Abstract
There was a lack of evidence on the association between dairy intake and metabolic health status in overweight/obese adolescents. This study evaluated the association between dairy intake and metabolic health status in overweight/obese Iranian adolescents. Overweight/obese adolescents (n = 203; 101 boys and 102 girls) selected by a multistage cluster random sampling method have participated in this cross-sectional study. Dietary intake was assessed using a validated 147-item food frequency questionnaire. Anthropometric indices, blood pressure, fasting glucose, insulin, and lipid profile were measured. Participants were categorized to metabolically healthy obese (MHO) and metabolically unhealthy obese (MUO) according to International Diabetes Federation (IDF) criteria and a combination of IDF with Homeostasis Model Assessment Insulin Resistance (HOMA-IR) criteria. The frequency of MUO based on IDF, and IDF/HOMA-IR definitions was 38.9% and 33.0%, respectively. In fully-adjusted model, participants in the highest tertile of dairy intake had 61% lower odds of MUO based on IDF criteria (OR = 0.39, 95% CI 0.15–0.99). Higher dairy intake was associated with a non-significant lower risk of MUO according to IDF/HOMA-IR definition in the maximally-adjusted model (OR = 0.44, 95% CI 0.17–1.16). Stratifies analysis by sex and body mass index revealed that the association was stronger in girls and overweight subjects. Furthermore, higher intake of low-fat dairy was related to a reduced likelihood of MUO, while higher intake of high-fat dairy was related to increased odds of MUO. This community-based cross-sectional study revealed that higher intake of dairy was associated with a significant lower odd of MUO among Iranian adolescents, especially in girls and overweight subjects.
Similar content being viewed by others
Introduction
Childhood and adolescent overweight/obesity have been considered as one of the most serious public health challenges of the twenty-first century by the world health organization (WHO)1. The global prevalence of overweight/obesity in children and adolescents has increased tremendously since 19802. Pooled results from population-based studies comprising 31.5 million individuals aged 5–19 years from 200 countries indicated that global age-standardized prevalence of obesity have increased in both sexes worldwide3. Overweight/obesity in adolescents imposes a substantial burden on affected individuals, their families, and health care systems, especially in low- and middle-income countries with limited resources. Excess body weight in adolescents often is associated with serious complications such as hypertension, dyslipidemia, insulin resistance, and fatty liver diseases which all convey an increased risk of future cardiovascular disease (CVD), type 2 diabetes mellitus, and subsequent premature death4,5. Thus, an effective management for overweight and obesity and their related complications in this age population is essential.
Despite the above-mentioned relations, cardiometabolic risk factors do not develop in some clinically obese individuals known as metabolically healthy obese (MHO) individuals6. There has been no consensus regarding the definition of MHO and different definitions and consequently, varying prevalence rates of this condition have been proposed in the literature6,7. However, it is evident that MHO individuals display a desirable metabolic profile presented by better insulin sensitivity, lipid profile, and blood pressure8,9 and lower mortality rate10,11. A combination of genetic and lifestyle-related factors such as dietary intake and physical activity plays a role in the etiology of this condition and prevention of developing metabolically unhealthy obese (MUO) condition12,13. For example, previous investigations have reported that healthy dietary patterns with higher intake of fruits and vegetables14,15 and lower intake of fats12 and soft drinks13 were related to MHO.
A limited number of previous studies have investigated the relationship between dairy intake and metabolic health status in adolescents; no consistency was seen between available results. A cohort study of 531 participants aged 6–18 years without the metabolic syndrome (MetS) at baseline showed a reduced risk for MetS incident among those with higher intake of dairy foods, mainly for low-fat milk and yogurt16. Abreu et al. have also showed that higher milk intake was associated with lower cardiometabolic risk score in adolescents. However, they found no association between total dairy, yogurt, or cheese intake and this score17. Conversely, the results of a cross-sectional study of 785 adolescents aged 10–19 years by Mohammadi et al. did not support the association between dairy intake and MetS or its components18. To the best of our knowledge, no previous study has addressed the association between dairy intake and MHO/MUO status in adolescents. The aim of the present study was to investigate the association between dairy intake and metabolic health status in Iranian overweight and obese adolescents.
