Abstract
This review aims to consolidate current views on the cells of one of the peripheral nerve sheath layers, perineurium. The relevance of the subject matter owes the lack of basic knowledge about the involvement of these cells in the restoration of damaged nerve conductors, as well as the need to unravel the molecular mechanisms that stimulate the regeneration of damaged nerves. The review summarizes recent data on the morphofunctional features of the perineurium, phylogenetic and ontogenetic origins of perineurial cells, and molecular features of the regulation of the blood–nerve barrier. It accentuates the uniqueness of the ontogenetic origin of the perineurium, characterizes immunohistochemical markers of perineurial cells, describes the features of the perineurium in the dorsal root ganglia and spinal nerve roots.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
The perineurium is one of the nerve sheaths, which consists of cells whose morphofunctional features make them unique among other cells of the animal and human organism. The relevance of studying perineurial cells is due to the lack of basic information about their involvement in the restoration of damaged nerve conductors, as well as the need to elucidate the molecular mechanisms that stimulate nerve regeneration after damage. Despite the high regenerative ability of peripheral nerve fibers, it is not always possible to achieve complete post-traumatic functional recovery of the nerve using surgical methods [1, 2]. The success of neuroplasty and suture techniques used in clinical practice depends on the degree of nerve injury. The search for new methods to assess this degree, as well as methods to stimulate their regeneration, are in rapid progress now [1–5]. To develop and improve these methods, it is necessary to study the molecular mechanisms that regulate the reparative processes in the damaged nerve and the relationship among the cells that provide endoneural homeostasis and the functioning of the blood–nerve barrier.
Studies of the morphofunctional features of nerves in health and disease have been carried out for many decades, dating back to the classic works by an English histologist August Waller (1816–1870) and a Spanish neurobiologist Santiago Ramón y Cajal (1852–1934). The results of recent studies using immunohistochistry, electron, confocal and fluorescence microscopy, Western blotting, PCR, and other methods, are summarized in a number of monographs and reviews [2, 6–12]. Currently, much of the focus is on the glial elements of the peripheral nervous system (PNS), Schwann cells [8, 11, 13, 14]. Other cellular elements of the nerve remain by far less studied, specifically it concerns perineurial cells, which, alongside with Schwann cells, are involved in creating a microenvironment needed for the growth and regeneration of axons. The present review aims to generalize the available literature data on perineurial cells, their origin in phylo- and ontogeny, injury responsiveness, and regenerative potential.
NERVE SHEATHS
The sheaths that create a microenvironment ensuring the normal functioning of the nerve fiber (epineurium, perineurium, endoneurium) were described as early as the 19th century. They represent a continuation of the meninges covering the brain and spinal cord: dura mater, arachnoid mater and pia mater, respectively [15, 16]. In some modern studies, they are sometimes called not sheaths, but parts or layers of nerve conductors [17]. The term “sheath” accounts for the fine structure of the nerve (Fig. 1a). Individual nerve fibers enveloped by Schwann cells are located in the endoneurium. Among them, there are myelinated and nonmyelinated fibers. The fascicles of such fibers are enveloped by a perineurial sheath. The nerve trunk comprising several nerve fascicles is covered on the outside by the epineurium [7, 9, 10].
The endoneurium contains (apart from nerve fibers, SCs, capillaries and individual arterioles with few pericytes) mast cells, resident macrophages, fibroblasts, and collagen fibers consisting of collagen types I and III, which are produced by fibroblasts and Schwann cells [18]. Blood vessels penetrate into the endoneurium from the epineurial outer sleeve through the perineurium, acquiring a sheath of perineurial cells [15]. The mechanical strength of the nerve trunk is provided by collagen fibers. The percentage of endoneurial cells is as follows: account for 10%, 2–9% fall on macrophages and few mast cells, while the rest of the cells belongs to peripheral glia, myelinating and nonmyelinating Schwann cells [18]. Most of endoneurial vessels receive no innervation. Importantly, endothelial cells of endoneurial vessels are interlinked by tight contacts and are involved, along with perineurial cells, in the formation of a specific blood-nerve barrier [9, 19].
The epineurium is the outer connective-tissue sheath of the nerve trunk, containing fibroblasts, mast cells, adipose tissue, numerous type 1 collagen and elastic fibers, blood and lymphatic vessels [9, 20]. Throughout the entire length of the nerve, the epineurium has a different thickness, because its constituent adipose tissue does not form a continuous layer along, but is concentrated as discrete islets. Adipose tissue protects nerve fascicles from compression. It has been shown that the depletion of adipose tissue in the epineurium during general exhaustion leads to the development of paralysis [18]. The epineurial sheath allows the nerve to retain some mobility, i.e. the ability to lengthen and shorten to a limited extent. The epineurial blood vessels are quite permeable. Epineurial arterial and venous vessels of different calibers anastomose, thus forming a vasculature, which is linked with large-caliber arteries and veins running along the nerve trunk. Epineurial vessels are amply innervated: sympathetic adrenergic and peptidergic nerve terminals provide their tone, constriction and dilation [9]. The innervation of the nerve sheaths involves thin unmyelinated axons exiting from the endoneurium of the nerve trunk (nervi nervorum) [9, 21]. In the epineurium, there are nervi nervorum that are not associated with blood vessels and revealed by immunohistochemical reactions to calcitonin gene-related peptide (CGRP) and peripherin [21]. Lymphatic vessels of the epineurium are linked with regional lymph nodes. It is noteworthy that lymphatic vessels are present only in the epineurium, being absent in other nerve structures [9, 18]. Having penetrated through the perineurial sheath, epineurial vessels form a vasculature of the inner sheath of the nerve trunk, endoneurium.
The composite human nerves, containing afferent and efferent fibers and associated with extensive innervation zone, are covered with the paraneurium on the outside of the epineurium. This is a connective tissue structure located between the nerve and muscles [22]. It contains a large amount of adipose tissue and collagen fibers. In the recent studies, the paraneurium is often called circumneurium [22]. For some reasons, the problem of studying the paraneurium is very topical and acquires great practical significance [22–25]. Firstly, it is related with elucidating the processes that occur inside and outside the nerve trunk after surgical interventions or intraneural injections. In medical practice, it is important to explore the distribution of local anesthetics used in anesthesiology, as well as the sequelae of unintentional intraneural injections [26]. Secondly, changes in the paraneurium can lead to degenerative processes in the nerve trunk itself.
All nerve sheaths and the paraneurium are structurally and functionally interrelated. The medium sheath of the nerve trunk, perineurium, differs in a number of morphofunctional features not inherent to other nerve sheaths.
A diagram of the sheaths covering the nerve (a) and spine nerve roots (b). I—endoneurium; II—perineurium; III—epineurium; 1—nerve fiber; 2—subperineurial space; 3—basement membrane; 4—collagen fibers; 5—adipocyte; 6—blood vessel; 7—subarachnoid angle; 8—dura mater; 9—arachnoid mater; 10—pia mater; 11—nerve root sheath; SC—spinal cord; G—dorsal root ganglion; DR—dorsal root; VR—ventral root; N—nerve. Modified from [46, 49] using our own histological slides.
FEATURES OF PERINEURIAL CELLS
First light microscopic studies. The results of structural studies of nerves and their sheaths, carried out as early as the 19th century and even earlier, are surveyed in a number of articles and monographs [17, 27–29]. The first histological descriptions of the perineurial sheath date back to the studies of the German physiologist and anatomic pathologist Friedrich Gustav Jacob Henle (1809–1885), Swedish physicians and anatomists Ernst Axel Henrik Key (1832–1901) and Magnus Gustav Retzius (1842–1919), and French histologist Louis-Antoine Ranvier (1835–1922). In different years, it was possible to come across various names for the perineurial sheath, such as the Henle layer, sheath of Ranvier, neurothelium, perilemma, etc. Ranvier, when studying the three sheaths of nerve conductors, called them the intrafascicular tissue, lamellated sheath, and the perifascicular tissue. The terms endo-, peri- and epineurium, which are still being used in neuroscience, were coined by Key and Retzius.
Studies carried out in the middle of the past century on several vertebrate species [15, 30] demonstrated that the perineurial sheath envelopes both common nerve trunks and their segments, peripheral nerve fascicles. It was shown that it consists of flattened cells arranged in several layers. In the same years, it was proved that nerve sheaths have a barrier function [27].
The perineurial nerve sheath has some specific features in different animals. It has been studied in detail in fish occupying different rungs of the “evolutionary ladder”: in a cartilaginous elasmobranch fish (shark, Ginglymostoma cirratum) and in a teleost fish (Danio rerio). It was found that the shark perineurium consists of as few as three cell layers [30]. In the zebrafish Danio rerio, the perineurial sheath shows a structural similarity with the mammalian perineurium. In zebrafish larvae, it was shown that perineurial progenitor cells migrate from the ventral part of the developing spinal cord [31, 32]. In amphibians, specifically in a frog, in contrast to mammals whose perineurium comprises 4–5 layers of perineurial cells [15], and humans, where the number of cell layers ranges from 8 to 18 [10] (according to some reports, up to 20), the perineurium is not a laminar structure and consists of two layers that are stained on histological preparations in different colors (Mallory’s staining) [27]. The morphology of the perineurium in birds is similar to that in mammals. Studies of the sciatic nerve, carried out on chickens and their embryos, have shown that perineurial features, characteristic of an adult, form at the age of 10–20 days [33]. It should be noted that there are no works in the literature that would generalize data on the evolutionary patterns of the perineurium development in phylogenesis. There are only separate studies devoted to a comparison of the paraneurium (circumneurium) structure in animals of different taxa [24, 34].
Ultrastructural studies of perineurial cells. The structure of the perineurial sheath in different animals and humans has been studied in more detail using electron microscopy and the freeze-etching technique [6, 7, 10, 18, 35]. It was established that the perineurium that envelopes the nerve fascicle consists of several layers of flattened cells interlaid with collagen fibers of connective tissue. Each layer is formed by polygonal cells tightly interlinked via specialized contacts. The number of perineurial cell layers depends on the thickness of the fascicle [17]. In humans, the number of perineurial cell layers in the sciatic nerve varies from 8 to 18 [10], and the thickness of the perineural sheath reaches 20 µm. The laminar arrangement of the perineurium, described previously in studies performed at the light-optical level, was confirmed and detailed by electron microscopy. It was found that each layer of perineurial cells is covered on either side with the basement membranes. Between the layers of perineurial cells, along with type IV collagen fibers (675 to 765 nm in diameter), there are extracellular matrix proteins, such as fibronectin and laminin, as well as glycosaminoglycans [36, 37]. The nuclei of perineurial cells, like the cells themselves, are typically flattened. Electron microscopic studies of perineurial cells have revealed cytoplasmic actin-containing structures resembling actin filaments in smooth muscle cells [18]. The function of these structures in perineurial cells is not entirely clear. Presumably, they provide the contractile properties of the perineurial sheath, preserve the nerve fascicle’s shape, and allow this to alter when damaged. It is also possible that, due to peristaltic movements, perineurial cells contribute to the flow of endoneurial fluid along the nerve fascicles.
Within the layer, there are no basal laminae between adjacent perineurial cells, which are interconnected via tight junctions. The latter are produced by marginal cytoplasmic invaginations of adjacent cells, forming a “zip lock” between the opposing plasma membranes [7]. Freeze-etching studies have shown that tight junctions are much more common in the perineurium than shown on ultrathin sections [18]. There are also rare gap contacts indicating the presence of an active diffusion barrier. It has been shown that such contacts are more characteristic of the early periods of ontogeny; therefore, immature nerves are more sensitive to toxins and infectious agents [18]. Electron microscopy reveals intracytoplasmic pinocytic vesicles and caveolae in the outer layers of the perineurium [10, 18]. Perineural cells are able to take up via pinocytosis and transport various substances from the endoneurial space.
