Abstract
The influence of low-dose ionizing radiation on a human being is increasing in the modern world (medical diagnostics etc.). The issue of the effect of low-doses on human health is topical and controversial. It is known that in the population up to 15% of people react to radiation exposure differently from what has been expected, which, according to the published data, happens owing to their genome peculiarities. The objective of the current study was to investigate the influence of chronic lowdose rate exposure (doses to red bone marrow varied within the range 3—4600 mGy) of the Techa River residents (South Urals) on the radiosensitivity of T cells in vivo and in vitro under additional gamma exposure of peripheral blood T lymphocytes (0.5, 1, and 2 Gy). Such cytogenetic parameters as frequency of unstable chromosome aberrations and micronuclei were used as irradiation markers. Persons were considered radiosensitive if the obtained values of the analyzed parameters for them exceeded the 90% percentile. On the basis of the findings of the performed study, the following conclusions were drawn: about 10% of donors demonstrated increased radiosensitivity; moreover, the effect did not depend on the dose of chronic exposure; no age dependence of radiosensitivity in the studied age range (49–89 years) of the donors was revealed. In most cases, we did not detect a reproducible radiosensitivity effect in the same donor under different irradiation regimes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Today the influence of low doses of radiation on people is considerable. Numerous medical procedures and adverse environmental conditions increase the presence of the radiation factor in people’s lives. In the case of accidental exposure or an emergency for professionals and the community, the goal of radiation protection is to prevent deterministic effects and limit stochastic effects in humans in clinical practice [1]. To achieve this goal, it is necessary to determine the DNA damage most accurately. It plays a role in realization of the effects of irradiation in the human body. DNA damage is also used to assess the exposure dose of a person in the absence of physical dosimetry or for validating its assessments.
The most common method for detecting DNA damage is cytogenetic. This approach is based on counting the frequency of chromosomal aberrations or micronuclei in human peripheral blood T cells, which can, under certain restrictions, be recalculated to an exposure dose using a dose–effect calibration curve [2].
Accumulated scientific data prove the existing variations in the individual radiation responses of organisms, which is also a limitation for biodosimetry methods. For example, it was noted that, even in people with acute radiation syndrome who survived the atomic bombing in Hiroshima and Nagasaki (Japan), there were individual differences in the intensity of hair loss, in the reaction of hemopoiesis, etc. [3].
The study of the mechanisms of individual radiosensitivity of people is one of the promising areas of research in the field of radiation genetics. The relevance of this topic is due to not only possible emergency situations, but the need for professional selection of specialists in contact with ionizing radiation, selection of sources and adequate radiation doses during radiation therapy, justification of the need for a large number of medical diagnostic procedures, and clarification of radiation safety standards for the public and personnel of nuclear plants [4].
Individual radiosensitivity means the ability of a biological object to react in a certain way to ionizing radiation. Individual radiosensitivity can be assessed using several criteria: different reactions of patients to radiation therapy, reactions of healthy tissues to radiation therapy long time after it, presence of individuals most susceptible to radiation-induced cancers in the population, interindividual variability in the DNA breaks repair or the elimination rate of damaged cells, different cell response to ionizing radiation at certain doses and dose rates [5]. The induction of double DNA breaks, which result in chromosomal aberrations and partially in the micronuclei, is considered a manifestation of the organism’s individual sensitivity to the effect of radiation [2]. Recently, much attention has been paid by researchers not to the direct effect of radiation on the cell (target theory), but to the so-called “non-targeted effects,” which are described as “bystander effect,” “abscopal effect,” “adaptive response,” genomic instability, and delayed apoptosis [6].
One of the most important issues in modern radiobiology is the question of the correlation of the organism’s genome characteristics and its radiosensitivity. So, it is known that radiation therapy is especially fatal for carriers of homozygotes of the ATM gene and with a high probability can trigger cancer in ATM-, BRCA1- and BRCA2-, and TP53-heterozygous carriers. It is believed that total gene mutations associated with a predisposition to radiosensitivity or cancer can be represented in the population in a substantial proportion of 5 to 15% [7].
