Abstract
The purpose of the work on normotensive rats of different age groups (3, 15, and 22 months) is to study the synchronism between the functioning of the cardiovascular system and the locomotor activity of animals in open field tests by a single injection of exogenous melatonin in different doses (1 and 10 mg/kg). The studies show a unidirectional dose-dependent effect of exogenous melatonin on the locomotor activity of rats of different ages and an age-dependent effect of melatonin on the parameters of the cardiovascular system. The results show the possible desynchronization between the circadian rhythms of locomotor activity and the functioning of the cardiovascular system with aging, which can lead to a discrepancy between hemodynamic parameters and the level of locomotor activity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
It is known that the functions of organisms are subject to daily and seasonal dynamics. The suprachiasmatic nucleus (SCN) of the hypothalamus is the main pacemaker crucial for circadian rhythms in physiology and behavior; SCN has nerve connections with the pineal gland, or epiphysis, and other parts of the brain. Daily alteration of light and dark is the strongest signal for synchronizing the biological clock. This alteration regulates melatonin secretion by the pineal gland and synchronizes the functions of the whole body through SCN by means of transcriptional/translational feedback consisting of the clock genes and their protein products [1, 2, 6, 36]. In addition, each organ has its own biological clock system. To illustrate, the rhythmic expression of clock genes in the heart, aorta, as well as in the endothelium and smooth muscles of blood vessels, has been shown [6].
Circadian and circannual cycles are linked to changes of the melatonin level in the body. Melatonin is a hormone that is produced by the pineal gland during the dark phase of the day [10]. After biosynthesis, the pineal melatonin is released into the circulatory system and reaches all biological fluids, including the cerebrospinal fluid, bile, saliva, synovial fluid, sperm, follicular fluid, amniotic fluid, breast milk, and tears. Melatonin is also produced extrapineally by the skin, retina, thymus, spleen, heart, muscles, liver, stomach, pancreas, intestine, placenta, testicles, ovary, bone marrow, brain cortex, and striatum [8, 29]. Endogenous melatonin triggers numerous physiological reactions, including synchronization of circadian rhythms, sleep-wake cycle regulation, antioxidant capacity, and modulation of the immune and cardiovascular systems. Melatonin implements its effects via the MT1 and MT2 G-protein-coupled membrane receptors. MT receptors binding melatonin have been found in various parts of the CNS: the brain cortex, hippocampus, thalamus, epiphysis, pituitary gland, midbrain, cerebellum, and SCN [2, 37]. In addition to the brain and retina, MT1 and MT2 have been found in almost all organ systems, including the cardiovascular system. MT1 and MT2 receptors have been detected in the heart ventricles, aorta, and arteries [18, 19, 40].
MT1 and MT2 receptors differ in molecular structure. MT1 receptors are mainly coupled to Gαi and Gαq proteins, whereas MT2 receptors are mainly Gαi-protein coupled. Stimulation of Gαi proteins reduces cellular cAMP levels and upregulates potassium channels [40]. Gαq stimulation activates phospholipase C, triggers the production of diacylglycerol and inositol-3-phosphate, and also increases the level of intracellular Ca2+ [40]. Melatonin has a higher affinity to MT1 receptors than MT2 [19, 34]. Probably, sequential activation of Gαi and Gαq subunits by melatonin can phase shift the circadian cycle [10]. Gαq-stimulated melatoninergic receptors in the cardiovascular system cause vasoconstriction and Gαi-protein-mediated stimulation results in vasodilation [40]. Melatonin enhanced the vasoconstrictor effect of noradrenaline and vasopressin in vitro in a fragment of the caudal artery from an adult rat in [32, 48]; the vasodilatory effect of melatonin was demonstrated in experiments using fragments of the aorta and the mesenteric artery in [51, 55]. The vascular effects of melatonin largely depend on the density of MT1 and MT2 receptors in the vessels. The effect of melatonin on hemodynamic parameters involves the activation of MT receptors located in the cardiovascular system, as well as modulation of the tone of the autonomic nervous system [40], which ultimately synchronizes the cardiovascular system, other body systems, and behavioral activity.
Experimental studies have revealed an age-related change in the expression of MT1 and MT2 receptors both in peripheral tissues [46] and in the central nervous system [28, 52], including due to a decline in endogenous melatonin levels [28, 31]. Certainly, the effect of exogenous melatonin on hemodynamic parameters and behavior will depend on its dose as well as the age of the subject.
