Abstract
Radiosensitivity to low and medium doses of X-ray radiation and the ability to induce a radiation adaptive response (RAR) of lymphocytes during in vitro irradiation of peripheral blood of patients with cancer were studied. The criterion for cytogenetic damage was the frequency of micronuclei (MN) in cytochalasin-blocked binucleate lymphocytes in culture. It was found that the spontaneous level of cytogenetic damage in the lymphocytes of patients was 2.6 times higher than in healthy volunteers, and there was also significant interindividual variability in values compared to the control cohort. There were no differences in mean values for radiosensitivity to low and medium doses of X-ray between the study groups. There was no correlation between the spontaneous level of MN in lymphocytes and the radiosensitivity of individuals in both groups. RAR was induced with the same frequency and to the same extent in lymphocytes from both patients and healthy individuals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In recent years, the clinical application of a number of specific non-target effects that were discovered in the studies of the effect of low doses of radiation on living objects has been actively studied [1]. The most interesting of them is the phenomenon of radiation adaptive response (RAR), which manifests itself in the fact that preliminary irradiation of biological objects with low doses of ionizing radiation increases the body’s resistance to subsequent exposure to high damaging doses of radiation or other genotoxic substances [2]. The ability to induce RAR was demonstrated at the organismal level in vivo in representatives of almost all taxonomic levels of the fauna and flora. Since the induction of RAR reduces damage by 40−75%, which is comparable or superior to the effectiveness of modern chemical protectors, many researchers consider RAR as an approach to increase the overall resistance of organisms not only to adverse environmental factors, but also to protect healthy tissues and organs during radiotherapy of cancer, diabetes mellitus, and modulation of inflammatory immune reactions in acute and chronic diseases of the musculoskeletal system and immunodeficiency states [3]. Previously, using SHK mice, we selected conditions for the induction of RAR, which was retained throughout the life of the animals and led to a decrease in the spontaneous level of cytogenetic damage associated with aging, which indicated epigenetic changes that led to an increased genome stability [4]. In this regard, research into the mechanisms and patterns of RAR induction in humans in vivo and in vitro is actively continued. A number of studies performed mainly on healthy donors showed a large individual variability in the recorded parameters and dependence on genetic and epigenetic factors [1]. There are quite few publications on the possibility of inducing RAR in patients depending on the diagnosis, because only the level of spontaneous damage or radiosensitivity of cells is usually studied. To date, it has been shown that increased levels of these indices are observed in cancer patients, residents of areas with increased background radiation, and employees of enterprises working with radioactive materials [5, 6]. In studies of individual human radiosensitivity, the number of micronuclei (MN) in cytochalasin-blocked binuclear lymphocytes (CBBLs) is commonly used as a biomarker of genomic instability. This is a sensitive, reproducible, and unified technique that makes it possible to rapidly assess the level of chromosomal damage, accumulate individual data over several years, and combine and compare results obtained in different laboratories [7].
The purpose of this work was to study the radiosensitivity and the ability to induce RAR in peripheral blood lymphocytes of patients with cancer as compared to healthy donors.
The study involved 31 patients (24 women and 7 men, average age 55 years) with cancer in remission: most women had breast and ovarian cancer, and men had prostate and thyroid cancer. The control group included 21 healthy volunteers (13 women and 8 men, average age 48 years). All participants had no bad habits (smoking or alcohol), adhered to a traditional diet and lifestyle, and were not subjected to X-ray or CT examinations for 1 month.
Blood samples (5 mL) were collected from volunteers in the morning on an empty stomach from the cubital vein into sterile vials with heparin (10 units/mL). The study was conducted in accordance with the principles of medical ethics set out in the “Ethical Principles for Medical Research Involving Human Subjects of the World Medical Association” (Declaration of Helsinki 2013) [8].