Methods
Study design and participants
The current cross-sectional study was performed among a representative sample of Iranian adolescents. For sample size calculation, the prevalence of MUO was considered as 60%, based on previous studies among overweight and obese Iranian adolescents19,20. Considering a power 80%, type I error of 0.05, desired confidence interval (CI) of 0.95, and precision (d) of 7%, the required sample size was estimated to be 188. A stratified, multistage cluster sampling design was used to randomly select participants involving students aged 12–18 years old from 16 middle and high schools in six various education districts in Isfahan, Iran. The age-sex-specific percentile curves of body mass index (BMI)21 were used to screen overweight/obese adolescents and invite them to participate in the study. The exclusion criteria were having genetic or endocrine disorders such as type 1 diabetes mellitus, hypothyroidism, and Cushing’s syndrome, being on a weight-loss diet, taking nutritional supplements (including vitamin and mineral supplements) or medications that might influence metabolic markers such as body weight, lipid profile, blood glucose, or blood pressure. Finally, a total of 203 overweight/obese adolescents comprising 102 girls and 101 boys were included in the present study. The study protocol was approved by the ethics committee of the Isfahan University of Medical Sciences and a written informed consent was obtained from each participant and their parents.
Assessment of dairy intakes
Dietary intakes of participants were assessed by a validated 147-item food frequency questionnaire (FFQ) completed by a trained nutritionist22. Previous investigations have documented that this questionnaire has a desirable validity and reliability for the assessment of food intake among Iranian adolescents23,24. The participants were asked to report the frequency of intake for each food item on a daily, weekly, and monthly basis. The amount of consumed food items was also reported based on standard portion sizes, and then the household measures were used to convert the portion sizes of consumed foods into grams per day25. Finally, Nutritionist IV software was applied to compute the daily intake of energy and nutrients. Dairy items in the applied FFQ were low-fat milk, whole milk, cocoa milk, regular yogurt, whole yogurt, strained yogurt, cheese, cream cheese, cream, ice cream, dough, and kashk. Sum of intakes of all dairy products was considered as total dairy intake. Low-fat dairy (< 2% fat) was considered as low-fat milk, regular yogurt, dough, and kashk. While high-fat dairy (> 2% fat) was considered as whole milk, cocoa milk, whole yogurt, strained yogurt, cheese, cream cheese, cream, and ice cream.
Assessment of anthropometric indices and cardio-metabolic risk factors
Anthropometric indices were estimated by a trained nutritionist. Weight was measured by a digital scale (Seca Instruments, Germany) to the nearest 100 g while the participants were wearing thin clothes and no shoes. A stadiometer was used to measure height to the nearest 0.1 cm while the participants were standing with shoulders relaxed, and wearing no shoes. BMI was calculated by dividing weight (kg) by squared height (m2) and categorized according to the WHO growth curve of age-sex-specific BMI percentiles to normal weight (5th < BMI < 85th percentile), overweight (85th < BMI < 95th percentile), and obese (BMI > 95th percentile)21. Waist circumference (WC) was twice measured in midway between the lowest rib and the superior border of the iliac crest, after a normal expiration and without any pressure on the body surface, to the nearest 0.1 cm by an un-stretchable flexible anthropometric tape. The average of two measurements was considered as WC value. Blood pressure was measured twice after 15 min of rest on the right arm by a mercury sphygmomanometer in the morning and fasting condition.
Blood samples were collected after 12 h of fasting to assess biochemical indices. Fasting blood glucose (FBG) concentration was measured with an enzymatic colorimetric method using glucose oxidase (Pars Azmoon commercial kits, Tehran, Iran) on the day of blood collection. Serum insulin levels were measured using an ELISA kit (Diagnostic Biochem Canada Inc.). To estimate insulin resistance, the homeostasis model assessment insulin resistance (HOMA-IR) was calculated by the following formula: HOMA-IR = [(fasting insulin (mU/L) × FBG (mmol/L)]/22.5. Additionally, commercial kits (Pars Azmoon commercial kits, Tehran, Iran) were used to measure serum high-density lipoprotein cholesterol (HDL-c) and triglyceride (TG) levels.
