Abstract
The abuse of antibiotics in therapy has lead to the development of resistance in the target organisms. The failure of presented antibiotics to control infections makes it essential to discover option to presently available drugs. Quorum sensing (QS) is a used by many bacteria to regulate gene expression in accordance with population density through the use of signal molecules or autoinducers. The QS is used by Bacteria populations to communicate and coordinate their group interactions, which is applied by pathogens in infection processes. The QS pathways in bacteria are composed of several parts, including bacteria populations, signal molecules, protein activators and target genes. The pathogenicity in numerous bacteria is regulated by QS signaling systems. The QS inhibition system may cause the reduction of virulence and defense against bacterial infections. The QS is the main regulator of virulence and biofilm formation in Pseudomonas aeruginosa and other relevant bacteria. In P. aeruginosa, the expression of many virulence factors appears to be controlled by QS. So, according to the role of this mechanism in the regulation and production of many virulence factors, the function of QS is required for P. aeruginosa to cause disease and infection. In this article, we discussed the QS mechanism in gram-negative and gram-positive bacteria with a closer look at the P. aeruginosa. A variety of plants showed their effects on P. aeruginosa virulence. Extract of various plants control the regulatory QS genes and factors with marginal effects on bacterial growth. The quorum-quenching (QQ) mechanisms are unrelated to static or cidal effects. In fact, anti-QS have already shown promise in the battle against P. aeruginosa infections.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Bacterial growth, virulence or pathogenic ability primarily depends on the ability of bacteria for cell-to-cell communication through a variety of signal molecules. This type of communication among or between bacteria is referred to as quorum sensing (QS). To defeat the difficulties of antibiotic therapy with resistant infections, new remedies are ever more crucial. Pseudomonas aeruginosa is a notorious bacterium due to its substantial virulence factors, affinity to form stubborn biofilm and the most prevalent cause of nosocomial infection like pneumonia, urinary tract (UT) infections and other pathogenic conditions. Along this P. aeruginosa is most radically showed increasing resistance towards antibiotics like imipenem, quinolones and cephalosporins etc [1]. To struggle against these infections a broad study on the novel antimicrobials is achieved. The current approaches against these infections are quorum sensing (QS) inhibition. The QS is not only a population-dependent fact by which bacteria make sense about their population solidity but also is a controller of diverse roles like luminescence, bioflim development, virulence factor production and many others. The disruption of bacterial cell-cell contact is identified to attenuate virulence, while restrictive selective strain toward bacterial resistance. Plants can make diverse antimicrobial substances like quinones, flavanones, phenolics, catechins, polyphenolics, alkaloids, terpenoids etc. Like antibiotics, these substances are aiming at killing of the pathogens and work via a specific mechanism like disrupting microbe cell membranes. However, plants have a different way of dealing with microbes for targeting microbe cell’s communication system. The intercellular communication in bacteria is identified as quorum sensing (QS). Anti-QS agents were first described in the red marine alga, Delisea pulchra [2] in a south Florida [3] and also present few higher plants [4, 5]. In this review we discussed to an ethnobotanically directed exploration for QS inhibiting agents in several medicinal plants for anti-QS action. The terrestrial plants not only generate autoinducer [6], a mimic to the bacterial QS system and respond to microbial signals [7, 8] and discussed about complications related to P. aeruginosa infection and the plants which could showed potentially novel therapeutic way for the treatment of P. aeruginosa infections. Some plants, Conocarpus erectus, Tetrazygia bicolor, Chamaesyce hypericifolia, Callistemon viminalis, Bucida buceras and Quercus virginiana have anti-QS effects using Chromobacterium violaceum and Agrobacterium tumefaciens NTL4 as biomonitors [9–12].
QUORUM SENSING
Quorum sensing (QS) is a population-dependent event [13]. The capability to sense the size of a bacterial population is arbitrated through small signaling molecules or autoinducers [14, 15]. These molecules are continually formed and received at a basal level by bacterial cells. There is an excess of signaling molecules in the surroundings, with high population density and the signals diffuse back into the cell where they ease the regulation of gene expression [14]. The QS systems are everywhere among bacteria and have present to control diverse functions like biofilm formation, luminescence, antibiotic and virulence factor formation, pigment formation, plant-microbe interactions and motility [16, 17]. Although there are a various different QS systems [18], the most broadly studied prototype is based on the Lux system of Vibrio fisheri and V. harveyi [19, 20]. This QS event engage a three part system: a liberally diffusible signal, a synthetase to make this signal, and a regulator that interacts in union with the signal to control gene expression.
The key signaling molecules formed by gram-negative bacteria are acyl-homoserine lactones (AHLs; Fig. 1) [21]. In V. fisheri, LuxI makes an AHL signaling molecule which connects to LuxR at a certain level [20, 22]. This level is reached only when enough bacteria are present (a quorum) to create sufficient amounts of the AHL [23–26]. The AHLs connect to LuxR (product of luxR) at a certain level and activate transcription of luxI and the luciferase genes [18]. AHL-mediated QS systems based on the LuxI/R pattern have been distinguished in human pathogens like P. aeruginosa [27], Yersinia pseudotuberculosis and Escherichia coli [28], and plant linked bacteria like Rhizobium leguminosarum [29], Erwinia carotovora and Ralstonia solanacearum [30]. In every cases QS systems can control virulence. Thus, the innovation of QS has given us a novel target or novel technique to attack and attenuate bacterial pathogenicity [31–34].
Mechanisms of QS Inhibition
There are numerous ways to inhibit cell-cell communication together with competitive inhibition, signal binding, signaling molecule degradation, and inhibition of upstream precursor or genetic regulation system [35]. These antagonists are based on the C12-AHL composition and cause a decline in LasR activity. AHL-antibodies developed to suppress QS during signal binding [36, 37]. A C12-AHL-protein conjugate was capable to reduce lasB expression, and a like molecule with greatly binding affinity for C12-AHL. Blocking S-adenosyl methionine (SAM) or the fatty acid precursors essential to synthesize AHLs leads to reduced formation of C12-AHL by LasI [38]. The genetic alteration of upstream regulators like Vfr and GacA has been shown to significantly reduce QS action and successive making of virulence factors [39]. Various bacteria with Bacillus sp., Arthrobacter sp., Variovorax paradoxus and A. tumefaciens create lactonases, enzymes that cleave and neutralize the lactone ring of various AHLs [40, 41]. Lactonase expression in P. aeruginosa, outcome in a considerable reduces in AHL making and virulence factor expression. The sensible use of anti-QS in drug resistant bacteria therapy is due to increased occurrence of drug failure due to the various pathogenic bacteria developing resistance to presently used antibiotics [42, 43].
Pseudomonas aeruginosa
Pseudomonas aeruginosa is a aerobic bacillus, gram-negative, with length and width ranges from 1.5–3.0 and 0.5–0.8 μm respectively. It is motile, single polar flagella, oxidase-positive, non-fermentative and non-sporulating species [44]. Other diagnostic features are beta-hemolysis of blood agar, pigment formation together with pyocyanin (blue-green), pyorubin (red-brown), pyoverdin (yellow-green), and a distinctive grape-like odor. It is an ubiquitous organism with the capability to colonize varied role due to its range of metabolic and resistance abilities to ecological faces [45].
Virulence Factors and Toxins
The pathogenicity of P. aeruginosa is a massive amount of secreted toxins and virulence factors (Fig. 2) like rhamnolipid, superoxide dismutase, HCN, exotoxin A, phospholipase C, exoenzyme, pyoverdin, pyocyanin, LasA protease and LasB elastase. Several of these factors cause or catalyze effects in the host leading to tissue necrosis and cell death. Pyoverdin, a yellow-green florescent pigment formed by P. aeruginosa to compete with mammalian transferrin for iron, the misuse of which really starves the host tissues [46]. It also encourages pathogenicity by exciting bacterial growth [47]. LasA and LasB are zinc metallo-endopeptidases, belong to the proteases family β-lytic endopeptidase enzyme. LasA has partial substrate specificity as contrast to LasB, however they activate in combination to degrade elastin, a key part in tissue plasticity. LasA cut elastin permitted it to be cleaving by LasB and other proteases. These proteases are capable of inactivating a extensive range of tissues and immunological agents [48, 49].