The aim of this work was to study the effect of single injection of exogenous melatonin in different doses (1 and 10 mg/kg) on hemodynamic parameters, components of the heart rate variability, and the behavior of animals in open field tests using normotensive rats of different age groups (3, 15, and 22 months). Conclusions about synchronicity between the cardiovascular system and locomotion of animals from different age groups are made.
MATERIALS AND METHODS
The experiments were performed using conventional male Wistar rats aged 3, 15, and 22 months (farm Rappolovo). The animals were divided into three groups (1—aged 3 months; 2—aged 15 months; 3—aged 22 months); each group included 24 animals. The rats were kept under natural light at a temperature of 20°C and were given ad libitum access to food and water.
All experiments were performed from 10 a.m. to 3 p.m. (the length of daylight was 11–13 h), when the level of endogenous melatonin is minimal. The effects of single administration of exogenous melatonin at different doses on hemodynamic parameters and components of the heart rate variability (HRV), as well as on the behavior of rats in the open field test were studied in young and mature aged rats.
Melatonin (Purtan’s Pride, United States) was used in the experiments. Each group of rats was divided into three subgroups: control and two experimental ones, with eight animals in each subgroup. A solution of melatonin in physiologic saline (1 and 10 mg/kg, 3 mL) was injected into the rats of the experimental subgroups by intraperitoneal route. The animals of the control subgroups were injected intraperitoneally with physiologic saline at a volume of 3 mL. 30 min after administration of the solutions, an open field test was performed and hemodynamic parameters were then assessed.
The influence of exogenous melatonin on the behavior of rats was investigated by the open field test [24]. The open-field arena was a square open white plastic arena (76 cm width and 27 cm wall height) divided into sectors of 19-cm squares; the arena had round holes sized 2 cm in diameter at the corners of the squares. The rat behavior in the open field test was monitored using a camera (car video recorder) installed in such a way as to completely observe the arena. The arena was located on the floor of the manipulation area of the vivarium with the same microclimate (temperature, humidity) as in the area for keeping and raising animals. The illumination in the manipulation area was 487 lux (artificial light).
During the test, a rat was placed in the center of the arena and their behavior was monitored for 5 min. The following indicators were assessed: the latent period in seconds (from placement of the animal onto the arena to onset of locomotor activity), horizontal motion (the number of square sectors crossed), vertical motion (the number of times when front paws were elevated and rat was in an upright posture), the number of crossings through the center in the open field, the number of explored holes, urination (the number of acts), defecation (the number of fecal boluses), and grooming acts. We also calculated the total locomotor activity as the sum of grooming acts and horizontal and vertical activities. After testing each animal for removing organic marks, the arena was wiped with napkins impregnated with a weak solution of hydrogen peroxide.
The hemodynamic parameters were measured in awake restrained rats using the Chart software with a non-invasive blood pressure measurement system (ADInstruments, Australia) equipped with the ML125 NIBP controller, the MLT125R pulse rate sensor, and a tail cuff sensor for rats. The sampling frequency was 100 Hz, FFT was 1024. This system allows recording systolic blood pressure (SBP) and the inter-systolic interval (ISI) on the rat’s tail. A total of 5–6 tests were performed to measure the parameters and the arithmetic mean was then calculated.
The hemodynamic parameters were measured simultaneously with an analysis of the HRV spectrum using the Chart software. Short segments of recorded pulses with duration of 40 s were analyzed. The low frequency component of the heart rate variability spectrum (LF: 0.15–0.8 Hz) used as a reflection of the sympathetic activity and the high frequency component of the HRV spectrum (HF: 0.8–2.5 Hz) describing the parasympathetic activity were estimated in ms2/Hz using mathematical methods adopted by the North American Society of Pacing and Electrophysiology [7]. The LF/HF ratio indicated the sympathovagal balance in the regulation of heart function and the sum LF + HF reflected total HRV.
The data were analyzed statistically using the Statistica 6.0 software. Data were analyzed by nonparametric statistics due to small sample sizes. Two independent subgroups were compared using the U-Mann–Whitney test. Differences in data at p < 0.05 were significant. The measurement results are presented as median and interquartile range (25th and 75th percentiles). The expression of the effect of melatonin on the studied parameters was also estimated in percentage. Parameter medians for each subgroup were used for statistics; the median of the control subgroup was taken as 100%.