Between the perineurium and endoneurium, there is a subperineurial space filled with a weakly basophilic homogeneous matrix, which includes glycosaminoglycans [38]. It also contains thin collagen fibers and blood vessels involved in the formation of the endoneurial microcirculatory bed. Presumably, the subperineurial space provides homeostasis and molecular transport [38].
As mentioned above, the perineurium is associated with the arachnoid mater of the spinal cord. As the nerve moves away from the spinal cord meninges distalward, the number of nerve fascicles increases, and the perineurial sheath becomes ever thinner. Its termination at the distal end depends on the fiber type. In unmyelinated fibers, the perineurium fades away in the area of the nerve terminals.
In myelinated nerve fibers, the perineurium ends near the neuromuscular synapses at a distance of 1–1.5 mm [17]. While ending near the nerve terminals, the perineurium gradually alters. It loses the basement membranes and tight junctions, and nerve fibers becomes surrounded only by an accumulation of single fibroblasts.
In some encapsulated sensory endings, perineurial cells do not disappear, but enter into the composition of their capsules. This is typical of Ruffini and Vater–Pacini corpuscles, as well as similar Timofeew’s bodies, which occur in the human body in the late prenatal and early postnatal periods [39]. It has been shown that in the encapsulated sensory endings, the perineurium is represented by a continuous outer, but not inner, layer. For instance, it has been proven immunohistochemically that the outer layers of the Vater-Pacini corpuscle’s capsule are indeed derivatives of perineurial cells, while the cells of the inner layers express S100+ and Leu-7+ proteins and, therefore, originate from Schwann cells [40].
The structure of the perineurium is heterogeneous. Pinã-Oviedo and Ortiz-Hidalgo [17] distinguish three zones therein: (1) the inner zone, which is separated from the endoneurium by a subperineurial space and is formed by a single layer of perineurial cells connected via mutual interdigitations and tight junctions; (2) the intermediate zone consisting of several cell layers whose number depends on the size of the nerve fascicle and ranges from 3 to 15 concentric layers (5 to 20 µm wide); and (3) the outer zone, which is transitional between the perineurium and epineurium. The third zone does not have a laminar structure, but consists of several wide collagen bundles similar to those in the epineurium [17]. The modern domestic histological nomenclature distinguishes two parts of the perineurium: the epithelioid part (pars epitheloidea) and the fibrous part (pars fibrosa) [41].
Features of the perineurium in spinal nerve roots and dorsal root ganglia. The perineurial sheath is inherent not only to nerves, but also to spinal roots and ganglia, where its structure has a number of distinctive features. The ventral (anterior) root contains the axons of motor neurons. The dorsal (posterior) root consists of the processes of sensory neurons located in the dorsal root ganglia. Their sheaths protect nerve fibers of the roots only from chemical and mechanical exposures, but not from deformation and stretching as they are not elastic enough. Unlike nerve sheaths, root sheaths are also not suited for suturing [42]. The area of spinal roots is a transitional zone between the PNS and CNS. All the details of the transition of the spinal meninges into nerve sheaths have not yet been fully elucidated. The CNS–PNS transition zone also requires further investigation [43].
Outside the subarachnoid space, the ventral and dorsal spinal roots have three sheaths typical for peripheral nerves: epineurium, perineurium, and endoneurium. In the region of the subarachnoid angle, the epineurium of peripheral nerves turns into the spinal dura mater (Fig. 1b). The endoneurium remains unchanged until the area where the roots contact the spinal cord. In the area of the subarachnoid angle, the structure of the perineurial sheath undergoes considerable alterations [44, 45]. In this zone, the outer part of the nerve perineurium passes between the spinal dura mater and arachnoid mater, and the spinal arachnoid mater coalesces with the outer perineurial layers of the roots [42, 44, 45]. The inner perineurial layers reach the CNS within the sheath of spinal roots. An electron microscopic study of the mutual arrangement of the nerve and spinal sheaths [46] showed that the inner layers of the root sheath look like the perineurium of the nerve trunk. The outer part of this sheath structurally resembles the arachnoid mater, and in some places, the pia mater [42, 46]. A typical rat spinal root sheath consists of three or four layers of flattened cells, with cells of the inner layers containing a large number of pinocytic vesicles and cytoplasmic vacuoles. In contrast to the perineurium of the nerve trunk, the basement membranes in the spinal root may have an intermittent structure [46]. Nearby the spinal cord, perineurial cells in the spinal roots gradually lose the basement membrane, the number of collagen fibers decreases, the cells become more and more alike the flattened meningothelial cells that line the spinal meninges [7].
The relationship between the subarachnoid space and the endoneurium of the spinal root and peripheral nerve is understudied. Previously, it was believed that perineurial cells isolate spinal roots from the subarachnoid space, and due to this, there is no direct communication between the subarachnoid space and endoneurium [47]. Currently, tracer studies have established that the cerebrospinal fluid (CSF) of the subarachnoid space spreads along all nerves and can transport various antigens [48]. Some authors suggest that the dorsal root entry zone and motor exit point may represent the areas, where the subarachnoid space contacts the root endoneurium, and is definitely the site of contact between the endoneurial fluid and CSF [49]. It still remains unclear how the CSF flow is realized: through the perineurial space between the perineurial layers [33], through the perineurial space between the perineurium and epineurium [48, 50], or directly via the endoneurium [49, 51].
The urgency of solving this issue is tightly associated with the problem of the penetration of pathogens into the CNS organs. Studies performed on the cranial and spinal nerves have shown that, along with the hematogenous route of penetration, there is a perineurial invasion of some pathogens and tumor cells [52–55]. It is also believed that the continuity between the subperineurial space and the subarachnoid space with its CSF ensures drug penetration into the brain and spinal cord.
As for the capsule of the autonomic and spinal ganglia, it consists of two parts. The inner part is equivalent to the perineurium of peripheral nerves, while the outer part represents an enlarged epineurium containing collagen fibers and fibroblasts [56]. The use of tracers (horseradish peroxidase and ferritin) has shown that the inner part of the superior cervical ganglion capsule in rats and mice, consisting of several layers of perineural cells, forms a barrier similar to the blood–nerve barrier [57]. In this case, the blood vessels of the ganglion are more permeable than the endoneural vessels of the nerve. Among them, there are fenestrated capillaries. It has been shown that horseradish peroxidase (but not large ferritin molecules) penetrates into such vessels and is present in perivascular macrophages.
According to modern views, each perineurial cell layer of the sensory ganglia, like the perineurium of nerve conductors, is limited on both sides by the basement membranes; the cells of each layer have numerous tight junctions and desmosomes, as well as few gap junctions [58]. Cell layers are separated by extracellular spaces containing collagen fibers. The perineurium of spinal ganglia consists of a larger number of cells than the perineurium of the nerve. For example, in a rat, cat and rabbit, the perineurium of the ganglion has 7–11 cell layers, while in the sciatic nerve, up to 5. Moreover, in the ganglion, the perineurial layers themselves are thicker than in the nerve [7].
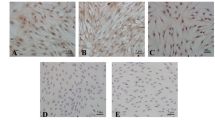
Immunohistochemical labeling of the perineurium. The advent of novel immunohistochemical methods allowing identification of different cell types through visualization of their specific proteins opened a new era in studying morphofunctional features of the perineurium. Currently, a host of neuronal and glial markers are widely used to explore the PNS structures (nerve plexuses, fibers, terminals, neurons and glial cells) [12, 59–61]. Meanwhile, the number of immunohistochemical markers for the identification of perineurium cells is not that large.
Immunohistochemical studies have shown that perineurial cells express vimentin, a ubiquitous type III intermediate filament protein of mesenchymal (connective tissue) cells, as well as the glucose transporter 1 (GLUT1), epithelial membrane antigen (EMA), but do not express the Schwann cell-specific S100 protein and nerve cell markers, such as neurofilament proteins [17].
As noted above, the overlapping polygonal cells of the perineurium are linked by tight junctions. Specific proteins of these junctions are used as markers for perineurial cells. Using the methods of indirect immunofluorescence and immunoelectron microscopy, it has been shown that the tight junction proteins—claudins, ZO-1, occludin—are expressed in the perineurium of the mammalian and human nerve [62].
Claudins, intercellular adhesion molecules located in the area of tight junctions, are involved in the maintenance of cellular homeostasis, intercellular signal transmission, and cytoskeleton organization [63]. Claudin-1 (Cldn1) is expressed in the PNS and CNS as the main protein of the blood–nerve and blood–brain barriers (BBB). Studies of peripheral nerves have shown a high Cldn1 expression in the perineurium of peripheral nerves, as well as in the Schmidt–Lanterman incisures and mesaxon [64]. When the rat sciatic nerve is damaged by ligation, the expression of Cldn1, Cldn5, and other tight junction proteins decreases [65]. It this case, using intravenous and local administration of the Evans blue azo dye, it was found that the blood–nerve barrier is disrupted, and its restoration only occurs a week later [65]. It has been noted that spinal ganglion injury does not entail similar changes [66].
In the mammalian nervous system, species-specific differences were noted in the presence of certain claudins. In addition, using real-time PCR, it was demonstrated that claudin-11 is expressed in the CNS cells, whereas claudin-19 is more PNS-specific. Claudin-19 was identified in the perineurium, as well as in Schwann cells of the mesaxon area [64, 67]. In the spinal ganglion, this protein is present in the zone where the processes of sensory neurons concentrate [66]. The significance of claudins is very high: in claudin-19-deficient knockout mice, the normal conductance of the sciatic nerve is impaired [64, 68].
The tight junction protein ZO-1, which forms complexes with Cldn1, occludin and cytoskeletal actin, is an integral part of the blood–nerve barrier and is expressed not only in the perineurium, but also in the walls of endoneurial blood vessels. Immunohistochemical staining for ZO-1 reveals a clear-cut zigzag pattern, which is blurred in neuropathy [69]. In the sciatic nerve of mice and humans, the expression of the ZO-1 protein has also been described in myelinating Schwann cells [64].
Occludin is an integral protein with a molecular weight of 65 kDa, consisting of four domains. The N- and C-termini of the occludin molecule are located on the outer surface of the plasma membrane. Occludin performs a regulatory function and is associated with other tight junction proteins [70]. Occludin is expressed in the perineurium of peripheral nerves, endothelial cells of endoneurial vessels, as well as in the Schmidt–Lantermann incisures and mesaxon of myelinating Schwann cells [64]. Occludin has been shown to colocalize with another protein of tight contacts, tricellulin [67].
Such structural cytoskeletal proteins, characteristic of perineurial cells, as talin and vinculin, are involved in establishing contacts between perineurial cells and other cellular elements and extracellular matrix via integrin receptors. It was found that the talin content in the perineurium diminishes in diabetes [71].
In immunohistochemical studies of the perineurium, along with proteins of cell contacts, the proteins of the extracellular space are used as markers. As noted before, the basement membranes, which contain type IV collagen, are located between the perineurial cells. Double immunolabeling of type IV collagen and Cldn1 (as well as other tight junction proteins) made it possible to study the embryogenesis of the perineurial sheaths of the human sciatic nerve [62]. Immunohistochemical detection of laminin and integrin is also used in studies of the perineural membrane [72]. It was established that, under in vitro conditions, all laminin isoforms can be expressed both by perineurial cells and endoneurial fibroblasts. However, it was noted that in vivo, these cell types express different laminin isoforms: A, B2, and S chains in perineurial cells, in contrast to B1, B2, M and S chains in endoneurial fibroblasts [17].