Pseudomonas aeruginosa Disease Association
Due to its virulence factors and affinity to form obstinate biofilms, P. aeruginosa is not one of the microbes implicated in nosocomial infections. The P. aeruginosa is the second most ordinary cause of nosocomial pneumonia (17% of isolated microbes), the third most frequent cause of urinary tract infections (11%), fourth in bacterial species dependable for nosocomial infections (9%) the fifth most frequent cause of surgical site infections (8%), and sixth most frequent isolated blood stream pathogens (3%) [1]. The P. aeruginosa has only augmented in occurrence and antibiotic resistance and created a exact threat for vulnerable patients. The P. aeruginosa has the capability to colonize various diverse infection sites when the host immune system is compromised (Table 1). This can happen in patients with a severe basic condition like AIDs, cancer, burn wounds, immune suppression from surgery, organ transplant [50, 51]. Neonates are also very vulnerable to P. aeruginosa infection due to their immature immune system [52]. P. aeruginosa enter the body by any orifice and minor infections, can progress into severe and critical infections. In the ophthalmological system, P. aeruginosa can colonize and infect the cornea, aqueous humors and vitreous humors, or nearby structures after cataract or curative surgery. P. aeruginosa has been linked with a rising number of cases of contact lens-related kerititis [53]. Infections can growth rapidly from minor conjunctivitis or kerititis to scleral wounds and corneal ulcers due to cell lysis by P. aeruginosa extracellular enzymes. The P. aeruginosa also colonizes in the auditory canal and cause minor otitis externa to inner ear problems (otitis media) [54]. Lacking proper handling secondary infections of the nearby bones (mastoiditis) or neurological structures can happen [55–58].
Distraction of the gastrointestinal (GI) system often happens in pediatric patients or those with neutropenia or blood linked disorders [59]. Colonization in the gastro-intestine can range from diarrhea to severe rectal wounds and necrotizing enterocolitis in patients. Urinary tract infections (UTIs) are general due to regular catheterization and the existence of drug resistant bacteria [60]. If left unrestricted, these infections can lead to kidney disorders and renal failure. Proximal bone infections like osteomylitis of the lumbosacral vertebrae and pelvis can happen as a secondary hurdle to UTIs [61]. The P. aeruginosa infection can also happen by an scrape or break in the skin, due to wound, surgery, catheterization and dermatological conditions like dermatitis or folliculitis [62] to life threatening cases of cellulitis or necrotizing fascitis. Infections with deep tissue injure particularly in burning state can extend to the bloodstream causing bacteremia and septicemia [44]. Blood borne P. aeruginosa can go to the heart causing endo- and pericarditis. Complications in the pulmonary system can start as sinusitis or an upper respiratory tract infection and lead to pneumonia, bronchitis, or pulmonary lesions. Infections of the sinuses can also cause meningitis and cerebral lesions due to the nearness to the brain.
Current Treatment Procedures
The current treatment procedures can vary greatly since a patient may be infected with one or more drug resistant P. aeruginosa strains. Therapeutic tactics to treat infections include use of a single antibiotic or combination of two or three antibiotics drugs. Monotherapy has normally dealing with β-lactam antibiotics like penicillins, cephalosporins, or newer β-lactams like imipenem and meropenem. These antibiotics act by interfere with the production of peptidoglycan into bacterial cell walls. Unfortunately, P. aeruginosa has evolved an efficient way of inactivating these drugs which led to the progress of novel approach for the treatment [63].
Anti-pseudomonal mixtures include combinations of a β-lactam like aztreonam, ticarcillin or ceftazidime plus a β-lactamase inhibitor like sulbactam, and aminoglycoside antibiotic like tobramycin or amikacin. Aminoglycosides are interfering with protein production by binding to the 30S ribosomal subunit of the bacterial cells. Combinations of ceftazidime and fluoroquinolone like ciprofloxacins are also effective. The quinolones are exhibiting their bactericidal action by blocking DNA replication through inhibition of gyrase [64]. Option combinations include pairing ciprofloxacin with animoglycoside or with the broad-spectrum antibiotic fosfomycin, which prevent cell wall formation by inhibiting production of N-acetylmuramic acid [65]. Even though there are a few achievements in eliminating P. aeruginosa with these treatments, many patients need continuing treatment and toxicity can extend with recurrent use. There is an rising trend of antibiotic resistance that will quickly provide these therapeutics uselessness.
Antibiotic Resistance in Pseudomonas aeruginosa
Antibiotic resistant P. aeruginosa infections are rising. 21.1% of the nosocomial infections were imipenem resistant and enhance of 15% over the previous five years (1998–2002). Similarly, 29.5% of P. aeruginosa infections were resistant to quinolones and 31.9% were resistant to cephalosporins; raises of 9 and 20% over the previous five years respectively [1]. The encouragement of antibiotic resistance, either through overuse and successive mutation or via gene transfers. The more recently acquired resistance mechanisms P. aeruginosa has several factors that are measured intrinsic. The pathogenic strains of P. aeruginosa possess creative mechanisms which give to reduced antibiotics vulnerability including:
A. Biofilm development
B. Restricted surface accessibility
C. Exclusion via efflux pumps
D. Enzymatic inactivation of antibiotics
E. Modification of target proteins
The planktonic method of bacterial growth is often studied, the most of bacteria survive in nature as component of a surface-adherent, matrix-enclosed biofilm [11]. P. aeruginosa is not an exception to this rule, and some strain of it can control to a mucoid phenotype through infections [63]. Owing to the secretion of an exopolysaccharide, biofilm cells form a slime layer in which they are permanently bound to a substratum and to each other [66]. This protected pattern results in changed growth rates, transcription patterns, and prominently, an improved ecological resistance from that of their planktonic counter parts [67]. Antimicrobials are prohibited from getting the innermost cells of a biofilm and are therefore incapable to completely eliminate the infection [68]. The alginate layer of mucoid P. aeruginosa avoids optimal host immune role by masking antibody opsonization and inhibiting clearance [69]. The latter is accomplished by promoting permanent adherence of the bacteria to lung epithelial cells [70–72].
Pseudomonas aeruginosa QS Specifics
Complexity in treating obstinate infections and the growing resistance to antibiotics, new remedial tactics are becoming more necessary. Targeting the QS system of P. aeruginosa, one of the main complicated pathogens in the lung, is a original plan of attack. This arrangement is a key controller of pathogenicity in P. aeruginosa and other relevant bacteria, thus inhibition of QS may cause decrease of virulence and defend against infections [73, 74]. The QS system of P. aeruginosa is based on the luxI–luxR prototype. This complicated QS communication system is reflected in various gram-negative bacteria, where it manages regulation of virulence, with biofilm creation, motility, and toxin creation [75]. P. aeruginosa complicated two main sets of QS systems: lasI–lasR and rhlI–rhlR [41]. The LuxI homologues, LasI and RhlI are synthetases that produce the autoinducer signaling molecules N-butanoyl-L-homoserine lactone (BHL), and N-(3-oxododecanoyl)-L-homoserine lactone (OdDHL) respectively [76]. These signaling molecules diffuse out into the environment and, upon reaching a supposed threshold meditation, activate receptors lasR and rhlR [77]. These receptors, coordinate directive of pathogenicity through transcriptional activation of various virulence factors [78, 79]. A third signal, PQS (Pseudomonas Quinolone Signal) plays an essential role in the QS system and is concerned in the creation of N-(3-oxohexanoyl)-L-homoserine lactone (OHHL) [75, 77]. This secondary metabolite of P. aeruginosa is included into the QS hierarchy in times of cell stress, and interfering with this signal has been shown reduce virulence factor phrase [80] and a fourth system exists regulated by cyclic dipeptides (DKPs) [81]. This study focuses on the las and rhl systems [82]. The superfluous and auto-regulatory nature of the QS system is fairly complex [83], the P. aeruginosa QS hierarchy suggests that las controls rhl with virulence proteins [41]. The virulence factors LasA (staphylolytic protease) and LasB (elastase) are under control of the lasI/R system [84], however rhlI/R also controls effect to a lesser amount [85]. Pyoverdin is under rhlI/R control [85], whereas biofilm formation is partially under QS control [67]. The las–rhl system also falls under the umbrella of various “global” regulators like Vfr (homologue of E. coli cAMP receptor protein, CRP) [39] or GacA (sRNA binding protein) [78]. Control from these genes also influence downstream virulence and thus to inhibit pathogenicity and a therapeutic agent could display an effect directly on the las/rhl system or the PQS or DKP pathways. The halogenated furanones inhibit P. aeruginosa both in vitro and in a murine models [86, 87]. These compounds act by transferring the signaling molecule from its receptor, thus accelerate receptor turnover [88.89]. They also have persuade on siderophore biosynthesis [90].