Assessment of metabolic health status
Two strategies were applied to demonstrate the metabolic health status (MHO vs. MUO): (1) based on the International Diabetes Federation (IDF) criteria, individuals with at least two of following risk factors were considered as MUO: increased TG (≥ 150 mg/dL), decreased HDL-c (< 40 mg/dL for the age of < 16 years, and < 50 mg/dL in girls/< 40 mg/dL in boys for the age of ≥ 16 years), increased fasting blood glucose (≥ 100 mg/dL) and increased blood pressure (≥ 130/85 mmHg)26, (2) based on a combination of the first strategy and the presence of insulin resistance (IR) based on HOMA-IR, MUO was considered as individuals with HOMA-IR > 3.16 and at least two mentioned metabolic risk factor; MHO was considered as subjects with HOMA-IR < 3.16, without considering the number of their cardiometabolic risk factors27.
Assessment of other variables
Physical activity of participants was evaluated using the validated physical activity questionnaire for adolescents (PAQ-A) which consists of 9 items scoring from 1 to 528. Eight items of this questionnaire are about usual activities such as their activity during spare time, physical education classes, lunch, after school, evenings, and weekends, as well as the frequency of physical activity during the last 7 days. The last item asks adolescents if they were prevented from engaging in regular physical activity by sickness or other reasons. Students were classified as sedentary (or not having an orderly week activity) (score < 2), low active (2 ≤ score < 3), moderately active (3 ≤ score < 4), and highly active (score ≥ 4), based on their total score of physical activity. A standard checklist was applied to collect the information regarding the students’ age, sex, and medical history of diseases, taking medications or supplements. A validated questionnaire was also used to gather information about socioeconomic variables (including parental job, parental education level, family size, having cars in the family, having computers/laptops, having a personal room, and taking trips in the last year)29.
Statistical analysis
The normality of quantitative variables was examined using the Kolmogorov–Smirnov test. First, energy-adjusted dairy intake was calculated based on residual method30, in order to have an exposure of interest independent from energy intake. Continuous and categorical variables were respectively presented as mean ± SD/SE and frequency (percentage). Then, participants were categorized based on energy-adjusted tertiles of dairy intake. The chi-square test and one-way ANOVA were respectively used to determine categorical and continuous variables across tertiles of dairy intake. Additionally, energy, age, and sex-adjusted dietary intakes of subjects across tertiles of dairy intake were evaluated using analysis of covariance (ANCOVA). Odds ratios (ORs) and their attributed 95% confidence intervals (95% CIs) for MUO across tertiles of dairy intake were estimated by binary logistic regression in crude and multivariable-adjusted models. Based on previous literature16,18,31, in the first model, adjustments were made for age, sex, energy intake and fat intake (percent of energy). In the second model, physical activity and socioeconomic variables were additionally adjusted. Finally, BMI was added to the adjustments in the third model, to obtain an independent association from obesity. The first tertile of dairy intake was considered as the reference category in all models. To determine trends, tertiles of dairy intake were treated as an ordinal variable in logistic regression models. Furthermore, stratified analyses were performed based on BMI categories, sex, and low vs. high fat dairy intake. Data analyses were performed using SPSS version 20 software and the value of P < 0.05 was considered as statistically significant.
Ethical approval and consent to participate
The study procedure was performed according to declaration of Helsinki and STROBE checklist. All participants provided informed written consent. The study protocol was approved by the local Ethics Committee of Isfahan University of Medical Sciences.
Results
A total of 203 adolescents (101 boys and 102 girls) with a mean age of 13.98 ± 1.61 (SD) years and an average BMI of 27.35 ± 3.24 kg/m2 participated in the present study. Among participants, 38.9% (37 boys, and 42 girls) were classified as MUO based on IDF criteria, while 33% (35 boys, and 32 girls) were categorized as MUO based on IDF/HOMA-IR definition.
General characteristics and cardiometabolic factors of study participants across energy-adjusted tertiles of dairy intake are summarized in Table 1. Participants with the highest dairy intake (tertile 3) were more likely to be boys (P = 0.01), and physically active (P < 0.001) compared to those in the lowest tertile. Additionally, the mean FBG (P = 0.01) and HOMA-IR index (P = 0.03) were significantly lower among adolescents in the highest tertile in comparison to those in the lowest one. However, no significant difference was observed regarding other general or cardiometabolic features across tertiles of dairy intake. General characteristics and cardiometabolic factors of adolescents across energy-adjusted tertiles of dairy intake, stratified by sex are shown in the Supplemental Table 1. Both girls and boys in the highest tertile of dairy intake were more likely to be physically active. In addition, the mean FBG was significantly lower in subjects in the highest category of dairy intake in both genders (P < 0.05).
