Abstract
PI3K-δ inhibitors have shown impressive activity in lymphoid malignancies but have been hampered by autoimmune and infectious toxicities, leading to market withdrawals. We previously demonstrated activity of the PI3K-δγ inhibitor duvelisib in T cell lymphomas (TCLs) that was associated with inflammatory adverse events. As reported here, we conducted a phase 1b/2a study of duvelisib in combination with either romidepsin (n = 66) or bortezomib (n = 32) in patients with relapsed/refractory TCL and found that the addition of romidepsin, but not bortezomib, appeared to increase efficacy while attenuating PI3K inhibitor-driven toxicity. The primary endpoint of the study was to determine the safety and maximum tolerated dose of duvelisib, which was 75 mg twice daily when combined with romidepsin versus 25 mg twice daily when combined with bortezomib. The most common adverse events were neutropenia (42%, 25/59) and fatigue (37%, 22/59) in patients treated with duvelisib and romidepsin and diarrhea (48%, 11/23) and neutropenia (30%, 7/23) in patients treated with duvelisib and bortezomib. Duvelisib and romidepsin resulted in less grade 3/4 hepatotoxicity (14%, 8/59) compared to 40% (14/35) in our previous study with duvelisib monotherapy. This was associated with reductions in circulating inflammatory mediators and myeloid cell inflammatory gene expression. Secondary endpoints of overall and complete response rates were 55% (35/64) and 34% (22/64) for patients treated with duvelisib and romidepsin and 34% (11/32) and 13% (4/32) for patients treated with duvelisib and bortezomib. Among patients with peripheral T cell lymphomas (PTCLs), overall and complete response rates of duvelisib and romidepsin were 56% (27/48) and 44% (21/48), respectively, with exploratory analyses showing increased response rates in patients with a follicular helper T cell subtype. These findings support further development of combined PI3K and histone deacetylase (HDAC) inhibition in TCLs and suggest a unique strategy to enable PI3K inhibitor-based combinations for additional patient populations. ClinicalTrials.gov identifier: NCT02783625.



Similar content being viewed by others
Data availability
For original clinical data, contact horwitzs@mskcc.org. De-identified participant data can be shared. External data requests will be answered within 1 month. The study protocols are included as a data supplement available with the online version of this article. Bulk RNA sequencing data are available in the Sequence Read Archive (PRJNA1098020). Single-cell transcriptomic data are available in the Gene Expression Omnibus (GSE266760). Source data are provided with this paper.
References
Leseux, L. et al. Syk-dependent mTOR activation in follicular lymphoma cells. Blood 108, 4156–4162 (2006).
Rudelius, M. et al. Constitutive activation of Akt contributes to the pathogenesis and survival of mantle cell lymphoma. Blood 108, 1668–1676 (2006).
Rassidakis, G. Z. et al. Inhibition of Akt increases p27Kip1 levels and induces cell cycle arrest in anaplastic large cell lymphoma. Blood 105, 827–829 (2005).
Uddin, S. et al. Role of phosphatidylinositol 3′-kinase/AKT pathway in diffuse large B-cell lymphoma survival. Blood 108, 4178–4186 (2006).
Slupianek, A. et al. Role of phosphatidylinositol 3-kinase-Akt pathway in nucleophosmin/anaplastic lymphoma kinase-mediated lymphomagenesis. Cancer Res. 61, 2194–2199 (2001).
Maeda, T., Yagasaki, F., Ishikawa, M., Takahashi, N. & Bessho, M. Transforming property of TEL-FGFR3 mediated through PI3-K in a T-cell lymphoma that subsequently progressed to AML. Blood 105, 2115–2123 (2005).
Vallois, D. et al. Activating mutations in genes related to TCR signaling in angioimmunoblastic and other follicular helper T-cell-derived lymphomas. Blood 128, 1490–1502 (2016).
Li, Z. et al. Recurrent mutations in epigenetic modifiers and the PI3K/AKT/mTOR pathway in subcutaneous panniculitis-like T-cell lymphoma. Br. J. Haematol. 181, 406–410 (2018).
Heavican, T. B. et al. Genetic drivers of oncogenic pathways in molecular subgroups of peripheral T-cell lymphoma. Blood 133, 1664–1676 (2019).