ETHNOPHARMACOGNOSY: LOOKING TO THE PAST FOR EXPLANATION OF THE FUTURE
The excess use of antibiotics began a rising tendency of resistance in various pathogens. Even though combinatorial and synthetic chemistry can offer us with some clarification for infectious diseases, various medicinal compounds already present in nature and are pending to detection [91–93]. The high biological range is a possible linked to high chemical multiplicity, allow for the development of many toxic and bioactive plant substances. Plants create precise compounds to provide desires like reproduction and defense [3, 9, 76]. Plants have evolved toxic and bioactive substances to defend against herbivores and pathogen attacks [94] because plants have relied more heavily on chemical defenses than motile organisms. In lots of cases, the connection between toxin and medicine is dosage, and numerous plant toxins have originate their way into pharmacopoeia, example, foxglove or Digitalis spp.; if ingested, can generate convulsions, bradycardia, cerebral disturbances and eventual death [95]. Though, at the correct dosage, the cardiac glycosides digoxin and digitoxin have effective in the treatment of atrial fibrillation and heart failure [96].
Advantages of a Directed Search
Various plants with chemical variety are the basis for testing medicinal compounds [97]. Though, unite these natural qualities of plants make even better place in search for new drugs. Most plants have some type of constitutive or inducible resistance against pathogens, but plants used medicinally may also have chemical defenses to human pathogens [98].
Relating Traditional and Modern Medicines
Expressive the traditional use of the plants can guides drug discovery and giving an idea of its potential use in the society. For example, plants used as snakebite medication may be useful in discovery hypotensive drugs. If an individual wants to survive the bite of a snake, it is beneficial to lower the blood pressure and slow the heart rate so as to not reach the venom or poison to susceptible organs before it could be metabolized. This led to the finding of hypotensive alkaloids in Rauwolfia (Apocynaceae) spp.; [99]. Ethnopharmacology is beneficial to traditional medicinal societies and support to modern scientific methods to help and improve healthcare in rural areas. The ethno-pharmacology study would begin with the cultural anthropology of a group and their medical system in the context of culture and include local medical data to avoid loss of information to upcoming generation. The botanical, chemical, and pharmacological studied of the plants give potentially useful and unique medicinal drugs. Each of these parts (botany, anthropology, pharmacology and chemistry) could take time to fully explore. Thus, most studies focused on aspect of ethnopharmacology depending on the expertise and interests of the investigators.
Botanicals as Anti-Bacterial Therapies
Various ethno-botanical explored for antibacterials, confirmed not only the requirement for drugs but also the various plant species that used for bacterial circumstances [100]. While medicinal plant researches have led to the discovery of various key drugs like morphine, quinine, camptothecin and paclitaxel, there is not a huge degree of overlap between generally used plant drugs and antimicrobials [101–105].
Tea Tree Oil
Melaleuca alternifolia Cheel (Myrtaceae)/tea tree is an aromatic tree. The essential oil of M. alternifolia is a topical antimicrobial, its activity has attributed to terpinen-4-ol, a main mono-terpenoid of the oil [10]. Other terpene constituents include γ-terpinene, α-terpineol, cineole and p-cymene [99]. Monoterpenoids are present mainly in plants with volatile oils like those in the Lamiaceae, Myrtaceae, and Rutaceae. These compounds causes membrane disruption in bacteria [100].
Oregano Oil
Origanum vulgare L. (Lamiaceae) is a herb, essential oil fraction is effective against bacterial and fungal infections in gastrointestinal and genitourinary tract [106, 107]. Its antimicrobial activity is recognized to the phenolic monoterpenoids, carvacrol and thymol, along with various other terpene alcohols, phenols and sesquiterpenes [108]. The two main chemotypes of O. vulgare showed either high thymol or high carvacrol substance [108], both are antimicrobial [100], though the latter is more effective [109]. The antimicrobial effect is due to membrane disruption [109] Oil of oregano has shows antibacterial effect against Helicobacter pylori, a causative agent of gastric ulcers [107], and a various clinically isolated pathogens including Haemophyllus influenzae, Staphylococcus aureus, E. coli, Streptococcus pneumoniae, and Enterobacter cloacae [110] and also effect in vitro against C. albicans.
Myrrh
Myrrh is a oleo-gum resin of Commiphora Jacq. species of Buseraceae family. It contained mainly aromatic peeling bark. Commiphora bark is achieved to collect the resin and has religious and medicinal use [100, 106]. It is usually used in mouthwashes and toothpastes due to its antimicrobial effects. Myrrh consists of about 30–60% water soluble gum, 20–40% alcohol soluble resin and 8% volatile oils. The volatile oils fraction contains antimicrobial mono-terpenes like α-camphorine, myrcene and also furanosesesquiterpenes. The antibacterial effects of Commiphora mulkul (Commiphora wightii (Arn.) Bhandari) was showed in vitro antibacterial effect against various gram-positive and gram-negative bacteria [111]. It is also used for topically on wounds and oral and pharyngeal mucosa as a mouthwash [106].
UNUSED POTENTIAL OF PLANTS FOR ANTIMICROBIAL ACTION
Plants are great source of antimicrobial agents. In fact, about 75% of the antibiotics are derived from the actinomycetes (group of gram-positive bacteria) [112]. Antibiotic-creating microbes possess genes which defend them from the toxic property of these compounds. It is easy for microbe to acquire antibiotic resistance through plasmid transfer or transposons. Plants are genetically dissimilar from the organisms they are trying to eradicate. There is small chance for a microbe to gain resistance from a plant. Plants produce a multitude of diverse antimicrobials like phenolics, flavanones, catechins, quinones, alkaloids, polyphenolics, and terpenoids [100]. Like antibiotics, these agents are targeted at killing the pathogen and work via a non-species specific means like disrupting microbial cell membranes. Plants have other way of deal with microbes-targeting cell’s communication system or QS [12]. Breakdown of this system causes an attenuation of microbial pathogenicity [87]. The discovery of anti-QS agents in plants provides us with yet another type of antimicrobial agents.
ANTI-QUORUM SENSING FROM ETHNOBOTANICALS
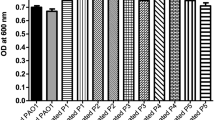
The discovery of compounds that inhibit QS, could provide a novel method of combating infection [42]. Anti-QS agents were first depicted in the red marine alga Delisea pulchura. This alga has anti-fouling property and contains halogenated furanones which block AHLs via competitive inhibition and destabilization of LuxR. The structural similarity allows furanones to competitive inhibit the effect of AHL signaling molecules [89]. The QS inhibition defends themselves from attack by other microbes. Plant (Table 2), bacteria, fungi could produce compound which interfere the QS-regulated gene expression in pathogenic microbes [113, 114]. Since the discovery of AHL inhibitors in D. pulchura, anti-QS activity has found in Caulerpa species and various higher plants including fruits and vegetables [115–117]. Pisum sativum (pea) seedlings and root exudates formed an inhibition of pigment production, exochitinase effects and protease activity in C. violaceum [116]. Carrot (Daucus carota), chamomile (Matricaria sp.), garlic (Allium sativum), water lily (Nymphaea sp.) and various peppers (Capsicum spp.) were possess anti-QS activity against a luxI-gfp reporter strain. Toluene extracts of garlic exhibited anti-QS activity against gram-negative transcriptional regulators Lux R or Las R [114]. Garlic was also inhibit biofilm formation in P. aeruginosa, and prevented nematode death [115]. Garlic and several plants extract like Thymus vulgaris also reported to increase killing effect against Pseudomonas species and shown anti-QS activity [117, 118]. Rosmarinic acid excreted from the root of sweet basil, is a caffeic acid ester has inhibitory actions on Pseudomonas species and interfere with QS activity and bioflim formation [119]. Various fruits and herbs were possess anti-QS activity in a C. violaceum strain and on the swarming motility of E. coli and P. aeruginosa [117].
Fruits like blueberry, raspberry, blackberry, cranberry, grape, and herbs like ginger, oregano, kale and turmeric exhibited moderate anti-QS actionv. Other than signal mimics like furanones, ellagic acid, tannic acid, and epigallocatechin gallate have shown anti-QS action in both an E. coli and P. aeruginosa strain [120]. The polyphenolics should be explored as anti-QS compounds. The antipathogenic anti-QS effects were exhibited with Laurus nobilis leaves, fruits, flowers and bark extracts. The S. oleraceus exhibited prominent anti-QS activity, almost equals to L. nobilis extracts. Rosmarinus officinalis leaves and Tecoma capensis leaves had moderate anti-QS activity. Weak anti-QS effects were observed with extracts of Populus alba (leaves), Jasminum sambac (flowers and leaves) and Populus nigra. Day by day anti-QS effects of several extract of natural plants extracts have been reported. Hexane extract of clove bud (Syzygium aromaticum) has significant anti-QS action on two P. aeruginosa strains [121, 122]. Capparis spinosa traditionally used in Italy, posses’ antibacterial activity [123], methanolic extract of fruit of C. spinosa showed anti-QS activity on P. aeruginosa PAO1 strain [124]. Methanolic extract of the Myristica cinnamomea bark also have anti-QS action [125]. Lagerstroemia speciosa, known as ‘jarul’ prevalent in south-east Asia, revealed that this plant can modulated the QS of micro organism specially P. aeruginosa.Lagerstroemia speciosa can attenuate QS-related genes (las andrhl) and their particular signalling molecules like N-acylhomoserine lactones, but interestingly not affecting their growth by using a specific strain P. aeruginosa PAO1. Significant inhibition of virulence factors: LasA protease, LasB elastase, and pyoverdin production, was also reported [126]. Extract of Melicope lunu-ankenda edible plant of Malasyia, shown proficient anti-QS against P. aeruginosa PAO1. Some Chinese traditional system of medicine like Cnidium monnieri, Angelica sinensis, Astragalus membranaceus, Aloe barbadensis, Lilium brownii, Crataegus cuneata, Dioscorea nipponica, Magnolia officinalis, Ephedra were showed activity against pathogenic microbes like C. violaceum and P. aeruginosa [127–130].