Another immunohistochemical marker of perineurial cells, typically used in combination with occludin or laminin labeling, is the reaction for the protein of cell contacts connexin 43 [73].
Some authors believe that, apart from Cldn1, the best perineurium markers are EMA and GLUT1 [17]. EMA belongs to a heterogeneous family of highly glycosylated transmembrane proteins that were originally found on the surface of mammary epithelial cells, and that are also present in the cells of virtually all epithelial tumors. It was found that, under normal conditions, this protein occurs in the cytoplasm of perineurial, arachnoid and pia mater cells. The GLUT1 protein belongs to the group of glucose transporters and was found in many cell types. It has been shown that GLUT1 occurs all perineurial areas, as well as in the endothelium of endoneurial blood vessels. The normal distribution of GLUT1 was studied in the PNS and CNS of young and aged animals, using immunohistochemical methods, in situ hybridization, and Evans blue perfusion [74]. It was shown that shortly after birth, GLUT1 is not expressed in the perineurium and appears only in adult animals in the perineurial sheath of nerves and spinal roots, as well as in the capsule of the dorsal root ganglia and in the pia mater. In humans, it was noted that, at the early stages of ontogeny, GLUT1 is absent in the fetal perineurium, and is expressed in amounts quite sufficient for visualization beginning from weeks 22–26 of gestation [75, 76]. After nerve injury, its content declines and is restored in the process of regeneration [74, 77].
To date, studies that employ immunohistochemical detection of the above proteins in a vertebrate lineage have been mainly carried out on the perineurium of laboratory animals (rats and mice). There are no data on the availability and characteristics of perineurial markers in other animal species.
Thus, a study of perineurial cells using classical histological staining methods and electron microscopy showed their structural similarity in different vertebrates and humans. The structure of the perineurium is complicating in the lineage leading from amphibians to mammals, as manifested in the multiplication of perineurial cell layers. In the available literature, we failed to find any works on the alternative developmental patterns of the perineurial sheath during phylogeny. The lack of such works may be due to the fact that the issue of whether perineurial cells belong to a definite tissue type is still debatable. In 1876, Kay and Retzius found the resemblance between the cells forming a sheath that envelopes the nerve fascicles and endothelial cells and called them “endothelial-like”.
Ranvier, having describing the laminar arrangement of the perineurium, emphasized that each of its lamellae consists of “fibrillar stroma and endothelium”. Indeed, the structure of cells in that part of the perineurium, which directly borders on the endoneurium, is similar to the endothelium of endoneurial microvessels [78]. There is also a similarity in the structure of intercellular contacts between perineurial and endothelial cells. At the same time, the laminar structure of the perineurium and the alternation of tight (zonula occludens) and adhesive (zonula adherens) cell–cell contacts are characteristic of epithelial tissues. In this regard, in studies carried out in the middle of the past century, the perineurium was referred to epithelial tissues [15]; later, in the 1980s, it was called an “epitheliomorphic” structure [7], while perineurial cells were christened “neurothelial epithelioid cells” [79]. In vitro studies have emphasized an epithelial growth of perineurial cells [80]. Some authors call perineurial cells modified fibroblasts [18, 81], others call them epithelioid myofibroblasts [19]. In modern studies, perineural cells are often referred to as peripheral glial cells [75, 82–84]. Thus, the nature and origins of perineurial cells is still under discussion. A study of the perineurium embryogenesis sheds some light on this issue.
EMBRYOGENESIS OF THE PERINEURIUM
The ontogenetic development of perineurial cells was studied in embryos of birds [33] and rodents [7], as well as in and human fetuses [62, 72, 76, 85]. It was shown that at the initial stage of embryogenesis, nerve fibers are separated into fascicles by loosely spaced fibroblasts. Later, there occurs a maturation of the perineurial sheath in the nerve, i.e. the formation of typical tight junctions between cells and basement membranes between layers of perineurial cell layers. This process coincides with the onset of axonal myelination.
Electron microscopic studies performed on rats [7] showed that on prenatal days 10–11, there are no perineurial sheaths around the embryonic primordium of peripheral nerves and dorsal root ganglia. On prenatal day 15, i.e. in the period when the growing axons get into a relationship with the Schwann cell precursors, flattened cells appear on the surface of the developing nerves and ganglia, and collagen fibers begin to concentrate around them. On prenatal day 18, when individual myelinated fibers appear in the developing rat nerve trunks, there are already 1–2 layers of perineurial cell precursors at the periphery, which have a heavily flattened cytoplasm and nucleus and are interconnected by tight junctions. Two-three weeks after birth, the structure of the perineurium resembles that of adult animals. A month after birth, the perineurium begins to perform a barrier function [86, 87].
Du Plessis et al. [33], when studying the formation of the chicken perineurium, distinguished three phases in its development. The early period, when the embryonic perineurium is just beginning to organize, the second period, which includes the differentiation and formation of a multilayer structure, and the third phase associated with the formation of a barrier. The authors emphasize that perineurial differentiation occurs during the period of active proliferation of neurolemmocytes (Schwann cells) and is closely related to the development of axon-neurolemmocyte complexes. Having traced perineurial differentiation at all stages of the chicken development, the authors found that perineurial cells are of mesenchymal origin, and do not derive from Schwann cells as previously thought. It has been shown that differentiation of perineurial cells from the surrounding mesenchymal cells can be influenced by factors released from growing axons and neurolemmocytes. On prenatal day 17, the basement membranes form in the perineurium, and at the same time, blood vessels appear in the endoneurial area. The authors consider this period as an onset of the formation of the blood–nerve barrier. However, a perineurial laminar organization inherent to an adult organism, as well as a characteristic ultrastructure of perineurial cells, are only observed in chickens aged 10 days.
The formation of the perineurium in human embryos and fetuses was studied using various methods (electron microscopy, immunohistochemistry, Western blotting) [62, 72, 76, 85]. It was found that the basement membranes in the developing sciatic and tibial nerves appear first around Schwann cells (already at 11 weeks), and only in the period from weeks 17 to 35, they gradually form around the perineurial cells; tight junctions appear in the perineurium at 14 weeks, GLUT1 expression starts from weeks 22 to 26. It has been shown that in the period from weeks 11 to 35, the diameter of the fetal sciatic nerve increases. This is due to an increase in the diameter of the nerve fascicles, which in turn is associated with the onset of axonal myelination and an increase in the amount of the endoneurial extracellular matrix. During these periods, thin septa extending from the perineurium into the endoneurial space divide the fascicles into the smaller ones. At this time, the nuclei of perineurial cells have a flattened shape, which resembles that of the nuclei in perineurial cells of adult animals. As development advances, there is a gradual increase in the number of perineurial cell layers.
A study of the appearance of the tight junction proteins Cldn1, Cldn3, ZO-1, and occludin during the embryogenesis of the human sciatic nerve [62] showed that Cldn1 is expressed first, being identified in the perineurium already at 11 weeks of gestation and forming an intense dotted pattern. Cldn3 and occludin exhibited more diffuse dotted labeling of the perineurial sheath. ZO-1, by all appearances, became detectable by week 35. Thus, in the works of these authors, it was shown that the perineurial barrier in developing peripheral nerves matures quite late in embryogenesis, in the third trimester. In the earlier period, the barrier remains permeable.
Regarding the origins of perineurial cells in embryogenesis, there is no consensus in the literature. Cells of the following embryonic primordia are considered as the sources of perineurium development: neural crest and ectomesenchyme, mesenchyme (mesoderm) and neural tube.
The neural crest as the origins of perineurial cells. Initially, it was believed that perineurial cells are of neural origin and descend from the cells of the neural crest [29]. During the embryogenesis of vertebrates, the neural crest derives from the dorsal part of the neural tube. Epidermal neural crest stem cells (NCSCs) are multipotent and give rise to many neural and non-neural structures [88–90]. It has recently been shown that some neural crest derivatives, e.g., Schwann cell precursors, retain their multipotency even after birth and can differentiate into both neural and mesenchymal cells [91]. As for perineurial cells, there is no complete clarity on the possibility of their descent from NCSCs. For instance, Joseph et al. (2004) [92] studied peripheral nerve development using a Cre-Lox recombination technology to trace the fate of migrating cells. They found that in the developing nerve, NCSCs mainly differentiate into Schwann cells (more than 75%) and endoneurial fibroblasts. The authors emphasized that neither perineurial cells, nor pericytes, nor endothelial cells derive from NCSCs. However, in the summary table of the obtained results, it was pointed out that a small part of perineurial cells (about 3%), in the area immediately adjacent to the endoneurium, may nevertheless be derived from NCSCs.
Anderson et al. [83] set up original experiments using a three-dimensional model of the developing nerve to prove the origin of the perineurium from NCSCs. The dorsal root ganglia of rat embryos were cultured in a capillary alginate gel (Capgel™). Ganglion explants, when placed in Capgel, retained their viability for 35 days and comprised neurons and satellite glial cells. The axons of ganglion cells grew into parallel capillaries 30–50 µm in diameter. Laminin, an extracellular matrix protein that promotes axonal growth, was applied onto the inner surface of the gel capillaries. The axons of sensory neurons grew through the capillaries at a distance of 1 cm as axonal fascicles. A study of the axonal fasciculation dynamics revealed that, along with axons and Schwann cells, flattened cells formed in the capillary along the periphery of the fascicle. Using immunohistochemical methods, it was shown that these cells contained claudin-1, GLUT1 (a mature perineurium marker), and type IV collagen (a basement membrane marker). The authors believed that, since the cultures contained only a dorsal root ganglion explant whose cells derive from the neural crest, it is quite likely that at least some cells of the definitive perineurium in this system also originate from NCSCs.
It is well known that some part of the mesenchyme, called ectomesenchyme or mesoectoderm [93, 94], forms from NCSCs. The ectomesenchyme gives rise to adipocytes, chondrocytes, osteocytes, smooth muscle cells, pericytes, cutaneous facial fibroblasts, and many other cell types [95, 96]. It was previously believed that the ectomesenchyme engenders the brain and spinal cord meninges, as well as the perineurial sheath. It has now been established that the brain meninges derive from the cells of the cranial neural crest, whereas the spinal cord meninges are of mesodermal origin [43, 90]. This property also extends to the perineurium: some of its cells form from the ectomesenchyme (i.e., they are neural crest derivatives), while the other part is of mesodermal origin.
Mesodermal origin of perineurial cells. The mesodermal (mesenchymal) origin of perineurial cells follows from the results of studies conducted in vitro. According to some authors, during long-term culturing, perineurial cells adopt morphological features inherent to fibroblasts and become fibroblast-like [97, 98]. However, when comparing perineurial cells with fibroblasts, Kusenas [29] fairly noted that they differ significantly from the latter. For example, they are covered by a basement membrane on both sides, while fibroblasts on the one side only. Furthermore, they are interlinked via tight junctions, thus forming characteristic layers not inherent to fibroblasts in any organs. The author emphasized yet another distinctive feature of perineurial cells: a single perineurial cell can envelope a small axonal fascicle, which is also not typical for fibroblasts. Nevertheless, the original in vitro studies [99] demonstrated a close relationship of fibroblasts (more precisely, their precursors) with perineurial cells. When co-culturing embryonic fibroblasts, obtained from the cranial periosteum, with Schwann cells and sensory neurons [99], it was found that a sheath similar to the perineurium formed around the nerve fascicles developing in the explants. The authors’ task was to find out from which cells of this culture the perineurium can form: Schwann cells (neural crest derivatives) or fibroblasts (mesodermal derivatives). For this purpose, Schwann cells and fibroblasts were alternately labeled with retrovirus. It was shown that developing perineurial cells contained a label only provided that fibroblasts, but not Schwann cells, were pre-labeled. Consequently, under the given in vitro conditions, perineurial cells differentiated from fibrobasts, but not from Schwann cells or their precursors.