RESULTS AND DISCUSSION
In the control subgroups of rats of different ages, there were no significant differences in the hemodynamic parameters and the HRV spectrum components, or on the behavior in the open field test, except for a significant decrease in vertical upright postures made by 22-month-old rats compared to 3-month-old rats (p = 0.04); this may have occurred due to age-related changes in the musculoskeletal system of the animals.
It was shown that blood pressure (BP) decreased in rats with prolonged administration of melatonin at a dose of 10 mg/kg [26, 39]. Meanwhile, a single intravenous administration of melatonin at a dose of 5 and 15 mg/kg did not cause significant changes in BP and heart rate (HR) in rats [15]. In this work, a single intraperitoneal injection of melatonin at a dose of 1 mg/kg did not cause significant changes in the hemodynamic parameters and HRV components in 15- and 22-month-old normotensive awake rats; only 3-month-old rats showed a trend of SBP increase (p = 0.2 compared to the control subgroup) and an increase in the total degree of HRV (p = 0.03 compared to the control subgroup) (Table 1). At the same time, a single dose of melatonin (10 mg/kg) led to an increase in SBP in 15‑month-old rats (p = 0.006 compared to the control subgroup). In 22-month-old rats, administration of melatonin at a dose of 10 mg/kg caused slight tachycardia (p = 0.15, compared to the control subgroup) and changed the HRV components versus the control subgroup: inhibition of LF (p = 0.02), a tendency of HF inhibition (p = 0.09), and a decrease in LF + HF (p = 0.03) (Table 1). The different effects of melatonin on cardiovascular function in young and aged rats may be associated with alteration of MT1- and MT2-receptor expression in the heart and blood vessels during aging. Thus, Sanchez-Hidalgo et al. in experiments [46] showed that the quantity of MT1 and MT2 receptors in the heart and other peripheral tissues significantly decreased in normotensive rats by the age of 12 months compared to 3-month-old animals. In experiments in vitro, melatonin caused a stronger vasoconstrictor response when exposed to segments of the distal caudal artery from adolescent rats than from adult animals [20].
Laudon et al. revealed that the density of MT receptors decreased significantly in different parts of the brain in old rats [31]. However, the results of studies using mice indicate that the reduced expression of MT receptors in the central nervous system has an insignificant effect on the melatonin-induced phase shifts of circadian rhythms and sensitivity to melatonin does not decrease with age [12]. In this paper, in the open field test, the locomotor activity in rats of all age groups increased after a single administration of melatonin at a dose of 1 mg/kg (Table 2). The effect was maximal in young animals. In 3-month-old rats after administration of melatonin at a dose of 1 mg/kg, the most frequent locomotion acts were increase in motion activity (both vertical and horizontal motion) and increase in the number of explored holes and grooming acts. In 15-month-old animals, melatonin at a dose of 1 mg/kg caused a significant reduction in the latent period and increased the number of grooming acts (Table 2). In 22-month-old rats there was an increase in horizontal activity after administration of melatonin at a dose of 1 mg/kg. Melatonin at a dose of 10 mg/kg had no effect on the behavior of rats in the open field test (Table 2).
A growth of locomotor activity after administration of low melatonin doses was shown by other researchers. An increased locomotor activity was observed in experiments using mice after administration of melatonin at a dose of 1.2 mg/kg [27]. Beier et al. in experiments [4] showed that melatonin administered intraperitoneally at a dose of 0.1 mg/kg to rats increased horizontal and vertical motion as well as the number of grooming acts. In contrast, administration of melatonin at a dose of 60 mg/kg decreased mobility of rats [16], and melatonin at a dose of 10 mg/kg had no significant effect on animal behavior [3]. The fact of an increase in locomotor activity of animals after administration of low melatonin doses and the opposite effect (or lack of effect) after administration of high melatonin doses confirms the dose-dependent effect of melatonin induced through the activation of different protein subunits in the MT receptors. This dose-dependent effect of melatonin is probably phase-shifting circadian rhythms. Experiments on mice with a deletion of MT1 and MT2 receptors have shown that the lack of MT receptors has no significant effect on the diurnal locomotor activity of animals, but reduces the accuracy of diurnal locomotor rhythms compared to mice with an intact melatoninergic system [41].