QUORUM SENSING AS DRUG TARGET
The importance of the qourum sensing (QS) in controlling pathogenicity of bacteria such as P. aeruginosa, a new generation of antibiotics can be imagined which are designed based on the inhibition of QS system. These inhibitors can be used as a synergism with other drugs to reduce their dose. Biofilm that causes resistance against many normally used antibiotics is regarded as one of the main challenges in treatment. The QS system plays a fundamental role in the regulation, control and formation of biofilm and many virulence factors. So, it is possible that the inhibition of QS regulatory process for removing and reducing the drug resistance in infectious bacteria to be effective. The genes under the control of P. aeruginosa QS system were investigated 388, 315 and 163 genes in the bacterial genome. The bacteria QS system had been inactivated by mutation and the gene induction was controlled by foreign autoinducers. The gene activity in the presence or absence of autoinducer, 97 genes were reported that jointly are controlled by the QS system. About 10% of the bacterial genomes are under the control of QS system. Therefore, it was suggested that the bacterial QS system can be considered as a suitable target in order to research about the control of bacterial infection [131–134]. This goal can be achieved using several methods (Fig. 1) including: (I) The blockage of R proteins activation by AHL antagonists or AHL antibodies and AHL degredation by chemical or enzymic destruction; (II) The metabolism inhibition of AHL by compounds that can compete with substrates which are used in the synthesis of autoinducers; (III) Inhibition of regulatory factors that have a positive effect on QS genes; (IV) Using antisense oligos against main genes of the QS system [135–137].
Quorum Sensing Signals as Biosensor Markers
The QS signals can be used as markers for the presence of pathogenic bacteria in clinical and environmental samples by bacterial whole-cell QS biosensors. These biosensors are composed of two main parts: a plasmid constructs containing an AHL-responsive transcriptional regulator, relatory promoter, reporter gene; and bacterial host cell. QS-deficient mutants can be developed by pathogenic bacteria after colonization in the host, so QS signals should not be used as the only inputs for microbial biosensors, but can be used for detection of pathogenic bacteria in contaminated environments and products such as ground water, dairy, and meat products [138–140].
Quorum Sensing Signals and Anticancer Therapy
The 3-oxo-C12-HSL QS signal of P. aeruginosa inhibits proliferation and induces apoptosis in human breast cancer cell and considered as an anticancer drug. This feature may be prevented due to some side effects, for example 3-oxo-C12-HSLcan lead to macrophage apoptosis. Nevertheless, this QS signal is a good starting point for developing synthetic AHL homologs with anticancer toxicity and reducing side effects [136, 138]. Studies in mouse models have shown that some bacteria such as E. coli, Bifidobacterium longum, and attenuated strains of Vibrio cholerae, Salmonella typhimurium, and Listeria monocytogenes have a tendency to localization and prolifration in solid tumors and metastases, perhaps through immune system surveillance, which provides barrier against the host immune system [138, 140]. The bacterial aggregation can be used to produce biosensors that target cancer cells which can be achieved by designing synthetic genetic circuits to recognize cancer microenvironment conditions or cancer cell surface antigenes [141]. A genetic network was developed in E. coli in which the Yersinia pestis invasin gene was regulated by the V. Fischeri LuxI/R system. Followed by high HSL levels, invasin will expresse and allows E. coli to bind and invade mammalian cancer-derived cells displaying β1-integrin cell surface receptors. So, whole-cell QS biosensors and gene delivery vehicles can be designed to recognize cancer cell aggregations in vivo [142].
Quorum Quenching and Biological Control
The application of quorum quenching (QQ) strategy may be an alternative approach to control bacterial pathogens which employ the AHL based QS mechanism to regulate pathogenicity. The strategy includes several methods to achieve an artificially increased level of AHLs such as the introduction of a gene coding AHL synthase directly to the plant cells, the employment of AHL-degrading bacteria to protect plants and heterologous expression of genes encoding AHL-degrading enzymes in pathogen cells or in plant tissue. Therefore, bacteria misinterprete the population size and the misinterpretation leads to the production of virulence determinants long before the pathogen population is large enough to sustain infection [143]. Several studies showed that the application of bacterial cells producing AHL degrading enzymes can be as biological control agents of plant bacterial diseases. The first example of such purposeful usage for the attenuation of infection symptoms development in plants was transgenic potato and tobacco plants expressing the gene encoding AiiA lactonase manifested strong resistance against infection by P. carotovorum subsp. carotovorum. Heterologous expression of the aiiA gene encoding the AiiA lactonase from Bacillus sp. in plant pathogens cells P. carotovorum, Burkholderia thailandensis and Erwinia amylovora diseased symptoms development. In order to silence QS system of P. aeruginosa, the same approach was used to reduce 3-oxo-C12- HSL followed by preventing the accumulation C4-HSL. This result was also observed by addition of purified AhlM protein to the growth medium of P. aeruginosa. Consequently, the AHL degrading enzymes together with QS inhibitors may be successfully be applied to disrupt bacterial cell to cell communication and to control bacterial infections [144].
CONCLUSION
The plants are used as a source of different types of compounds. These natural agents can be used as antipathogenic agents, mainly focused on antibacterial effects. Focus on to anti-QS and anti virulence property that may reveal quorum-quenching (QQ) compounds from plants for provide a novel method for the treatment of infections against resistant microbial strains particularly against P. aeruginosa. The actions of the plant extracts on P. aeruginosa are very complicated and perhaps beyond the area of the QS control hypothesis. The failure of accessible antibiotics to control infectious and makes it critical to find options to presently used drugs. The pathogenicity in numerous bacteria is regulated by QS that is the key regulator of virulence and biofilm construction in P. aeruginosa and other bacteria. Various plants extracts were showed effects on P. aeruginosa virulence factors and the QS has significant inhibition of LasA protease, LasB elastase, pyoverdin and biofilm formation. In fact, anti-QS approach has shown promise in the combat against P. aeruginosa infections. However, the decrease of QS gene expression and signaling molecule levels and effect on virulence factor formation offer these plants were used in the future to combat P. aeruginosa and other bacterial infections.
REFERENCES
Centers for Disease Control and Prevention, H.I.P. National Nosocomial Infections Surveillance (NNIS) Report, data summary from January 1992–June 2004, issued October 2004: a report from the NNIS System, Am. J. Infection Control., 2004, vol. 32, pp. 470–485.
Manefield, M., Rasmussen, T.B., Henzter, M., Andersen, J.B., Steinberg, P., Kjelleberg, S., and Givskov, M., Halogenated furanones inhibit quorum sensing through accelerated LuxR turnover, Microbiology, 2002, vol. 148, pp. 1119–1127.
Cumberbatch, A., Characterization of the Anti-Quorum Sensing Activity Exhibited by Marine Macroalgae of South Florida, Miami: Florida International University, Department of Biological Sciences, 2002.
Bjarnsholt, T., Jensen, P.O., Rasmussen, T.B., Christophersen, L., Calum, H., Hentzer, M.H., Hougen, P., Rygaard, J., Moser, C., Eberl, L., Hoiby, N., and Givskov, M., Garlic blocks quorum sensing and promotes rapid clearing of pulmonary Pseudomonas aeruginosa infections, Microbiology, 2005, vol. 151, pp. 3873–3880.
Gao, M., Teplitski, M., Robinson, J.B., and Bauer, W.D., Production of substances by Medicago truncatula that affect bacterial quorum sensing, Mol. Plant Microbe Interact., 2003, vol. 16, pp. 827–834.
Yoon, Y. and Sofos, J.N., Absence of association of autoinducer-2-based quorum sensing with heat and acid resistance of Salmonella,J. Food Sci., 2010, vol. 75, pp. 444–448.
Adonizio, A.L.K., Downum, B.C., Bennett, and Mathee, K., Antiquorum sensing activity of medicinal plants in southern Florida, J. Ethnopharmacol., 2006, vol. 103, pp. 427–435.
