Abstract
Association between lymphocyte activation and formation of immune tolerance, as well as pregnancy outcome, in the case of immunocytotherapy (ICT) was studied in women with idiopathic recurrent pregnancy loss (IRPL). The content and phenotypic characteristics of activated T lymphocytes and NK cells were investigated in the peripheral blood of IRPL patients with different pregnancy outcomes (pregnancy prolongation to the full term and habitual miscarriage). The fraction of activated cells in the subpopulation of cytotoxic T lymphocytes (CD3+CD8+/CD3+CD8+CD69+) before ICT was significantly lower in women who lost the pregnancy. After ICT, the fraction of these cells during weeks 5-6 of pregnancy in woman with miscarriage was higher than in women with pregnancy prolonged to the full-term. Excessive content of activated cytotoxic lymphocytes can be a mechanism underlying impaired maternal immunotolerance to fetal alloantigens, which is a leading factor of early pregnancy loss. The obtained data confirm the involvement of activated Th17 cells and FOXP3+ Treg cells in the formation of tolerance to paternal antigens of the fetus. Comparison of the decrease in the fraction of CD4+CD25highRORt+ lymphocytes at the early gestation period (5-6 weeks) and significant upregulation of the IL-17 production by in vitro stimulated whole blood cells in women with miscarriage with the same parameters in women with prolonged pregnancy suggested an imbalance between pro-inflammatory Th17 cells and Treg cells. No such imbalance in the content effector T lymphocytes was observed in women with the full-term pregnancy. Taken together, our data indicate an important role of gestational activation of lymphocytes in the formation of maternal immune response to fetal alloantigens necessary for the prolongation of pregnancy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Tolerance to paternal antigens is an obligatory condition for the normal course of pregnancy and a key factor of normal fetal development. It is established that signals from the fertilized oocyte (surface antigens and secreted polypeptides, such as growth factors, cytokines, human chorionic gonadotropin, preimplantation factor) appear already several hours after fertilization and trigger a cascade of hormonal responses that prepare mother’s body for pregnancy [1]. Recognition of “foreign” paternal antigens of the fetus results in the allogenic stimulation of maternal immune system and development of cellular and humoral responses that contribute to the formation of immune tolerance preventing fetus rejection and providing normal course of pregnancy. However, early spontaneous recurrent pregnancy loss is observed in 1-5% women [2]. Pregnancy loss before weeks 7-8 with of gestation in the absence of known miscarriage-causing factors (e.g., infections) is believed to be associated with immune disorders, first of all, impaired recognition of paternal antigens resulting in insufficient control over the development of inflammatory response. Impaired maternal immune tolerance to fetal alloantigens can be a leading factor in the pregnancy interruption, including idiopathic recurrent pregnancy loss (IRPL), i.e., a complex of symptoms associated with multiple recurrent miscarriages.
The problem of controlling and directing inflammatory responses in the early pregnancy has been discussed in the reproduction immunology for several decades, especially the use of various approaches to immune response correction, including alloimmunization with paternal lymphocytes, immunocytotherapy (ICT), that was proposed as a method for controlling immune tolerance formation and prolongation of pregnancy to the full term in women with IRPL. Despite that ICT has been used for a rather long time to prevent early pregnancy loss, there is no unambiguous opinion on its efficiency [3]. For this reason, the mechanisms underlying impaired maternal immune tolerance to the fetal alloantigens, as well as the effects of ICT, are still actively investigated.
Manifestations of alloimmune disorders during pregnancy are studied at the cellular and molecular levels, both in patients and experimental models; however, immune mechanisms responsible for the tolerance formation and changes in the molecular and cellular factors that lead to the impaired gestation remain unknown. For a long time, the Th1/Th2 response paradigm had been popular, which emphasized an importance of a ratio between pro- and anti-inflammatory factors. According to this paradigm, cells producing Th2-type cytokines are essential for the tolerance induction and maintenance during pregnancy, especially, at the early stages. This paradigm has been replaced by another one, which includes regulatory T cells (Th1/Th2/Th17/Treg cells). At present, it is believed that an important role in the tolerance formation and maintenance belongs to cytotoxic and regulatory T cells, as well as natural killer (NK) cells. To elucidate how ICT influences the immune system of women with IPRL, it is necessary to take into consideration not only the ratio between lymphocyte subpopulations, but also the ability of these cells to respond to activating stimuli, e.g., mitogens that can act as polyclonal activators and induce a cascade of changes in T and B lymphocytes. These changes are similar to the changes occurring in response to specific antigens, although they do not lead to further differentiation of lymphocytes. The earliest marker of activation is the membrane glycoprotein CD69 which is transiently expressed in activated lymphocytes. CD69 expression is induced by the activating signal through the T-cell receptor (TCR). Incomplete activation can lead to the anergy of effector T cells and dysfunction of Treg cells (via dysregulated production of the transforming growth factor TGF-). In the case of the full-fledged activation, induced CD69 expression correlates with the proliferation of T lymphocytes, their differentiation, increase production of TGF-, decrease in the severity of inflammation, and formation of tolerogenic dendritic cells [4]. Treg cells also respond to the mitogen-induced activation with an increase in the CD69 expression and changes in the functional state [5].