Watatani, Y. et al. Molecular heterogeneity in peripheral T-cell lymphoma, not otherwise specified revealed by comprehensive genetic profiling. Leukemia 33, 2867–2883 (2019).
Baohua, Y., Xiaoyan, Z., Tiecheng, Z., Tao, Q. & Daren, S. Mutations of the PIK3CA gene in diffuse large B cell lymphoma. Diagn. Mol. Pathol. 17, 159–165 (2008).
Pfeifer, M. et al. PTEN loss defines a PI3K/AKT pathway-dependent germinal center subtype of diffuse large B-cell lymphoma. Proc. Natl Acad. Sci. USA 110, 12420–12425 (2013).
Scarisbrick, J. J., Woolford, A. J., Russell-Jones, R. & Whittaker, S. J. Loss of heterozygosity on 10q and microsatellite instability in advanced stages of primary cutaneous T-cell lymphoma and possible association with homozygous deletion of PTEN. Blood 95, 2937–2942 (2000).
Nakahata, S. et al. Loss of NDRG2 expression activates PI3K-AKT signalling via PTEN phosphorylation in ATLL and other cancers. Nat. Commun. 5, 3393 (2014).
Sasaki, T. et al. Function of PI3Kγ in thymocyte development, T cell activation, and neutrophil migration. Science 287, 1040–1046 (2000).
Okkenhaug, K. et al. Impaired B and T cell antigen receptor signaling in p110δ PI 3-kinase mutant mice. Science 297, 1031–1034 (2002).
Flinn, I. W. et al. The phase 3 DUO trial: duvelisib vs ofatumumab in relapsed and refractory CLL/SLL. Blood 132, 2446–2455 (2018).
Flinn, I. W. et al. DYNAMO: a phase II study of duvelisib (IPI-145) in patients with refractory indolent non-Hodgkin lymphoma. J. Clin. Oncol. 37, 912–922 (2019).
Dreyling, M. et al. Phase II study of copanlisib, a PI3K inhibitor, in relapsed or refractory, indolent or aggressive lymphoma. Ann. Oncol. 28, 2169–2178 (2017).
Gopal, A. K. et al. PI3Kδ inhibition by idelalisib in patients with relapsed indolent lymphoma. N. Engl. J. Med. 370, 1008–1018 (2014).
Furman, R. R. et al. Idelalisib and rituximab in relapsed chronic lymphocytic leukemia. N. Engl. J. Med. 370, 997–1007 (2014).
Richardson, N. C., Kasamon, Y., Pazdur, R. & Gormley, N. The saga of PI3K inhibitors in haematological malignancies: survival is the ultimate safety endpoint. Lancet Oncol. 23, 563–566 (2022).
Matasar, M. J. et al. Copanlisib plus rituximab versus placebo plus rituximab in patients with relapsed indolent non-Hodgkin lymphoma (CHRONOS-3): a double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Oncol. 22, 678–689 (2021).
Barr, P. M. et al. Phase 2 study of idelalisib and entospletinib: pneumonitis limits combination therapy in relapsed refractory CLL and NHL. Blood 127, 2411–2415 (2016).
Lampson, B. L. et al. Idelalisib given front-line for treatment of chronic lymphocytic leukemia causes frequent immune-mediated hepatotoxicity. Blood 128, 195–203 (2016).
Chellappa, S. et al. The PI3K p110δ isoform inhibitor idelalisib preferentially inhibits human regulatory T cell function. J. Immunol. 202, 1397–1405 (2019).
Campo, E. et al. The 2008 WHO classification of lymphoid neoplasms and beyond: evolving concepts and practical applications. Blood 117, 5019–5032 (2011).
Horwitz, S. M. et al. Activity of the PI3K-δ,γ inhibitor duvelisib in a phase 1 trial and preclinical models of T-cell lymphoma. Blood 131, 888–898 (2018).
Alaggio, R. et al. The 5th edition of the World Health Organization Classification of Haematolymphoid Tumours: Lymphoid Neoplasms. Leukemia 36, 1720–1748 (2022).
Campo, E. et al. The International Consensus Classification of Mature Lymphoid Neoplasms: a report from the Clinical Advisory Committee. Blood 140, 1229–1253 (2022).