Bauer, W.D. and Mathesius, U., Plant responses to bacterial quorum sensing signals, Curr. Opin. Plant Biol., 2004, vol. 7, pp. 429–433.
Carson, C.F., Riley, T.V., and Cookson, B.D., Efficacy and safety of tea tree oil as a topical antimicrobial agent, J. Hosp. Infect., 1998, vol. 40, pp. 175–178.
Carson, C.F. and Riley, T.V., Antimicrobial activity of the major components of the essential oil of Melaleuca alternifolia,J. Appl. Bacteriol., 1995, vol. 78, pp. 264–269.
Costerton, J.W., Lewandowski, Z., Caldwell, D.E., Korber, D.R., and Lappin-Scott, H.M., Microbial biofilms, Ann. Rev. Microbiol., 1995, vol. 49, pp. 711–745.
Bauer, W.D. and Tepletski, M., Can plants manipulate bacterial quorum sensing?, Aust. J. Plant Physiol., 2001, vol. 28, pp. 913–921.
Nealson, K.H., Platt, T., and Hastings, J.W., Cellular control of the synthesis and activity of the bacterial luminescent system, J. Bacteriol., 1970, vol. 104, pp. 313–322.
Hastings, J.W. and Greenberg, E.P., Quorum sensing: The explanation of a curious phenomenon reveals a common characteristic of bacteria, J. Bacteriol., 1999, vol. 181, pp. 2667–2668.
Schauder, S. and Bassler, B.L., The languages of bacteria, Genes Dev., 2001, vol. 15, pp. 1468–1480.
McClean, R.J.C., Pierson, I., Leland, S., and Fuqua, C., A simple screening protocol for the identification of quorum signal antagonists, J. Microbiol Methods, 2004, vol. 58, pp. 351–360.
Rasmussen, T.B., Manefield, M., Andersen, J.B., Eberl, L., Anthoni, U., Christophersen, C., Steinberg, P., Kjelleberg, S., and Givskov, M., How Delisea pulchra furanones affect quorum sensing and swarming motility in Serratia liquefaciens MG1, Microbiology, 2000, vol. 146, pp. 3237–3244.
Henke, J.M. and Bassler, B.L., Bacterial social engagements, Trends Cell Biol., 2004, vol. 14, pp. 648–656.
Bassler, B.L., Wright, M., Showalter, R.E., and Silverman, M.R., Intercellular signalling in Vibrio harveyi: Sequence and function of genes regulating expression of luminescence, Mol. Microbiol., 1993, vol. 9, pp. 773–786.
Stevens, A. and Greenberg, E., Quorum sensing in Vibrio fischeri: Essential elements for activation of the luminescence genes, J. Bacteriol., 1997, vol. 179, pp. 557–562.
Fuqua, C. and Greenberg, E.P., Self perception in bacteria: Quorum sensing with acylated homoserine lactones, Curr. Opin. Microbiol., 1998, vol. 1, pp. 183–189.
Whitehead N.A., Barnard A.M., Slater H., Simpson N.J., Salmond G.P. Quorum-sensing in gram-negative bacteria, FEMS Microbiol. Rev., 2001, vol. 25, pp. 365–404.
Cao, M., Feng, Y., Wang, C., Zheng, F., Li, M., Liao, H., Mao, Y., Pan, X., Wang, J., Hu, D., Hu, F., Tang, J., Functional definition of LuxS, an autoinducer-2 (AI-2) synthase and its role in full virulence of Streptococcus suis serotype 2, J. Microbiol., 2011, vol. 49, pp. 1000–1011.
Halliday, N.M., Hardie, K.R., Williams, P., Winzer, K., and Barrett, D.A., Quantitative liquid chromatography-tandem mass spectrometry profiling of activated methyl cycle metabolites involved in LuxS-dependent quorum sensing in Escherichia coli,Anal. Biochem., 2010, vol. 403, pp. 1–2.
Hagen, S.J., Son, M., Weiss, J.T., and Young, J.H., Bacterium in a box: Sensing of quorum and environment by the LuxI/LuxR gene regulatory circuit, J. Biol. Phys., 2010, vol. 36, pp. 317–327.
Sperandio, V. and Sdi, A., Sensing of acyl-homoserine lactones by enterohemorrhagic E. coli (EHEC) serotype O157:H7 in the bovine rumen, Gut Microbes, 2010, vol. 1, pp. 432–435.
Pesci, E., Pearson, J., Seed, P., and Iglewski, B., Regulation of las and rhl quorum sensing in Pseudomonas aeruginosa,J. Bacteriol., 1997, vol. 179, pp. 3127–3132.
Surette, M.G. and Bassler, B.L., Quorum sensing in Escherichia coli and Salmonella typhimurium,Proc. Natl. Acad. Sci. U. S. A., 1998, vol. 95, pp. 7046–7050.
Rodelas, B., Lithgow, J.K., Wisniewski-Dye, F., Hardman, A., Wilkinson, A., Economou, A., Williams, P., and Downie, J.A., Analysis of quorum-sensing-dependent control of rhizosphere-expressed (rhi) genes in Rhizobium leguminosarum bv. viciae, J. Bacteriol., 1999, vol. 181, pp. 3816–3823.
Von Bodman, S.B., Bauer, W.D., and Coplin, D.L., Quorum sensing in plant-pathogenic bacteria, Ann. Rev. Phytopathol., 2003, vol. 41, pp. 455–482.
Fuqua, C. and Greenberg, E., Listening in on bacteria: Acyl-homoserine lactone signaling, Nat. Rev. Mol. Cell. Biol., 2002, vol. 3, pp. 685–695.
Fuqua, W.C., Winans, S.C., and Greenberg, E.P., Quorum sensing in bacteria: The LuxR–LuxI family of cell density-responsive transcriptional regulators, J. Bacteriol., 1994, vol. 176, pp. 269–275.
Dong, Y.H., Wang, L.H., Xu, J.L., Zhang, H.B., Zhang, X.F., and Zhang, L.H., Quenching quorum-sensing-dependent bacterial infection by an N-acyl homoserine lactonase, Nature, 2001, vol. 411, pp. 813–817.
Cha, C.G.P., Chen, Y.C., Shaw, P.D., and Farrand, S.K., Production of acyl-homoserine lactone quorum-sensing signals by gram-negative plant-associated bacteria, Mol. Plant Microbe Interact., 1998, vol. 11, pp. 1119–1129.
Smith, R.S. and Iglewski, B.H., Pseudomonas aeruginosa quorum sensing as a potential antimicrobial target, J. Clin. Invest., 2003, vol. 112, pp. 1460–1465.
Smith, R.S. and Iglewski, B.H., Pseudomonas aeruginosa quorum-sensing systems and virulence, Curr. Opin. Microbiol., 2003, vol. 6, pp. 56–60.
Debler, E.W., Kaufmann, G.F., Kirchdoerfer, R.N., Mee, J.M., Janda, K.D., and Wilson, I.A., Crystal structures of a quorum-quenching antibody, J. Mol. Biol., 2007, vol. 368, pp. 1392–1402.
Hoang, T.T., Sullivan, S.A., Cusick, J.K., and Schweizer, H.P., beta-Ketoacyl acyl carrier protein reductase (FabG) activity of the fatty acid biosynthetic pathway is a determining factor of 3-oxo-homoserine lactone acyl chain lengths, Microbiology, 2002, vol. 148, pp. 3849–3856.
Albus, A., Pesci, E., Runyen-Janecky, L., West, S., and Iglewski, B., Vfr controls quorum sensing in Pseudomonas aeruginosa,J. Bacteriol., 1997, vol. 179, pp. 3928–3935.
Dong, Y.H. and Zhang, L.H., Quorum sensing and quorum-quenching enzymes, J. Microbiol., 2005, vol. 43, pp. 101–109.
Schuster, M. and Greenberg, E.P., A network of networks: Quorum-sensing gene regulation in Pseudomonas aeruginosa,Int. J. Med. Microbiol., 2006, vol. 296, pp. 73–81.
Hentzer, M. and Givskov, M., Pharmacological inhibition of quorum sensing for the treatment of chronic bacterial infections, J. Clin. Invest., 2003, vol. 112, pp. 1300–1307.
Whitehead, N.A., Welch, M., and Salmond, G.P.C., Silencing the majority, Nat. Biotechnol., 2001, vol. 19, pp. 735–736.
Bodey, G.P., Bolivar, R., Fainstein, V., and Jadeja, L., Infections caused by Pseudomonas aeruginosa,Rev. Infect. Dis., 1983, vol. 5, pp. 279–313.
Vasil, M.L., Pseudomonas aeruginosa: Biology, mechanisms of virulence, epidemiology, J. Pediatrics, 1986, vol. 108, pp. 800–805.