The radiosensitivity and RAR induction was studied using in vitro irradiation of whole human peripheral blood with X-ray radiation. The blood volume was aliquoted into 0.5-mL samples in duplicate for the following variants: (1) non-irradiated control; (2) irradiation at a dose of 10 cGy; (3) irradiation at a dose of 2 Gy; and (4) irradiation according to the RAR scheme (first at an adapting dose of 10 cGy and then after 5 h at a revealing dose of 2 Gy). The radiation doses were selected on the basis of the results of our previous studies of RAR induction in mice and lymphocytes from healthy donors [9]. Blood samples were transported (for ~1 h) and irradiation was performed at room temperature, since earlier, when determining cytogenetic damage in blood cells, we showed that the radiosensitivity of lymphocytes irradiated at 37°C and 20°C in similar doses does not depend on the temperature of storage and irradiation of samples [10]. Irradiation of blood samples was performed for 20–120 s using the RUT instruments as a source of X-ray radiation (200 kV, 2 keV/µm, 1 Gy/min; Radiation Sources Core Facility, Institute of Cell Biophysics, Russian Academy of Sciences, Pushchino).
Cells were cultured and cytogenetic samples of lymphocytes were prepared using the generally accepted method of Fenesh [11]. The criterion for damage was the frequency of MNs in CBBLs. In analyzing MNs in CBBLs, we used the criteria described in [7]. At least 500 CBBLs were counted for each experimental point for an individual donor.
Statistical differences between groups were assessed using the nonparametric Mann–Whitney U test. The degree of variation of values within the group was determined using the coefficient of variation. Pairwise correlation analysis was performed using Pearson correlation coefficients.
Figure 1 shows the spontaneous frequency of MNs in CBBLs of cancer patients and healthy donors.
Individual frequencies of MNs in the control group were in the range 0.50−2.80%; in the group of patients, 1.95−7.30%. The average value of the spontaneous level of cytogenetic damage in cancer patients was 2.6 times higher than that in the control group. In addition, in the group of patients, significant individual variability in values was observed compared to the cohort of healthy donors. The average values of CBBLs with MNs in patients significantly exceeded the average values in healthy donors (4.07 and 1.57, respectively); the median values in the groups also differed significantly (3.5 and 1.4, respectively). Increased and comparable spontaneous levels of MNs in CBBLs were detected not only in cancer patients but also in patients with diabetes mellitus, thyroid diseases, in nuclear industry employees who received a dose of ~20 cGy as a result of chronic irradiation, as well as in medical personnel of X-ray rooms and those working with diagnostic radionuclides [12]. A long-term interlaboratory study of 7000 individual values of spontaneous MN levels in CBBLs showed that, for apparently healthy persons of different ages, the values are in the range of 1−6% [13]. In this and other studies using counting chromosomal aberrations, it was not possible to demonstrate the correlation between the increase in the spontaneous level of damage in lymphocytes and person’s age, as well as smoking or living in unfavorable environmental conditions. However, an increased spontaneous level of MNs in CBBLs (closer to the upper limit of normal) in individuals was correlated with the risk of inducing cancer [14].
Figure 2 shows the average number of MNs (after subtracting the spontaneous background values) in lymphocytes after irradiation at a dose of 10 cGy. Individual values of the number of MNs in lymphocytes in the control group were in the range 0.7−8.63%; in the group of patients, 1.2−6.67%. The within-group variability of values in the groups was similar.
The average radiosensitivity in cancer patients (2.04) did not differ from healthy donors (2.28). The median values in the groups were similar (1.42 and 1.7). Low-dose radiation exposure simulates the sensitivity of individuals to radiation loads associated with environmental pollution, occupational activities, as well as CT scanning, mammography, and other X-ray examinations, the use of which in diagnostics has increased manifold over the past decade. We have previously shown that, in patients with secondary immunodeficiency syndrome, the radiosensitivity of lymphocytes to a dose of 10 cGy also did not differ from that in healthy donors, but the median values in immunodeficiency donors were twice higher [15].
Figure 3 shows the number of MNs (after subtracting the spontaneous background) in lymphocytes irradiated at a dose of 2 Gy in patients and healthy subjects. Individual values of the number of MNs in lymphocytes were in the range 5.50−26.10% in the control group and 5.00−31.91% in the group of patients, whereas the within-group variability of values in both groups was the same. The average values of CBBLs with MNs in cancer patients and apparently healthy individuals did not differ significantly and were 16 and 14.13, respectively. The median values in the groups were similar (15.34 and 11.94, respectively).