Ma, H. & Abdul-Hay, M. T-cell lymphomas, a challenging disease: types, treatments, and future. Int. J. Clin. Oncol. 22, 18–51 (2017).
Vose, J., Armitage, J. & Weisenburger, D. International peripheral T-cell and natural killer/T-cell lymphoma study: pathology findings and clinical outcomes. J. Clin. Oncol. 26, 4124–4130 (2008).
Bellei, M. et al. The outcome of peripheral T-cell lymphoma patients failing first-line therapy: a report from the prospective, International T-Cell Project. Haematologica 103, 1191–1197 (2018).
Coiffier, B. et al. Results from a pivotal, open-label, phase II study of romidepsin in relapsed or refractory peripheral T-cell lymphoma after prior systemic therapy. J. Clin. Oncol. 30, 631–636 (2012).
O’Connor, O. A. et al. Belinostat in patients with relapsed or refractory peripheral T-cell lymphoma: results of the pivotal phase II BELIEF (CLN-19) study. J. Clin. Oncol. 33, 2492–2499 (2015).
Horwitz, S. M. et al. Objective responses in relapsed T-cell lymphomas with single-agent brentuximab vedotin. Blood 123, 3095–3100 (2014).
O’Connor, O. A. et al. Pralatrexate in patients with relapsed or refractory peripheral T-cell lymphoma: results from the pivotal PROPEL study. J. Clin. Oncol. 29, 1182–1189 (2011).
Winkler, D. G. et al. PI3K-δ and PI3K-γ inhibition by IPI-145 abrogates immune responses and suppresses activity in autoimmune and inflammatory disease models. Chem. Biol. 20, 1364–1374 (2013).
Dong, S. et al. IPI-145 antagonizes intrinsic and extrinsic survival signals in chronic lymphocytic leukemia cells. Blood 124, 3583–3586 (2014).
Kaneda, M. M. et al. PI3Kγ is a molecular switch that controls immune suppression. Nature 539, 437–442 (2016).
De Henau, O. et al. Overcoming resistance to checkpoint blockade therapy by targeting PI3Kγ in myeloid cells. Nature 539, 443–447 (2016).
Horwitz, S. M. et al. Dose optimization of duvelisib in patients with relapsed or refractory peripheral T-cell lymphoma from the phase 2 PRIMO trial: selection of regimen for the dose-expansion phase. Blood 134, 1567–1567 (2019).
Lemonnier, F. et al. Recurrent TET2 mutations in peripheral T-cell lymphomas correlate with TFH-like features and adverse clinical parameters. Blood 120, 1466–1469 (2012).
de Leval, L. et al. The gene expression profile of nodal peripheral T-cell lymphoma demonstrates a molecular link between angioimmunoblastic T-cell lymphoma (AITL) and follicular helper T (TFH) cells. Blood 109, 4952–4963 (2007).
Couronne, L., Bastard, C. & Bernard, O. A. TET2 and DNMT3A mutations in human T-cell lymphoma. N. Engl. J. Med. 366, 95–96 (2012).
Cortes, J. R. et al. RHOA G17V induces T follicular helper cell specification and promotes lymphomagenesis. Cancer Cell 33, 259–273 (2018).
Ng, S. Y. et al. RhoA G17V is sufficient to induce autoimmunity and promotes T-cell lymphomagenesis in mice. Blood 132, 935–947 (2018).
Schaefer, A., Reinhard, N. R. & Hordijk, P. L. Toward understanding RhoGTPase specificity: structure, function and local activation. Small GTPases 5, 6 (2014).
Yu, B. et al. Structural and energetic mechanisms of cooperative autoinhibition and activation of Vav1. Cell 140, 246–256 (2010).
Xie, Y. & Jaffe, E. S. How I diagnose angioimmunoblastic T-cell lymphoma. Am. J. Clin. Pathol. 156, 1–14 (2021).
Wakatsuki, Y., Neurath, M. F., Max, E. E. & Strober, W. The B cell-specific transcription factor BSAP regulates B cell proliferation. J. Exp. Med. 179, 1099–1108 (1994).
Vogelzang, A. et al. A fundamental role for interleukin-21 in the generation of T follicular helper cells. Immunity 29, 127–137 (2008).
Nurieva, R. I. et al. Generation of T follicular helper cells is mediated by interleukin-21 but independent of T helper 1, 2, or 17 cell lineages. Immunity 29, 138–149 (2008).