CD69 interacts through its cytoplasmic fragment with proteins of the Jak3/Stat5 signaling pathway that regulate the function of RORt, which is a transcription factor of Th17 cells that directs differentiation of T helpers towards the Th17 cells [6]. This might explain CD69 participation in the polarization of effector immune response toward Th1/Th17/Treg cells, which is especially important in the early pregnancy. It was found that STAT5 plays a key role in the induction of FOXP3 expression. FOXP3 is a transcription factor of T cells with natural suppressor activity, which is confirmed, on one hand, by the presence of STAT5-binding sites in the promoter region of the FOXP3 gene and, on the other hand, by the absence of FOXP3+ Treg cells in STAT5-deficient mice [7]. Therefore, CD69 can directly participate in the regulation of the Th17/Treg cell balance [8, 9] and can be considered as a natural modulator of T cell differentiation programs. Unlike T lymphocytes, activation of NK cells is not associated with proliferation, but with the effector function based on the balance between inhibitory and activating receptors.
It is important to identify specific features of immune system in IRPL patients, as well as the ratio between cytotoxic and Treg cells and the levels of their activation after ICT in the cases of miscarriage and successful prolongation of pregnancy resulting in the birth of a viable baby, since this information can be helpful in predict the outcome of pregnancy in women with IRPL.
In this work, we studied the role of lymphocyte activation after ICT in the formation of immune tolerance in women with IRPL.
MATERIALS AND METHODS
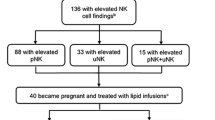
Thirty-six patients with IRPL were studied, who became pregnant after pregestational alloimmunization. In 30 patients, the pregnancy was full-term, followed by the birth of a viable baby; 6 patients experienced miscarriage before 12 weeks of gestation. The control group included 15 fertile non-pregnant women and 11 women with 12-week physiological pregnancy.
Indications for being included into the group under study were as follows: at least two cases of pregnancy loss in the first trimester (with the same partner); the absence of infectious, anatomic, genetic, hormonal, and autoimmune factors of pregnancy loss; the absence of severe extragenital pathologies.
Indications for being included into the control group were as follows: at least one labor in the history; no complication in the obstetric and gynecological history; physiological course of pregnancy.
In both groups, women were 20 to 40 years old and the pregnancy was started naturally.
Blood samples for analysis were taken on an empty stomach from the ulnar vein. Blood from non-pregnant women was withdrawn on days 18-22 of menstrual cycle; blood samples from pregnant women were taken at weeks 5-6, 8-9, and 12 of pregnancy.
ICT procedure was performed using lymphocytes collected from male partners before the conception and during the first trimester of the pregnancy. All procedures for the lymphocyte isolation and ICT were approved by the Scientific Council of the National Medical Research Center for Obstetrics, Gynecology, and Perinatology, Ministry of Healthcare of Russian Federation (protocol no. 19; December 25, 2012). Lymphocytes used for the procedure corresponded to the criteria for donorship.
Male blood samples were taken from the ulnar vein into a 50-ml sterile tube containing 200 μl of heparin (5000 IU/ml) as an anticoagulant. Lymphocyte suspension was isolated in a special room equipped with sterile laminar flow box (AMS-MZMO, Russia) and centrifuge (ELMI, Latvia). After careful mixing, the blood samples were incubated at 37°C for 1–1.5 h. After separation into two layers (upper layer, plasma with mononuclear cells; lower layer, erythrocytes), the upper layer was transferred to a sterile 14-ml centrifuge tube and centrifuged for 7 min at 1500 rpm. The supernatant was removed and the pellet was resuspended in 6 ml of sterile saline. The resulting suspension was divided in two portions; each portion was layered onto 3 ml of Ficoll in a tube at a 1 : 2 ratio and centrifuged for 30 min at 1500 rpm. Lymphocyte rings were collected into a 14-ml sterile tube and washed twice with saline by centrifuging for 7 min at 1500 rpm. The supernatant was removed and the precipitate was carefully mixed with 2 ml of sterile saline. The lymphocyte concentration in the saline was (30-50) · 106 per ml. The lymphocytes were injected intracutaneously on day 5-10 of menstrual cycle into the palm surface of the woman’s forearm two times with an interval of 1 month. After the onset of pregnancy, immunization was performed during weeks 5-6 and 8-9.
The content of lymphocytes expressing CD69 was evaluated after stimulation with 10 μg/ml phytohemagglutinin (PHA) for 2 h in a CO2-incubator (SANYO, Japan) at 37C. The surface phenotype (CD3/CD4/CD69, CD3/CD8/CD69, CD45/CD56/CD69) of the stimulated lymphocytes was assessed with monoclonal antibodies (mAb) from the FastImmune kit (Becton Dickinson, USA). Antibodies to CD3 and CD45 were labeled with peridinin-chlorophyll-protein complex (PerCP); antibodies to CD4, CD8, CD56 – with fluorescein isothiocyanate (FITC); and antibodies to CD69 – with phycoerythrin (PE). MAbs were added directly to the whole blood; the cells were lysed with OptiLyse solution (Beckman Coulter, USA).
