Abstract
Erectile dysfunction (ED) is defined as the inability to attain and maintain erection of the penis sufficient to permit satisfactory sexual activity. ED most commonly affects men from 40 years of age with a clear age-associated increase in prevalence. The condition may have significant negative impact on quality of life for both the patients and their partners. Over recent years, low-intensity shockwave therapy (LIST) has gained popularity in the treatment of ED, based on the assumption that LIST application may result in neoangiogenesis and thus increased blood flow to the corpora cavernosa. The increasing usage of LIST is contrasting with current guidelines, with the EAU guideline on ED stating that LIST can be used in mild organic ED patients or poor responders to PDE5I’s, but with a weak strength of recommendation. In the AUA guideline on ED, the panel makes a conditional recommendation of grade C that LIST should be considered investigational. In this review, we will briefly review practice patterns, and critically discuss the evidence based on which these guideline statements have been made.
Similar content being viewed by others
Introduction
Erectile dysfunction (ED) is defined as the inability to attain and maintain erection of the penis sufficient to permit satisfactory sexual activity [1]. ED most commonly affects men from 40 years of age with a clear age-associated increase in prevalence [2]. There is a large number of disorders known to contribute to the development of ED, including but not limited to diabetes, hypogonadism, metabolic syndrome, cardiovascular disease, cigarette smoking, pelvic nerve injury, and local disorders, such as Peyronie’s disease [3,4,5,6,7,8]. The condition may have significant negative impact on quality of life for both the patients and their partners [9].
Understanding of the molecular aspects of ED pathogenesis has successfully resulted in widespread use of phosphodiesterase type 5 inhibitors (PDE5i). As these drugs interfere with the nitric oxide (NO)–cyclic guanosine monophosphate (cGMP) pathway, an intact NO supply from the nerves and endothelium is needed to guarantee the efficacy of these agents [10]. Several prevalent diseases reduce the bio-availability of NO and men with these underlying pathologies, such as diabetes, commonly do not respond as well to PDE5 inhibitors as patient without these comorbidities [11]. Available pharmacological treatments are effective in about 60% of patients and mostly well tolerated, but in some patients usage is limited by the frequent occurrence of bothersome side effects, such as headache, dyspepsia, muscular pains, and hot flushes [12, 13]. Furthermore, PDE5 inhibitors are contraindicated in combination with nitrate medication for angina, because of the risk of hypotension, while there is a clear overlap in patient population due to the similar underlying pathogenesis [14]. Most of these treatments take the spontaneity out of sex as it needs to be planned accordingly and this may feel unnatural to some patients and their partners. Patients experiencing treatment failure or adverse events now face no other choice than to resort to more invasive options such as intracavernous injection, vacuum devices, and finally penile prosthesis implantation [15]. Besides these well-known limitations to the currently available treatment armamentarium, these modalities are solely providing symptom relief and do not provide a permanent improvement of the condition or an increase in spontaneous erections by targeting the underlying pathophysiological processes. Notably, however, in a 1998 study published at the time of marketing of the first available PDE5 inhibitor sildenafil, the highest rank measure of treatment success in terms of importance for ED patients was “cure” [16]. A cure for ED resulting in spontaneous unassisted intercourse entices research into novel regenerative treatment methods, and as stated by Fode et al. [17], low-intensity extracorporeal shockwave therapy (LIST) is the only currently marketed treatment for ED that may achieve this goal. Over the last 10 years, LIST has emerged and is looked at as a putative solution for ED [18].
A shockwave is a longitudinal acoustic wave consisting of a short pulse of about 5 μs duration that is characterized by a near instantaneous jump to a peak positive acoustic pressure, hence the referral to a “shock”, which is then followed by a longer-lasting negative pressure period [19]. When these shockwaves are of low intensity, the application there-of is non-invasive and the shockwaves can be focused to target specific areas of organs to induce the desired effects. The exact mechanism of action in ED is unknown but briefly, the ruling belief is that acoustic waves release energy by the formation and collapse of so-called microbubbles, which in turn activate cellular pathways resulting in the expression of local growth factors and chemoattractants, which in turn set in motion a variety of cellular events which lead to improved endothelial function, angiogenesis, and perhaps even regeneration of nerve fibers [17, 20,21,22,23].