One more evidence for the mesodermal origin of perineurial cells is the Renaut corpuscle. These cylindrical or rounded structures, described by the French physician Joseph Louis Renaut (1844–1917) as early as the 19th century, are formed from the inner layer of the perineurium through its invagination into the endoneurium [17, 100]. Renaut corpuscles occur in peripheral nerves of humans and animals (more often in horses and donkeys), and their number increases with compression and some other neuropathies. Renaut bodies contain typical structural components of connective tissue: fibroblasts, glycosaminoglycans, basement membranes and elastic fibers. It was shown immunohistochemically that Renaut bodies immunopositive to the perineurial markers EMA and GLUT1, while being immunonegative to such a Schwann cell marker as the S100 protein.
Current studies on the development of new technologies to stimulate the regeneration of peripheral nerves using stem cells (neural stem/progenitor cells, mesenchymal stem cells obtained from various sources, hair follicle stem cells, etc.) can also serve as evidence of the mesodermal origin of perineurial cells [see reviews 101–103]. Using various methods of assessing the degree of peripheral nerve regeneration (behavioral tests, electrophysiological nerve conduction studies, histomorphometric analysis), it has been shown that such a therapy can indeed promote the regeneration of the recipient’s nerve. These studies are not only of great applied significance, but also make it possible to reveal the differentiation potential of transplanted cells developing under conditions of an altered microsurrounding. Some researchers apply NCSCs for experimental cell therapy [104–106]. It was found that most of the transplanted cells differentiate into Schwann cells and express their specific markers (S100β, GFAP) [104, 105]. Some studies have shown that a part of the transplanted NCSCs can differentiate not only into S100β+ Schwann cells, but also into FSP1+ fibroblasts and CD31+ endotheliocytes of growing blood vessels [104]. At the same time, there are no works demonstrating that transplanted NCSCs are able to differentiate into perineurial cells. When using bone marrow mesenchymal stem cells for cell therapy of an injured nerve, it was shown that some of them can migrate into the perineurium of a recipient rat and differentiate into perineurial cells [107, 108]. This argues in favor of the fact that at least some of the perineurial cells may be of mesodermal origin.
Neuroectodermal origin of perineurial cells. When studying migration of perineurial cell precursors during zebrafish embryogenesis, it was found that these cells take their origin from the ventral region of the developing spinal cord and migrate to the periphery along with the growth of ventral root fibers [32, 109]. It was also established that migration and further differentiation of the precursors are regulated by Notch-dependent signaling pathways [32].
In zebrafish, the perineurium of the motor nerve consists of Nkx2.2a-containing cells derived from the CNS [31, 109]. This has been recently reconfirmed in a study of glial cells in the motor exit point, carried out on the Zebrabow (zebrafish Brainbow) transgenic construct, a multispectral cell labeling tool designed to trace and analyze clones) [84]. Using this transgenic model, it was proved that a certain population of glial cells in the spinal nerve roots, which originates from Nkx2.2a+ precursors of the ventral spinal domain, migrates from the CNS during embryogenesis. This peripheral glial subpopulation of central origin forms the perineurium along motor nerves.
It has recently been established that not only in fish, but also in mammals, a part of perineurial cells derives from Nkx2.2+ precursors residing in the embryonic spinal cord [82]. Using transgenic mice, it was found that at E15.5, Nkx2.2+ cells are located in close proximity to α-tubulin-containing axons of motor neurons at the periphery. Moreover, it was noted that Nkx2.2 knockout mice exhibit perineurial defects. It was concluded that a part of the ventral root perineurium originate from Nkx2.2+ precursors situated in the ventral region of the spinal cord (presumably, the p3 progenitor domain). Perineurial cells originating from CNS cells exit the spinal cord through the nascent motor exit point and combine with their peripherally generated counterparts, forming a continuous sheath around motor nerves [43]. Importantly, such cells are only characteristic of the perineurium in the ventral root of axons from motor neurons, while the origin of dorsal root perineurial cells remains unknown [29].
Thus, the perineurium is a unique structure, whose cells derive from different embryonic primordia [29, 82, 83, 110]. Nevertheless, in different species of animals and humans, the perineurium and its components share a similar structure, which is due to similar functions performed by these cells.
FUNCTIONS OF THE PERINEURIUM
Protective function. One of the major functions of the nerve sheaths is the mechanical protection of nerve fibers, which permanently experience mechanical loads due to changes in body position, especially limbs. The structure of nerves and their sheaths allows controlling the local environment of nerve fibers and modulating physical loads [37]. Nerves have the ability to withstand stretching and contraction, sliding (excursion) and compression [111]. Changes in the biomechanical properties of nerves were studied under different conditions: in varying limb positioning, during motion, in late ontogeny, as well as in pathology (diabetes mellitus) [111]. The perineurium modulates external influences, protecting the nerve from mechanical injury, and provides its mechanical strength [17]. This is reflected in its structure: maximum thickness of the perineurial sheath (i.e., the largest number of cell layers therein) occurs in the nerves that experience maximum stress, as well as at the sites where nerve trunks ramify [37]. Perhaps one of the adaptations to mechanical loads observed during motion and changes in body positioning is the presence of contractile filaments and vesicles in the cytoplasm of perineural cells [18, 112].
The perineurium also performs an immunoprotective function. Its cells express a number of proteins that regulate the compliment system, such as inhibitors of the complement system (C1IHN and C4b-binding protein), inhibitors of the complement membrane attack complex (glycoprotein CD59), and the complement decay-accelerating factor (DAF) [113, 114].
Nerve homeostasis maintenance. Perineurial cells interconnected via tight junctions in concert with endotheliocytes of endoneurial capillaries create the environment needed for the functioning of nerve fibers and help maintain the required pressure of the endoneurial fluid, 2–3 mm Hg [17, 37]. When the capillaries are damaged due to trauma, altered pressure of the endoneurial fluid leads to hyperfusion, ischemia, Schwann cells and axon injury. Excess fluid removal occurs very slowly, since the endoneurium lacks lymphatic vessels [37].
Barrier function. Histo-hematological barriers are described in various organs; they include the BBB, blood–ocular, blood–testis and other barriers. The formation of histo-hematological barriers in any organ involves both cellular and non-cellular components: endotheliocytes, pericytes, basement membranes, pericapillary space, and cells of the organs themselves [115]. The barrier function of the perineurial sheath of peripheral nerves was discovered in the second half of the past century [30, 47, 116]. The blood–nerve barrier that occurs in the PNS organs is also called by some authors the “blood–nerve interface” [49]. It has now been established that the main components of the blood–nerve barrier in the PNS organs are the inner perineurial layers, which control the flow of interstitial fluid elements between the epineurium and endoneurium, and the endoneurial microvessels, which control the penetration of ions, dissolved nutrients, water, macromolecules and leukocytes from the bloodstream into the endoneurial space [19, 66]. The endoneurial space extends from the spinal root to the peripheral nerve endings and is protected from the penetration of substances that can impair or block nerve conduction, as well as from the penetration of potential carcinogens [17].
Tracer studies of the perineurial barrier permeability using ferritin [117] or horseradish peroxidase [118, 119] showed that tracer molecules are unable to penetrate through the perineurium or, at best, reach only its most superficial layer [118]. According to some authors, a high selectivity of the perineurial barrier is due to the fact that this structure is multilayer [38]. Nevertheless, in terms of permeability, the nerve-tissue barrier in the PNS is inferior to the BBB. The perineurial barrier is most permeable in the area of nerve endings, where relatively large molecules can penetrate into the axoplasm, and at the sites of penetration of epineurial vessels passing through the perineurium to the endoneurium [17, 38, 49]. Besides, the barrier is absent in the dorsal spinal roots and in some autonomic ganglia [17]. The absence of a laminar perineurium, and hence of the perineurial barrier, characterizes the ganglia of nerve plexuses located in the walls of the gastrointestinal tract organs.
The relevance of studying the molecular mechanisms that regulate the permeability of the blood–nerve barrier is explained by the fact that its disruption leads to severe diseases. The main focus of current studies is on the endothelial component of the blood–nerve barrier. It has been shown that tight junctions between endotheliocytes of endoneurial blood vessels are formed by the same proteins as the contacts between adjacent perineurial cells, such as occludin, claudin-5, ZO-1 and ZO-2 [120]. Recent studies carried out on cultures of human endoneurial endotheliocytes enabled the identification of 133 molecules of the intercellular junctional complex in these cells. Under in situ conditions, such proteins as catenin α1 (CTNNA1), cadherin-5 (CHD5), cadherin-6 (CDH6), Cldn4, Cldn5, protocadherin-1, and vesatin have been identified in the endothelium of endoneurial microvessels of the human sural nerve [121]. Using confocal laser microscopy, it was found that Cldn4 is associated with tight junctions of the blood–nerve barrier, CDH5 with adhesive contacts. The proteins ZO-1 and Cldn5 are identified as scaffold proteins that bind endothelial cell membranes to the cytoskeleton [19].
Current data obtained on in vitro and in situ models allow several hypotheses to be advanced about the influence that Schwann cells, pericytes and other structural nerve elements exert on the permeability of the blood–nerve barrier. For instance, endothelial cells of endoneurial vessels have receptors for growth and neurotrophic factors, such as the glial cell line-derived neurotrophic factor (GDNF; GFRα1), vascular endothelial growth factor (VEGF), basic fibroblast growth factor (BFGF), and transforming growth factor-β (TGF-β) [120], which are synthesized by such endoneurial cells as neurolemmocytes, pericytes, mast cells and fibroblasts. There is a hypothesis that GDNF-synthesizing Schwann cells regulate the permeability of the blood–nerve barrier through the RET/MAPK (receptor tyrosine kinase/mitogen-activated protein kinase signaling pathway [122]. It is hypothesized that Schwann cells influence the formation of the blood–nerve barrier during ontogeny through GDNF production; GDNF also induces the specialization of perineurial cells [19]. The functioning of the blood–nerve barrier is provided by transporter proteins (509 transcripts), including GLUT1, monocarboxylate-1, creatine and other transporters [120].
Normal functioning of the blood–nerve barrier requires endoneurial water balance, which is regulated by aquaporins, integral membrane proteins that form pores in cell membranes (AQP1, AQP3, and AQP11) [120]. AQP1 production occurs not only by endotheliocytes and pericytes, but also by cells of the perineural sheath. The involvement of immunocompetent cells in the regulation of the nerve barrier function has been noted, but this issue requires further investigation.
Nerve injury impairs the blood–nerve barrier and alters the function of endothelial cells in endoneurial microvessels [66, 123]. It has been shown that the disruption of the vascular barrier entails Hedgehog signaling pathway dysfunction as early as 1 h after injury, leading to a change in the expression of Cldn5 and other molecules [124]. Moreau et al. [123], using a model of chronic nerve compression, showed that the Wnt/β-catenin signaling pathway is also involved in impairing the blood–nerve barrier in interaction with the activation of the toll-like receptor 4 (TLR4). It was established that activation of the Wnt/β-catenin pathway and inhibition of Hedgehog signaling in the endothelium of endoneurial microvessels lead to a chronic impairment of the blood–nerve barrier after nerve injury. Importantly, impaired permeability is observed before macrophages penetrate into the damaged nerve during Wallerian degeneration. Changes in the synthesis of the adhesive contact protein cadherin and the simultaneous suppression of the synthesis of tight junction proteins Cldn-1, Cldn-5 and occludin precede the infiltration of immune cells and toxic molecules during local inflammation and the development of neuropathic pain.