Analysis of the published data shows that the body’s radiosensitivity is manifested differently when exposed to low and high doses of ionizing radiation. In [8], the manifestation of individual radiosensitivity was recorded when exposed to a dose of 1 mGy using fluorescence for the γH2AX marker. It was noted that in normal human skin cells at low (10 mGy) and high (2 Gy) radiation doses, changes in expression were observed in different sets of genes [9]. When working with DNA microarrays (10 500 gene probes), it was found that, among 853 probes, the expression of 214 genes was specifically determined by low doses (10 mGy), and the expression of 370 other genes was determined by exposure to high doses (2 Gy). A set of 140 known genes that respond to low-dose exposure included mainly genes for homeostasis, cell communication, signaling, membrane structure, cytoskeleton, RNA and protein synthesis, chromatin, energy metabolism, stress, cell death, and transport. Most importantly, DNA repair genes were rarely expressed under conditions of low doses. Thus, cellular and tissue reactions to radiation in the range of low doses are very specific and differ from those caused by high doses.
When studying the irradiation effects on humans in vitro and in vivo, it was suggested that the question of the existence of radiosensitive and radioresistant genotypes is not as straightforward as radiobiologists had previously thought. The authors suppose that at least three partially intersecting groups of polymorphic loci of genes that are associated with susceptibility to increased somatic mutagenesis should be isolated. These groups are (1) loci associated with the level of spontaneous chromosomal aberrations (for example, the loci of genes GSTM1 and GSTT1), (2) loci associated with radiosensitivity during in vivo irradiation (possibly the SOD2 gene), and (3) loci the variability of which determines the radiosensitivity of chromosomes during irradiation in vitro (for example, CYP1A1, CAT). So, it was shown that the frequencies of spontaneous (in vivo) and induced (in vitro) chromosomal aberrations are associated with different groups of genes. Large deletions of detoxification genes were more often associated with reduced levels of cytogenetic disorders. Most SNPs, including those associated with DNA repair, weakly correlated with the radiosensitivity of chromosomes [10, 11]. These data can serve as evidence that, during the evolution of the cell, several different mechanisms or ways of cellular response have been developed, which can substitute or complement each other in stressful situations. The genetic diversity of the cells of one tissue allows them to respond differently to the harmful effects (in our case, γ radiation), adapt to new conditions, or launch apoptosis mechanisms without affecting the activity of the tissue and the whole organism.
The aim of this study is to analyze the effect of chronic low-intensity irradiation of the body on the radiosensitivity of peripheral blood T cells after γ irradiation in vitro. For this, the data obtained from the residents of the South Urals who were subjected to chronic cumulative exposure in the dose range from 0.003 to 4.6 Gy were taken from the cytogenetic base of the Urals Research Center for Radiation Medicine (URCRM). Unstable chromosomal aberrations (UCA) of the exchange type and the frequency of micronuclei (MN) in cytokinesis-blocked mitosis were selected as DNA damage markers. The study evaluated the effect of gender and age on the radiosensitivity of T cells.
MATERIALS AND METHODS
Criteria for the donor grouping for research. Cytogenetic studies, the results of which are given in this work, were carried out at the URCRM for several years among persons exposed to chronic exposure in the South Urals as a result of accidental discharges of liquid radioactive waste from PA Mayak into the Techa River from 1948 to 1956. The population exposure was cumulative: external due to γ exposure from the river water and internal β exposure due to intake of 89,90Sr with drinking water and food [12]. The range of cumulative doses of exposure of red bone marrow (RBM) of the examined people was from 0.003 to 4.6 Gy. Individual exposure doses for the residents of the coastal villages of the Techa River were calculated in the biophysics laboratory of the URCRM using the updated dosimetric system TRDS-2016 [13].