Dietary intakes of study participants across energy-adjusted tertiles of dairy intake, stratified by sex are presented in the Supplemental Table 2. In both groups, no significant difference was observed in energy intake across tertiles of dairy intake (P > 0.05). However, girls in the third tertile of dairy intake had a significantly higher intake of protein, cholesterol, saturated fatty acid (SFA), vitamin C, vitamin A, riboflavin, vitamin B6, folate, vitamin B12, magnesium, calcium, and total fiber (P < 0.05), while no significant difference was observed between dietary intake of poly-unsaturated fatty acid (PUFA), thiamin, niacin, and vitamin E across tertiles of dairy intake among girls (P > 0.05). Furthermore, boys in the third tertile of dairy intake had a significantly higher intake of protein, fat, cholesterol, SFA, monounsaturated fatty acid (MUFA), vitamin C, vitamin A, riboflavin, vitamin B6, folate, vitamin E, magnesium, calcium, total fiber and lower intake of carbohydrates, thiamin, and niacin (P < 0.05). No significant difference was observed between dietary intake of PUFA and vitamin B12 across tertiles of dairy intake among boys (P > 0.05).
The distribution of adolescents with MUO phenotype across energy-adjusted tertiles of dairy intake is presented in Fig. 1. Based on IDF definition, 52.2%, 44.1%, and 20.6% of individuals were identified as MUO in tertiles 1, 2 and 3 of dairy intake (P < 0.001). In addition, based on IDF/HOMA-IR definition, the frequency of adolescents with MUO phenotype across tertiles of dairy intake was respectively 46.3%, 33.8%, and 19.1% (P < 0.001).
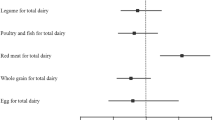
Multivariate adjusted odds ratio (OR) and 95% confidence interval (CI) for MUO across energy-adjusted tertiles of dairy intake are indicated in Table 2. Based on IDF criteria, individuals in the highest tertile of dairy intake had 76% lower odds of MUO, compared to those in the bottom tertile, in the crude model (OR: 0.24, 95% CI 0.11–0.51). This association remained significant after adjustment for potential confounders. Such that, in fully-adjusted model, adolescents in the highest tertile had 61% lower odds of MUO in comparison to the reference tertile (OR: 0.39, 95% CI 0.15–0.99). A significant inverse association was also observed between energy-adjusted dairy intake and odds of MUO based on IDF/HOMA-IR criteria in the crude model (OR: 0.27, 95% CI 0.13–0.59). Nevertheless, when physical activity and socioeconomic status were taken into account as the confounders, this association disappeared. So, dairy intake was associated with a non-significant decreased odd of MUO, in the fully-adjusted model (OR: 0.44, 95% CI 0.17–1.16).
Multivariate adjusted odds ratio (OR) and 95% confidence interval (CI) for MUO across energy-adjusted tertiles of dairy intake, stratified by BMI categories are shown in Table 3. According to IDF definition, the highest category of dairy intake was significantly associated with 88% decreased odds of MUO both in the crude (OR: 0.12, 95% CI 0.03–0.41) and fully adjusted model (OR: 0.12, 95% CI 0.02–0.66), among overweight adolescents. On the other hand, among obese adolescents, no significant association was observed between dairy intake and MUO in the crude (OR: 0.44, 95% CI 0.16–1.23) or fully adjusted model (OR: 0.66, 95% CI 0.19–2.21), based on IDF definition. The same pattern was observed for the association between dairy intake and MUO among overweight and obese adolescents, based on IDF/HOMA-IR criteria. Such that, overweight individuals in the highest tertile of dairy intake had 89% and 88% reduced odds of MUO in the crude (OR: 0.11, 95% CI 0.03–0.44) and fully-adjusted model (OR: 0.12, 95% CI 0.02–0.73). However, there was no significant association between dairy intake and MUO either in the crude (OR: 0.56, 95% CI 0.20–1.53) and fully-adjusted model (OR: 0.86, 95% CI 0.25–2.90), among obese adolescents.