To determine the fraction of RORt+ Th17 cells among CD4+CD25high lymphocytes, the cells were isolated by centrifugation in a density gradient using Ficoll-verographin mixture with a density of 1.077 [28]. Before permeabilization, the cells were stained with FITC-labeled anti-CD4 antibodies and PE-labeled anti-CD25 antibodies; after permeabilization, the cells were stained with anti-RORt antibodies labeled with allophycocyanine (APC) (eBioscience, USA). The number of cells in the lymphocytic gate was (1-1.5) · 106.
Flow cytometry analysis was performed with a Gallios flow cytometer (Beckman Coulter) using Kaluza Software Version 1.2 (Beckman Coulter).
The content of IL-17 was assessed by the multiplex analysis using a Cytometric Bead Array (CBA) analytic system and with a standard Human IL-17A Flex set (Becton Dickinson, USA) in the supernatants of cells cultures after addition of mitogens [4 μg of PHA, 4 μg of concanavalin A (Con A), 2 μg of lipopolysaccharide; Cytokin-stimul-best kit, Vector-Best, Russia] to 1 ml of whole blood. The cells were incubated in a CO2 incubator at 37C for 24 h. The supernatant was obtained by centrifugation for 10 min at 3000g and then for 3 min at 10,000g (Hettich, Germany); the specimens were aliquoted and stored at –80C. Analysis was performed with a FACSCalibur flow cytofluorometer (Becton Dickinson). The results were calculated using the FlowCytomix-Pro-3.0 program (Becton Dickinson).
The data were processed statistically using Microsoft Office Excel 2007 and MedCalc12 program for Windows 7. The hypothesis on the normal distribution was tested using Kolmogorov–Smirnov and Shapiro–Wilk criteria [29]. The data are presented as mean ± standard error (M ± m). The significance of differences between the groups was assessed with the Student’s t‑test; the differences were considered significant at p ˂ 0.05.
RESULTS
The content of CD69-expressing lymphocytes in the peripheral blood of women with IRPL.Table 1 shows the results of retrospective analysis of the content of lymphocytes expressing CD69 spontaneously and after in vitro stimulation in the blood of IRPL patients with different outcomes of pregnancy that started after pregestational ICT and in non-pregnant fertile women of the control group.
As seen from Table 1, no differences in the studied parameters were observed between the control group and IPRL patients with pregnancy prolonged to the full-term on the ICT background either before and after the treatment. In women who had miscarried in the first trimester, the content of lymphocytes responding to the stimulation in vitro before ICT was significantly lower than in the control (subpopulations CD45+CD69+, CD3+CD8+CD69+, and CD45+CD56+CD69+) and women with prolonged pregnancy (subpopulations CD45+CD69+, CD3+CD8+CD69+, CD45+CD56+CD69+, and CD45+CD3+CD69+). In this group, ICT caused a trend (0.05 ≤ p ≤ 0.09) to the increase in the content of these subpopulations as compared to the initial values, whereas the content of cytotoxic lymphocytes expressing CD69 after in vitro stimulation (CD3+CD8+CD69+) was significantly higher than in women with prolonged pregnancy. It is likely that the initial decrease in the amount of lymphocytes followed by the stimulation of response to the in vitro activation in women with miscarriage could be associated with altered functional activity of these cells, especially, with their cytotoxicity.
To elucidate whether the favorable outcome of pregnancy is associated with changes in the content of CD69-expressing lymphocytes, the amount of lymphocytes responding to the activating stimuli in vitro was determined during the first trimester (Table 2). No changes in the studied parameters were found during this period in women with prolonged pregnancy.
Comparison of the content of CD69-expressing lymphocytes after pregestational ICT during weeks 5-6 of pregnancy in women with prolonged pregnancy on the ICT background and women with miscarriages revealed significant differences between the two groups (Table 3). In the ICT-subjected women who miscarried, the content of CD69-expressing lymphocytes was significantly higher than in women with prolonged pregnancy. Women who experienced miscarriage demonstrated an increased content of lymphocytes expressing CD69 either spontaneously (CD45+CD69+ and CD45+CD3+CD69+) or in response to mitogens- (CD45+CD3+CD69+, CD3+CD4+CD69+, and CD3+CD8+CD69+), i.e., such increase was observed for T lymphocytes, but not NK cells (CD45+CD56+CD69+).
We also evaluated the fraction of activated lymphocytes (CD69+) in the CD45+CD56+, CD3+CD8+, and CD3+CD4+ subpopulations (Table 4) and found that that in patients who lost pregnancy, the fraction of cytotoxic T-lymphocytes expressing CD69 on their surface (CD3+CD8+CD69+, p = 0.006) before pregestational ICT was lower than in women with prolonged pregnancy. After ICT, there was a tendency for the elevation in the fraction of activated T cells (CD3+CD4+CD69+, p = 0.09; CD3+CD8+CD69+, p = 0.1), that became becoming at weeks 5-6 of pregnancy, especially for the fraction of cytotoxic T lymphocytes (CD3+CD8+CD69+ cell fraction of CD3+CD8+ lymphocytes, p = 0.016). No differences in the relative content of activated NK cells were found.