A cytogenetic study was carried out for persons born before 1960, of both genders, mainly of three nationalities (Russians, Tatars, Bashkirs) who lived in the coastal villages of the Techa River. Persons with a history of autoimmune, cancer, chronic inflammatory diseases in the acute phase and individuals receiving cytostatics and antibiotics, as well as those who underwent diagnostic irradiation in the 6 months prior to taking a blood sample, were excluded from the study. Information about the health status of donors was obtained from the DB Man of the URCRM, and information on the history of oncological morbidity in the subjects was provided by the staff of the epidemiological laboratory of the URCRM. In accordance with applicable international standards (Helsinki Declaration, 1964) and with the permission of the Ethics Committee of the URCRM, all patients gave informed consent for blood sampling and further research.
Metaphase chromosome preparations to assess the frequency of unstable chromosomal aberrations. To assess the frequency of the UCA of exchange type (dicentric and ring chromosomes, acentric rings), preparations of metaphase chromosomes from donor peripheral blood T lymphocytes were prepared according to the protocol presented in [2]. The protocol includes four consecutive stages: cultivation of cells up to the metaphase stage, hypotonic treatment of metaphase cells, fixation of metaphase plates, and the actual preparation of chromosome preparations. Five milliliters of blood was taken from the ulnar vein in the morning on an empty stomach in syringes with heparin. The cultivation of T cells was performed in sterile flasks. From one to several samples was prepared for one donor. One sample was cultured without irradiation in vitro, and the rest were subjected to γ irradiation in vitro at doses of 0.5, 1, and 2 Gy. Additional irradiation was performed on the Igur-1 facility, the γ-irradiation power was 0.014 Gy/s; the irradiation source was 137Cs; the nonuniformity of irradiation reached 5%.
Cells were cultured in a CO2 incubator at 37.5°C for 54 h after irradiation. Three hours before the end of cultivation colcemid was added to the culture at a total concentration of 0.1 mg/mL (Paneko, Russia). Cells were fixed three times with cold 4°С freshly prepared fixative (3 parts of ethyl alcohol : 1 part of glacial acetic acid). To obtain preparations of chromosomes, the suspension was pipetted on cooled, fat-free glasses, which were dried in air. The quality of the preparation was assessed with phase-contrast microscopy [14].
The preparations were stained with 2% Giemsa solution for 10 min. The analysis was carried out with light microscopy, at 1000× magnification on an AxioImagerZ2 microscope (Carl Zeiss, Germany). From 100 to 500 cells were analyzed per person.
According to the results of the UCA study, four groups of donors were formed depending on the dose of irradiation of the samples in vitro (Fig. 1):
(1) The “baseline” group: blood culture of donors was not irradiated in vitro, but T cells were exposed in vivo as a result of chronic exposure of the residents of the coastal villages of the Techa River. This was the largest group represented in this work (533 participants).
(2) The “0.5 Gy” group: blood culture of donors was additionally irradiated in vitro at a dose of 0.5 Gy. This was the second largest group in this work (108 participants).
(3) The “1 Gy” group: blood culture of donors was additionally irradiated in vitro at a dose of 1 Gy.
(4) The “2 Gy” group: blood culture of donors was additionally irradiated in vitro at a dose of 2 Gy.
The high-dosed groups of 1 Gy and 2 Gy were represented by the same donors; i.e., they intersected completely (included 33 participants in each group). For all donors who belonged to the 0.5 Gy, 1 Gy, and 2 Gy groups, the baseline UCA level was estimated; i.e., these groups overlapped completely with the “baseline” donor group.
Preparation of cytokinesis-blocked lymphocytes. The protocol of the micronucleus test procedure consisted of several stages: cultivation of peripheral blood T lymphocytes, blocking cytokinesis, hypotonic treatment, fixing of cell suspension, and then preparation of specimens [15].
The whole blood samples were taken from the ulnar vein in a syringe with heparin. All preparations of working solutions and cell culture production were performed under sterile conditions. Two culture flasks were prepared for each blood sample. The flasks were incubated in a CO2 incubator at 37°C and 5% CO2. After 29 h from the start of incubation, the second sample was subjected to γ irradiation at a dose of 1 Gy in vitro. Samples were irradiated at the IGUR-1 facility. After 48 h from the start of incubation, 70 μL of a cytochalasin B working solution in DMSO was added to the samples. The samples were treated with hypotonic KCl solution (0.125 M) and fixed with a mixture of ethanol and glacial acetic acid in 3 : 1 ratio after 72 h from the start of incubation. Then, preparations were prepared from the fixed cell suspension, which after drying were stained with 2% Romanovsky–Giemsa solution for 2 h.