The development of personalized medicine, the search for approaches to overcoming the negative consequences of radiotherapy, and the introduction of hadron therapy make determining the individual radiosensitivity of patients an extremely relevant task. Most studies use doses of 1–2 Gy, which, according to dose dependences obtained on human lymphocytes using cytogenetic methods, characterize the cellular response that is the result of the action of stress-induced DNA repair systems and cell death. The absence of a difference in radiosensitivity in the cancer patients studied by us indicates that DNA damage repair systems were not disturbed after irradiation at a dose of 2 Gy. Analysis of the data obtained also showed that there was no correlation between the spontaneous level of MNs in CBBLs and the radiosensitivity of individuals in both groups. In [16], it was shown that the radiosensitivity of human lymphocytes after irradiation in vivo and in vitro at doses up to 3 Gy was the same, which makes it possible to consider irradiation of whole blood as an adequate test system for determining individual radiosensitivity. Since peripheral lymphocytes are distributed throughout the body and are in constant circulation, the studied index demonstrates the degree of damage to the most sensitive cells of normal tissue at a dose equal to a single fraction of irradiation during radiotherapy of tumors. Published data on the radiosensitivity of patients depending on the type and stage of cancer are discrepant: a decrease, an increase, or no changes relative to healthy subjects were shown, and a high variability of values was observed [17, 18]. Data on the correlation of the spontaneous level of cytogenetic damage with the radiosensitivity of lymphocytes in vitro are also contradictory, which is associated with individual variability and the difficulty of selecting adequate cohorts for comparison.
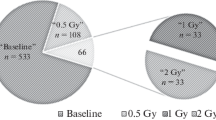
Figure 4 shows the average values of MN levels in lymphocytes of healthy donors and patients after sequential irradiation first at a dose of 10 cGy and then, 5 h later (the time required for the development of RAR), at a dose of 2 Gy. As in the case of a single irradiation with low and therapeutic doses, a significant individual scatter was observed in the groups: in the control group, the values were in the range 4.20−26.00%; in the experimental group, 6.10−31.70%. The variability of values did not differ in both groups, and no significant differences in radiosensitivity were detected. The average values of CBBLs with MNs in cancer patients and healthy donors were similar (12.87 and 11.37, respectively). The median values in the groups were 11.17 and 9.2, respectively, which differed significantly from the corresponding values after exposure to X-ray at a dose of 2 Gy only.
On the basis of the data obtained, we calculated the value of RAR using to the formula RAR = ((D1 – D0) + (D2 – D0))/(D1+2 – D0), where D1 is the number of MNs in lymphocytes after irradiation at a dose of 10 cGy; D2 is the number of MNs in lymphocytes after irradiation at a dose of 2 Gy; D0 is the number of MNs in non-irradiated lymphocytes; and D1+2 is the number of MNs in lymphocytes after irradiation at a dose of 10 cGy + 2 Gy.
Four types of cellular response were analyzed: reliable RAR (at values >1.2, since this level corresponds to the dose reduction factor values of the most effective chemical radioprotectors [19]), unreliable RAR (values 1.0−1.2), unreliable (0.8−1.0), and reliable increase in radiosensitivity (< 0.8) [6].
As can be seen in Table 1, individuals of both groups had the same frequency of RAR induction, the maximum value of which was 3.51 in the control group and 2.56 in cancer patients. The average RAR value was also the same in both cohorts and was equal to 1.60 in healthy subjects and 1.49 in patients. Previously, similar results were obtained when comparing healthy donors and patients with immunodeficiency states [15], as well as in residents of contaminated areas and nuclear industry employees [5, 20, 21]. The RAR value depends on hereditary factors, conditions of RAR induction, and environmental conditions. The groups differed only in the number of individuals with increased radiosensitivity: they were observed only among patients. We assume that the revealed oppositely directed response of cells to irradiation according to the RAR scheme may also indicate the induction of genetic instability, which is revealed only after additional irradiation of lymphocytes at a stress non-lethal dose or according to the RAR scheme.