Comparative analysis of the content of activated lymphocytes in the studied subpopulations at week 12 of pregnancy in patients with prolonged pregnancy and women with physiological course of pregnancy revealed no significant differences in the amount of CD69-expressing lymphocytes after in vitro stimulation. However, the content of lymphocytes spontaneously expressing CD69 in vitro (CD45+CD69+ and CD45+CD3+CD69+) was lower (p = 0.04 and 0.02, respectively) than in women with physiological pregnancy (Table 5). The assessment of the fraction of activated lymphocytes (CD69+) in the CD45+CD56+, CD3+CD8+, and CD3+CD4+ subpopulations of stimulated cells revealed no significant differences between the groups.
Therefore, the response of T lymphocytes to the stimulation during the first trimester in the ICT-subjected IRPL patients with prolonged pregnancy did not differ from the lymphocyte response in the control group.
The content of Th17 lymphocytes andin vitroIL-17 production in women with IRPL. No differences were found in the fraction of Th17 cells (RORt+) among CD4+CD25high lymphocytes in the peripheral blood, as well as in the IL-17 production by stimulated whole blood cells in vitro, before and after pregestational ICT in women who experienced miscarriage and patients with prolonged pregnancy (Fig. 1).
A significant increase in the IL-17 production by the stimulated whole blood cells along with a significant decrease in the fraction of CD4+CD25highRORt+ lymphocytes were observed at weeks of 5-6 of pregnancy in women who miscarried as compared to the corresponding values in women with prolonged pregnancy. No significant differences in the fraction of CD4+CD25highRORt+ lymphocytes and IL-17 production by the stimulated whole blood cells was found between women with prolonged pregnancy and women with physiological course of pregnancy at 12 weeks of gestation (Fig. 2).
The fraction of the RORt+ subpopulation among CD4+CD25high lymphocytes (a) and in vitro IL-17 production by stimulated whole blood cells (b) in IRPL patients with prolonged pregnancy at week 12 of pregnancy. Open bars, women with physiological course of pregnancy; light-gray bars, women with prolonged pregnancy.
Therefore, the fraction of Th17 cells among CD4+CD25high lymphocytes and IL-17 production by in vitro mitogen-stimulated whole blood cells in patients with prolonged pregnancy were not different from the corresponding values in the control group.
The observed decrease in the fraction of CD4+CD25highRORt+ lymphocytes at weeks 5-6 of pregnancy and significantly increased IL-17 production by the stimulated whole blood cells in women with miscarriage as compared to women prolonged pregnancy suggests a disturbance in the balance between Th17 and Treg cells, which is essential for normal formation of immune tolerance and regulation of immune response in the earliest period of pregnancy.
DISCUSSION
Immune tolerance to paternal antigens is an obligatory condition for the normal course of pregnancy and a key factor in the normal development of the fetus. The control of developing inflammatory responses during early gestation is necessary for creating a balance between the functional and anatomic integrity of mother’s body during uterus decidualization, embryo implantation, trophoblast invasion, placenta formation, and subsequent growth of the fetus (if it does not have genetic abnormalities). The limiting events take place before weeks 5-6 weeks of pregnancy, when the fetal egg can be clearly visualized by ultrasonic examination and heart rhythm is established. Therefore, pregnancy loss before weeks 7-8 in the absence of known factors of miscarriage is believed to be associated with immune disorders and insufficient control of inflammatory processes related to the recognition of paternal antigens, which might lead to either rejection of the fetus or arrest of its growth (missed pregnancy). IRPL is the only obstetric complication which is commonly believed to be caused mainly by immunity-related factors.
Controlling the intensity and direction of inflammatory responses during early gestation by ICT is still a debated problem. So far, there is no common opinion on the effectiveness of this procedure, because of differences in the case histories of women included in the studies, different immunization protocols, and different set of parameters used for the assessment of female immune system during immunization [10, 11]. Up to now, successful prolongation of pregnancy by ICT is believed to be associated with the transition of pregnant woman’s immune system from the pro-inflammatory status to the anti-inflammatory one. However, there is a growing body of evidence that the pro-inflammatory status of maternal immune system is required for successful embryo implantation and placenta formation, which implies a revision of the ICT role in the prolongation of pregnancy in women with IRPL [12].
Here, we analyzed the content in the peripheral blood of lymphocyte subpopulations expressing CD69 in response to in vitro stimulation with mitogens. CD69 is the earliest antigen whose appearance on the cell surface is a marker of cell response to activating stimuli. CD69 is induced in the majority of hemopoietic cell lines, including T and B lymphocytes and NK cells that can be detected already an hour after the activating stimulus action [13].
The assessment of cell subpopulations expressing CD69 in response to the activating stimuli during pregnancy can be important for understanding the mechanisms of immune tolerance formation and regulation of responses of maternal immune system to the fetal antigens of paternal origin.