Metabolic function. The perineurium is a metabolically active structure [18, 62]. Numerous basement membranes in its composition provide a high selectivity of penetration of various molecules into the endoneurium from the epineurium [75]. One of the methods to transport the necessary molecules across the perineurium is transcytosis (endo- and exocytosis within the same cell is typical for flattened cells, e.g., endotheliocytes [125]), which was confirmed by autoradiography, electron microscopy and tracer studies [62, 126, 127].
Morphogenetic function. During embryogenesis, the precursors of nascent peripheral nerves (precursors of neurons, Schwann cells, endoneurial fibroblasts and perineurial cells) are closely interrelated. It has been shown that the development and differentiation of the perineurium in embryogenesis is influenced by Schwann cells. The differentiation of perineurial cells, formation of a typical laminar structure of the perineurium, as well as the formation of the blood–nerve barrier, owe a signaling molecule “desert hedgehog” (Dhh), which is expressed by Schwann cells [128, 129]. In turn, perineurial cells themselves also affect the development and functioning of Schwann cells. It has been shown that genetic elimination of perineurial cells at an early ontogenetic stage leads to a hindrance in the development of Schwann cells and to motor nerve defects [109]. The interplay between perineurial and Schwann cells at different stages of motor nerve development has been demonstrated in knockout animals with impaired Notch signaling [32, 82]. Perineurial cells are indispensable not only for the survival and differentiation of Schwann cells, but also for the implementation of their axon-myelinating function [32].
The morphogenetic function of the perineurium also manifests itself during the period when the axons of developing motor neurons reach the periphery [31]. At the CNS–PNS interface, perineurial cells perform the functions similar to those of boundary cap cells: they prevent the migration of motor neuron precursor bodies beyond the CNS, control the barrier, and participate in the regulation of axon guidance [82, 130].
Involvement in nerve regeneration. As noted above, structural changes in peripheral nerves during reparative regeneration were first described in classical neurobiological studies by A. Waller and S. Ramón y Cajal. Later, owing to electron microscopy, the ultrastructural details of changes that occur in the nerve after injury were elucidated. A large body of studies has shown that Schwann cells are essential participants in the processes of both degeneration and regeneration of nerve fibers. Following nerve injury, they undergo dedifferentiation, proliferate, produce growth factors, extracellular matrix proteins and cytokines, ensuring the growth of regenerating axons (see reviews: [2, 11, 131, 132]). At the same time, much less attention is paid to the response of perineurial cells to nerve injury.
In a rabbit model of tibial nerve injury, it was shown that perineurial cells respond to nerve injury by detaching from one another and their basement membranes and assuming the fibroblast morphology. After that, they surround small fascicles of regenerating axons and restore their structure [81].
When studying the perineurium in the distal segment of the mouse phrenic nerve after clamping, it was shown that in the first week after injury (during Wallerian degeneration), some of the perineurial cells looked hypertrophied [33]. Many cells proliferated, and mitotic figures were observed for one week. Intracellular microcavities were detected in the cytoplasm of perineurial cells due to an increase in the number of pinocytotic vesicles. The perineurial cells adjacent to the endoneurium contained lipid droplets, the number of which increased over time.
To study the response of the perineurium to nerve injury, a convenient model, called the “perineurial window”, has been developed [134]. This model makes it possible to study the nerve response to a limited perineurial injury, which leads to demyelination of nearby nerve fibers and impairment of nerve conduction [47]. There is evidence that the microsurrounding influences the regenerative potencies of the perineurium. For example, when a nerve segment is transplanted into an injured spinal root, the perineurium does not regenerate, but when a root segment is transplanted into a nerve, it regenerates [47, 135].
In recent studies on a zebrafish laser nerve transection, it has been shown that perineurial cells are among the first (along with Schwann cells) to respond to nerve injury. They form a “bridge” that links the proximal and distal segments of the nerve trunk yet before the onset of axonal fragmentation at the distal end [29, 136].
According to current data, reparative regeneration of the perineurium is associated with proteins of intercellular junctions, the amount of which decreases after injury. At the same time, there occurs a suppression of the synthesis of Cldn1, Cldn5, ZO-1, and other proteins of intercellular junctions [66, 137]. It was shown that 7 days after nerve injury, the immunoreactivity to occludin and ZO-1 was restored. The restoration of the immunoreactivity to connexin 43 was only observed after 21 days. It was noted that the restoration of gap junctions lags behind that of tight junctions [137].
A study of the molecular mechanisms of nerve regeneration showed that, despite the fact that perineurial cells actively exploit Notch signaling during the ontogenetic development of nerves, this mechanism is not implicated in reparative regeneration [32].
The regenerative potential of perineurial cells can be traced when analyzing the works performed on the clinical material of nerve pathology. It has been shown that perineurial cells are able to proliferate and form benign and malignant tumors (perineuromas) [17, 138]. In addition, they enter into the composition of such heterogeneous tumors as neurofibromas, schwannomas, and malignant tumors of the nerve sheaths. Immunolabeling of Cldn1, EMA, GLUT1 and other perineurial markers is used to identify perineurial cells in neurofibromas, which also include Schwann cells and fibroblasts [139, 140]. The location of perineurial cells in neurofibromas is not random; the perineurium forms around rudimentary nerve fascicles [139], indicating that, like in ontogenesis, the formation of perineurial cells occurs under the influence of the nascent nerve fibers and surrounding Schwann cells. It is hypothesized that, in neurofibromatosis-1, a disruption of intercellular junctions between perineurial cells leads to an impairment of their barrier function and penetration of growth factors and cytokines from the nearby tissues into the perineurium, which stimulate proliferation and tumor growth of perineurial cells [139].
Phagocytic function. Phagocytosis is the most important cellular process for peripheral nerves after their injury. Nerve injury in the distal segment of the nerve triggers Wallerian degeneration, including the destruction of axons and their myelin sheaths. In order to implement subsequent regeneration of nerve fibers, the endoneurium needs first to be cleared from the axonal and myelin degradation products, which is mainly executed by macrophages of hematogenous origin [141]. Resident macrophages and Schwann cells are also involved in phagocytosis of myelin debris [11, 142]. In some studies, it was shown that perineurial cells can also be implicated in this process [136, 141, 143] as demonstrated in studies carried out on different experimental models (cold injury, LPS administration, nerve clamping, etc.) [143]. There are suggestions that perineurial cells may transform into macrophages when involved in phagocytosis [7]. In some ultrastructural studies, the cytoplasm of some perineurial cells was found to contain the vacuoles [141] and lipid droplets [143] characteristic of phagocytic cells, although there is an assumption that these cells may represent macrophages migrating from the endoneurium to epineurium during nerve injury [18]. The issue of the phagocytic function of perineurial cells requires further clarification.
CONCLUSION
This review article covers a range of issues related to the features of one of the sheaths of the nerve trunks, the perineurium. Here we summarize the data available in the literature on the structure and functions of perineurial cells, their phylo- and ontogenetic origin, responses to injury, and possible ways to identify these cells using immunohistochemical reactions. An analysis of the available literature has shown that, despite the fact that the nerve sheaths have been an object of studies for several decades, many issues regarding the structural and functional features of the perineurium still remain unresolved. For example, there is not enough information about the evolutionary developmental patterns of the perineurium. It has been shown that in the vertebrate lineage, the perineurial sheath is a universal structure inherent to all nerves. In the lineage from amphibians to mammals, its structure undergoes complication as manifested in an increase in the number of perineurial cell layers. Electron microscopy showed that the ultrastructural features of the perineurial sheath are similar across different species. At the same time, studies of the perineurial sheath using modern immunohistochemical methods were carried out only on humans and laboratory animals, and practically were not carried out in representatives of other species. This is probably due to the fact that selective immunohistochemical markers specific exclusively to perineurial cells have not yet been found. Most of the antigens used for the immunohistochemical identification of perineurial cells are proteins of intercellular tight junction.
In-depth structural studies of the perineurium using modern methods and experimental in vitro and in vivo models made it possible to expand the idea of the perineurium as just a protective sheath and to elucidate some of the regulatory mechanisms of the blood–nerve barrier. When analyzing the data available in the literature, it has turned out that perineurial cells are responsible not only for mechanical, but also immunological protection of the nerve, are involved in the regulation of metabolic processes, play an important morphogenetic role in early ontogeny, and are actively implicated in the reparative regeneration of nerves.
This review presents the data available in the modern literature on the morphofunctional features of the cells constituting the perineurial sheath of spinal roots and ganglia in comparison with the perineurium of the nerve trunk. We analyze evidence of the ontogenetic origin of perineurial cells from different embryonic primordia. Various experimental models have shown that the perineurium can descend from neural crest cells, mesoderm, and neuroectoderm. For a long time, the issue of the origin of perineurium was considered disputable and controversial. Currently, many researchers have come to the conclusion that the perineurium is a unique structure consisting of cells that are structurally and functionally similar but have different origins. It is not yet clear what determines from which embryonic primordium the perineurium of different nerves, spinal roots and ganglia is derived, and whether there are distinctive features of the histoblastic potencies of cells derived from different primordia. The data published over the past few years indicate that the cells of the ventral root perineurium derive from the neuroectoderm and may therefore belong to peripheral glia. At the same time, there is no idea about the origins of dorsal root perineurial cells. Further studies aimed at elucidating the peculiarities of the origin of these cells in mammals and humans may lead to a revision of ideas on the origin of peripheral glia. An analysis of evidence available in the literature on the origin of perineurial cells from different embryonic primordia allows a conclusion that the perineurium consists of different cell populations. All the aforesaid indicates the need to continue versatile research in this direction.
One of the most important functions of the perineurium is its involvement in the formation of the blood–nerve barrier. Along with endoneurial microvascular endotheliocytes, the the perineurium is involved in the creation of a microenvironment favorable for the growth and development of nerve fibers, as well as in the maintenance of endoneurial homeostasis. Currently, there is not enough information about the molecular mechanisms that regulate this barrier. There are virtually no data on the formation of the blood–nerve barrier across different animal species. Hopefully, a comparative investigation of the molecular mechanisms regulating the blood–nerve barrier will provide deeper insight into the processes underlying the sophistication of this barrier during evolution.
It should be noted that a study of the blood–nerve barrier is of great practical importance. It has been shown that impaired barrier function precedes the development of traumatic and metabolic neuropathies, as well as tumors. In this regard, unraveling the mechanisms regulating the blood–nerve barrier will promote further development of new therapeutic approaches to treat chronic peripheral neuropathies and neuropathic pain.
REFERENCES
Bersnev VP, Hamzaev RI, Boroda JuI (2009) Results of using an epineural suture of the sciatic nerve. Vestnik hirurgii im. I.I. Grekova 168 (1): 61–63 (In Russ).
Shchanitsyn IN, Ivanov AN, Bazhanov SP, Ninel VG, Puchin’jan DM, Norkin IA (2017) Stimulation of peripheral nerve regeneration: current status, problems and perspectives. Uspekhi fiziologicheskih nauk 48(3): 92–112 (In Russ).
Shchudlo NA, Borisova IV, Shchudlo MM (2013) Morphometric assessment of the effectiveness of post–traumatic regeneration of peripheral nerves using single and repeated courses of electrostimulation. Neuroscience and Behavioral Physiology 43(9): 1097–1101. https://doi.org/10.1007/s11055-013-9855-4
Litvinenko IV, Odinak MM, Zhivolupov SA, Bulatov AR, Rashidov NA, Bardakov SN (2018) Clinical and instrumental characteristics of traumatic lesions of peripheral nerves of limbs. Vestnik Rossiyskoi Voyenno-meditsinskoi akademii 3 (63): 50–56 (In Russ).