Assessment of cells with micronuclei was performed with light microscopy of 10 × 100 on an AxioImager microscope (Germany). The number of binuclear lymphocytes with micronuclei per 1000 binuclear lymphocytes was estimated.
Two donor groups were formed to analyze with micronucleus test:
(1) the baseline group: blood culture of donors was not irradiated in vitro, but T cells were exposed to chronic exposure;
(2) the 1 Gy group: blood culture of donors was additionally irradiated in vitro at a dose of 1 Gy.
For all donors from the 1 Gy group, the initial level of cells with micronuclei was evaluated; i.e., the groups overlapped with respect to donors. The baseline group was represented by 633 donors, and the 1 Gy group had 497 donors.
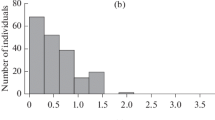
Selection criteria for radiosensitive persons. In this study, persons who had an increased cytogenetic cellular response to radiation exposure were considered as radiosensitive donors. As shown by the analysis of cytogenetic data distributions presented in this work, the data did not follow a normal distribution, which corresponds to the published data. Radiosensitive donors included people whose indices were above the 90th percentile [16]. In each sample, we analyzed the influence of the dose of chronic exposure of RBM on the indices of radiosensitivity. The influence of gender and age at the time of examination on the increased level of cytogenetic disorders was also assessed. For those donors who were represented in different dose groups, the reproducibility of T-cell radiosensitivity was assessed at different doses of radiation in vitro.
Statistical data processing was performed using the SigmaPlot program; the nonparametric Mann–Whitney rank test was used to compare two data samples.
RESULTS
Table 1 presents the results of the analysis of UCA frequency in the examined groups. In the baseline group, 5.25% of radiosensitive individuals were identified among 533 participants. The age of these donors ranged from 49 to 89 years; the range of RBM exposure in them varied from 0.01 to 2.6 Gy; cells with elevated levels of UCA were detected 2 times more often in women.
In the 0.5 Gy group, an increased level of chromosomal aberrations was observed more often in women (9 and 2, respectively); the age of these donors ranged from 56 to 76 years; individual doses of chronic exposure of RBM ranged from 0.05 to 1.43 Gy.
Since the baseline and 0.5 Gy groups were the most numerous, it was assumed that in these groups the highest reproducibility of the increase in the frequency of radiation markers among the same persons would be revealed. However, only one woman, 73 years old, with a dose of 0.75 Gy to RBM, showed elevated levels of UCA in the baseline group and in the 0.5 Gy group. Thus, the remaining individuals who had an UCA level above the 90th percentile in the 0.5 Gy group did not have the same high UCA values in the baseline group.
In the 1 Gy group, elevated levels of chromosomal exchanges were detected in three people (one woman and two men). These were donors aged 60, 70, and 79 at the time of the survey. RBM doses ranged from 0.007 to 1.71 Gy in them. Four radiosensitive donors (three women and one man) were identified in the 2 Gy group. The age interval was also wide: from 57 to 82 years, and RBM doses varied from 0.007 to 1.39 Gy. Despite the fact that the last two groups completely included the same donors, the effect of radiosensitivity was found in different subjects examined. None of them was defined as radiosensitive in assessing the baseline level of UCA.
Analysis of the frequency of T cells with micronuclei revealed significant differences in indicators depending on gender. Therefore, cytogenetic data are presented separately for men and women (Tables 2 and 3).
As can be seen from Table 2, the baseline level of the frequency of lymphocytes with MN from an indicator of 30‰ was exceeded in 37 women, which accounted for 9.5% of the examined 388 samples. The age range of radiosensitive women ranged from 51 to 88 years; the dose to RBM was in a wide range from 0.01 to 2.78 Gy.