At present, the mechanism of CD69 participation in the polarization of effector immune response toward Th1/Th17/Treg cells is under discussion [4, 14, 15]. On one hand, galectin-1 (Gal-1), which is expressed by the endometrial stromal cells during the entire menstrual cycle and whose expression is significantly activated during embryo implantation, was identified as one of specific CD69 ligands. Gal-1 induces differentiation of dendritic cells toward the phenotype that suppresses Th1/Th17 differentiation via IL-10 and IL-27. Gal-1 interaction with CD69 stimulates the JAK3/STAT5 signaling pathway involved in the formation of cells with the phenotype specific for cells with natural regulatory (suppressor) activity (Treg or FOXP3-expressing Treg cells).
On the other hand, CD69 expression in the activated lymphocytes promotes internalization and degradation of the S1PR1 receptor and suppression of the STAT3-induced expression of IL-17, because interaction of sphingosine-1-phosphate-1 (S1P1) with the G-protein-associated S1PR1 stimulates the mTORc/HIF-1α (mammalian target of rapamycin/hypoxia-inducible factor 1-alpha) and JAK2/pSTAT3 signaling pathways, triggering the formation of the Th1 or Th17 effector responses. In this case, signaling pathways directed to the formation of Treg cells are supported [14, 15].
CD69 also contributes to the balance of Th1/Th17/Treg cells by promoting the transport of tryptophan by the LAT1-CD98 complex and activation of aromatic hydrocarbon receptor (AHR) as a result of binding with the high-affinity natural ligand FICZ (6-formylindolo[3,2-b] carbazol). FICZ induces the Th17 direction of immune response via signal transduction to the corresponding promoter region [DRE (dioxin responsible element) or AHRE (aryl hydrocarbon responsible element)] [30]. The transport of amino acids by CD69/LAT1-CD98 also activates serine/threonine protein kinase mTOR (a subunit of the intracellular multimolecular signaling complexes TORC1 and TORC2), directing the development of the Th1 and Th17 effector response and preventing differentiation of Treg cells. Moreover, mTOR controls the activity of HIF-1α, which negatively regulates the function of Treg cells by promoting FOXP3 degradation. AHR activation attenuates HIF-1α-mediated effects, thus influencing the differentiation of effector T cells [14, 15].
In the early pregnancy, when metabolism is affected and altered by hormones and proteins specific for this period, signal transmission through CD69 can be associated mostly with the increased tryptophan transfer by the LAT1-CD98 complex and AHR activation. Moreover, insufficient formation of Treg cells can be caused by disturbances of regulatory mechanisms during early pregnancy characterized by hypoxia development due to endometrium decidualization and rearrangement of uterine spiral arteries.
It is possible that both these mechanisms are activated during ICT, because in addition to the metabolic activation, introduction of multiple antigens also activates specific immune response to weak antigens (adjuvant effect). Lymphocyte response to the activation is different in different environment (skin, uterus). It is likely that in the uterus during pregnancy, at least one of the mechanisms does not favor Treg formation under transient hypoxic conditions.
All the above said is summarized in Fig. 3 (modified from Cibrian and Sancher-Madrid [14]).
Activation of immune system in women with IRPL by immunization with lymphocytes from the male partner was confirmed by appearance of anti-paternal anti-leukocyte antibodies and by the dynamics in the content of these antibodies from one procedure to another in pregnant and in non-pregnant women [16, 17]. However, no signs of T cell activation, including changes in the content of CD4+CD25highCD127low/– Treg cells, were observed in the lymphocyte subpopulations in the peripheral blood of women with the full-term pregnancy subjected to ICT before the conception [18]. No changes were also found in the content of CD4+CD25highRORt+ Th17 lymphocytes (Fig. 1a) and IL-17 production (Fig. 1b) in the subpopulations of CD69-expressing lymphocytes (Table 1). The changes in the content of Treg cells were observed during the first trimester in women with the full-term pregnancy [19], which indicated an important role of gestational metabolic activation and regulatory proteins and peptides specific for the early pregnancy in the formation of the maternal immune system response to fetal alloantigens. The subpopulations of lymphocytes in the peripheral blood of IRPL patients with the full-term pregnancy were the same as in women with the physiological course of pregnancy beginning week 12 of gestation [20]. No differences were found in the content of CD69-expressing lymphocytes (Table 5), the fraction of CD4+CD25highRORt+ lymphocytes, and IL-17 production of (Fig. 2). Therefore, ICT was beneficial for the pregnancy prolongation in these women, and the success of ICT was associated with the formation of a balance between the content of effector T lymphocytes and cytokine production essential for pregnancy maintenance (Fig. 3).
Before the ICT, the amount of lymphocytes responding to the in vitro stimulation in women with IRPL who lost pregnancy in the first trimester was significantly lower than in women with prolonged pregnancy (Table 1). After pregestational ICT, the level of CD3+CD8+CD69+ lymphocytes in these women increased. At weeks 5-6 of pregnancy, the amount of T lymphocytes expressing CD69 spontaneously (CD45+CD69+ and CD45+CD3+CD69+) and in response to the stimulation with mitogens (CD45+CD3+CD69+, CD3+CD4+CD69+, and CD3+CD8+CD69+) significantly increased. The fraction of cytotoxic CD3+CD8+CD69+ T lymphocytes among CD3+CD8+ lymphocytes also increased (Tables 3 and 4). There were no differences in the content of CD69-expressing NK cells and the fraction of activated NK cells.