Under natural conditions, daily melatonin levels peak at night and seasonal ones peak in winter [9, 10, 43]. In people, the daily minimum BP is observed at night [17, 22] and the seasonal minimal BP occurs in summer [44]. This fact casts doubt on the presence of a significant hypotensive effect of endogenous melatonin. Circadian dynamics similar to BP dynamics have also been shown for HR [22]. In addition, daily changes in HRV components are established [13, 30]. People have the maximum power of the HRV spectrum and the minimum value of LF/HF during the night; during the day, the minimum power of the HRV spectrum and the maximum value of LF/HF are observed. Studies involving healthy volunteers have shown that exogenous melatonin enhances vagal tone and exerts a suppressive effect on sympathetic innervation of the heart [38]. In contrast to humans, rats are animals with nocturnal activity, and they are characterized by the reverse circadian profile of the SBP, HR, and HRV spectrum components [25, 49]. Meanwhile, the daily melatonin profile in all mammals, regardless of their lifestyle, shows a maximum at night, but studies have shown that the clearance of melatonin in rats is higher than in humans [53].
It is known that the level of endogenous melatonin decreases with age [1, 5, 52]. Studies involving men have shown that the concentration of melatonin in urine peaks at 19–29 years; it reaches minimum values at 40–49 years and rises again slightly after 60 years [5]. In addition, the density of MT1 and MT2 receptors declines with aging [12, 28, 31, 46], and photoreception, the structure of the pineal gland, and innervation between SCN and the pineal gland are disturbed [1, 14]. Furthermore, experiments using male Wistar rats have shown that in 12- and 24-month-old animals, the expression of clock genes (Per1, Per2, Cry1, Cry2, and Bmal1) in SCN changes significantly compared to 3-month-old animals, with abolition of daily rhythms of Cry1, Cry2, and Bmal1 in 24-month-old rats [36]. This phenomenon is associated with age-related telomerase shortening and a decrease in the activity of proteins binding cAMP-sensitive elements [6]. All this changes circadian rhythms. Studies involving humans as subjects have shown an age-related decrease in the amplitude of circadian oscillations of BP and HR and shifting in the acrophase of the circadian cycle [11, 14, 50].
In experiments [47, 54], a strong relationship between the locomotor activity of rats during the day and hemodynamic parameters has been revealed; i.e., higher values of BP and HR corresponded to an increased locomotor activity than the rest state. This ratio may change with age. Thus, in experiments with normotensive rats, 23–24-month-old animals were observed to have higher BP levels and lower motor activity at night compared to 3-month-old rats [47]. The unidirectional dose-dependent effect of exogenous melatonin on locomotion of rats of different ages and the age-dependent effect of melatonin on the functioning of the cardiovascular system found in our study indicate the possible age-related desynchronization between the circadian rhythms of the locomotor activity and the functioning of the cardiovascular system, which can lead to discrepancies between hemodynamic parameters and the level of locomotor activity.
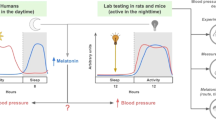
Therefore, in our experiments after administration of melatonin at a dose of 1 mg/kg, the increase in locomotor activity was accompanied by a tendency of SBP increase only in 3-month-old rats (Tables 1 and 2; Fig. 1). In 15-month-old rats, the maximum level of SBP was recorded after administration of melatonin at a dose of 10 mg/kg, while locomotor activity was not significantly increased (Tables 1 and 2, Fig. 1). In 22-month-old rats, administration of melatonin at a dose of 10 mg/kg was associated with a tendency of tachycardia, while locomotor activity did not differ from the activity of animals in the control subgroup (Tables 1 and 2, Fig. 1). HRV increase after melatonin administration observed in 3-month-old rats alternated to HRV decrease in 22-month-old animals (Table 1, Fig. 1).
The relative parameters of hemodynamics, heart rate variability, and total locomotor activity in rats of different ages after melatonin injection. ISI—the inter-systolic interval; LF + HF–the total power of the heart rate variability spectrum; TLA—total locomotor activity. * p < 0.05—difference significance compared to control subgroup.
