G., Wang, T., An, L. et al. U-shaped correlation of lymphocyte count with all-cause hospital mortality in sepsis and septic shock patients: a MIMIC-IV and eICU-CRD database study. Int J Emerg Med 17, 101 (2024). https://doi.org/10.1186/s12245-024-00682-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12245-024-00682-6