It has become generally accepted that in normal pregnancy, NK cells mainly ensure trophoblast invasion and remodeling of spiral arteries under the influence of microenvironment that develops in response to the recognition of fetal antigens, which in its turn, is a prerequisite for the generation of specific peripheral tolerance in physiological pregnancy [21]. The balance between the cytotoxic activity of T lymphocytes and NK cells is very important for the normal pregnancy course [22]. It is possible that the level of CD69 expression on the T lymphocyte surface in the peripheral blood before the in vitro stimulation during ICT can be a marker of specific response of T lymphocytes to the paternal antigens of the fetus. In such case, we may assume that in women with IRPL, an increased response of cytotoxic lymphocytes to the polyclonal stimulation also reflects an increase in the specific response to fetal antigens.
Hence, the results of our study do not confirm the hypothesis on the impaired recognition of paternal antigens of the fetus as a leading factor of pregnancy loss. Instead, we suggest a possibility of controlling the inflammatory reactions in response to the appearance of antigens of the semi-allogenous fetus in woman’s reproductive tract. It is likely that ICT acts as one of such controlling therapeutic measures. It cannot be excluded that in the majority of patients, ICT can suppress the excessive response of lymphocytes to both polyclonal stimulation and stimulation of T lymphocytes by fetal antigens, as indicated by the observed steady levels of CD69 expression on the surface of CD3+ lymphocytes at all times of prolonged pregnancy, but not in patients with miscarriage, in which mitogen-stimulated in vitro expression of CD69 by cytotoxic T lymphocytes was higher than in women with prolonged pregnancy, in the absence of differences in the response of NK cells to the polyclonal stimulus.
We have shown earlier that in women who lost pregnancy, the content of NK cells before the immunization in the pregestational period had been lower than in patients with prolonged pregnancy. The correlation between the low level of CD56+ lymphocytes and probability of pregnancy loss in the first trimester was retained also at weeks 5-6 of pregnancy [23]. This confirms the suggestion that that low levels of both Treg and NK cells are reliable markers of spontaneous abortion [24]. The low level of CD4+CD25highCD127low/– Treg cells in the peripheral blood both before the pregestational ICT and at weeks 5-6 of pregnancy was characteristic of IRPL women patients [23, 25]. As mentioned above, an increase in the content of these lymphocytes was observed only in patients with prolonged pregnancy. Moreover, we found that in patients subjected to ICT, not only the level of NK cells decreased to the minimum at weeks 5-6 weeks of pregnancy as compared to the initial level in women who lost this pregnancy [23], but that the fraction of CD4+CD25highRORt+ lymphocytes also decreased to the minimum at the same time, which was accompanied by a high production of IL-27 by the stimulated cells of the peripheral blood (Fig. 1). On one hand, low blood level of CD4+CD25highRORt+ cells can reflect activated migration of Th17 cells from the peripheral blood; on the other hand, high production of IL-17 indicates the presence in peripheral blood of cells which are able to intensively secrete IL-17 upon stimulation and to provide the Th17-type of proinflammatory response.
All the above said allows us to suggest formation of impaired immune response in IRPL patients who lost pregnancy and inability of ICT to control inflammatory reactions in these patients during early pregnancy. Note that the high levels of IL-17 production by stimulated peripheral blood cells in women with physiological course of pregnancy and in IRPL patients with prolonged pregnancy at week 12 indicate that procedures performed for prolonging the pregnancy should weaken but not abolish the Th17 response in women with IRPL.
Our data confirm the involvement of activated Th17 cells along with FOXP3+ Treg cells in the formation of tolerance to paternal antigens of the fetus. In the future, it will be necessary to assess the role of the transcription factor RORt and Th17 cells in the formation or suppression of tolerance to the paternal antigens during pregnancy [26]. Although we have not demonstrated the possibility of concurrent expression of RORγt and FOXP3 in CD4+CD25high cells, there are experimental data on the association of RORγt expression in FOXP3+ Treg cells with the high-level synthesis of the interferon-regulating factor 4 which provides Treg cells with the ability to suppress the Th2 response, which is very important in early pregnancy [27].
Thus, our assessment of the ability of peripheral blood lymphocytes of patients with IRPL to respond to the in vitro stimulation by expressing CD69 is in agreement with the current concepts on the immune relations between mother and fetus in early pregnancy. These results also confirm the formation of immune tolerance to fetal alloantigens of paternal origin in patients with IRPL whose pregnancy was prolonged to the full term and ended with birth of a viable child, in response to ICT in the pregestational period and during the first trimester. We showed that ICT was unable to control the tolerance formation in the IRPL women who lost the observed pregnancy. These results expand our knowledge on the role of lymphocyte activation in the formation of immune tolerance to fetal alloantigens in early pregnancy in women with IRPL.