The discrepancy between functioning of the cardiovascular system and the level of locomotor activity after administration of melatonin in old groups may be due to the fact that the expression of MT receptors changes to a greater extent during aging in the cardiovascular system than in the CNS possibly due to the stronger decrease in the level of endogenous melatonin in peripheral tissues than in the brain. Desynchronization in the functioning of the body systems can also occur as a result of age-related changes in the CNS [14, 36]. In addition, age-related remodeling in the heart and blood vessels (collagen deposition in the myocardium, changes in cardiac conduction system, atherosclerosis, arterial rigidity, and others) [33, 45], as well as age-related suppression of autonomic hemodynamic control mechanisms (e.g., baroreceptor reflex) [21, 42, 47], may also contribute to this desynchronization, ultimately reducing the adaptive capacities of the cardiovascular system. Indirect evidence for the reduction in the adaptive capacity of the cardiovascular system in this paper is the HRV decrease in 22-month-old rats after administration of melatonin. It is known that HRV indicates the ability of the heart to respond to numerous physiological and environmental stimuli such as breathing, physical activity, psychological stress, hemodynamic and metabolic changes, sleep and orthostasis, as well as disorders caused by diseases [42].
To date, the effect of exogenous melatonin on the correction of circadian dysfunction and age-related changes in cardiovascular function has been investigated in numerous studies. In experiments using mice, it was found that everyday 6-month therapy with melatonin at a dose 10 mg/kg started at 16 months of age attenuated the age-related reduction of MT-receptor expression [28]. In addition, melatonin restored circadian gene expression in SCN in 12- and 24-month-old rats [36]. Furthermore, numerous clinical and experimental studies have shown that long-term administration of melatonin provided cardioprotective and mild hypotensive benefits due to activation of membrane MT receptors, the antioxidant action of melatonin, and its ability to mediate accumulation of natural vasodilators in vessel walls, like nitrogen oxide [29, 40]. A meta-analysis of clinical trials has shown that prolonged-release melatonin was the most effective for correcting circadian rhythms of BP [23]. However, caution needs to be taken for the possible weak hypertensive effect of melatonin, which we observed, as well as several other authors [35].
CONCLUSIONS
The increase in locomotor activity of animals after administration of the low melatonin dose and the lack of effect after administration of the high melatonin dose confirms the dose-dependent effect of this substance mediated by upregulation of different protein subunits in MT receptors.
The unidirectional dose-dependent effect of exogenous melatonin on the locomotor activity of rats of different ages and the age-dependent effect of melatonin on the cardiovascular system indicate a possible age-related desynchronization between the circadian rhythms of locomotion and cardiovascular system activity. This can lead to a discrepancy between hemodynamic parameters and the level of locomotor activity.
REFERENCES
Anisimov, V.N., Epiphysis, biorhythms, and aging of an organism, Usp. Fiziol. Nauk, 2008, vol. 39, no. 4, pp. 40–65.
Arushanyan, E.B. and Popov, A.V., Modern concepts on the role of the suprachiasmatic nuclei of the hypothalamus in the organization of diurnal periodism of physiological functions, Usp. Fiziol. Nauk, 2011, vol. 42, no. 4, pp. 39–58.
Beier, E.V. and Skornyakov, A.A., Comparative assessment of psychotropic activity of melatonin on various behavioral models, Trudy X Mezhdunarodnogo kongressa “Zdorov’e i obrazovanie XXI veka” (Proc. X Int. Congr. “Health and Education in 21st Century”), Moscow, 2011, vol. 13, no. 7, p. 319.
Beier, E.V., Skornyakov, A.A., and Arushanyan, E.B., Effect of pineal gland removal on the psychotropic activity of adaptogenic agents in rats, Med. Vestn. Sev. Kavk., 2014, vol. 9, no. 3, pp. 254–258.
Kim, L.B., Putyatina, A.N., Russkikh, G.S., and Tsypysheva, O.B., Melatonin and the aging process in men in the European part of the Arctic zone of Russia, Adv. Gerontol., 2019, vol. 9, no. 1, pp. 67–74.
Kurbatova, I.V., Topchieva, L.V., and Nemov, N.N., Circadian genes and cardiovascular pathologies, Tr. Karel. Nauchn. Tsentra, Ross. Akad. Nauk, 2014, no. 5, pp. 3–17.