Chtanova, T. et al. T follicular helper cells express a distinctive transcriptional profile, reflecting their role as non-Th1/Th2 effector cells that provide help for B cells. J. Immunol. 173, 68–78 (2004).
Ishii, S., Kurasawa, Y., Wong, J. & Yu-Lee, L. Y. Histone deacetylase 3 localizes to the mitotic spindle and is required for kinetochore-microtubule attachment. Proc. Natl Acad. Sci. USA 105, 4179–4184 (2008).
Noh, E. J. & Lee, J. S. Functional interplay between modulation of histone deacetylase activity and its regulatory role in G2–M transition. Biochem. Biophys. Res. Commun. 310, 267–273 (2003).
Britschgi, A. et al. JAK2/STAT5 inhibition circumvents resistance to PI3K/mTOR blockade: a rationale for cotargeting these pathways in metastatic breast cancer. Cancer Cell 22, 796–811 (2012).
Moskowitz, A. J. et al. A phase 2 biomarker-driven study of ruxolitinib demonstrates effectiveness of JAK/STAT targeting in T-cell lymphomas. Blood 138, 2828–2837 (2021).
Bourd-Boittin, K. et al. CX3CL1/fractalkine shedding by human hepatic stellate cells: contribution to chronic inflammation in the liver. J. Cell. Mol. Med. 13, 1526–1535 (2009).
Shen, X. et al. CD4 T cells promote tissue inflammation via CD40 signaling without de novo activation in a murine model of liver ischemia/reperfusion injury. Hepatology 50, 1537–1546 (2009).
Kimura, K., Nagaki, M., Takai, S., Satake, S. & Moriwaki, H. Pivotal role of nuclear factor κB signaling in anti-CD40-induced liver injury in mice. Hepatology 40, 1180–1189 (2004).
Ikeda, A. et al. Progression of autoimmune hepatitis is mediated by IL-18-producing dendritic cells and hepatic CXCL9 expression in mice. Hepatology 60, 224–236 (2014).
Tsutsui, H. et al. IL-18 accounts for both TNF-α- and Fas ligand-mediated hepatotoxic pathways in endotoxin-induced liver injury in mice. J. Immunol. 159, 3961–3967 (1997).
Ho, R. T., Liew, C. T. & Lai, K. N. The expression of hepatocyte growth factor (HGF) and interleukin 6 (IL-6) in damaged human liver and kidney tissues. Hepatogastroenterology 46, 1904–1909 (1999).
Jo, J. C. et al. Peripheral T cell lymphomas in elderly patients: a retrospective analysis from the Hematology Association of South East Korea (HASEK). Ann. Hematol. 95, 619–624 (2016).
Mehta, N. et al. A retrospective analysis of peripheral T-cell lymphoma treated with the intention to transplant in the first remission. Clin. Lymphoma Myeloma Leuk. 13, 664–670 (2013).
Robert, C. et al. Improved overall survival in melanoma with combined dabrafenib and trametinib. N. Engl. J. Med. 372, 30–39 (2015).
Oki, Y. et al. Phase I study of panobinostat plus everolimus in patients with relapsed or refractory lymphoma. Clin. Cancer Res. 19, 6882–6890 (2013).
Witzig, T. E. et al. The mTORC1 inhibitor everolimus has antitumor activity in vitro and produces tumor responses in patients with relapsed T-cell lymphoma. Blood 126, 328–335 (2015).
Szolek, A. et al. OptiType: precision HLA typing from next-generation sequencing data. Bioinformatics 30, 3310–3316 (2014).
Zaitsev, A. et al. Precise reconstruction of the TME using bulk RNA-seq and a machine learning algorithm trained on artificial transcriptomes. Cancer Cell 40, 879–894 (2022).
Racle, J., de Jonge, K., Baumgaertner, P., Speiser, D. E. & Gfeller, D. Simultaneous enumeration of cancer and immune cell types from bulk tumor gene expression data. eLife 6, e26476 (2017).
Ng, S. Y. et al. Targetable vulnerabilities in T- and NK-cell lymphomas identified through preclinical models. Nat. Commun. 9, 2024 (2018).