When assessing the radiosensitivity of donor lymphocytes in the 1 Gy dose group, the frequency of lymphocytes with MN exceeded 206.5‰ in 29 women, which accounted for 9.8% of 294 samples examined. The age range of the examined individuals ranged from 54 to 79 years.
Radiosensitive donors whose frequency of cells with micronuclei exceeded the 90th percentile both in the baseline and in the 1 Gy groups were the same three women. Their age was 65, 66, and 67 years; doses to RBM were 1.26, 1.29 and 1.96 Gy; i.e., they were women with chronic exposure doses to RBM exceeding 1 Gy.
As can be seen from Table 3, in the baseline group, the frequency of lymphocytes with MN exceeded the value of 26.3‰ in 24 men, which accounted for 9.8% of the entire 245 samples. The age of radiosensitive men ranged from 54 to 84 years; the doses to RBM varied in a wide range from 0.01 to 1.46 Gy.
When assessing the radiosensitivity of donor lymphocytes in the 1 Gy dose group, the frequency of lymphocytes with MN exceeded 183.4‰ in 20 men, which accounted for 9.8% of 203 patients examined. Their age ranged from 55 to 73 years. The range of doses to RBM in these individuals was 0.08–1.53 Gy.
Radiosensitive donors whose frequency of cells with micronuclei exceeded the 90th percentile both in the baseline and 1 Gy groups were seven men. Their age was 58, 63, 63, 65, 68, 73, and 73 years; the doses to RBM were 0.77, 0.93, 1.17, 0.14, 0.18, 1.01, and 1.24 Gy.
Thus, in the course of cytogenetic research conducted with two assays and in vitro γ irradiation among the population of the Southern Urals subjected to chronic radiation exposure, an increase in cytogenetic indicators was revealed in a small part of the participants examined (about 10%). There was no effect of dose to RBM after chronic radiation exposure on T-cell radiosensitivity, since excess DNA damage in PHA-stimulated lymphocytes was observed in donors with both low and high doses to RBM (from 0.007 to 2.78 Gy). High levels of UCA were more often detected in women, but the micronucleus test did not reveal the gender effect. No effect of age on the radiosensitivity of T cells in individuals in the studied age range (48–89 years) was detected either. Only one woman demonstrated elevated values of chromosomal aberrations in both the baseline and 0.5 Gy groups. The micronucleus test revealed deviations in both groups in three women and seven men (1 and 3.4% of donors, respectively).
DISCUSSION
The question of the radiosensitivity of the body is rather complicated, since the body is a complex system and includes many elements and connections between them. Radiosensitivity is usually estimated on the basis of cell culture survival or in animal experiments in classical radiobiology [4].
The data of other researchers and the results presented in our work demonstrate that it is not yet possible to clearly assess the “radiosensitivity” of the whole body on the basis of the known “cellular” approaches. A complex multilevel system with a huge number of regulatory links and mechanisms (which is the human body) can modify the radiobiological response and show a different response to irradiation in comparison with cell culture irradiated in vitro. The analysis of products of genes responsible for the cell cycle regulation (TP53, CHK2, MDM2, NBS1, BRCA1, RAD17, ATM) revealed that an insufficient amount or absence of enzymes that regulate certain stages of the cell cycle leads to an increase in the frequency of mutation and genomic instability of the cell [17].
Radiosensitivity of the body can be detected after both low and high doses of ionizing radiation, which is indirectly confirmed by the data obtained in this study. Importantly, two independent cytogenetic methods (simple staining method of metaphase chromosomes and micronucleus test) provided similar results regarding the effect of hazardous chronic exposure on the radiosensitivity of T cells of the examined individuals. The data analysis demonstrated that radiosensitivity was detected at low doses to RBM (0.007 Gy) and at high doses to RBM (up to 2.78 Gy) in all groups of donors. Thus, no effect of the dose of RBM chronic irradiation on the manifestation of the radiosensitivity of PHA-stimulated T lymphocytes was detected in this work.