The results obtained in our work showed that the spontaneous level of cytogenetic damage in lymphocytes of cancer patients is 2.6 times higher than that in healthy individuals of the same age. There were no differences in radiosensitivity to low and medium doses of X-ray between groups, and RAR was induced in lymphocytes of patients at the same frequency and to the same extent as in healthy donors. These data may indicate that the processes responsible for the onset and development of various types of cancer, as well as subsequent treatment, do not affect the mechanisms involved in the formation of RAR (in particular, those associated with the induction of error-free DNA damage repair, which is induced in a narrow range of low doses of radiation specific to each biological object, as well as the regulation of apoptosis, which leads to the death of the most damaged cells after irradiation with higher doses). The use in our work of indices that characterize the individual genetic instability of human lymphocytes at different levels of oxidative stress, in our opinion, is useful for understanding the role of the adaptive potential of patient stem cells in the long term after therapy and searching for new ways to protect healthy tissues.
REFERENCES
Pelevina, I.I., Petushkova, V.V., Biryukov, V.A., et al., The “radiation-induced non-targeted effects” and their role in human cell response to low radiation forcing, Radiats. Biol. Radioecol., 2019, vol. 59, no. 3, pp. 261–273. https://doi.org/10.1134/S086980311903010X
Kogarko, I.N., Akleev, A.V., Petushkova, V.V., et al., Adaptive response as a criterion for assessing individual human radiosensitivity. Review, Radiats. Risk, 2022, vol. 31, no. 1, pp. 93–104. https://doi.org/10.21870/0131-3878-2022-31-1-93-104
Rödel, F., Frey, B., Gaipl, U., et al., Modulation of inflammatory immune reactions by low-dose ionizing radiation: molecular mechanisms and clinical application, Curr. Med. Chem., 2012, vol. 19, no. 12, pp. 1741–1750. https://doi.org/10.2174/092986712800099866
Balakin, V.E., Zaichkina, S.I., Rozanova, O.M., et al., Low-dose ionizing radiation inhibits the aging-related rise in accumulation of spontaneous cytogenetic abnormalities: the genome-stabilizing effect, Dokl. Biol. Sci., 2000, vol. 374, pp. 488–490.
Ghiassi-Nejad, M., Mortazavi, S.M., Cameron, J.R., et al., Very high background radiation areas of Ramsar, Iran: preliminary biological studies, Health Phys., 2002, vol. 82, no. 1, pp. 87–93. https://doi.org/10.1097/00004032-200201000-00011
Petushkova, V.V., Pelevina, I.I., Serebryanyi, A.M., et al., Components of adaptive response induced by occupational exposure to ionizing radiation. Some approaches to analysis, Radiats. Risk, 2020, vol. 29, no. 4, pp. 97–105. https://doi.org/10.21870/0131-3878-2020-29-4-97-105
Fenech, M., Chang, W.P., Kirsch-Volders, M., et al., HUMN project: detailed description of the scoring criteria for the cytokinesis-block micronucleus assay using isolated human lymphocyte cultures, Mutat. Res., 2003, vol. 534, nos. 1–2, pp. 65–75. https://doi.org/10.1016/s1383-5718(02)00249-8
World Medical Association, World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects, JAMA, 2013, vol. 310, no. 20, pp. 2191–2194.
Zaichkina, S.I., Rozanova, O.M., Aptikaeva, G.F., et al., Low doses of gamma-radiation induce nonlinear dose responses in mammalian and plant cells, Nonlinearity Biol. Toxicol. Med., 2004, vol. 2, no. 3, pp. 213–221. https://doi.org/10.1080/15401420490519861
Zaichkina, S.I., Aptikaeva, G.F., Rozanova, O.M., et al., Action of chronic irradiation on the cytogenetic damage of human lymphocyte culture, Environ. Health Perspect., 1997, vol. 105, suppl. 6, pp. 1441–1443. https://doi.org/10.1289/ehp.97105s61441
Fenech, M., The in vitro micronucleus technique, Mutat. Res., 2000, vol. 455, no. 1–2, pp. 81–95. https://doi.org/10.1016/s0027-5107(00)00065-8
Andreassi, M.G., Barale, R., Iozzo, P., and Picano, E., The association of micronucleus frequency with obesity, diabetes and cardiovascular disease, Mutagenesis, 2011, vol. 26, no. 1, pp. 77–83. https://doi.org/10.1093/mutage/geq077
Bonassi, S., Znaor, A., Ceppi, M., et al., An increased micronucleus frequency in peripheral blood lymphocytes predicts the risk of cancer in humans, Carcinoge-nesis, 2007, vol. 28, no. 3, pp. 625–631. https://doi.org/10.1093/carcin/bgl177
Bonassi, S., El-Zein, R., Bolognesi, C., and Fenech, M., Micronuclei frequency in peripheral blood lymphocytes and cancer risk: evidence from human studies, Mutagenesis, 2011, vol. 26, no. 1, pp. 93–100. https://doi.org/10.1093/mutage/geq075
Rozanova, O.M., Smirnova, E.N., Belyakova, T.A., et al., A study on the radiosensitivity and induction of adaptive response in peripheral blood lymphocytes of patients with secondary immunodeficiency syndrome, Biophysics (Moscow), 2023, vol. 68, no. 5, pp. 767–773. https://doi.org/10.31857/S0006302923050137
Gantenberg, H.W., Wuttke, K., Streffer, C., and Müller, W.U., Micronuclei in human lymphocytes irradiated in vitro or in vivo, Radiat. Res., 1991, vol. 128, no. 3, pp. 276–281.