Abbreviations
- AHR:
-
aromatic hydrocarbon receptor
- ICT:
-
immunocytotherapy
- IRPL:
-
idiopathic recurrent pregnancy loss
- FOXP3:
-
forkhead box p3 protein (transcription factor regulating cell differentiation and expression of cytokine participating in immune response suppression)
- NK cell:
-
natural killer cell
- RORt:
-
retinoid-related orphan receptor (transcription factor regulating differentiation of T lymphocytes to Th17 cells)
- Th1:
-
type 1 T helper
- Th17:
-
type 17 T helper
- Treg cell:
-
regulatory T cel
REFERENCES
Sukhikh, G. T., and Vanko, L. V. (2003) Immunology of Pregnancy [in Russian], Russian Academy of Medical Sciences Publishers, Moscow.
Sidelnikova, V. M., and Sukhikh, G. T. (2011) Pregnancy Loss: A Guide for Practitioners [in Russian], Medical Inform. Agency, Moscow.
Carp, H. J. A. (2014) Recurrent Pregnancy Loss: Causes, Controversies, and Treatment, CRC Press London.
Sancho, D., Gomez, M., and Sanchez-Madrid, F. (2005) CD69 is an immunoregulatory molecule induced following activation, Trends Immunol., 26, 136-140, doi: 10.1016/j.it.2004.12.006.
Hu, Y. P., Li, X. J., and Liu, S. W. (2010) Effects of ConA on early activation and function of CD4+ CD25+ Treg cells in mice, Chinese J. Cell. Mol. Immunology, 26, 118-120, [in Chinese].
Martin, P., Gomez, M., Lawana, A., Cruz-Adalia, A., Ramirez-Huesca, M., Ursa, M. A., Yañez-Mo, M., and Sanchez-Madrid, F. (2010) CD69 association with Jak3/Stat5 proteins regulates Th17 cell differentiation, Mol. Cell. Biol., 30, 4877-4889, doi: 10.1128/MCB.00456-10.
Lu, L. F., and Rudensky, A. (2009) Molecular orchestration of differentiation and function of Regulatory T cells, Genes Dev., 23, 1270-1282, doi: 10.1101/gad.1791009.
Martin, P., and Sanchez-Madrid, F. (2011) CD69: an unexpected regulator of Th17 cell-driven inflammatory responses, Sci. Signal., 4, 14, doi: 10.1126/scisignal.2001825.
Miki-Hosokawa, T., Hasegawa, A., Iwamura, C., Shinoda, K., Tofukuji, S., Watanabe, Y., Hosokawa, H., Motohashi, S., Hashimoto, K., Shirai, M., Yamashita, M., and Nakayama, T. (2009) CD69 controls the pathogenesis of allergic airway inflammation, J. Immunol., 183, 8203-8215, doi: 10.4049/jimmunol.0900646.
Farquharson, R. G., and Stephenson, M. D. (2017) Early Pregnancy, Cambridge University Press, Cambridge.
Porter, T. F., LaCoursiere, Y., and Scott, J. R. (2006) Immunotherapy for recurrent miscarriage, Cochrane Database Syst. Rev., 2, CD000112, doi: 10.1002/14651858.CD000112.pub2.
Mor, G. (2008) Inflammation and pregnancy: the role of toll-like receptors in trophoblast-immune interaction, Ann. N. Y. Acad. Sci., 1127, 121-128, doi: 10.1196/annals.1434.006.
Marzio, R., Mauel, J., and Betz-Corradin, S. (1999) CD69 and regulation of the immune function, Immunopharmacology Immunotoxicology, 21, 565-582, doi: 10.3109/08923979909007126.
Cibrian, D., and Sancher-Madrid, F. (2017) CD69: from activation marker to metabolic gatekeeper, Eur. J. Immunol., 47, 946-953, doi: 10.1002/eji.201646837.
Labiano, S., Melendez-Rodriguez, F., Palazon, A., Teijeira, A., Garasa, S., Etxeberria, I., Aznar, M. A., Sanchez-Paulete, A. R, Azpilikueta, A., Bolanos, E., Molina, C., de la Fuente, H., Maiso, P, Sanchez-Madrid, F., de Landazuri, M. O., Aragones, J., and Melero, I. (2017) CD69 is a direct HIF-1α target gene in hypoxia as a mechanism enhancing expression on tumor-infiltrating T lymphocytes, Oncoimmunology, 6, doi: 10.1080/2162402X.2017.1283468.
Krechetova, L. V., Khachatryan, N. A., Tetruashvili, N. K., Vtorushina, V. V., Stepanova, E. O., Golubeva, E. L., Nikolaeva, M. A., and Sukhikh, G. T. (2015) Dynamics of production of antileukocytic antibodies to paternal antigens at immunization with the allogenous cells of women with habitual miscarriage, Akusherstvo Ginekologiya, 3, 16-20, [in Russian].
Krechetova, L. V., Tetruashvili, N. K., Vtorushina, V. V., Nikolaeva, M. A., Golubeva, E. L., Saribekova, V. A., Agadzhanova, A. A., and Vanko, L. V. (2017) Dynamics of production of antileukocytic antibodies during the pregnancy in women with habitual miscarriage on the background of immunocytotherapy, Akusherstvo Ginekologiya, 9, 48-55, doi: 10.18565/aig.2017.9.48-55, [in Russian].