The major potential advantage of LIST is the promise of restoration of the ability to have natural erections. The treatment has also been suggested to improve the effect of PDE5i in non-responders, thus negating the need for more invasive treatments [24,25,26,27]. Although not all studies have shown convincing effects, this has created great enthusiasm about LIST for ED, resulting in a large uptake in the use of this therapeutic option worldwide. The increasing usage of LIST is contrasting with current guidelines, with the EAU guideline on ED stating that LIST can be used in mild organic ED patients or poor responders to PDE5Is, but with a weak strength of recommendation [15]. It is further elaborated that therefore “clear and definitive recommendations cannot be given”, and that “the publication of unequivocal evidence from additional randomized controlled trials (RCTs) and longer-term follow-up would provide more confidence regarding the use of LIST”. In the AUA guideline on ED, the panel makes a conditional recommendation of grade C that LIST should be considered investigational [28].
In this review, we will briefly review practice patterns, and critically discuss the evidence based on which these guideline statements have been made.
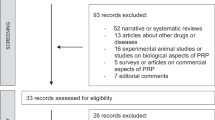
Methods
We performed a non-systematic narrative and interpretative literature review.
An extensive research using Medline has been conducted retrieving English articles until 30 October 2018. The search terms included: “erectile dysfunction” OR (“erection” OR “sexual dysfunction”) AND (“shockwave” OR “shockwave therapy” OR “low-intensity shockwave” OR “LIST” OR “ESWT”). Reference lists of retrieved articles were scanned for additional suitable articles.
We included original RCTs and single-arm studies that investigated the clinical application of LIST for the treatment of ED in human adults. We excluded original research articles applying shockwaves for other either-or-not related medical conditions such as chronic pelvic pain syndrome, prostatitis, and Peyronie’s disease. Meta-analyses and systematic reviews were included when they discussed and made conclusions on LIST for ED, also if a subset of included patients had LIST for related conditions and ED improvement was a secondary outcome parameter.
Single-arm studies and non-placebo-controlled RCTs
Vasculogenic ED
The first single-arm-study showing a proof of concept for the use of LIST in ED was performed by Vardi et al. [18] in 2010 and included mainly vasculogenic ED patients. As the principle disease mechanism is a reduction in cavernosal arterial blood flow, these researchers hypothesized that effects on neovascularization induced by LIST in the heart might also hold potential for the treatment of ED, by improving arterial blood supply to the erectile tissue in the corpora cavernosa. This pilot study included 20 patients and employed a focussed hydraulic generator. Patients received 12 sessions of 1500 shocks to five areas of the corpora and crura with an energy flux density (EFD) of 0.09 mJ/mm [2]. The employed protocol was based on the methodology used in two clinical trials investigating LIST in patients with cardiovascular disease. The improvement observed after 6 months of follow-up was +7.1 mean points on the Internationale Index of Erectile Function (IIEF)-EF domain, which is a relatively large effect size, and is comparable to the effect seen in clinical trials on PDE5 inhibitors in this subset of patients. This study generated a lot of interest, and several single arm and comparative trials have since ensued. Other studies using focused shockwaves in vasculogenic patients have, in spite of varying treatment protocols in terms of energy settings, number of sessions, and number of shocks, consistently shown beneficial effects with increases of IIEF-EF or IIEF-5 scores ranging from 2.5 to 5.8 points when employed as monotherapy or combined with PDE5 inhibitors (Table 1). In various studies investigating the effects of shockwave therapy on ED, achieving an erectile hardness score (EHS) of 3–4 (which corresponds to having erections sufficiently rigid for penetration) is defined as success of treatment. The percentage of patients achieving an erectile hardness score of >3 are close to 60% in patients with mild–moderate vascular ED (Table 1). In the one study employing the sexual encounter profile (SEP) as outcome measure, the percentage of positive responses to SEP question 2 (recording the percentage of attempts where the penis was sufficiently rigid for penetration) was 85.5% in patients treated with 6 × 5000 shocks with the Aries 2 device to 91% when the number of shocks was doubled in a comparative randomized non-placebo-controlled trial designed to compare different protocols (Table 1) [29].