Su, Y. et al. Multi-omics resolves a sharp disease-state shift between mild and moderate COVID-19. Cell 183, 1479–1495 (2020).
Acknowledgements
This was an investigator-initiated study funded initially by Infinity Pharmaceuticals and subsequently by Verastem and Secura Bio as well as by Leukemia & Lymphoma Society (LLS) Specialized Center of Research (SCOR) 7011-16, LLS SCOR 7026-21 and National Cancer Institute (NCI) R35 CA231958. Medical writing support was provided by S. Lalchandani. S.M.H. was supported by Nonna’s Garden Foundation. A.J.N. was supported by NCI R00 CA256497. S.A.V. was supported by a Steven A. Greenberg Lymphoma Research Grant. We would like to thank our patients and their families as well as the faculty and research staff of our various institutions.
Author information
Authors and Affiliations
Contributions
S.M.H. designed the study, with input from Infinity Pharmaceuticals and Verastem. S.M.H., E.D., N. Ganesan, N. Galasso, T.D., H.H., L.P., C.M., A. Bahgat, E.M., E.C., Z.C., J.W.A., C.T. and S.A. contributed to clinical trial execution and monitoring. S.M.H., A.M., A. Noy, A.K., E. J., D.C.F., N.M.-S., Y.K., W.W. and M.K. enrolled patients on the study. J.R., R.X., N.K., A. Nirmal, O.K., V.Z., K.Z., N.S., M.S., S.D., E.P. and A. Bagaev analyzed genomic and transcriptomic data. A.J.N., R.X. and D.M.W. performed in vitro assays and in vivo xenograft studies. K.H., D.M. and J.J.B. performed Olink proteomic analysis. S.M.H., A.J.N., J.R., R.X., D.M.W. and S.A.V. wrote the manuscript, with writing support from Secura Bio. All authors edited the manuscript and approved of all edits before submission.
Corresponding authors
Ethics declarations
Competing interests
D.M.W. is an employee of Merck and Co.; owns equity in Merck and Co., Bantam, Ajax and Travera; received consulting fees from AstraZeneca, Secura Bio, Novartis and Roche/Genentech; and received research support from Daiichi Sankyo, AstraZeneca, Verastem, AbbVie, Novartis, Abcura and Surface Oncology. S.A.V. has served as an advisor for Immunai and has received consulting fees from ADC Therapeutics and Koch Disruptive Technologies. J.J.B. received consulting fees from Sobi, Omeros, Bluebird Bio, Sanofi, Immusoft, SmartImmune, Bluerock and Advanced Clinical. N.M.-S. has received institutional clinical trial funding from AstraZeneca, Bristol Myers Squibb, Celgene, C4 Therapeutics, Corvus Pharmaceuticals, Daiichi Sankyo, Genentech/Roche, Innate Pharmaceuticals, Secura Bio/Verastem, Yingli Pharmaceuticals and Dizal Pharmaceuticals. N.M.-S. has also received compensation for service as a consultant for AstraZeneca, Secura Bio/Verastem, Daiichi Sankyo, C4 Therapeutics, Genentech, Janssen, Karyopharm Therapeutics and Kyowa Hakko Kirin. N.M.-S. is funded as a Scholar in Clinical Research through the Leukemia & Lymphoma Society, and this study was reviewed as part of the ASCO/AACR Workshop. S.M.H. has received research support from ADC Therapeutics, Affimed, C4, Celgene, CRISPR Therapeutics, Daiichi Sankyo, Dren, Kyowa Hakko Kirin, Millennium/Takeda, Seattle Genetics and Secura Bio. S.M.H. has also received consulting fees from Affimed, Abcuro, Corvus, Daiichi Sankyo, Kyowa Hakko Kirin, ONO Pharmaceuticals, SeaGen, Secura Bio, Takeda and Yingli Pharmaceuticals. A.J.M. has received research support from BeiGene, Seattle Genetics, Merck, Bristol Myers Squibb, Incyte, Affimed and AstraZeneca. A.J.M. has also received consulting fees from Affimed, Merck, Seattle Genetics and Takeda. The remaining authors declare no competing interests.
Peer review
Peer review information
Nature Medicine thanks Weili Zhao, Sonali Smith and Michael Schell for their contribution to the peer review of this work. Primary Handling Editor: Saheli Sadanand, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Expanded enrollment diagram for NCT#02783625.