Nisht AYu, Chirskii VS, Fomin NF (2019) Morphological foundations of restoration of motor innervation in injuries of peripheral nerves. Journal of Anatomy and Histopathology 8 (4): 66–73 https://doi.org/10.18499/2225-7357-2019-8-4-66-73
Pannese E (1981) The satellite cells of the sensory ganglia. Adv Anat Embryol Cell Biol 65: 1–111. https://doi.org/10.1007/978-3-642-67750-2
Nozdrachev AD, Chumasov EI (1999) Peripheral Nervous System. Nauka, SPb (In Russ).
Chelyshev YuA, Saitkulov KI (2000 Development, phenotypic characteristics and communication of Schwann cells). Uspekhi fiziologicheskih nauk 31 (3): 54–69 (In Russ).
Zochodne DW (2008) Neurobiology of peripheral nerve regeneration. Cambridge, New York, Melbourne, Madrid, Cape Town, Singapore, Sao Paulo: Cambridge University Press.
Reina MA, Arriazu R, Collier CB, Sala-Blanch X, Izquierdo L, de Andrés J (2013) Electron microscopy of human peripheral nerves of clinical relevance to the practice of nerve blocks. A structural and ultrastructural review based on original experimental and laboratory data. Rev Esp Anestesiol Reanim 60(10): 552–562. https://doi.org/10.1016/j.redar.2013.06.006
Petrova ES (2019) Current views on Schwann cells: development, plasticity, functions. J Evol Biochem Phys 55: 433–447. https://doi.org/10.1134/S0022093019060012
Chumasov EI, Kolos EA, Petrova ES, Korzhevskii DE (2020) Immunohistochemistry of the Peripheral Nervous System. SpecLit, SPb.
Bhatheja K, Field J (2006) Schwann cells: origins and role in axonal maintenance and regeneration. Int J Biochem Cell Biol 38: 1995–1999. https://doi.org/10.1016/j.biocel.2006.05.007
Salzer JL (2015) Schwann cell myelination. Cold Spring Harb. Perspect Biol 7 (8): a020529. https://doi.org/10.1101/cshperspect.a020529
Shanthaveerappa TR, Bourne GH (1966) Perineural epithelium: a new concept of its role in the integrity of the peripheral nervous system. Science 154(3755): 1464–1467.
Kundalić B, Ugrenović S, Jovanović I, Stefanović N, Petrović V, Kundalić J, Stojanović V, Živković V, Antić V (2014) Morphometric analysis of connective tissue sheaths of sural nerve in diabetic and nondiabetic patients. Biomed Res Int 2014: 870930. https://doi.org/10.1155/2014/870930
Pinã-Oviedo S, Ortiz-Hidalgo C (2008) The normal and neoplastic perineurium. A review. Adv Anat Pathol 15:147–164. https://doi.org/10.1097/PAP.0b013e31816f8519
Berthold C-H, Fraher JP, King RHM, Rydmark M (2005) Microscopic anatomy of the peripheral nervous system. In: Dyck PJ, Thomas PK (Eds) Peripheral Neuropathy. Elsevier Health Sciences. pp 35–91.
Ubogu EE (2020) Biology of the human blood-nerve barrier in health and disease. Exp Neurol 328: 113272. https://doi.org/10.1016/j.expneurol.2020.113272
Barros CS, Franco SJ, Müller U (2011) Extracellular matrix: functions in the nervous system. Cold Spring Harb Perspect Biol 3(1):a005108. https://doi.org/10.1101/cshperspect.a005108
Bove GM, Light AR (1995) Calcitonin Gene-Related peptide and peripherin immunoreactivity in nerve sheaths. Somatosensory and Motor Research 12 (1): 49–57. https://doi.org/10.3109/08990229509063141
Reina MA, Boezaart AP, Tubbs RS, Zasimovich Y, Fernández-Domínguez M, Fernández P, Sala-Blanch X (2019) Another (internal) epineurium: beyond the anatomical barriers of nerves. Clin Anat 33(2):199–206. https://doi.org/10.1002/ca.23442
Sala-Blanch X, Reina MA, Ribalta T, Prats-Galino A (2013) Sciatic nerve structure and nomenclature: epineurium to paraneurium: is this a new paradigm? Reg Anesth Pain Med 38 (5):463–465. https://doi.org/10.1097/AAP.0b013e3182a1b6c5
Zatolokina MA (2016) Morphogenesis of Changes in the Paraneural Connective Tissue Structures of Peripheral Nerves in an Evolutionary Aspect. KGMU, Kursk (In Russ).
Murthy NK, Spinner RJ (2020) Letter to the editor: the paraneurium (circumneurium) and its clinical implications with benign and malignant nerve lesions. Clin Anat 34(8):1133-1134. https://doi.org/10.1002/ca.23639
Reina MA, Boezaart A, Nin OC, Zasimovich Y, Sala-Blanch X (2020) Yet another perineural layer: so what? Reg Anesth Pain Med 45(6):483–484. https://doi.org/10.1136/rapm-2019-100765
Krnjevic K (1954) The connective tissue of the frog sciatic nerve. Q J Exp Physiol Cogn Med Sci 39(1): 55–72. https://doi.org/10.1113/expphysiol.1954.sp001048
Marani E, Lakke EAJF (2012) Peripheral Nervous System. In: Mai JK, Paxinos G (eds) The human nervous system. Elsevier, Amsterdam, pp 82–140.
Kucenas S (2015) Perineurial glia. Cold Spring Harb Perspect Biol 7(6): a020511. https://doi.org/10.1101/cshperspect.a020511
Shanthaveerappa TR, Bourne GH (1963) Demonstration of perineural epithelium in whale and shark peripheral nerves. Nature197: 702–703. https://doi.org/10.1038/197702a0
Kucenas S, Takada N, Park HC, Woodruff E, Broadie K, Appel B (2008) CNS-derived glia ensheath peripheral nerves and mediate motor root development. Nat Neurosci 11:143–151. https://doi.org/10.1038/nn2025
Binari LA, Lewis GM, Kucenas S (2013) Perineurial glia require Notch signaling during motor nerve development but not regeneration. J Neurosci 33(10):4241–4252. https://doi.org/10.1523/JNEUROSCI.4893-12.2013
Du Plessis DG, Mouton YM, Muller CJ, Geiger DHJ (1996) An ultrastructural study of the development of the chicken perineurial sheath. Anat 189 (Pt 3): 631–641.
Server A, Reina MA, Boezaart AP, Prats-Galino A, Esteves Coelho M, Sala-Blanch X (2018) Microanatomical nerve architecture of 6 mammalian species: Is trans-species translational anatomic extrapolation valid? Reg Anesth Pain Med 43(5):496–501. https://doi.org/10.1097/AAP.0000000000000772
Chumasov EI (1975) On the structure of the perineurium of the peripheral nervous system. Arch of Anatomy, Histology and Embryology 68 (4): 29–34 (In Russ).
Takebe K, Nio-Kobayashi Y, Takanashi-Iwanaga H, Iwanaga T (2006) Histochemical demonstration of a monocarboxylate transporter in the mouse perineurium with special reference to GLUT1. Biomedical Res 29 (6): 297–306. https://doi.org/10.2220/biomedres.29.297
Topp KS, Boyd BS (2012) Peripheral nerve: from the microscopic functional unit of the axon to thebiomechanically loaded macroscopic structure. J Hand Ther 25(2):142–151; quiz 152. https://doi.org/10.1016/j.jht.2011.09.002
Dolzhikov AA, Dolzhikova IN (2018) Perineurium of peripheral nerves: fundamental and applied issues of its morphology and functions. Aktual’nye problemy gumanitarnykh i estestvennykh nauk 9: 54–62 (In Russ).
Dixon JS, Jen PY, Gosling JA (1998) Immunohistochemical characteristics of human paraganglion cells and sensory corpuscles associated with the urinary bladder. A developmental study in the male fetus, neonate and infant. J Anat 192 (3): 407–415. https://doi.org/10.1046/j.1469-7580.1998.19230407.x
Vega JA, Del Valle ME, Haro JJ, Naves FJ, Calzada B, Uribelarrea R (1994) The inner-core, outer-core and capsule cells of the human Pacinian corpuscles: an immunohistochemical study. Eur J Morphol 32(1):11–18.
Banin VV, Bykov VL (ed) (2009) Terminologia histological. International Terms in Human Cytology and Histology with an Official List of Russian Equivalents. GEOTAR-Media, M. (In Russ).
Matejčík V, Haviarová Z, Kuruc R, Šteňo A, Šteňo J (2019) The composition and structure of peripheral nerves. In: Intraspinal Variations of Nerve Roots. Springer, Cham, pp 3–13.
Suter TACS, Jaworski A (2019) Cell migration and axon guidance at the border between central and peripheral nervous system. Science 365(6456):eaaw8231. https://doi.org/10.1126/science.aaw8231
Andres KH (1967) On the fine structure of the arachnoidea and dura mater of mammals. Z Zellforsch Mikrosk Anat 79(2): 272–295.
McCabe JS, Low FN (1969) The subarachnoid angle: an area of transition in peripheral nerve. Anat Rec 164 (1):15–33. https://doi.org/10.1002/ar.1091640102
Haller FR, Low FN (1971) The fine structure of the peripheral nerve root sheath in the subarachnoid space in the rat and other laboratory animals. Am J Anat 131(1):1–19. https://doi.org/10.1002/aja.1001310102
Umovist MN, Tchaikovsky YB (1987) Modern concepts of the structure and function of the nerve sheaths. Archive of anatomy, histology and embryology 1: 98–96 (In Russ).
Bechter K, Schmitz B (2014) Cerebrospinal fluid outflow along lumbar nerves and possible relevance for pain research: case report and review. Croat Med J 55(4): 399–404. https://doi.org/10.3325/cmj.2014.55.399
Mizisin AP, Weerasuriya A (2011) Homeostatic regulation of the endoneurial microenvironment during development, aging and in response to trauma, disease and toxic insult. Acta Neuropathol 121 (3): 291–312. https://doi.org/10.1007/s00401-010-0783-x
Pettersson CA (1993) Sheaths of the spinal nerve roots. Permeability and structural characteristics of dorsal and ventral spinal nerve roots of the rat. Acta Neuropathol 85(2): 129–137. https://doi.org/10.1007/BF00227759
Zakharov A, Papaiconomou C, Djenic J, Midha R, Johnston M (2003) Lymphatic cerebrospinal fluid absorption pathways in neonatal sheep revealed by subarachnoid injection of Microfil. Neuropathol Appl Neurobiol 29(6):563–573. https://doi.org/10.1046/j.0305-1846.2003.00508.x
Frater JL, Hall GS, Procop GW (2001) Histologic features of zygomycosis: emphasis on perineural invasion and fungal morphology. Arch Pathol Lab Med 125 (3): 375–378. https://doi.org/10.1043/0003-9985(2001)125<0375:HFOZ>2.0.CO;2
Dando SJ, Mackay-Sim A, Norton R, Currie BJ, St John JA, Ekberg JA, Batzloff M, Ulett GC, Beacham IR (2014) Pathogens penetrating the central nervous system: infection pathways and the cellular and molecular mechanisms of invasion. Clin Microbiol Rev 27(4): 691–726. https://doi.org/10.1128/CMR.00118-13
Schmitt M, Neubauer A, Greiner J, Xu X, Barth TF, Bechter K (2011) Spreading of acute myeloid leukemia cells by trafficking along the peripheral outflow pathway of cerebrospinal fluid. Anticancer Res 31(6):2343–2345.