In order to overcome the theoretical limitation that focused shockwaves are providing energy to a very small area, it has been proposed that linear distribution of shockwaves may provide a better coverage of the corpora cavernosa and thus improve treatment outcomes. Based on this assumption, most treatment protocols using linear shockwaves have reduced the number of sessions to four once-weekly sessions of 3600–5000 shocks (Table 1). Results of four single-arm trials and one non-placebo-controlled RCT comparing two different protocols delivering the same number of shocks in a different distribution show improvements in IIEF-EF scores reaching a maximum of +7.5 in patients with vasculogenic ED [18, 29,30,31,32].
PDE5 inhibitor non-responders
Five noncomparative trials have assessed the effects of LIST in patients who previously did not respond to PDE5 inhibitors, and have shown consistently positive effects in improving unassisted erections as well as improving the response to PDE5 inhibitors (Table 1) [24,25,26, 33, 34]. Overall review of the available data suggests that PDE5I non-responders have lower response rates than those observed in the treatment-naïve or PDE5I responders, which may or may not be associated with the fact that they are more likely to suffer from moderate or severe ED, rather than from mild ED. While the improvements in unassisted erections were therefore modest, Gruenwald et al. [24] have shown that responses to PDE5 inhibition after shockwave therapy can be ameliorated to the realm of a 10 point increase in the IIEF-EF domain score.
Post-prostatectomy ED
Only one non-placebo-controlled study looked into the effects of LIST in the population of patients who developed ED as a result of undergoing nerve-sparing radical prostatectomy (Table 1). Frey et al. [35] studied 18 patients with mild to severe postoperative ED, who were median 2 years post-prostatectomy. They provided six treatment sessions over a 6-week period, using the Duolith SD1, which delivers focused shockwaves. The median change in IIEF-5 score was +3.5 points after 1month, which had been reduced to +1 point after 12 months. Another study included 30 men with mild-moderate or mild ED of mixed aetiologies [33]. Only three of these men had post-prostatectomy ED. While the authors showed positive effects for the whole group, they did mention there was a greater improvement in erectile function (EF) in men with vasculogenic ED compared with those who had undergone radical prostatectomy, without giving specific numbers for each subgroup.
Heterogeneity in outcomes and methodology
Of note, most of the patient-reported outcome measures used by these single-arm trials have been validated and can be regarded as reliable. However, the heterogeneity in the use of EHS, IIEF-EF, IIEF-5, and the SEP makes comparison of the various trials difficult (Table 1). For the IIEF-EF, so-called “minimal clinically important differences” (MCID) have been defined as the minimal amount of change needed in the EF domain to be clinically meaningful to patients. These were defined according to baseline ED severity (mild: 2; moderate: 5; severe: 7) by Rosen et al. in 2011 [36]. If no specific severity category is considered, the MCID for the IIEF-EF is 4. Nonetheless, some authors have employed other variations as outcome measures, such as defining success of treatment when a patient has a 5-point improvement in IIEF-EF or IIEF-5 score. Except for the MCIDs defined by Rosen et al., these measures have not been validated and should be used with caution.
A factor that makes interpretation of study results difficult is the heterogeneity in terms of devices and protocols employed. Various studies have used devices with linear vs focussed shockwave application, have used different numbers of shocks and sessions, and different EFD (Table 1). As a direct comparison of devices is lacking, it remains very difficult to reach any conclusion on the “ideal” means of LIST. Until recently, there had not been any dose-finding studies reported. In 2018 however, Kalvyanakis et al. [29] showed an improvement of 3.1 point on IIEF-EF after six sessions, and 5.1 points after 12 sessions of 5000 shocks each on the Aries device [29]. SEP2 responses improved correspondingly. This was the first report that showed a dose-dependent effect of LIST, which supports the notion that protocols may need optimization to reach maximal effect, and many single-arm studies (as well as RCTs) may have not been using optimal settings. A second trial coordinated by Ramasamy at the university of Florida is running and the first interim results show that results may differ according to the protocol employed; however, the number of patients who have completed their treatment in this interim report is still very low (n = 21) [37].