It is believed that, at low doses, “untargeted effects” play a significant role, which leads to a greater effect from exposure owing to an increase in the volume of tissue involved in the response, and dose-dependent effects are not observed. Probably, mechanisms underlying these effects affect individual diversity in the radiobiological response. It was convincingly shown that the intercellular gap channels and the secretion of soluble factors into the extracellular space, where the exosomes play an active role, are involved in transmitting signals from radiation-damaged cells to neighboring unirradiated cells [18]. It is noted that, even at low doses, the damage from radiation is greater than the initial volume of tissue exposed to radiation.
It is important to note that, in the present work, cells from 5 to 12% of examined donors in all groups were radiosensitive. This can prove the significant influence of genome features on radiosensitivity. For example, the structural features of chromatin and genes (SNPs, mutations) can modify the cellular radiobiological response in several ways. They can cause an increased level of chromosomal aberrations, enhance or inhibit the expression of individual genes, change the intensity of biochemical reactions and their cascades, etc. [19]. The influence of the genetic factor on the variation of the radiobiological response is proved by the existence of rare human syndromes that suggest high radiosensitivity when exposed to ionizing radiation (for example, ataxia telangiectasia, Li-Fraumeni syndrome, Fanconi anemia, Nijmegen breakage syndrome (NBS), Cornelia de Lange syndrome, etc.) [7]. With such syndromes, the fraction of surviving cells is from 10 to 50% after irradiation of 2 Gy (SF2); also, the yield of induced chromosomal aberrations increases 1.5–2 times. Homozygous carriers of mutations of the LIG4 or ATM genes are characterized by SF2 of only 1%. They respond well to radiation therapy and it is appropriate to use the term “hyperradiosensitivity” for them [20, 21].
Radiosensitivity has been most well studied in patients after radiation therapy. Various degrees of tissue damage and wide variability of chromosomal damage were noted in these people. Polymorphism of the GSTP1 gene could be attributed to ∼35% of the variability of the response to radiotherapy [22, 23].
The correlation of the frequency of γ-induced (1 Gy in vitro) chromosomal aberrations with the polymorphism of 45 candidate genes contributing to reparation, detoxification of xenobiotics, and oxidative stress was studied. A total of 53 sites were studied in 99 participants. The association of chromosomal aberration levels with the carrying of minor alleles of the polymorphic sites of the OGG1 Ser326Cys, ABCB1 Ile1145, and NQO1 Pro187Ser genes (p = 0.0002) was found during the study. The combination of genetic and cytogenetic predictors explained more than 30% of the population variability in radiosensitivity of chromosomes [24].
The wide variability of cytogenetic parameters was also noted in the present study, even at high doses of radiation in vitro. Thus, the frequency of UCA in the 1 Gy group varied from 5 to 24 per 100 cells, and in the 2 Gy group, from 18 to 104 per 100 cells. The frequency of cells with micronuclei in the 1 Gy group ranged from 30 to 336‰.
Factors that model the radiobiological response are known to include age, smoking, the presence of diabetes, and vascular diseases associated with collagen. Whether this indicator is affected by gender, ethnicity, diet, alcohol, and other habits remains either not known or contradictory [25]. We did not find any effect of age on the radiosensitivity of T lymphocytes in our study. Analysis of the data showed that an increased level of DNA damage was observed in people of a wide age range from 49 to 89 years.
As for the reproducible high radiosensitivity of T cells, evaluation of the UCA frequency revealed only one woman (which is less than 1% of the sample) in which an increased frequency of chromosomal exchanges was detected both in the baseline and 0.5 Gy groups. Contrary to our expectations, radiosensitive donors in the 1 Gy and 2 Gy groups did not have the same result in the baseline group. When using the micronucleus test, reproducible radiosensitivity of the cells was noted in a larger number of people examined (three women and seven men).
In our analysis of cytogenetic data, as in any study, there are shortcomings that could affect the results. These include a different number of cells (from 100 to 500) when analyzing metaphase plates, a small number of donors in high-dose groups, errors in estimating individual doses of RBM irradiation, which can in some cases be up to 30%. However, the conclusions that were made on the basis of the analysis performed correspond to the published literature data presented by us above.