Pelevina, I.I., Aleshchenko, A.A., Antoshchina, M.M., et al., Individual variability in the manifestation of the adaptive response of human cells to ionizing radiation. Approaches to its determination, Radiats. Biol. Radioecol., 2007, vol. 47, no. 6, pp. 658–666.
Ivanova, T.I., Khorokhorina, V.A., Sychenkova, N.I., et al., in Proceedings of the 3rd Russian Conference with International Participation “Radiobiological Foundations of Radiation Therapy,” October 17–18, 2019, Dubna, 2019, pp. 66–68.
Cortese, F., Klokov, D., Osipov, A., et al., Vive la radiorésistance!: converging research in radiobiology and biogerontology to enhance human radioresistance for deep space exploration and colonization, Oncotarget, 2018, vol. 9, no. 18, pp. 14692–14722. https://doi.org/10.18632/oncotarget.24461
Barquinero, J.F., Barrios, L., Caballín, M.R., et al., Occupational exposure to radiation induces an adaptive response in human lymphocytes, Int. J. Radiat. Biol., 1995, vol. 67, no. 2, pp. 187–191. https://doi.org/10.1080/09553009514550231
Gerić, M., Popić, J., Gajski, G., and Garaj-Vrhovac, V., Cytogenetic status of interventional radiology unit workers occupationally exposed to low-dose ionizing radiation: a pilot study, Mutat. Res. Genet. Toxicol. Environ. Mutagen., 2019, vol. 843, pp. 46–51. https://doi.org/10.1016/j.mrgentox.2018.10.001
ACKNOWLEDGMENTS
We express our sincere gratitude to the doctors of the Protvino Municipal Hospital for selecting cohorts and taking samples, as well as residents of Protvino and employees of the Institute of Theoretical and Experimental Biophysics of the Russian Academy of Sciences and Lebedev Physical Institute of the Russian Academy of Sciences who participated in the study as donors.
Funding
The work on studying radiosensitivity and the induction of radiation adaptive response in peripheral blood lymphocytes of patients with cancer was performed as part of basic research under the State Assignment no. 075-01025-23-01 (Institute of Theoretical and Experimental Biophysics of the Russian Academy of Sciences), as well as with partial funding from the research agreement no. 04/23 between the Physical-Technical Center of Lebedev Physical Institute of the Russian Academy of Sciences and the Institute of Theoretical and Experimental Biophysics of the Russian Academy of Sciences.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
CONFLICT OF INTEREST
The authors of this work declare that they have no conflicts of interest.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Experiments with animals were approved by the Commission of the Institute of Bioorganic Chemistry of the Russian Academy of Sciences for control over the keeping and use of laboratory animals (protocol no. 891/22 dated May 17, 2022).
Additional information
Translated by M. Batrukova
Publisher’s Note.
Pleiades Publishing remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Balakin, V.E., Rozanova, O.M., Strelnikova, N.S. et al. Study of Radiosensitivity and Induction of Radiation Adaptive Response in Peripheral Blood Lymphocytes of Patients with Oncological Diseases Using the Micronuclear Test. Dokl Biochem Biophys (2024). https://doi.org/10.1134/S1607672924600362
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1134/S1607672924600362