Follow-up is generally quite short (Table 1) and as clearly illustrated by Frey et al. [35] and Kitrey et al. [38], encouraging results can be obtained in the first few months which can relatively quickly wane over the months thereafter. It has been shown that a mere 50% have a long-term durable response. Again, this is a limitation in the majority of studies.
The placebo effect in clinical ED research
Placebo effect can be prominent in ED research, and it has been described that placebo effect in ED treatment may exceed 30% [39]. To illustrate this, Carvalho de Araujo et al. [40] designed a prospective, controlled, single-blind, parallel-group study with 123 patients with ED: all patients got placebo treatment. Group 1 was informed to be receiving a substance for ED treatment and in this group there was an increase in IIEF-EF scores of 3.3 points. Group 2 was informed that they could be receiving an active drug or placebo and increased their IIEF-EF with 2.9 points. The most striking result however, was observed in the third group which contained patients conscious to be using placebo, who improved their IIEF-EF with 4 points, thus representing a minimal clinically important difference according to Rosen’s criteria. The important lesson to learn from these data is that ED patients under active treatment in study setting are likely to experience an improvement in their IIEF scores. Hence, single-arm studies and open label non-controlled trails are to be regarded as hypothesis generating and should not be included in an evidence review aimed at making practice recommendations or guidelines.
Randomized placebo-controlled trials
Outcomes and quality
To overcome the limitations in interpretation of cohort studies, both prospective and retrospective, randomized, double-blind and placebo-controlled trials have been conducted in the field of LIST for ED. In our non-systematic review of the current literature, we were able to identify 10 RCTs. Eight out of ten RCTs focussed on vasculogenic patients, which, following the theoretical background of shockwave benefits, seems to be the most suitable target group. One RCT looked into the effects of LIST in PDE5 inhibitor non-responders [27]. All retrieved studies can be found in Table 2. A quick overview learns that some of these RCTs have looked at longer time points than most single-arm studies, with results being reported up to 12 months after initial treatment. Fojecki et al. [41, 42] reported initial and long-term follow-up in two separate papers; hence, this trial is included twice in the overview. Two trials report non-significant results on the primary outcome parameter [42, 43]. Another trial reports significant result in EHS, but non-significant results the primary outcome, being IIEF-5 [44]. Four other trials have a high risk of bias and we believe that therefore the results stemming from these trials should be interpreted with caution [45,46,47]. This leaves three nonbiased RCTs with positive results (ranging from a 4 to 7 point IIEF-EF increase) [27, 48,49,50]. All of the studies have a low number of randomized patients (40, 37, and 46 respectively) and two of them have a follow-up of only 1 month [27, 48].
Summarizing, we can conclude that the number of unflawed RCTs with positive outcome is rather low and does not supersede the number of negative unflawed RCTs. Furthermore, there may be issues with the power of most of these trials, details of which will be discussed below.
Limitations in methodology
One limitation in a number of RCTs is the use of a sham probe. LIST can be felt when applied as a tingling sensation or even as small shocks. The majority of RCTs use a special cap on the shockwave probe that limits transmission of the shockwave through this cap to the targeted tissue [42, 44]. This way, the device will make the exact same sound as it would during active treatment. The question remains whether patients do not expect to feel at least something in the penis during treatment and whether this is influencing results. This of course remains speculative and we do not have a specific suggestion on how this can be done differently. Others trials have used a sham probe provided by the manufacturer, making the same sound and vibration as the active probe used in the treatment group [27, 46,47,48,49]. One trial has played the sound of the shockwave machine trough speakers in the room while applying a non-functioning sham probe [45]. It is hard to believe that patients here did not have a sense they were in a sham-treatment group and this may lead to violation of allocation concealment and thus selection bias and performance bias. A similar methodological flaw is encountered in the article by Yee et al. [43], in which the sham treatment is vaguely described as being the same probe with energy setting at 0 and a similar noise being produced.