Meyer, J., Neely, A., Stintzi, A., Georges, C., and Holder, I., Pyoverdin is essential for virulence of Pseudomonas aeruginosa,Infect. Immun., 1996, vol. 64, pp. 518–523.
Cox, C.D. and Adams, P., Siderophore activity of pyoverdin for Pseudomonas aeruginosa,Infect. Immun., 1985, vol. 48, pp. 130–138.
Choi, Y., Park, H.Y., Park, S.J., Kim, S.K., Ha, C., Im, S.J., and Lee, J.H., Erratum to: Growth phase-differential quorum sensing regulation of anthranilate metabolism in Pseudomonas aeruginosa,Mol. Cells, 2011, vol. 32, p. 597.
Kessler, E., Beta-lytic endopeptidases, Methods Enzymol., 1995, vol. 248, pp. 740–756.
Krcmery, V., Koprnova, J., Gogova, M., Grey, E., and Korcova, J., Pseudomonas aeruginosa bacteraemia in cancer patients, J. Infect., 2006, vol. 52, pp. 461–463.
Meynard J.L., Barbut F., Guiguet M., et al., Pseudomonas aeruginosa infection in human immunodeficiency virus infected patients. J. Infect., 1999, vol. 38, pp. 176–181.
Foca, M.D., Pseudomonas aeruginosa infections in the neonatal intensive care unit, Semin. Perinatol., 2002, vol. 26, pp. 332–339.
Robertson, D.M., Petroll, W.M., Jester, J.V., and Cavanagh, H.D., Current concepts: Contact lens related Pseudomonas keratitis, Contact Lens Anterior Eye, 2007, vol. 30, pp. 94–107.
Roland, P.S., Chronic suppurative otitis media: A clinical overview, Ear Nose Throat J., 2002, vol. 81, pp. 8–10.
Mowat, E., Paterson, S., Fothergill, J.L., Wright, E.A., Ledson, M.J., Walshaw, M.J., Brockhurst, M.A., Winstanley, C., Pseudomonas aeruginosa population diversity and turnover in cystic fibrosis chronic infections, Am. J. Respir. Crit. Care Med., 2011, vol. 183, pp. 1674–1679.
Shi, M., Li, Y., Wang, Y., Huang, J., Huang, X., and Xu, Y., Regulation of GacA on two phz gene clusters and quorum sensing in Pseudomonas sp. M18, Wei Sheng Wu Xue Bao, 2009, vol. 49, pp. 1306–1316.
Pustelny, C., Albers, A., Buldt-Karentzopoulos, K., Parschat, K., Chhabra, S.R., Camara, M., Williams, P., and Fetzner, S., Dioxygenase-mediated quenching of quinolone-dependent quorum sensing in Pseudomonas aeruginosa,Chem. Biol., 2009, vol. 16, pp. 1259–1267.
Cotar, A.I., Chifiriuc, M.C., Dinu, S., Pelinescu, D., Banu, O., and Lazar, V., Quantitative real-time PCR study of the influence of probiotic culture soluble fraction on the expression of Pseudomonas aeruginosa quorum sensing genes, Roum. Arch. Microbiol. Immunol., 2010, vol. 69, pp. 213–223.
Tsai, M.J., Teng, C.J., Teng, R.J., Lee, P.I., and Chang, M.H., Necrotizing bowel lesions complicated by Pseudomonas septicaemia in previously healthy infants, Eur J. Pediatrics, 1996, vol. 155, pp. 216–218.
Nicolle, L.E., Resistant pathogens in urinary tract infections, J. Am. Geriatrics Soc., 2002, vol. 50, pp. 230–235.
Sapico, F.L. and Montgomerie, J.Z., Vertebral osteomyelitis, Infect. Dis. Clin. North Am., 1990, vol. 4, pp. 539–550.
Yu, Y., Cheng, A.S., Wang, L., Dunne, W.M., and Bayliss, S.J., Hot tub folliculitis or hot hand-foot syndrome caused by Pseudomonas aeruginosa,J. Am. Acad. Dermatol., 2007, vol. 57, pp. 596–600.
Adonizio, A., Kong, K.F., and Pritt, K., Inhibition of quorum sensing-controlled virulence factor production in Pseudomonas aeruginosa by south Florida plant extracts, Antimicrob. Agents Chemother., 2008, vol. 52, pp. 198–203.
Hooper, D.C., Mode of action of fluoroquinolones, Drugs, 1999, vol. 58, pp. 6–10.
Flanders, S.A., Collard, H.R., and Saint, S., Nosocomial pneumonia: State of the science, Am. J. Infect. Control., 2006, vol. 34, pp. 84–93.
Donlan, R.M. and Costerton, J.W., Biofilms: Survival mechanisms of clinically relevant microorganisms, Clin. Microbiol. Rev., 2002, vol. 15, pp. 167–193.
Davies, D.G., Parsek, M.R., Pearson, J.P., Iglewski, B.H., Costerton, J.W., and Greenberg, E.P., The involvement of cell-to-cell signals in the development of a bacterial biofilm, Science, 1998, vol. 280, pp. 295–298.
Hoyle, B. and Costerton, J.W., Bacterial resistance to antibiotics: The role of biofilms, Progr. Drug Res., 1991, vol. 37, pp. 91–105.
Lyczak, J.B., Cannon, C.L., and Pier, G.B., Lung infections associated with cystic fibrosis, Clin. Microbiol. Rev., 2002, vol. 15, pp. 194–222.
Lazar, V. and Chifiriuc, M.C. Architecture and physiology of microbial biofilms, Roum. Arch. Microbiol. Immunol., 2010, vol. 69, pp. 95–107.
Martinez, L.R. and Fries, B.C., Fungal biofilms: Relevance in the setting of human disease, Curr. Fungal Infect. Rep., 2010, vol. 4, pp. 266–275.
Sintim, H.O., Smith, J.A., Wang, J., Nakayama, S., and Yan, L., Paradigm shift in discovering next-generation anti-infective agents: Targeting quorum sensing, c-di-GMP signaling and biofilm formation in bacteria with small molecules, Future Med. Chem., 2010, vol. 2, pp. 1005–1035.
Hentzer, M. and Givskov, M., Pharmacological inhibition of quorum sensing for the treatment of chronic bacterial infections, J. Clin. Invest., 2003, vol. 112, pp. 1300–1307.
Smith, R.S. and Iglewski, B.H., Pseudomonas aeruginosa quorum sensing as a potential antimicrobial target, J. Clin. Invest., 2003, vol. 112, pp. 1460–1465.
McKnight, S.L., Iglewski, B.H., and Pesci, E.C., The Pseudomonas quinolone signal regulates rhl quorum sensing in Pseudomonas aeruginosa.J. Bacteriol., 2000, vol. 182, pp. 2702–2708.
Espin, J.C., Garcia-Conesa, M.T., and Tomas-Barberan, F.A., Nutraceuticals: Facts and fiction, Phytochemistry, 2007, vol. 68, pp. 2986–3008.
Pesci, E.C., Milbank, J.B.J., Pearson, J.P., McKnight, S., Kende, A.S., Greenberg, E.P., and Iglewski, B.H., Quinolone signaling in the cell-to-cell communication system of Pseudomonas aeruginosa,Proc. Natl. Acad. Sci. U. S. A., 1999, vol. 96, pp. 11 229–11 234.
Reimmann, C., Beyeler, M., Latifi, A., Winteler, H., Foglino, M., Lazdunski, A., and Haas, D., The global activator GacA of Pseudomonas aeruginosa PAO positively controls the production of the autoinducer N-butyryl-homoserine lactone and the formation of the virulence factors pyocyanin, cyanide, and lipase, Mol. Microbiol., 1997, vol. 24, pp. 309–319.
Throup, J., Winson, M.K., Bainton, N.J., Bycroft, B.W., Williams, P., and Stewart, G.S.A.B., Signalling in bacteria beyond bioluminescence, in Bioluminescence and Chemiluminescence: Fundamentals and Applied Aspects, Campbell, A., Kricka, L., and Stanley, P., Eds., Chichester: Wiley, 1995.
Calfee, M.W., Coleman, J.P., and Pesci, E.C., Interference with Pseudomonas quinolone signal synthesis inhibits virulence factor expression by Pseudomonas aeruginosa,Proc. Natl. Acad. Sci. U. S. A., 2001, vol. 98, pp. 11 633–11 637.
Holden, M.T.G., Chhabra, S.R., de Nys, R., Stead, P., Balnton, N.J., Hill, P.J., Manefield, M., Kumar, N., Maurice, L., England, D., Rice, S., Glvskov, M., Salmond, G.P.C., Stewart, G.S.A.B., Bycroft, B.W., Kjelleberg, S., and Williams, P., Quorum-sensing cross talk: Isolation and chemical characterization of cyclic dipeptides from Pseudomonas aeruginosa and other Gram-negative bacteria, Mol. Microbiol., 1999, vol. 33, pp. 1254–1266.