American Heart Association, Heart rate variability: standards of measurement, physiological interpretation, and clinical use, Circulation, 1996, vol. 93, no. 5, pp. 1043–1065.
Acuña-Castroviejo, D., Escames, G., Venegas, C., et al., Extra pineal melatonin: sources, regulation, and potential functions, Cell Mol. Life Sci., 2014, vol. 71, no. 16, pp. 2997–3025.
Adamsson, M., Laike, T., and Morita, T., Annual variation in daily light exposure and circadian change of melatonin and cortisol concentrations at a northern latitude with large seasonal differences in photoperiod length, J. Physiol. Anthropol., 2016, vol. 36, no. 1, p. 6. https://doi.org/10.1186/s40101-016-0103-9
Arendt, J., Melatonin and the pineal gland: influence on mammalian seasonal and circadian physiology, Rev. Reprod., 1998, vol. 3, pp. 13–22.
Atkinson, G., Witte, K., Nold, G., et al., Effects of age on circadian blood pressure and heart rate rhythms in patients with primary hypertension, Chronobiol. Int., 1994, vol. 11, no. 1, pp. 35–44.
Benloucif, S., Masana, M.I., and Dubocovich, M.L., Responsiveness to melatonin and its receptor expression in the aging circadian clock of mice, Am. J. Physiol., 1997, vol. 273, no. 6, pp. R1855– R1860.
Bilan, A., Witczak, A., Palusiński, R., et al., Circadian rhythm of spectral indices of heart rate variability in healthy subjects, J. Electrocardiol., 2005, vol. 38, no. 3, pp. 239–243.
Campos Costa, I., Nogueira Carvalho, H., and Fernandes, L., Aging, circadian rhythms and depressive disorders: a review, Am. J. Neurodegener. Dis., 2013, vol. 2, no. 4, pp. 228–246.
Cheung, R.T., Tipoe, G.L., Tam, S., et al., Preclinical evaluation of pharmacokinetics and safety of melatonin in propylene glycol for intravenous administration, J. Pineal Res., 2006, vol. 41, no. 4, pp. 337–343.
Chuang, J.I. and Lin, M.T., Pharmacological effects of melatonin treatment on both locomotor activity and brain serotonin release in rats, J. Pineal Res., 1994, vol. 17, no. 1, pp. 11–16.
Douma, L.G. and Gumz, M.L., Circadian clock-mediated regulation of blood pressure, Free Radical Biol. Med., 2018, vol. 119, pp. 108–114.
Dubocovich, M.L., Melatonin receptors: Are there multiple subtypes?, Trends Pharmacol. Sci., 1995, vol. 16, pp. 50–56.
Emet, M., Ozcan, H., Ozel, L., et al., A review of melatonin, its receptors and drugs, Eurasian J. Med., 2016, vol. 48, no. 2, pp. 135–141.
Evans, B.K., Mason, R., and Wilson, V.G., Evidence for direct vasoconstrictor activity of melatonin in “pressurized” segments of isolated caudal artery from juvenile rats, Naunyn-Schmiedeberg’s Arch. Pharmacol., 1992, vol. 346, no. 3, pp. 362–365.
Franchini, K., Moreira, E.D., Ida, F., and Krieger, E.M., Alterations in the cardiovascular control by the chemoreflex and the baroreflex in old rats, Am. J. Physiol.-Regul., Integr. Comp. Physiol., 1996, vol. 270, pp. R310–R313.
Gupta, A.K., Cornelissen, G., Greenway, F.L., et al., Abnormalities in circadian blood pressure variability and endothelial function: pragmatic markers for adverse cardiometabolic profiles in asymptomatic obeseadults, Cardiovasc. Diabetol., 2010, vol. 9, p. 58. https://doi.org/10.1186/1475-2840-9-58
Grossman, E., Laudon, M., and Zisapel, N., Effect of melatonin on nocturnal blood pressure: meta-analysis of randomized controlled trials, Vasc. Health Risk Manage., 2011, vol. 7, pp. 577–584.
Hall, C.S., Emotional behavior in the rat. III. The relationship between emotionality and ambulatory activity, J. Comp. Physiol. Psychol., 1936, vol. 22, pp. 345–352.