One trial was a potentially adequately powered RCT in 126 men, in which both placebo and active treatment groups experienced a slight increase in IIEF-EF scores in the magnitude of 1.5–2 points, but inter-group comparison revealed no statistically significant difference (Table 2) [41]. The protocol read that authors used a novel linear piezoelectric therapy source with a gel-pad number 0, which covers an area of 5 cm long and 1 cm deep (which should be adequate for reaching the cavernous tissue). However, manufacturer’s instructions read that the gel-pad 0 should be used for superficial indications (such as wound healing) as the maximum depth of penetration is at the surface of the pad. It is therefore questionable whether or not the patients received adequate energy to the corpora cavernosa.
The study that looked at the role of LIST in penile rehabilitation post nerve-sparing radical cystoprostatectomy was a non-blinded randomized controlled trial, with the lack of blinding causing an important risk of selection bias [50]. Furthermore, the study was potentially underpowered as the 152 patients were divided over three groups, being patients receiving LIST, PDE5i, and no therapy (with 49, 51, and 52 patients respectively). The authors found statistically significant recovery of EF in every group but no difference in the recovery of potency among the groups, stating that LIST could be an alternative to PDE5i when these are contraindicated. We find that the quality of the evidence, however, is not high enough to support this claim.
Limitations in outcome reporting
Not all RCTs that have been published mention a prospective registration on a publicly accessible registry such as clinicaltrials.gov, and not all RCTs report according to the CONSORT statement guidelines. In the trial by Olsen et al. [44], conducted in Denmark, researchers found that LIST improved the EHS but not the IIEF-5 score. There is no clear explanation for this inconsistency but as stated in our previous review, it may be speculated that EHS is a more robust tool while the IIEF-5 is able to detect more subtle differences [17]. However, it is important to note that IIEF-5 was stated as the main outcome of the study and that EHS is not validated in the relevant language. Furthermore, the primary outcome parameter when the study was registered on clinicaltrials.gov was the percentage of patients reaching an improvement of at least 5 points on the IIEF-5 (defined as “success”), and this was what the study was powered for. However, this outcome was not reported in the final manuscript, and hence, it is questionable whether the study was adequately powered for the outcomes reported and the occurrence of reporting bias should be considered here. The clinicaltrials.gov record, however, is no longer retrievable.
Motil et al. [45] report on a multicentric RCT with 125 participants and 1 month follow-up. Description of the used methodology in this trial was poor. The authors applied the MCID, which was validated for IIEF-EF on the IIEF-5. While they report a benefit of on average 4.2 points on the IIEF-5 and while they (erroneously) report 81% of patients achieve MCID, no statistical analysis is given to support these claims.
Sources of bias in RCTs
Srini et al. [46] report on a RCT which enrolled 135 patients but suffered from an unusually high drop-out rate of 58% in the placebo group and 42% in the active treatment group, leaving only 77 patients for final analysis with only 17 in the placebo arm. In this regard, a drop-out rate of >20% is considered to pose serious threats to study validity and incomplete outcome reporting will indeed result in attrition bias. This high drop-out rendered the trial underpowered resulting in unequal groups at baseline. While the authors claim that there was an increase in IIEF-5 score in the active treatment group of 8.7 points higher than the increase in het placebo arm, it should be noted that in the placebo group the number of patients with comorbidities and cardiovascular risk factors was higher. The trial performed by Yamaçake et al. [47] suffers from similar issues. They investigated the use of the Dolorclast® Smart (Electro Medical Systems, Switzerland) in patients with ED linked to kidney failure treated with transplantation. The authors find an apparent effect of 6 treatments sessions with 7/10 patients in the treatment group experiencing an improvement of at least 5 points on the IIEF-5 scale vs only 1/10 in the sham group. This study is underpowered by large with only 10 men in each group, again resulting in unequal groups at baseline following randomization. The baseline IIEF-5 score is lower in the LIST group compared to the sham group (10.9 vs 14.9). This is important because a given numeric improvement in the IIEF-5 score is likely to have less clinical meaning with low scores compared to higher scores. In addition, the finding that the changes in EHS scores do not differ over time between the groups and the lack of difference in penile hemodynamic parameters should raise concerns that confounding factors may in fact have played a role.