Krechetova, L. V., Stepanova, E. O., Nikolaeva, M. A., Vtorushina, V. V., Golubeva, E. L., Khachatryan, N. A., Tetruashvili, N. K., and Sukhikh, G. T. (2015) Dynamics in the composition of lymphocyte subpopulations in the peripheral blood of women with habitual miscarriage at pregestational immunocytotherapy, Akusherstvo Ginekologiya, 4, 37-43, [in Russian].
Krechetova, L. V., Tetruashvili, N. K., Vtorushina, V. V., Stepanova, E. O., Nikolaeva, M. A., Golubeva, E. L., and Khachatryan, N. A. (2015) Dynamics in the composition of lymphocyte subpopulations in the peripheral blood of women with habitual miscarriage in the first trimester of the pregnancy on the background of immunocytotherapy, Akusherstvo Ginekologiya, 6, 59-66, [in Russian].
Tetruashvili, N. K., Krechetova, L. V., Saribekova, V. A., Vtorushina, V. V., Golubeva, E. L., Khachatryan, N. A., and Agadzhanova, A. A. (2017) Dynamics in the composition of lymphocyte subpopulations in the peripheral blood in patients with habitual miscarriage of alloimmune origin during pregnancy, Akusherstvo Ginekologiya: Novels Opinions Education, 4, 28-36, [in Russian].
Siewiera, J., Siewiera, J., Gouilly, J., Hocine, H.R., Cartron, G., Levy, C., Al-Daccak, R., and Jabrane-Ferrat, N. (2015) Natural cytotoxicity receptor splice variants orchestrate the distinct functions of human natural killer cell subtypes, Nat. Commun., 6, 12. doi: 10.1038/ncomms10183.
Nakashima, A., Nakashima, A., Shima, T., Inada, K., Ito, M., and Saito, S. (2012) The balance of the immune system between T cells and NK cells in miscarriage, Am. J. Reprod. Immunol., 67, 304-310, doi: 10.1111/j.1600-0897.2012.01115.
Krechetova, L. V., Tetruashvili, N. K., Vtorushina, V. V., Nikolaeva, M. A., Khachatryan, N. A., Agadzhanova, A. A., Vanko, L. V., Ivanets, T. Y., and Sukhikh, G. T. (2017) Specific features of the phenotype of peripheral blood lymphocytes of women with the idiopathic habitual miscarriage in dependence of the pregnancy outcome on the immunocytotherapy background, Akusherstvo Ginekologiya, 7, 52-60, doi: 10.18565/aig.2017.7.52-60, [in Russian].
Vacca, P., Moretta, L., Moretta, A., and Mingari, M. C. (2011) Origin, phenotype and function of human natural killer cells in pregnancy, Trends Immunol., 32, 517-523, doi: 10.1016/j.it.2011.06.013.
Krechetova, L. V., Khachatryan, N. A., Tetruashvili, N. K., Vtorushina, V. V., Stepanova, E. O., Nikolaeva, M. A., and Sukhikh, G. T. (2014) Specific features of the phenotype of peripheral blood lymphocytes of women with habitual miscarriage, Akusherstvo Ginekologiya, 10, 27-33, [in Russian].
Nakachima, A., Ito, M., Yoneda, S., Shiozaki, A., Hidaka, T., and Saito, S. (2010) Circulating and decidual Th17 cell levels in healthy pregnancy, Am. J. Reprod. Immunol., 63, 104-109, doi: 10.1111/j.1600-0897.2009.00771.x.
Ohnmacht, C., Park, J. H., Cording, S., Wing, J. B., Atarashi, K., Obata, Y., Gaboriau-Routhiau, V., Marques, R., Dulauroy, S., Fedoseeva, M., Busslinger, M., Cerf-Bensussan, N., Boneca, I. G., Voehringer, D., Hase, K., Honda, K., Sakaguchi, S., and Eberl, G. (2015) The microbiota regulates type 2 immunity through RORγt+ T cells, Science, 349, 989-993, doi: 10.1126/science.aac4263.
Menshikov, V. V., Delektorskaya, L. N., and Zolotnitskaya, R. P. (1987) Laboratory Methods in Klinics [in Russian], Meditsina, Moscow.
Shapiro, S. S., and Wilk, M. B. (1965) An analysis of variance test for normality (complete samples), Biometrika, 52, 591-611.
Quintana, F. J., Basso, A. S., Iglesias, A. H., Korn, T., Farez, M. F., Bettelli, E., Caccamo, M., Oukka, M., and Weiner, H. L. (2008) Control of T reg and TH 17 cell differentiation by the aryl hydrocarbon receptor, Nature, 453, 65-71, doi: 10.1038/nature06880.
Funding
The work was performed within a framework of the State Task AAAA-A18-118053190024-2.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the Ethics Committee of the National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Healthcare of Russian Federation. All participants signed an informed consent about inclusion in the study. The authors declare no conflict of interests.
Rights and permissions
About this article
Cite this article
Krechetova, L., Vanko, L., Vtorushina, V. et al. Lymphocyte Activation in the Development of Immune Tolerance in Women with Recurrent Pregnancy Loss. Biochemistry Moscow 85, 583–593 (2020). https://doi.org/10.1134/S0006297920050077
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S0006297920050077