Multivariate adjusted odds ratio (OR) and 95% confidence interval (CI) for MUO across energy-adjusted tertiles of dairy intake, stratified by sex are presented in Table 4. In the crude model, girls in the top category of dairy intake had 90% and 91% reduced odds of MUO phenotype according to IDF (OR: 0.10, 95% CI 0.02–0.40) and IDF-HOMA-IR definition (OR: 0.09, 95% CI 0.02–0.46), compared to girls in the bottom category. These relationships remained significant after adjustment for potential confounders. Such that, in fully adjusted model, girls in the third tertile of dairy intake were 89% (OR: 0.11, 95% CI 0.02–0.58) and 92% (OR: 0.08, 95% CI 0.01–0.61) less likely to have MUO phenotype based on IDF and IDF/HOMA-IR definitions, respectively. Among boys, a significant inverse association was observed between dairy intake and MUO based on IDF definition in the crude model (OR: 0.38, 95% CI 0.15–0.99). The association disappeared after adjustment for potential confounders (OR: 0.80, 95% CI 0.22–2.89). No significant association was observed between dairy intake and MUO based on IDF/HOMA-IR definition either in the crude (OR: 0.43, 95% CI 0.17–1.11) and fully-adjusted model (OR: 1.01, 95% CI 0.28–3.72) among boys.
As reported in Table 5, we have also evaluated the association between MUO phenotype with high- and low-fat dairy intake. In the crude model, individuals in the top tertile of low-fat dairy intake had 81% (OR: 0.19, 95% CI 0.09–0.40) and 84% (OR: 0.16, 95% CI 0.07–0.36) lower odds of MUO based on IDF and IDF/HOMA-IR definitions, respectively. These associations remained significant after adjustment for confounding variables. Such that, in fully-adjusted model, adolescents in the third tertile of low-fat dairy intake compared to the first tertile had 64% (OR: 0.36, 95% CI 0.14–0.89) and 75% (OR: 0.25, 95% CI 0.09–0.63) reduced likelihood of MUO, based on IDF and IDF/HOMA-IR definitions, respectively. No significant association was found between high-fat dairy intake and MUO phenotype based on IDF criteria in the crude (OR: 1.91, 95% CI 0.96–3.83) and fully adjusted (OR: 1.62, 95% CI 0.67–3.93) models. While, a significant positive association was observed between high-fat dairy intake and MUO based on IDF/HOMA-IR in the crude model (OR: 2.61, 95% CI 1.26–5.41). This association was strengthened after adjustment for confounding variables (OR: 3.00, 95% CI 1.16–7.76).
Discussion
The present study indicated that more than 30% of Iranian adolescents have MUO phenotype, based on IDF or IDF/HOMA-IR definitions. Additionally, higher dairy intake in adolescents was significantly associated with reduced odds of MUO, based on both definitions. This association was stronger among girls and overweight individuals. However, the relationship between dairy intake and MUO among boys and obese subjects was dependent to covariates. Our findings also indicated that there was a significant inverse association between low-fat dairy intake and MUO according to both IDF, and IDF/HOMA-IR definitions, even after considering potential confounders, while a significant positive association was found between higher intake of high-fat dairy and MUO based on IDF/HOMA-IR definition. To the best of our knowledge, this was the first study that investigated the association between dairy intake and metabolic health status in overweight and obese adolescents.
In the present study, the comparison of metabolic health status components between tertiles of dairy intake showed that blood pressure values (SBP and DBP) had no significant difference across tertiles, while others factors including TG, HDL-c, and insulin levels had marginally significant differences across tertiles. In case of FBS and HOMA-IR, significant differences were observed between tertiles of dairy intake. These findings suggested that the metabolically unhealthy overweight/obese in adolescents could be regarded as more than the accumulation of the predisposing effects of its individual components.
Although the MHO phenotype is not essentially related to a better clinical outcome, prevention from shifting to MUO or even maintaining MHO status from adolescence to adulthood is valuable32,33. Our findings have suggested that overweight or obese adolescents can be clinically advised to increase their dairy intake, especially low-fat dairy intake, as an efficient strategy for achieving these goals.