Brown IS (2016) Pathology of perineural spread. J Neurol Surg B Skull Base 77(2): 124–130. https://doi.org/10.1055/s-0036-1571837
Reale E, Luciano L, Spitznas M (1976) Freeze-fracture aspects of the perineurium of spinal ganglia. J Neurocytol 5: 385–394. https://doi.org/10.1007/BF01181646
Arvidson B (1979) A study of the perineurial diffusion barrier of a peripheral ganglion. Acta Neuropathol 46(1–2):139–144. https://doi.org/10.1007/BF00684815
Weerasuriya A, Mizisin AP (2011) The blood-nerve barrier: structure and functional significance. Methods Mol Biol 686: 149–173. https://doi.org/10.1007/978-1-60761-938-3_6
Masliukov PM, Emanuilov AI, Madalieva LV, Moiseev KY, Bulibin AV, Korzina MB, Porseva VV, Korobkin AA, Smirnova VP (2014) Development of nNOS-positive neurons in the rat sensory and sympathetic ganglia. Neuroscience 256: 271–281. https://doi.org/10.1016/j.neuroscience.2013.10.013
Nikolaev SI, Gallyamov AR, Mamin GV, Chelyshev YuA (2014) Poly(ε-caprolactone) nerve conduit and local delivery of VEGF and FGF2 genes stimulate neuroregeneration. Bulletin of Experimental Biology and Medicine 157 (1): 155–158. https://doi.org/10.1007/s10517-014-2513-1
Emanuylov AI, Maslyukov PM, Nozdrachev AD (2019) Sympathetic innervation of the heart in early postnatal ontogenesis. Russian Journal of Physiology 105 (9): 1133–1141(In Russ). https://doi.org/10.1134/S086981391909005X
Pummi KP, Heape AM, Grenman RA, Peltonen JT, Peltonen SA (2004) Tight junction proteins ZO-1, occludin, and claudins in developing and adult human perineurium. J Histochem Cytochem 52 (8): 1037–1046. https://doi.org/10.1369/jhc.3A6217.2004
Tsukita S, Tanaka H, Tamura A (2019) The claudins: from tight junctions to biological systems.Trends Biochem Sci 44(2):141–152. https://doi.org/10.1016/j.tibs.2018.09.008
Alanne MH, Pummi K, Heape AM, Grenman R, Peltonen J, Peltonen S (2009) Tight junction proteins in human Schwann cell autotypic junctions. J Histochem Cytochem 57 (6): 523–529. https://doi.org/10.1369/jhc.2009.951681
Hirakawa H, Okajima S, Nagaoka T, Takamatsu T, Oyamada M (2003) Loss and recovery of the blood-nerve barrier in the rat sciatic nerve after crush injury are associated with expression of intercellular junctional proteins. Exp Cell Res 284 (2): 196–210. https://doi.org/10.1016/s0014-4827(02)00035-6
Lux TJ, Hu X, Ben-Kraiem A, Blum R, Chen JT, Rittner HL (2020) Regional differences in tight junction protein expression in the blood-DRG barrier and their alterations after nerve traumatic injury in rats. Int J Mol Sci: 21(1): E270. https://doi.org/10.3390/ijms21010270
Sauer RS, Krug SM, Hackel D, Staat C, Konasin N, Yang S, Niedermirtl B, Bosten J, Günther R, Dabrowski S, Doppler K, Sommer C, Blasig IE, Brack A, Rittner HL (2014) Safety, efficacy, and molecular mechanism of claudin-1-specific peptides to enhance blood-nerve-barrier permeability. J Control Release 185: 88–98. https://doi.org/10.1016/j.jconrel.2014.04.029
Miyamoto T, Morita K, Takemoto D, Takeuchi K, Kitano Y, Miyakawa T, Nakayama K, Okamura Y, Sasaki H, Miyachi Y, Furuse M, Tsukita S (2005) Tight junctions in Schwann cells of peripheral myelinated axons: a lesson from claudin-19-deficient mice. J Cell Biol 169(3): 527–538. https://doi.org/10.1083/jcb.200501154
Reinhold AK, Schwabe J, Lux TJ, Salvador E, Rittner HL (2018) Quantitative and microstructural changes of the blood-nerve barrier in peripheral neuropathy. Front Neurosci 12: 936. https://doi.org/10.3389/fnins.2018.00936. eCollection 2018
Ando-Akatsuka Y, Saitou M, Hirase T, Kishi M, Sakakibara A, Itoh M, Yonemura S, Furuse M, Tsukita S (1996) Interspecies diversity of the occludin sequence: cDNA cloning of human, mouse, dog, and rat-kangaroo homologues. Journal of Cell Biology 133 (1): 43–47. https://doi.org/10.1083/jcb.133.1.43
Mazzeo A, Rodolico C, Monici MC, Migliorato A, Aguennouz M, Vita G (1997) Perineurium talin immunoreactivity decreases in diabetic neuropathy. J Neurol Sci 146 (1): 7–11. https://doi.org/10.1016/s0022-510x(96)00285-7
Jaakkola S, Savunen O, Halme T, Uitto J, Peltonen J (1993) Basement membranes during development of human nerve: Schwann cells and perineurial cells display marked changes in their expression profiles for laminin subunits and beta 1 and beta 4 integrins. J Neurocytol 22(3): 215–230. https://doi.org/10.1007/BF01246360
Nagaoka T, Oyamada M, Okajima S, Takamatsu T (1999) Differential expression of gap junction proteins connexin 26, 32, and 43 in normal and crush-injured rat sciatic nerves. Close relationship between connexin43 and occludin in the perineurium. J Histochem Cytochem 47(7): 937–948. https://doi.org/10.1177/002215549904700711
Stark B, Carlstedt T, Cullheim S, Risling M (2000) Developmental and lesion-induced changes in the distribution of the glucose transporter Glut-1 in the central and peripheral nervous system. Exp Brain Res 131(1):74–84. https://doi.org/10.1007/s002219900300
Muona P, Sollberg S, Peltonen J, Uitto J (1992) Glucose transporters of rat peripheral nerve. Differential expression of GLUT1 gene by Schwann cells and perineural cells in vivo and in vitro. Diabetes 41: 1587–1596. https://doi.org/10.2337/diab.41.12.1587
Muona P, Jaakkola S, Salonen V, Peltonen J (1993) Expression of glucose transporter 1 in adult and developing human peripheral nerve. Diabetologia 36: 133–140. https://doi.org/10.1007/BF00400694
Tserentsoodol N, Shin BC, Koyama H, Suzuki T, Takata K (1999) Immunolocalization of tight junction proteins, occludin and ZO-1, and glucose transporter GLUT1 in the cells of the blood-nerve barrier. Arch Histol Cytol 62(5):459–469. https://doi.org/10.1679/aohc.62.459.
Takebe K, Nio-Kobayashi J, Takahashi-Iwanaga H, Iwanaga T (2008) Histochemical demonstration of a monocarboxylate transporter in the mouse perineurium with special reference to GLUT1. Biomed Res 29(6): 297–306. https://doi.org/10.2220/biomedres.29.297
Achtstätter T, Fouquet B, Rungger-Brändle E, Franke WW (1989) Cytokeratin filaments and desmosomes in the epithelioid cells of the perineurialand arachnoidal sheaths of some vertebrate species. Differentiation. 40(2):129–149. https://doi.org/10.1111/j.1432-0436.1989.tb00822.x
Kovalenko VL, Shevtsov VI, Shchudlo MM, Shchudlo NA (2000) Reactive properties of epi- and perineurium: experimental and morphological basis for nerve suture technique. Bulletin of Experimental Biology and Medicine 130(2): 793–797. https://doi.org/10.1007/BF02766098
Thomas PK, Bhagat S (1978) The effect of extraction of the intrafascicular contents of peripheral nerve trunks on perineurial structure. Acta Neuropathol (Berl) 43: 135–141. https://doi.org/10.1007/BF00685008
Clark JK, O’Keefe A, Mastracci TL, Sussel L, Matise MP, Kucenas S (2014) Mammalian Nkx2.2+ perineurial glia are essential for motor nerve development. Dev Dyn 243(9): 1116–1129. https://doi.org/10.1002/dvdy.24158
Anderson WA, Willenberg AR, Bosak AJ, Willenberg BJ, Lambert S (2018) Use of a capillary alginate gel (CapgelTM) to study the three-dimensional development of sensory nerves reveals the formation of a rudimentary perineurium. J Neurosci Methods 305: 46–53. https://doi.org/10.1016/j.jneumeth.2018.05.003
Fontenas L, Kucenas S (2021) Spinal cord precursors utilize neural crest cell mechanisms to generate hybrid peripheral myelinating glia. Elife 10: e64267. https://doi.org/10.7554/eLife.64267.
Peltonen S, Alanne M, Peltonen J (2013) Barriers of the peripheral nerve. Tissue Barriers 1:e24956. https://doi.org/10.4161/tisb.24956
Sima A, Sourander P (1973) The effect of perinatal undernutrition on perineurial diffusion barrier to exogenous protein. An experimental study on rat sciatic nerve. Acta Neuropathol 24 (3): 263–272. https://doi.org/10.1007/BF00687596
Sima A, Sourander P (1974) The permeability of perineurium to peroxidase after early undernutrition. An ultrastructural study on rat sciatic nerve. Acta Neuropathol 28(1):15–23. https://doi.org/10.1007/BF00687514
Le Douarin NM (1986) Cell line segregation during peripheral nervous system ontogeny. Science 231: 1515–1522
Le Douarin NM, Dupin E (2012) The neural crest in vertebrate evolution. Curr Opin Genet Dev 22(4): 381–389. https://doi.org/10.1016/j.gde.2012.06.001
Etchevers HC, Dupin E, Le Douarin NM (2019) The diverse neural crest: from embryology to human pathology. Development 146(5): dev169821. https://doi.org/10.1242/dev.169821
Petersen J, Adameyko I (2017) Nerve-associated neural crest: peripheral glial cells generate multiple fates in the body. Curr Opin Genet Dev 45: 10–14. https://doi.org/10.1016/j.gde.2017.02.006
Joseph NM, Mukouyama YS, Mosher JT, Jaegle M, Crone SA, Dormand E-L, Lee K-F, Meijer D, Anderson DJ, Morrison SJ (2004) Neural crest stem cells undergo multilineage differentiation in developing peripheral nerves to generate endoneurial fibroblasts in addition to Schwann cells. Development 131(22): 5599–5612. https://doi.org/10.1242/dev.01429
Dupin E, Sommer L (2012) Neural crest progenitors and stem cells: from early development to adulthood. Developmental Biology 366: 83–95. https://doi.org/10.1016/j.ydbio.2012.02.035
Le Douarin NM, Dupin E (2018) The “beginnings” of the neural crest. Dev Biol 444 (1): S3–S13. https://doi.org/10.1016/j.ydbio.2018.07.019
Graham A (2003) The neural crest. Curr Biol 13(10): R381–384. https://doi.org/10.1016/s0960-9822(03)00315-4
Graham A, Begbie J, McGonnell I (2004) Significance of the cranial neural crest. Dev Dyn 229(1): 5–13. https://doi.org/10.1002/dvdy.10442
Chumasov EI (1976) Morphology of perineurium in organotypic culture of sensitive ganglia. In: Tissue Biology. Tartu. 79–82.
Chumasov EI, Konovalov GV (1977) The Morphology of the Nervous Tissue in Culture. Nervous Tissue Culture. Medicina, M, 63–127 (In Russ).