Li, Q., Ni, H., Meng, S., He, Y., Yu, Z., and Li, L., Suppressing Erwinia carotovora pathogenicity by projecting N-acyl homoserine lactonase onto the surface of Pseudomonas putida cells, J. Microbiol. Biotechnol., 2011, vol. 21, pp. 1330–1335.
Van Delden, C. and Iglewski, B.H., Cell-to-cell signaling and Pseudomonas aeruginosa infections, Emerg. Infect. Dis., 1998, vol. 4, pp. 551–560.
Gambello, M.J. and Iglewski, B.H., Cloning and characterization of the Pseudomonas aeruginosa lasR gene, a transcriptional activator of elastase expression, J. Bacteriol., 1991, vol. 179, pp. 3000–3009.
Pritt, K., McPherson, C., and Ohman, D., Posttranslational control of the algT (algU)-encoded sigma22 for expression of the alginate regulon in Pseudomonas aeruginosa and localization of its antagonist proteins MucA and MucB (AlgN), J. Bacteriol., 1997, vol. 179, pp. 3711–3720.
Hentzer, M., Reidel, K., and Rasmussen, T.B., Inhibition of quorum sensing in Pseudomonas aeruginosa biofilm bacteria by a halogenated furanone compound, Microbiology, 2002, vol. 148, pp. 87–102.
Wu, H., Song, Z., Hentzer, M., Andersen, J.B., Molin, S., Givskov, M., and Hoiby, N., Synthetic furanones inhibit quorum-sensing and enhance bacterial clearance in Pseudomonas aeruginosa lung infection in mice, J. Antimicrob. Chemother., 2004, vol. 53, pp. 1054–1061.
Manefield, M., de Nys, R., Kumar, N., Read, R., Givskov, M., Steinberg, P., and Kjelleberg, S., Evidence that halogenated furanones from Delisea pulchra inhibit acylated homoserine lactone (AHL)-mediated gene expression by displacing the AHL signal from its receptor protein. Microbiology, 1999, vol. 145, pp. 283–291.
Manefield, M., Rasmussen, T.B., Henzter, M., Andersen, J.B., Steinberg, P., Kjelleberg, S., and Givskov, M., Halogenated furanones inhibit quorum sensing through accelerated LuxR turnover, Microbiology, 2002, vol. 148, pp. 1119–1127.
Ren, D., Zuo, R., and Wood, T.K., Quorum-sensing antagonist (5Z)-4-bromo-5-(bromomethylene)-3-butyl-2(5H)-furanone influences siderophore biosynthesis in Pseudomonas putida and Pseudomonas aeruginosa,Appl. Microbiol. Biotechnol., 2005, vol. 66, pp. 689–695.
Zahin, M., Hasan, S., Aqil, F., Khan, M.S., Husain, F.M., and Ahmad, I., Screening of certain medicinal plants from India for their anti-quorum sensing activity, Indian J. Exp. Biol., 2010, vol. 48, pp. 1219–1224.
Zhu, H., Liu, W., Tian, B., Liu, H., and Ning, S., Inhibition of quorum sensing in the opportunistic pathogenic bacterium Chromobacterium violaceum by an extract from fruiting bodies of Lingzhi or Reishi medicinal mushroom, Ganoderma lucidum (W.Curt.:Fr.) P. Karst. (higher basidiomycetes), Int. J. Med. Mushrooms, 2011, vol. 13, pp. 559–564.
Schulz, S., Dickschat, J.S., Kunze, B., Wagner-Dobler, I., Diestel, R., and Sasse, F., Biological activity of volatiles from marine and terrestrial bacteria, Mar. Drugs, 2010, vol. 8, pp. 2976–2987.
Balick, M.J. and Cox, P.A., Plants, People, and Culture: The Science of Ethnobotany, New York: Scientific American Library, 1999.
Lacassie, E., Marquet, P., Martin-Dupont, S., Gaulier, J.M., and Lachatre, G., A non-fatal case of intoxication with foxglove, documented by means of liquid chromatography-electrospray-mass spectrometry, J. Forensic Sci., 2000, vol. 45, pp. 1154–1158.
Bussey, H.I., Hawkins, D.W., Gaspard, J.J., and Walsh, R.A., A comparative trial of digoxin and digitoxin in the treatment of congestive heart failure, Pharmacotherapy, 1988, vol. 8, pp. 235–240.
Downie, J.A., The roles of extracellular proteins, polysaccharides and signals in the interactions of rhizobia with legume roots, FEMS Microbiol. Rev., 2010, vol. 34, pp. 150–170.
Khafagi, I.K. and Dewedar, A., The efficiency of random versus ethno-directed research in the evaluation of Sinai medicinal plants for bioactive compounds, J. Ethnopharmacol., 2000, vol. 71, pp. 365–376.
Dewick, P.M., Medicinal Natural Products: A Biosynthetic Approach, New York: Wiley, 2002, 2nd ed.
Cowan, M.M., Plant products as antimicrobial agents, Clin. Microbiol. Rev., 1999, vol. 12, pp. 564–582.
Tsao, C.Y., Wang, L., Hashimoto, Y., Yi, H., March, J.C., DeLisa, M.P., Wood, T.K., Valdes, J.J., and Bentley, W.E., LuxS coexpression enhances yields of recombinant proteins in Escherichia coli in part through posttranscriptional control of GroEL, Appl. Environ. Microbiol., 2011, vol. 77, pp. 2141–2152.
Kim, K., Kim, Y.U., Koh, B.H., Hwang, S.S., Kim, S.H., Lepine, F., Cho, Y.H., and Lee, G.R., HHQ and PQS, two Pseudomonas aeruginosa quorum-sensing molecules, down-regulate the innate immune responses through the nuclear factor-kappaB pathway, Immunology, 2010, vol. 129, pp. 578–588.
Wang, Y., Deng, C., Peng, Q., Chen, Z., Huang, D., Zhang, J., and Song, F., Effect of quorum sensing response regulator nprR deletion on expression of cry protein in Bacillus thuringiensis,Wei Sheng Wu Xue Bao, 2010, vol. 50, pp. 1550–1555.
Diţu, L.M., Chifiriuc, C., Lazar, V., and Mihaescu, G., Implication of quorum sensing phenomenon in the expression of genes that code for bacteriocines in lactic bacteria, Bacteriol. Virusol. Parazitol. Epidemiol., 2009, vol. 54, pp. 147–166.
Lazar, V., Miyazaki, Y., Hanawa, T., Chifiriuc, M.C., Diţu, L.M., Maruţescu, L., Bleotu, C., and Kamiya, S., The influence of some probiotic supernatants on the growth and virulence features expression of several selected enteroaggregative E. coli clinical strains, Roum. Arch. Microbiol. Immunol., 2009, vol. 68, pp. 207–214.
Blumenthal, M., Goldberg, A., and Brinckmann, J., Herbal Medicine: Expanded Commission E Monographs, Newton, MA: Integrat. Med. Comm., 2000.
Chun, S.S., Vattem, D.A., Lin, Y.T., and Shetty, K., Phenolic antioxidants from clonal oregano (Origanum vulgare) with antimicrobial activity against Helicobacter pylori,Proc. Biochem., 2005, vol. 40, pp. 809–816.
Rodrigues, M.R., Krause, L.C., Caramo, E.B., dos Santos, J.G., Dariva, C., and Vladimir de Oliveira, J., Chemical composition and extraction yield of the extract of Origanum vulgare obtained from sub- and supercritical CO2, J. Agric. Food Chem., 2004, vol. 52, pp. 3042–3047.
Chami, F., Chami, N., Bennis, S., Trouillas, J., and Remmal, A., Evaluation of carvacrol and eugenol as prophylaxis and treatment of vaginal candidiasis in an immunosuppressed rat model, J. Antimicrob. Chemother., 2004, vol. 54, pp. 909–914.
Hersch-Martinez, P., Leanos-Miranda, B.E., and Solórzano-Santos, F., Antibacterial effects of commercial essential oils over locally prevalent pathogenic strains in Mexico, Fitoterapia, 2005, vol. 76, pp. 453–457.
Saeed, A.M. and Sabir, A.W., Antibacterial activities of some constituents from oleo-gum-resin of Commiphora mukul,Fitoterapia, 2004, vol. 75, pp. 204–208.
Mendez, C. and Salas, J.A., The role of ABC transporters in antibiotic-producing organisms: Drug secretion and resistance mechanisms, Res. Microbiol., 2001, vol. 152, pp. 341–350.