Few previous studies have evaluated the association between dairy intake and metabolic syndrome (MetS) among children and adolescents with inconclusive results. None of these studies have reported their results across sex and BMI categories. Tehran Lipid and Glucose Study, a prospective investigation with 6.6 years follow-up on 531 healthy adolescents aged 6–18 years showed that higher dairy consumption was associated with reduced risk of MetS and some components of MetS, such as abdominal obesity, hypertension, and high serum TG levels16. Similar to our results, higher consumption of low-fat milk, and yogurt as well as moderate consumption of regular cheese in the mentioned cohort study was associated with reduced risk of MetS. While no significant relationship was observed between high-fat dairy intake and risk of MetS incidence16. Abreu et al. in a cross-sectional study examined the relationship between dairy intake and cardiometabolic risk score in adolescents aged 15 to 18 years. The cardiometabolic risk score was computed by summing up the age- and sex-adjusted z scores of total cholesterol/HDL-c, TG, HOMA, body fat percentage, systolic blood pressure, and cardiorespiratory fitness17. The results of this study showed that only a higher intake of milk was associated with reduced odds of cardiometabolic risk score. While no association was observed between cardiometabolic risk score and higher intake of total dairy, yogurt, and cheese17. In contrast to the findings of the above-mentioned studies, the study by Mohammadi et al. on 785 Iranian adolescents aged 10–19 years showed that there was no significant relationship between total, low-fat and high-fat dairy as well as specific dairy products such as milk, yogurt, and cheese and odds of MetS18. The observed inconsistencies in the findings of these studies are probably due to differences in study design, studied population, and potential confounders considered in the analyses.
Several potential mechanisms have been suggested explaining the relation of dairy intake and metabolic health status. It has been hypothesized that calcium, which is abundant in dairy products, interferes with fat absorption in the intestine via binding to saturated fatty acids and forming insoluble soaps; thereby may improve serum TG levels and HDL-c to LDL-c ratio34,35. Dietary calcium intake from dairy also affects calciotropic hormones and reduces intracellular calcium which inhibits the synthesis of fatty acids, and induces lipolysis36,37. In addition, bioactive peptides of fermented dairy products such as yogurt and cheese have beneficial influences on blood pressure and fat accumulation through inhibiting angiotensin-I converting enzyme38,39. Some previous researches have also proposed gut microbiota dysbiosis in overweight/obese children and adolescents40,41. Fermented dairy products that contain probiotic bacteria can possibly improve the metabolic status of overweight/obese adolescents by various pathways including modulating insulin sensitivity, inflammatory reactions, and fat metabolism42,43.
The present study has several limitations that should be addressed. First of all, cross-sectional design of this study did not allow us to establish a causal relationship between dairy intake and metabolic health status. In addition, the possibility of reverse causality should be considered in the study, since overweight/obese adolescents with MUO might change their dietary intakes to attenuate their symptoms. Furthermore, our sample of overweight and obese adolescents was relatively small and thus it was impossible to stratify the analysis based on each dairy product. We also did not gather data of other risk factors that might affect metabolic health status such as pubertal status, paternal obesity, the time of adiposity rebound, and sleep behaviors. Finally, self-reported dietary intakes could be biased, in spite of using a validated FFQ. However, the current study was conducted on a somehow representative sample of Iranian overweight/obese adolescents, although our sample was not large. The preliminary results of the study can be used for designing future prospective or clinical trial investigations.
In conclusion, the findings of the present cross-sectional study indicated that a higher intake of dairy was associated with lower odds of MUO among Iranian adolescents, especially in girls and overweight subjects. Further large-scale prospective studies are needed to confirm these results.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- FFQ:
-
Food frequency questionnaire
- OR:
-
Odds ratios
- 95% CI:
-
95% Confidence interval
- BMI:
-
Body mass index
- MHO:
-
Metabolically healthy obese
- MUO:
-
Metabolically unhealthy obese
- IDF:
-
International Diabetes Federation
- HOMA-IR:
-
Homeostasis Model Assessment Insulin Resistance
- IR:
-
Insulin resistance
- PAQ-A:
-
Physical Activity Questionnaire for Adolescents
- SES:
-
Socioeconomic status
- SFA:
-
Saturated fatty acids
- WHO:
-
World Health Organization
- WC:
-
Waist circumference
- BP:
-
Blood pressure
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- TG:
-
Triglycerides
- HDL-c:
-
High density lipoprotein cholesterol
- FBG:
-
Fasting blood glucose
- ANCOVA:
-
Analysis of covariance
- SPSS:
-
Statistical package for the social sciences
- SD:
-
Standard deviation
- SE:
-
Standard error
References
Organization, W. H. Adolescent obesity and related behaviours: trends and inequalities in the WHO European Region, 2002–2014: Observations from the Health Behaviour in School-aged Children (HBSC) WHO collaborative cross-national study. (2017).