Expanded diagram showing enrollment on NCT#02783625.
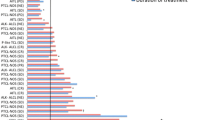
Extended Data Fig. 2 Study design and outcomes of NCT #02783625 in patients with PTCL and CTCL.
(a) Swimmer’s plot depicting responses of patients with PTCL to bortezomib + duvelisib (Arm B). (b) Kaplan-Meier curve showing event-free survival of all PTCL patients stratified by treatment arm. (c) Swimmer’s plot depicting responses of patients with CTCL to romidepsin + duvelisib (Arm a) or bortezomib + duvelisib (Arm B) as indicated. (d) Kaplan-Meier curve showing event-free survival of patients with CTCL, stratified by treatment arm.
Extended Data Fig. 3 A tumor-specific T follicular-helper phenotype is associated with response to romidepsin and duvelisib.
(a) Best response of patients with PTCL receiving romidepsin + duvelisib in Arm A compared with NCT00426764, stratified by whether PTCL were of follicular helper subtype. (b) Oncoprint of somatic mutations observed in pre-treatment biopsy samples from patients with PTCL, organized by treatment response and frequency. Stars indicate genes in which mutations are enriched in either responders (R) or non-responders (NR). (c) Lollipop plot of individual mutations in genes commonly mutated in PTCL with Tfh features. (d) Genes enriched in responders versus non-responders in pre-treatment samples obtained from patients with PTCL. (e) B-cell proportions estimated by CIBERSORT deconvolution in pre-treatment samples from responders (N=13) versus non-responders (N=10). Data are presented as box plots with center depicting median, bounds of box depicting interquartile range, and whiskers depicting minima and maxima. (f) Enrichment of IL21 in pre-treatment bulk RNA-seq samples from PTCL responders (N=5) versus non-responders (N=7) to romidepsin and duvelisib. Data are presented as box plots with center depicting median, bounds of box depicting interquartile range, and whiskers depicting minima and maxima. P values calculated by Chi squared test (a), Wald Test corrected for False Discovery Rate using the Benjamini-Hochberg procedure (d), student’s t-test (e), and two-sided Wilcoxon Rank-Sum Test (f).
Extended Data Fig. 4 Pre-treatment predictors of response to romidepsin and duvelisib in patients with PTCL and CTCL.
(a) Dot plot depicting enrichment of MSigDB genesets in pre-treatment bulk RNA-seq from responding vs. non-responding patients with PTCL. (b) Oncoprint of somatic mutations observed in pre-treatment biopsy samples from patients with CTCL, organized by treatment response and frequency. (c) Lollipop plot of individual mutations in NFKB2 in patients with CTCL. (d) Copy number plot depicting alterations by chromosome in patients with CTCL. RET and NFKB2 genes loci are indicated. (e) Genes enriched in responders versus non-responders in pre-treatment samples obtained from patients with CTCL. P values determined by Wald Test corrected for False Discovery Rate using the Benjamini-Hochberg procedure (e).
Extended Data Fig. 5 Mechanisms of response to romidepsin and duvelisib in PTCL xenografts and patient samples.
(a) Experimental design and survival of mice xenografted with an AITL xenograft and treated with either vehicle, romidepsin, duvelisib, or the combination. (b) Decrease in mitosis-associated MSigDB genesets in on-treatment versus pre-treatment samples from PTCL patients who responded to therapy (left) and AITL xenografts (right). Normalized enrichment score (NES), false discovery rate (FDR) and proportion of genes expressed in each gene set are as described. P values calculated using log-rank test (a) and estimated as the number of random gene set enrichment scores with the same or more extreme values divided by the total number of randomly generated gene sets, corrected for False Discovery Rate using the Benjamini-Hochberg procedure (b).
Extended Data Fig. 6 JAK/STAT-driven resistance to romidepsin and duvelisib.