CONCLUSIONS
Thus, we believe that our results allow us to conclude the following:
It is necessary to carefully draw conclusions about the individual reaction of the whole body to radiation on the basis of cellular techniques carried out in vitro.
The individual radiosensitivity of the body in about 10% of the people examined will significantly affect the results of individual biodosimetry. This should be considered when preparing expert opinions on the fact of human exposure, as well as when interpreting the values of accidental exposure doses in clinical practice.
REFERENCES
Di Giorgio, M., Sard, M., Busto, E., et al., Assessment of individual radiosensitivity in human lymphocytes using micronucleus and microgel electrophoresis “Comet” assays, in Presentadoen: 11th International Congress on the International Radiation Protection Association, Madrid, 2004.
International Atomic Energy Agency Technical Reports Series № 405, Cytogenetic Analysis for Radiation Dose Assessment: a Manual, 2011, pp. 30—45.
Awa, A., Persistent chromosome aberrations in the somatic cells of A-bomb survivors, Hiroshima and Nagasaki, Radiat. Res., 1991, suppl. 1, pp. 265–274. https://doi.org/10.1269/jrr.32.Suppl_1.265
Stewart, F.A., Akleyev, A.V., Hauer-Jensen, M., ICRP Statement on Tissue Reactions / Early and Late Effects of Radiation in Normal Tissues and Organs—Threshold Doses for Tissue Reactions in a Radiation Protection Context, ICRP Publication 118, Ann. ICRP, 41(1/2), 2012.
Le Guen, B., Views on emerging scientific and societal issues, in Radiological Protection Individual Radiosensitivity and Screening Tests in the Workplace, Workshop on Science and Values in Radiological Protection, Helsinki, 2008. https://inis.iaea.org.
Workshop on Science and Values in Radiological Protection, Helsinki, 2008. https://inis.iaea.org.
Foray, N. and Colin, C., Bourguignon 100 years of individual radiosensitivity: how we have forgotten the evidence, Radiology, 2012, vol. 264, pp. 627–631.
Franco, N., Lamartine, J., Frouin, V., et al., Low-dose exposure to gamma rays induces specific gene regulations in normal human keratinocytes, Radiat. Res., 2005, vol. 163, pp. 623–635. https://doi.org/10.1667/RR3391
Morgan, W. and Sowa, M., Effects of ionizing radiation in nonirradiated cells, Proc. Natl. Acad. Sci. U.S.A., 2005, vol. 102, no. 40, pp. 14127–14128. https://doi.org/10.1073/pnas.0507119102
Rubanovich, A.V. and Khromov-Borisov, N.N., Genetic risk assessment of the joint effect of several genes: critical appraisal, Russ. J. Genet., 2016, vol. 52, no. 7, pp. 757–769. https://doi.org/10.1134/S1022795416070073
Sal’nikova, L.E., Chumachenko, A.G., Vesnina, I.N., et al., Analysis of genotypic dependence of chromosome aberration frequency in human lymphocytes irradiated in vivo and in vitro, Radiats. Biol., Radioekol., 2010, vol. 50, no. 3, pp. 340–344.
Mediko-biologicheskie i ekologicheskie posledstviya radioaktivnogo zagryazneniya reki Techa (Biomedical and Ecological Effects of Radioactive Contamination of the Techa River) Akleev, A.V. and Kiselev, M.F., Eds., Moscow: Medbioekstrem, 2001.