Ng, M. et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 384, 766–781 (2014).
Abarca-Gómez, L. et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128· 9 million children, adolescents, and adults. Lancet 390, 2627–2642 (2017).
Daniels, S. Complications of obesity in children and adolescents. Int. J. Obes. 33, S60–S65 (2009).
Han, J. C., Lawlor, D. A. & Kimm, S. Y. Childhood obesity. Lancet 375, 1737–1748 (2010).
Damanhoury, S. et al. Defining metabolically healthy obesity in children: A scoping review. Obes. Rev. 19, 1476–1491 (2018).
Hinnouho, G.-M. et al. Metabolically healthy obesity and risk of mortality: Does the definition of metabolic health matter?. Diabetes Care 36, 2294–2300 (2013).
Phillips, C. M. Metabolically healthy obesity: Definitions, determinants and clinical implications. Rev. Endocr. Metab. Disord. 14, 219–227 (2013).
Karelis, A. D. et al. The metabolically healthy but obese individual presents a favorable inflammation profile. J. Clin. Endocrinol. Metab. 90, 4145–4150 (2005).
Calori, G. et al. Prevalence, metabolic features, and prognosis of metabolically healthy obese Italian individuals: The Cremona Study. Diabetes Care 34, 210–215 (2011).
Hamer, M. & Stamatakis, E. Metabolically healthy obesity and risk of all-cause and cardiovascular disease mortality. J. Clin. Endocrinol. Metab. 97, 2482–2488 (2012).
Li, L. et al. Identification of genetic and environmental factors predicting metabolically healthy obesity in children: Data from the BCAMS study. J. Clin. Endocrinol. Metab. 101, 1816–1825 (2016).
Prince, R. L., Kuk, J. L., Ambler, K. A., Dhaliwal, J. & Ball, G. D. Predictors of metabolically healthy obesity in children. Diabetes Care 37, 1462–1468 (2014).
Chun, S. et al. Clinical characteristics and metabolic health status of obese Korean children and adolescents. Korean J. Family Med. 36, 233 (2015).
Roberge, J.-B. et al. Lifestyle habits, dietary factors, and the metabolically unhealthy obese phenotype in youth. J. Pediatr. 204, 46-52.e41 (2019).
Yuzbashian, E. et al. Associations of dairy intake with risk of incident metabolic syndrome in children and adolescents: Tehran Lipid and Glucose Study. Acta Diabetol. 58, 447–457 (2021).
Abreu, S. et al. Intake of milk, but not total dairy, yogurt, or cheese, is negatively associated with the clustering of cardiometabolic risk factors in adolescents. Nutr. Res. 34, 48–57 (2014).
Mohammadi, S. G., Mirmiran, P., Bahadoran, Z., Mehrabi, Y. & Azizi, F. The association of dairy intake with metabolic syndrome and its components in adolescents: Tehran Lipid and Glucose Study. Int. J. Endocrinol. Metab. 13 (2015).
Yaghoubpour, K. et al. Association of obesity phenotypes in adolescents and incidence of early adulthood type 2 diabetes mellitus: Tehran lipid and glucose study. Pediatr. Diabetes 22, 937–945 (2021).
Qorbani, M. et al. Association of dietary behaviors, biochemical, and lifestyle factors with metabolic phenotypes of obesity in children and adolescents. Diabetol. Metab. Syndr. 12, 1–7 (2020).
Onis, M. D. et al. Development of a WHO growth reference for school-aged children and adolescents. Bull. World Health Organ. 85, 660–667 (2007).
Kelishadi, R. et al. Development and evaluation of a questionnaire for assessment of determinants of weight disorders among children and adolescents: The Caspian-IV study. Int. J. Prev. Med. 3, 699 (2012).
Daneshzad, E. et al. Food insecurity is positively related to dietary inflammatory index in Iranian high school girls. Int. J. Vitamin Nutr. Res. (2019).