Hashimoto, M., Kuwahara, M., Tsubone, H., and Sugano, S., Diurnal variation of autonomic nervous activity in the rat: investigation by power spectral analysis of heart rate variability, J. Electrocardiol., 1999, vol. 32, no. 2, pp. 167–171.
Huang, L., Zhang, C., Hou, Y., et al., Blood pressure reducing effects of piromelatine and melatonin in spontaneously hypertensive rats, Eur. Rev. Med. Pharmacol. Sci., 2013, vol. 17, no. 18, pp. 2449–2456.
Hutchinson, A.J., Hudson, R.L., and Dubocovich, M.L., Genetic deletion of MT(1) and MT(2) melatonin receptors differentially abrogates the development and expression of methamphetamine-induced locomotor sensitization during the day and the night in C3H/HeN mice, J. Pineal Res., 2012, vol. 53, no. 4, pp. 399–409.
Jenwitheesuk, A., Boontem, P., Wongchitrat, P., et al., Melatonin regulates the aging mouse hippocampal homeostasis via the sirtuin1-FOXO1 pathway, EXCLI J., 2017, vol. 16, pp. 340–353.
Jiki, Z., Lecour, S., and Nduhirabandi, F., Cardiovascular benefits of dietary melatonin: a myth or a reality?, Front. Physiol., 2018, vol. 17, no. 9, p. 528. https://doi.org/10.3389/fphys.2018.00528
Korpelainen, J.T., Sotaniemi, K.A., Huikuri, H.V., and Myllylä, V.V., Circadian rhythm of heart rate variability is reversibly abolished in ischemic stroke, Stroke, 1997, vol. 28, no. 11, pp. 2150–2154.
Laudon, M., Nir, I., and Zisapel, N., Melatonin receptors in discrete brain areas of the male rat. Impact of aging on density and on circadian rhythmicity, Neuroendocrinology, 1988, vol. 48, no. 6, pp. 577–583.
Lew, M.J. and Flanders, S., Mechanisms of melatonin-induced vasoconstriction in the rat tail artery: a paradigm of weak vasoconstriction, Br. J. Pharmacol., 1999, vol. 126, no. 6, pp. 1408–1418.
Lindesay, G., Ragonnet, C., Chimenti, S., et al., Age and hypertension strongly induce aortic stiffening in rats at basal and matched blood pressure levels, Physiol. Rep., 2016, vol. 4, no. 10, p. e12805. https://doi.org/10.14814/phy2.12805
Liu, J., Clough, S.J., Hutchinson, A.J., et al., Mt1 and Mt2 melatonin receptors: a therapeutic perspective, Ann. Rev. Pharmacol. Toxicol., 2016, vol. 56, pp. 361–383.
Lusardi, P., Piazza, E., and Fogari, R., Cardiovascular effects of melatonin in hypertensive patients well controlled by nifedipine: a 24-hour study, Br. J. Clin. Pharmacol., 2000, vol. 49, pp. 423–427.
Mattam, U. and Jagota, A., Differential role of melatonin in restoration of age-induced alterations in daily rhythms of expression of various clock genes in suprachiasmatic nucleus of male Wistar rats, Biogerontology, 2014, vol. 15, no. 3, pp. 257–268.
Ng, K.Y., Leong, M.K., Liang, H., and Paxinos, G., Melatonin receptors: distribution in mammalian brain and their respective putative functions, Brain Struct. Funct., 2017, vol. 222, no. 7, pp. 2921–2939.
Nishiyama, K., Yasue, H., Moriyama, Y., et al., Acute effects of melatonin administration on cardiovascular autonomic regulation in healthy men, Am. Heart J., 2001, vol. 141, no. 5, p. E9. https://doi.org/10.1067/mhj.2001.114368
Pechanova, O., Zicha, J., Paulis, L., et al., The effect of N-acetyl cysteine and melatonin in adult spontaneously hypertensive rats with established hypertension, Eur. J. Pharmacol., 2007, vol. 561, nos. 1–3, pp. 129–136.
Pechanova, O., Paulis, L., and Simko, F., Peripheral and central effects of melatonin on blood pressure regulation, Int. J. Mol. Sci., 2014, vol. 15, no. 10, pp. 17920–17937.
Pfeffer, M., Korf, H.W., and Wicht, H., The role of the melatoninergic system in light-entrained behavior of mice, Int. J. Mol. Sci., 2017, vol. 18, no. 3, p. E530.