Bunge MB,Wood PM, Tynan LB, Bates ML, Sanes JR (1989) Perineurium originates from fibroblasts: Demonstration in vitro with a retroviral marker. Science 243: 229–231. https://doi.org/10.1126/science.2492115
Kazamel M, Boes CJ (2017) Renaut Corpuscles or Peripheral Nerve Infarcts? A Historical Overview. Can J Neurol Sci 44(2): 184–189. https://doi.org/10.1017/cjn.2016.406.
Petrova ES (2012) The use of stem cells to stimulate the regeneration of the damaged nerve. Tsitologiya 54 (7): 525–540.
Petrova ES (2015) Injured nerve regeneration using cell-based therapies: current challenges. Acta Naturae 7(3): 38–47. https://doi.org/10.32607/20758251-2015-7-3-38-47
Petrova ES (2018) Differentiation potential of mesenchymal stem cells and stimulation of nerve regeneration. Russian Journal of Developmental Biology 49 (4): 193–205. https://doi.org/10.1134/S1062360418040033
Huang CW, Huang WC, Qiu X, Fernandes Ferreira da Silva F, Wang A, Patel S, Nesti LJ, Poo MM, Li S (2017) The differentiation stage of transplanted stem cells modulates nerve regeneration. Sci Rep 7(1):17401. https://doi.org/10.1038/s41598-017-17043-4
Du J, Zhen G, Chen H, Zhang S, Qing L, Yang X, Lee G, Mao HQ, Jia X (2018) Optimal electrical stimulation boosts stem cell therapy in nerve regeneration. Biomaterials 181: 347–359. https://doi.org/10.1016/j.biomaterials.2018.07.015
Xia B, Chen G, Zou Y, Yang L, Pan J, Lv Y (2019) Low-intensity pulsed ultrasound combination with induced pluripotent stem cells-derived neural crest stem cells and growth differentiation factor 5 promotes sciatic nerve regeneration and functional recovery. J Tissue Eng Regen Med 13(4): 625–636. https://doi.org/10.1002/term.2823
Petrova E, Isaeva E, Kolos E, Korzhevskii D (2018) Allogeneic bone marrow mesenchymal stem cells in the epineurium and perineurium of the recipient rat. Biological Communications 63 (2): 123–132. https://doi.org/10.21638/spbu03.2018.205
Petrova ES, Kolos EA, Korzhevskii DE (2021) Changes in the thickness of rat nerve sheaths after single subperineural administration of rat bone marrow mesenchymal stem cells. Bull Exp Biol Med 171: 547–552. https://doi.org/10.1007/s10517-021-05267-4
Kucenas S, Wang WD, Knapik EW, Appel B (2009) A selective glial barrier at motor axon exit points prevents oligodendrocyte migration from the spinal cord. J Neurosci 29: 15187–15194. https://doi.org/10.1523/JNEUROSCI.4193-09.2009
Lunn ER, Scourfield J, Keynes RJ, Stern CD (1987) The neural tube origin of ventral root sheath cells in the chick embryo. Development 101: 247–254.
Boyd BS, Gray AT, Dilley A, Wanek L, Topp KS (2012) The pattern of tibial nerve excursion with active ankle dorsiflexion is different in older people with diabetes mellitus. Clin Biomech (Bristol, Avon) 27 (9): 967–971. https://doi.org/10.1016/j.clinbiomech.2012.06.013
Ross MH, Reith EJ (1989) Perineurium: Evidence for contractile elements. Science 165: 604–606. https://doi.org/10.1126/science.165.3893.604
De Jonge RR, Vreijling JP, Meintjes A, Kwa MS, van Kampen AH, van Schaik IN, Baas F (2003) Transcriptional profile of the human peripheral nervous system by serial analysis of gene expression. Genomics 82(2): 97–108. https://doi.org/10.1016/s0888-7543(03)00124-1
De Jonge RR, van Schaik IN, Vreijling JP, Troost D, Baas F (2004) Expression of complement components in the peripheral nervous system. Hum Mol Genet 13(3): 295–302. https://doi.org/10.1093/hmg/ddh029
Pogorelov YV (2001) Histohematological barriers. Guide to Histology, vol. I. SpecLit, SPb, pp 465–494 (In Russ).
Burkel WE (1967) The histological fine structure of perineurium. Anat Rec 158(2):177–189. https://doi.org/10.1002/ar.1091580207
Hall SM, Williams PL (1971) The distribution of electron-dense tracers in peripheral nerve fibres. J Cell Sci 8(2):541–555.
Klemm H (1970) The perineurium: a diffusion barrier for peroxidase in epineurial and endoneurial application. Z Zellforsch Mikrosk Anat 108(3): 431–445.
Olsson Y, Reese TS (1971) Permeability of vasa nervorum and perineurium in mouse sciatic nerve studied by fluorescence and electron microscopy. J Neuropathol Exp Neurol 30(1):105–119. https://doi.org/10.1097/00005072-197101000-00011
Palladino SP, Helton ES, Jain P, Dong C, Crowley MR, Crossman DK, Ubogu EE (2017) The Human Blood-Nerve Barrier Transcriptome. Sci Rep 7(1): 17477. https://doi.org/10.1038/s41598-017-17475-y
Ouyang X, Dong C, Ubogu EE (2019) In situ molecular characterization of endoneurial microvessels that form the blood-nerve barrier in normal human adult peripheral nerves. J Peripher Nerv Syst 24(2):195–206. https://doi.org/10.1111/jns.12326
Dong C, Ubogu EE (2018) GDNF enhances human blood-nerve barrier function in vitro via MAPK signaling pathways. Tissue Barriers 6(4):1–22. https://doi.org/10.1080/21688370.2018.1546537
Moreau N, Mauborgne A, Couraud PO, Romero IA, Weksler BB, Villanueva L. Pohl M, Boucher Y (2017) Could an endoneurial endothelial crosstalk between Wnt/β-catenin and Sonic Hedgehog pathways underlie the early disruption of the infra-orbital blood-nerve barrier following chronic constriction injury? Mol Pain 13:1744806917727625. https://doi.org/10.1177/1744806917727625
Moreau N, Mauborgne A, Bourgoin S, Couraud PO, Romero IA, Weksler BB, Villanueva L, Pohl M, Boucher Y (2016) Early alterations of Hedgehog signaling pathway in vascular endothelial cells after peripheral nerve injury elicit blood-nerve barrier disruption, nerve inflammation, and neuropathic pain development. Pain 157(4): 827–839. https://doi.org/10.1097/j.pain.0000000000000444
Bykov VL (2007) Cytology and General Histology. Sotis, Sankt-Peterburg (In Russ).
Oldfors A, Johansson BR (1979) Barriers and transport properties of the perineurium. An ultrastructural study with 125I-labeled albuminin and horseradish peroxidase in normal and protein-deprived rats. Acta Neuropathol 47(2):139–143. https://doi.org/10.1007/BF00717037
Oldfors A (1981)Permeability of the perineurium of small nerve fascicles: an ultrastructural study using ferritin in rats. Neuropathol Appl Neurobiol 7(3):183–194. https://doi.org/10.1111/j.1365-2990.1981.tb00088.x
Parmantier E, Lynn B, Lawson D, Turmaine M, Namini SS, Chakrabarti L, McMahon AP, Jessen KR, Mirsky R (1999) Schwann cell-derived Desert hedgehog controls the development of peripheral nerve sheaths. Neuron 23(4): 713–724. https://doi.org/10.1016/s0896-6273(01)80030-1.
Jung J, Frump D, Su J, Wang W, Mozaffar T, Gupta R (2015) Desert hedgehog is a mediator of demyelination in compression neuropathies. Exp Neurol 271: 84–94. https://doi.org/10.1016/j.expneurol.2015.04.014
Fontenas L, Kucenas S (2017) Livin’ on the edge: glia shape nervous system transition zones. Curr Opin Neurobiol 47:44–51. https://doi.org/10.1016/j.conb.2017.09.008
Chen ZL, Yu WM, Strickland S (2007) Peripheral regeneration. Annu ReNeurosci 30: 209–233. https://doi.org/10.1146/annurev.neuro.30.051606.094337
Monk KR, Feltri ML, Taveggia C (2015) New insights on Schwann cell development. Glia 63: 1376–1393. https://doi.org/10.1002/glia.22852
Ohara S, Takahashi H, Ikuta F (1986) Ultrastructural alterations of perineurial cells in the early stage of Wallerian degeneration. Lab Invest 54(2): 213–221.
Spencer PS, Weinberg HJ, Raine CS, Prineas JW (1975) The perineurial window—a new model of focal demyelination and remyelination. Brain Res 96: 323–329. https://doi.org/10.1016/0006-8993(75)90742-8
Radek A, Thomas PK, King RH (1986) Perineurial differentiation in interchange grafts of rat peripheral nerve and spinal root. J Anat 147: 207–217.
Lewis GM, Kucenas S (2014) Perineurial glia are essential for motor axon regrowth following nerve injury. J Neurosci 34(38):12762–12777. https://doi.org/10.1523/JNEUROSCI.1906-14.2014
Ohta M, Okajima S, Hirakawa H, Tokunaga D, Fujiwara H, Oda R, Kobashi H, Hirata M, Kubo T (2005) Expression of tight and gap junctional proteins in the perineurial window model of the rat sciatic nerve. Int J Neurosci 115(10):1469–1481. https://doi.org/10.1080/00207450591001871
Toyoda T, Ochiai K, Ohashi K, Tomioka Y, Kimura T, Umemura T (2005) Multiple perineuriomas in chicken (Gallus gallus domesticus). Vet Pathol 42(2):176–183. https://doi.org/10.1354/vp.42-2-176
Pummi KP, Aho HJ, Laato MK, Peltonen JT, Peltonen SA (2006) Tight junction proteins and perineurial cells in neurofibromas. J Histochem Cytochem 54(1): 53–61. https://doi.org/10.1369/jhc.5A6671.2005
Shelekhova KV, Danilova AB, Michal M, Kazakov DV (2008) Hybrid neurofibroma-perineurioma: an additional example of an extradigital tumor. Ann Diagn Pathol 12(3): 233–234. https://doi.org/10.1016/j.anndiagpath.2008.02.012
Gibson JD (1979) The origin of the neural macrophage: a quantitative ultrastructural study of cell population changes during Wallerian degeneration. J Anat 129(1):1–19.
Hirata K, Kawabuchi M (2002) Myelin phagocytosis by macrophages and nonmacrophages during Walleriandegeneration. Microsc Res Tech 57: 541–547. https://doi.org/10.1002/jemt.10108
De la Motte DJ, Hall SM, Allt G (1975) A study of the perineurium in peripheral nerve pathology. Acta Neuropathol 33(3): 257–270. https://doi.org/10.1007/BF00688398
Funding
This work was supported by the State budget funding within a governmental assignment to the Institute of Experimental Medicine.
Author information
Authors and Affiliations
Contributions
E.S.P.—basic idea, writing a part of the review, E.A.K.—writing a part of the review.
Corresponding author
Ethics declarations
CONFLICT OF INTEREST
The authors inform that they have no conflict of interest associated with the publication of this article.
Additional information
Translated by A. Polyanovsky
Russian Text © The Author(s), 2022, published in Zhurnal Evolyutsionnoi Biokhimii i Fiziologii, 2022, Vol. 58, No. 1, pp. 3–23https://doi.org/10.31857/S0044452922010053.
Rights and permissions
About this article
Cite this article
Petrova, E.S., Kolos, E.A. Current Views on Perineurial Cells: Unique Origin, Structure, Functions. J Evol Biochem Phys 58, 1–23 (2022). https://doi.org/10.1134/S002209302201001X
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S002209302201001X