Mohseni, H. et al. The relationship between history of dietary nutrients intakes and incidence of aggressive behavior in adolescent girls: A case–control study. Clin. Nutr. ESPEN 43, 200–205 (2021).
Ghaffarpour, M., Houshiar-Rad, A. & Kianfar, H. The manual for household measures, cooking yields factors and edible portion of foods. Tehran Nashre Olume Keshavarzy. 7, 42–58 (1999).
Zimmet, P. et al. The metabolic syndrome in children and adolescents—An IDF consensus report. Pediatr. Diabetes 8, 299–306 (2007).
Matthews, D. R. et al. Homeostasis model assessment: Insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28, 412–419 (1985).
Kowalski, K. C., Crocker, P. R. & Donen, R. M. The physical activity questionnaire for older children (PAQ-C) and adolescents (PAQ-A) manual. Coll. Kinesio. Univ. Saskatchewan 87, 1–38 (2004).
Garmaroudi, G. R. & Moradi, A. Socio-economic status in Iran: A study of measurement index. Payesh (Health Monitor) 9, 137–144 (2010).
Willett, W. Issues in analysis and presentation of dietary data. Nutr. Epidemiol. 321–346 (1998).
Azadbakht, L., Mirmiran, P., Esmaillzadeh, A. & Azizi, F. Dairy consumption is inversely associated with the prevalence of the metabolic syndrome in Tehranian adults. Am. J. Clin. Nutr. 82, 523–530 (2005).
Blüher, S. & Schwarz, P. Metabolically healthy obesity from childhood to adulthood—Does weight status alone matter?. Metabolism 63, 1084–1092 (2014).
Phillips, C. M. Metabolically healthy obesity across the life course: Epidemiology, determinants, and implications. Ann. N. Y. Acad. Sci. 1391, 85–100 (2017).
Boon, N. et al. An intervention study of the effects of calcium intake on faecal fat excretion, energy metabolism and adipose tissue mRNA expression of lipid-metabolism related proteins. Int. J. Obes. 31, 1704–1712 (2007).
Lorenzen, J. K. et al. Effect of dairy calcium or supplementary calcium intake on postprandial fat metabolism, appetite, and subsequent energy intake. Am. J. Clin. Nutr. 85, 678–687 (2007).
Zemel, M. B. Role of dietary calcium and dairy products in modulating adiposity. Lipids 38, 139–146 (2003).
Zemel, M. B. Regulation of adiposity and obesity risk by dietary calcium: Mechanisms and implications. J. Am. Coll. Nutr. 21, 146S-151S (2002).
Choi, J., Sabikhi, L., Hassan, A. & Anand, S. Bioactive peptides in dairy products. Int. J. Dairy Technol. 65, 1–12 (2012).
Shah, N. P. Effects of milk-derived bioactives: An overview. Br. J. Nutr. 84, 3–10 (2000).
Del Chierico, F. et al. Gut microbiota markers in obese adolescent and adult patients: Age-dependent differential patterns. Front. Microbiol. 9, 1210 (2018).
Bervoets, L. et al. Differences in gut microbiota composition between obese and lean children: A cross-sectional study. Gut Pathogens 5, 1–10 (2013).
Mena-Sánchez, G., Becerra-Tomás, N., Babio, N. & Salas-Salvadó, J. Dairy product consumption in the prevention of metabolic syndrome: A systematic review and meta-analysis of prospective cohort studies. Adv. Nutr. 10, S144–S153 (2019).
Arora, T., Singh, S. & Sharma, R. K. Probiotics: Interaction with gut microbiome and antiobesity potential. Nutrition 29, 591–596 (2013).
Funding
The financial support for conception, design, data analysis and manuscript drafting comes from Nutrition and Food Security Research Center, Isfahan University of Medical Sciences, Isfahan, Iran.
Author information
Authors and Affiliations
Contributions
S.A.T., S.M., A.A., M.A., and P.S. contributed in conception, design, data collection, data interpretation, manuscript drafting, approval of the final version of the manuscript, and agreed for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tirani, S.A., Mirzaei, S., Asadi, A. et al. Dairy intake in relation to metabolic health status in overweight and obese adolescents. Sci Rep 12, 18365 (2022). https://doi.org/10.1038/s41598-022-22827-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-22827-4
- Springer Nature Limited