Hogan, D.A., Vik, A., and Kolter, R., A Pseudomonas aeruginosa quorum-sensing molecule influences Candida albicans morphology, Mol. Microbiol., 2004, vol. 54, pp. 1212–1223.
Persson, T., Hansen, T.H., Rasmussen, T.B., Skindersoe, M.E., Givskov, M., and Neilsen, J., Rational design and synthesis of new quorum-sensing inhibitors derived from acylated homoserine lactones and natural products from garlic, Org. Biomol. Chem., 2005, vol. 3, pp. 253–262.
Rasmussen, T.B., Bjarnsholt, T., Skindersoe, M.E., Hentzer, M., Kristoffersen, P., Kote, M., Nielsen, J., Eberl, L., and Givskov, M., Screening for quorum-sensing inhibitors (QSI) by use of a novel genetic system, the QSI Selector, J. Bacteriol., 2005, vol. 187, pp. 1799–1814.
Teplitski, M., Robinson, J.B., and Bauer, W.D., Plants secrete substances that mimic bacterial N-acyl homoserine lactone signal activities and affect population density–dependent behaviors in associated bacteria, Mol. Plant–Microbe Interact., 2000, vol. 13, pp. 637–648.
Vattem, D.A., Mihalik, K., Crixell, S.H., and McLean, R.J.C., Dietary phytochemicals as quorum sensing inhibitors, Fitoterapia, 2007, vol. 78, pp. 302–310.
Nascimento, G.G.F., Locatelli, J., Freitas, P.C., and Silva, G.L., Antimicrobial activity of plant extracts and phytochemicals on antibiotic resistant bacteria, Braz. J. Microbiol., 2000, vol. 31, pp. 247–256.
Walker, T.S., Bais, H.P., Deziel, E., Schweizer, H.P., Rahme, L.G., Fall, R., and Vivanco, J.M., Pseudomonas aeruginosa–plant root interactions. Pathogenicity, biofilm formation, and root exudation, Plant Physiol., 2004, vol. 134, pp. 320–331.
Huber, B., Eberl, L., Feucht, W., and Polster, J., Influence of polyphenols on bacterial biofilm formation and quorum-sensing, Z. Naturforsch. C: Biosci., 2004, vol. 58, pp. 879–884.
Al-Hussaini, R. and Mahasneh, A.M., Microbial growth and quorum sensing antagonist activities of herbal plants extracts, Molecules, 2009, vol. 14, pp. 3425–3435.
Krishnan, T., Yin, W.F., and Chan, K.G., Inhibition of quorum sensing controlled virulence factor production in Pseudomonas aeruginosa PAO1 by Ayurveda spice clove (Syzygium Aromaticum) bud extract, Sensors, 2012, vol. 12, pp. 4016–4030.
Boga, C., Forlani, L., Calienni, R., Hindley, T., Hochkoeppler, A., Tozzi, S., and Zanna, N., On the antibacterial activity of roots of Capparis spinosa L., Nat. Prod. Res., 2011, vol. 25, pp. 417–421.
Issac Abraham, S.V., Palani, A., Ramaswamy, B.R., Shunmugiah, K.P., and Arumugam, V.R., Antiquorum sensing and antibiofilm potential of Capparis spinosa,Arch. Med. Res., 2011, vol. 42, pp. 658–668.
Chong, Y.M., Yin, W.F., Ho, C.Y., Mustafa, M.R., Hadi, A.H.A., Awang, K., Narrima, P., and Koh, C.L., Malabaricone C from Myristica cinnamomea exhibits anti-quorum sensing activity, J. Nat. Prod., 2011, vol. 74, pp. 2261–2264.
Singh, B.N., Singh, H.B., Singh, A., Singh, B.R., Mishra, A., and Nautiyal, C.S., Lagerstroemia speciosa fruit extract modulates quorum sensing-controlled virulence factor production and biofilm formation in Pseudomonas aeruginosa,Microbiology, 2012, vol. 158, pp. 529–538.
Tan, L.Y., Yin, W.F., and Chan, K.G., Silencing quorum sensing through extracts of Melicope lunu-ankenda,Sensors, 2012, vol. 12, pp. 4339–4351.
Yeo, S.S.M. and Tham, F.Y., Anti-quorum sensing and antimicrobial activities of some traditional Chinese medicinal plants commonly used in South-East Asia, Malaysian J. Microbiol., 2012, vol. 8, pp. 11–20.
Ronald, P.C., Small protein-mediated quorum sensing in a Gram-negative bacterium: Novel targets for control of infectious disease, Discov. Med., 2011, vol. 12, pp. 461–470.
Bouyahya, A., Dakka, N., Et-Touys, A., Abrini, J., and Bakri, Y., Medicinal plant products targeting quorum sensing for combating bacterial infections, Asian Pac. J. Trop. Med., 2017, vol. 10, no. 8, pp. 729–743.
Kalia, V.C., Quorum sensing inhibitors: An overview, Biotechnol. Adv., 2013, vol. 31, pp. 224–245.
Amara, N., Krom, B.P., Kaufmann, G.F., and Meijler, M.M., Macromolecular inhibition of quorum sensing: Enzymes, antibodies, and beyond, Chem. Rev., 2011, vol. 111, pp. 195–208.
Kalia, V.C. and Purohit, H.J., Quenching the quorum sensing system: Potential antibacterial drug targets, Crit. Rev. Microbiol., 2011, vol. 37, pp. 121–140.
Smith, R.S. and Iglewski, B.H., Pseudomonas aeruginosa quorum sensing as a potential antimicrobial target, J. Clin Invest., 2003, vol. 112, pp. 1460–1465.
Rasmussen, T.B. and Givskov, M., Quorum sensing inhibitors: A bargain of effects, Microbiology, 2006, vol. 152, pp. 895–904.
Miyairi, S., Tateda, K., Fuse, E.T., Ueda, C., Saito, H., et al., Immunization with 3-oxododecanoyl-L-homoserine lactone-protein conjugate protects mice from lethal Pseudomonas aeruginosa lung infection, J. Med. Microbiol., 2006, vol. 55, pp. 1381–1387.
Hirakawa, H., Harwood, C.S., Pechter, K.B., Schaefer, A.L., and Greenberg, E.P., Antisense RNA that affects Rhodopseudomonas palustris quorum-sensing signal receptor expression, Proc. Natl. Acad. Sci. U. S. A., 2012, vol. 109, pp. 12 141–12 146.
Umesha, S. and Shivakumar, J., Bacterial quorum sensing and it is applications in biotechnology, Int. J. Pharm. Biol. Sci., 2013, vol. 4, pp. 850–861.
Winson, M.K., Swift, S., Fish, L., Throup, J.P., Jørgensen, F., et al., Construction and analysis of luxCDABE-based plasmid sensors for investigating N-acyl homoserine lactone-mediated quorum sensing, FEMS Microbiol. Lett., 1998, vol. 163, pp. 185–192.
Steindler, L. and Venturi, V., Detection of quorum-sensing N-acyl homoserine lactone signal molecules by bacterial biosensors, FEMS Microbiol. Lett., 2007, vol. 266, pp. 1–9.
Yu, Y.A., Shabahang, S., Timiryasova, T.M., Zhang, Q., Beltz, R., et al., Visualization of tumors and metastases in live animals with bacteria and vaccinia virus encoding light-emitting proteins, Nat. Biotechnol., 2004, vol. 22, pp. 313–320.
Anderson, J.C., Clarke, E.J., Arkin, A.P., and Voigt, C.A., Environmentally controlled invasion of cancer cells by engineered bacteria, J. Mol Biol., 2006, vol. 355, pp. 619–627.
Dong, Y., Wang, L.H., and Zhang, L.H., Quorum-quenching microbial infections: Mechanisms and implications, Philos. Trans. R. Soc. Lond. B: Biol. Sci., 2007, vol. 362, pp. 1201–1211.
Moghaddam, M.M., Khodi, S., and Mirhosseini, A., Quorum sensing in bacteria and a glance on Pseudomonas aeruginosa,Clin. Microbiol., 2014, vol. 3, p. 156. https://doi.org/10.4172/2327-5073.1000156
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
COMPLIANCE WITH ETHICAL STANDARDS
This article does not contain any studies involving human participants performed by any of the authors and does not contain any studies involving animals performed by any of the authors.
Conflict of Interests
The authors declare that they have no conflicts of interest.
Additional information
Corresponding author: phone: +91-9897088910; e-mail: aasif321@gmail.com.
Rights and permissions
About this article
Cite this article
Asif, M., Imran, M. Effect of Quorum Sensing Inhibitor Agents against Pseudomonas aeruginosa. Russ J Bioorg Chem 46, 149–164 (2020). https://doi.org/10.1134/S1068162020020041
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S1068162020020041