Rajendra, A.U., Paul, J.K., Kannathal, N., et al., Heart rate variability: a review, Med. Bio Eng. Comput., 2006, vol. 44, no. 12, pp. 1031–1051.
Romerowicz-Misielak, M., Oren, D.A., Sowa-Kucma, M., et al., Changes in melatonin synthesis parameters after carbon monoxide concentration increase in the cavernous sinus, J. Physiol. Pharmacol., 2015, vol. 66, no. 4, pp. 505–514.
Rosenthal, T., Seasonal variations in blood pressure, Am. J. Geriatr. Cardiol., 2004, vol. 13, no. 5, pp. 267–272.
Rossi, S., Fortunati, I., Carnevali, L., et al., The effect of aging on the specialized conducting system: a telemetry ECG study in rats over a 6month period, PLoS One, 2014, vol. 9, no. 11, p. e112697. https://doi.org/10.1371/journal.pone.0112697
Sánchez-Hidalgo, M., Guerrero Montavez, J.M., Carrascosa-Salmoral Mdel, P., et al., Decreased MT1 and MT2 melatonin receptor expression in extrapineal tissues of the rat during physiological aging, J. Pineal Res., 2009, vol. 46, no. 1, pp. 29–35.
Sei, H., Sano, A., Ohno, H., et al., Age-related changes in control of blood pressure and heart rate during sleep in the rat, Sleep, 2002, vol. 25, no. 3, pp. 279–285.
Vandeputte, C., Giummelly, P., Atkinson, J., et al., Melatonin potentiates NE-induced vasoconstriction without augmenting cytosolic calcium concentration, Am. J. Physiol. Heart Circ. Physiol., 2001, vol. 280, no. 1, pp. H420–H425.
Waki, H., Katahira, K., Polson, J.W., et al., Automation of analysis of cardiovascular autonomic function from chronic measurements of arterial pressure in conscious rats, Exp. Physiol., 2006, vol. 91, no. 1, pp. 201–213.
Watanabe, Y., Toyoshima, T., Otsuka, K., et al., Circadian profiles of blood pressure with respect to age, Nihon Ronen Igakkai Zasshi, 1994, vol. 31, no. 3, pp. 219–225.
Weekley, L.B., Melatonin-induced relaxation of rat aorta: interaction with adrenergic agonists, J. Pineal Res., 1991, vol. 11, no. 1, pp. 28–34.
Wu, Y.H. and Swaab, D.F., The human pineal gland and melatonin in aging and Alzheimer’s disease, Pineal Res., 2005, vol. 38, no. 3, pp. 145–152.
Yeleswaram, K., McLaughlin, L.G., Knipe, J.O., and Schabdach, D., Pharmacokinetics and oral bioavailability of exogenous melatonin in preclinical animal models and clinical implications, J. Pineal Res., 1997, vol. 22, no. 1, pp. 45–51.
Zaretsky, D.V., Zaretskaia, M.V., and DiMicco, J.A., Characterization of the relationship between spontaneous locomotor activity and cardiovascular parameters in conscious freely moving rats, Physiol. Behav., 2016, vol. 154, pp. 60–67.
Zhao, T., Zhang, H., Jin, C., et al., Melatonin mediates vasodilatation through both direct and indirect activation of BKC channels, J. Mol. Endocrinol., 2017, vol. 59, no. 3, pp. 219–233.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest. The authors delate that they have no conflict of interest.
Statement on the welfare of animals. The conditions of the research were in accordance with the ethical standards of the Almazov National Medical Research Centre (St. Petersburg), European Communities Council Directive 1986 (86/609/ EEC), and the rules stated in the Guide for the Care and Use of Laboratory Animals.
This study does not contain any studies involving human participants performed by any of the authors.
Additional information
Translated by M. Novikova
Rights and permissions
About this article
Cite this article
Pliss, M.G., Kuzmenko, N.V., Rubanova, N.S. et al. Dose-Dependent Mechanisms of Melatonin on the Functioning of the Cardiovascular System and on the Behavior of Normotensive Rats of Different Ages. Adv Gerontol 9, 327–335 (2019). https://doi.org/10.1134/S2079057019030111
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S2079057019030111