(a) Proportion of patients with activation mutations or amplifications of JAK/STAT genes, stratified by response. (b) Copy number plot depicting alterations by chromosome in patients with PTCL. STAT1 locus on chromosome 2 is highlighted. (c) Lollipop plot of pre-treatment mutations in JAK1 and JAK3 in non-responders to romidepsin + duvelisib. (d) UMAP of CD45+ cells isolated from pre- and on-treatment peripheral blood samples obtained from patients with high-burden circulating disease receiving romidepsin + duvelisib. (e) Expression of T-cell markers on malignant cells from Patients Y and Z visualized in 2-dimensional UMAP space. (f) Differently expressed genes in malignant cells isolated from the peripheral blood of a patient who did not respond to romidepsin + duvelisib. (g) Expression of IL6_JAK_STAT3 genes in pre-treatment and on-treatment circulating malignant T-cells from patients with (Z) or without (Y) response to romidepsin + duvelisib. (h) Gene set enrichment analysis of HALLMARK_IL6_JAK_STAT3_SIGNALING in PDX tumors refractory to duvelisib monotherapy. P values determined by Fisher’s exact test (a), two-sided Wilcoxon Rank-Sum Test with Bonferroni correction for multiple comparisons (f), student’s t-test (g), and estimated as the number of random gene set enrichment scores with the same or more extreme values divided by the total number of randomly generated gene sets, corrected for False Discovery Rate using the Benjamini-Hochberg procedure (h).
Extended Data Fig. 7 PI3K/mTORC1 reactivation in tumors resistant to romidepsin and duvelisib.
(a) Emergence of clones with indicated mutations in patients treated with romidepsin + duvelisib who ultimately experienced disease progression. (b) Expression of PI3K_AKT_MTOR genes in pre-treatment and on-treatment circulating malignant T-cells from patients with (Z) or without (Y) response to romidepsin + duvelisib. (c) Efficient CRISPR editing of TSC2 and PTEN expression by 2 independent guide RNAs as shown by western blot. (d) Sensitivity of OCI-ly13.2 cells expressing Cas9 and doxycycline-inducible sgRNA targeting TSC2 (above) or PTEN (below) to duvelisib in vitro, with (N=3) or without (N=3) the addition of doxycycline to induce gene editing. Data presented as mean values +/- SD and are representative of two independent experiments. (e) Decrease in phagocytosis-associated MSigDB genesets in on-treatment versus pre-treatment samples from PTCL patients who did not respond to therapy. (f) Estimated intratumoral macrophage abundance, based on CIBERSORT deconvolution, in pre-treatment and on-treatment biopsies of patients undergoing treatment with romidepsin + duvelisib, stratified by response (non-responder pre-treatment N=11, non-responder on-treatment N=10, responder pre-treatment N=12, responder on-treatment N=10). Data are presented as box plots with center depicting median, bounds of box depicting interquartile range, and whiskers depicting minima and maxima. P values determined using student’s t-test (b) and estimated as the number of random gene set enrichment scores with the same or more extreme values divided by the total number of randomly generated gene sets, corrected for False Discovery Rate using the Benjamini-Hochberg procedure (e).
Extended Data Fig. 8 Persistent NF-kB signaling and proliferation in patients with clinically significant adverse events following romidepsin and duvelisib.
(a) Changes in plasma analytes between C1D8 and C1D1 samples in patients treated with duvelisib or duvelisib + romidepsin as indicated. (b) UMAP of CD45+ cells isolated from pre- and on-treatment peripheral blood samples obtained from patients without circulating disease receiving romidepsin + duvelisib. (c) Dot plot depicting average expression and frequency of expression of genes defining CD4+T, CD8+T, and myeloid cell subsets as indicated. (d) Differentially expressed genes in pre-treatment peripheral blood CD14+ monocytes from patient experiencing clinically significant (Grade 2-3) versus non-significant (Grade 0-1) hepatotoxicity. P values calculated using two-sided Wilcoxon Rank-Sum Test with Bonferroni correction for multiple comparisons (d).
Supplementary information
Supplementary information
Supplementary Fig. 1, Supplementary Tables 1–5 and Protocol.
Source data
Source Data Extended Data Fig./Table 7
Unprocessed western blots for Extended Data Fig. 7.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Horwitz, S.M., Nirmal, A.J., Rahman, J. et al. Duvelisib plus romidepsin in relapsed/refractory T cell lymphomas: a phase 1b/2a trial. Nat Med 30, 2517–2527 (2024). https://doi.org/10.1038/s41591-024-03076-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-024-03076-6
- Springer Nature America, Inc.