Degteva, M.O., Shagina, N.B., Tolstykh, E.I., et al., Calculations of individual dose from environmental exposures on the Techa river and EURT using TRDS-2016 for members of the TRC members, Urals Research Center for Radiation Medicine and Pacific Northwest National Laboratory, Final Report for Milestone 13, part 1, 2017. https://doi.org/10.1016/j.jenvrad.2017.08.013
Vozilova, A.V., Shagina, N.B., Degteva, M.O., and Akleyev, A.V., Chronic radioisotope effects on residents of the Techa River (Russia) region: cytogenetic analysis more than 50 years after onset of exposure, Mut. Res. Gen. Toxicol. Environ. Mutagen., 2013, vol. 756. https://doi.org/10.1016/j.mrgentox.2013.05.016
Akhmadullina, Yu.R., Radiosensitivity of peripheral blood T-lymphocytes in first-generation offspring whose fathers were exposed to chronic radiation, Extended Abstract of Cand. Sci. Dissertation, Mosk. Gos. Univ., Moscow, 2014.
Glantz, S.A., Primer of Biostatistics, New York: McGraw‑Hill, 1997, 4th ed.
Xu, B., Kim, S., Lim, D., and Kastan, M.G., Two molecularly distinct G2/M checkpoints are induced by ionizing irradiation, Mol. Cell. Biol., 2002, vol. 22, no. 4, pp. 1049–1059. https://doi.org/10.1128/MCB.22.4.1049-1059.2002
Le, M., Fernandez-Palomo, C., McNeill, F.E., et al., Exosomes are released by bystander cells exposed to radiation-induced biophoton signals: reconciling the mechanisms mediating the bystander effect, PLoS One, 2017, vol. 12(3). e0173685. https://doi.org/10.1371/journal.pone.0173685
Gorbunova, V. and Seluanov, A., DNA double strand break repair, aging and the chromatin connection, Mut. Res., 2016, vol. 788, pp. 2–6. https://doi.org/10.1016/j.mrfmmm.2016.02.004
Gately, D.P., Hittle, G.S., Chan, K.T., and Yen, T.J., Characterization of ATM expression, localization, and associated DNA-dependent protein kinase activity, Mol. Biol. Cell, 1998, vol. 9, pp. 2361–2374.
Khandogina, E.K., Study of genetic control of radiosensitivity, Russ. J. Genet., 2010, vol. 46, no. 3, pp. 257–264. https://doi.org/10.1134/S1022795410030014
Karahalil, B., Sardas, S., Kocabas, N., et al., Chromosomal aberrations under basal conditions and after treatment with X-ray in human lymphocytes as related to the GSTM1 genotype, Mut. Res., 2002, p. 515. https://doi.org/10.1016/S1383-5718(02)00003-7
Marcona, F., Andreoli, C., Rossi, S., et al., Assessment of individual sensitivity to ionizing radiation and DNA repair efficiency in a healthy population, Mut. Res., 2003, vol. 541. https://doi.org/10.1016/S1383-5718(03)00171-2
Sal’nikova, L.E., Chumachenko, A.G., Belopol’-skaya, O.B., and Rubanovich, A.V., Genetic and cytogenetic predictors of human chromosomal radiosensitivity, Radiats. Biol., Radioekol., 2013, vol. 53, no. 3, pp. 259–266. https://doi.org/10.21870/0131-3878-2018-27-2-46-61
Bouffler, S., Evidence for variation in human radiosensitivity: potential impact on radiological protection, ICRP Symposium, Seoul, 2015. https://doi.org/10.1177/0146645315623158
ACKNOWLEDGMENTS
We thank I.A. Chikireva and Z.I. Sychenko for technical support of the work.
Funding
This work was supported by the Federal Biomedical Agency of Russia.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest. The authors declare no conflict of interest.
Statement of compliance with standards of research involving humans as subjects. All procedures carried out in a study with the participation of people comply with the ethical standards of the institutional and/or national research ethics committee and the 1964 Helsinki Declaration and its subsequent changes or comparable standards of ethics. Informed voluntary consent was obtained from each of the participants in the study.
Additional information
Translated by I. Shipounova
Rights and permissions
About this article
Cite this article
Vozilova, A.V., Akhmadullina, Y.R. Study of the Individual Radiosensitivity in Humans Based on the Assessment of the Frequency of Chromosome Aberrations and Micronuclei in Peripheral Blood T Lymphocytes. Russ J Genet 55, 1234–1241 (2019). https://doi.org/10.1134/S1022795419100156
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S1022795419100156