Meta-analyses and systematic reviews
In light of the conflicting results of often underpowered RCTs in this field, authors have attempted to summarize findings and increase the level of evidence for LIST for ED by performing systematic reviews and meta-analyses. While indeed meta-analyses of RCTs increase the level of evidence and are a tool to provide definitive answers on the efficacy of LIST, we believe that the five currently published meta-analyses have some flaws of their own, making their findings less reliable than expected (Table 3) [51,52,53,54,55]. First of all, various authors have neglected to exclude studies at high risk of bias even though the trial quality was correctly evaluated with dedicated tools, or they did not take account for possible biases in the studies [51,52,53,54,55]. Since the studies most burdened with a high risk of bias also have the largest reported effects size, the inclusion of these trials skew the results of meta-analyses towards positive results for LIST compared to placebo. Secondly, studies assessing ED as a secondary outcome have been included on equal terms in the analyses [51,52,53]. Those trials investigated the effects of shockwaves in Peyronie’s disease, chronic prostatitis, and chronic pelvic pain; as such, beneficial effects on ED may be only a consequence of the improvement of pain or other symptoms that could impact sexual or genito-urinary health and thereby quality of life. Thirdly, there are some methodological flaws that hamper the interpretation of the results of meta-analyses. Lu et al. [51] copied erroneous outcome data into their meta-analysis, and Clavijo et al. [53] included data from Feldman et al. [56], which was a conference abstract rather than a fully published manuscript and which may have included participants from studies from Israel, who were already independently included in the meta-analysis, thus resulting in a double inclusion of positive results. Even more, most meta-analyses have included Fojecki et al., which as discussed above used an inappropriate gel pad. This was a possible explanation for the negative results and therefore may skew the conclusions of meta-analysis in the direction of placebo [42]. The same goes for the study by Srini et al. [46], which has a high risk of bias because of the extensive drop-out rate and is included in four of the meta-analyses [52,53,54,55]. Last, methods and results of included RCTs are heterogenous, making comparison, even in a random effects model, very difficult.
When examining the results of contemporary meta-analyses, we have to conclude that in spite of methodological flaws, most of these analyses report a modest statistically significant benefit for active treatment, which is generally below the MCID, or report results above MCID [53] without reaching significance.
Conclusions and recommendations
In recent literature, frequent claims have been made on the beneficial effects of LIST for vascular ED, and LIST has been shown to potentially convert PDE5i non-responders into responders. We feel these claims are not always justified. Single-arm studies have consistently shown benefit but the placebo effect is very common in ED research which necessitates RCTs. Up to now, 10 RCTs have been performed with mixed results and many of those suffer from various sources of bias and/or are underpowered for reaching conclusions on the primary outcome parameters. Meta-analyses have been performed to summarize findings; however, these meta-analyses often suffer from various methodological flaws of their own, indicating that the results should be interpreted with caution. Evidence has shown that safety is excellent, which provides leverage for practitioners to recommend shockwave therapy in spite of heterogeneous outcome data. But even though there are very limited side effects, it has to be considered that LIST is an intensive therapy for patients and demands an investment of time from them, with current data suggesting that up to 12 treatment sessions could be necessary [29]. Furthermore, it comes with a price that, according to Rizk et al. [57], could run up to US$400 per treatment and US$4000 for a total regimen, or even US$1000 per treatment. In light of the available evidence, no definitive conclusion can be made on whether shockwave therapy has proven efficacy in terms of achieving a clinically meaningful improvement of EF. We believe that the statement of the EAU that clear and definitive recommendations cannot be given and the statement of the AUA that LIST for ED should be considered investigational, are correct until larger, sufficiently powered, unbiased multicentric RCT are conducted.
References
NIH Consensus Conference. NIH Consensus Conference. Impotence. NIH Consensus Development Panel on Impotence. JAMA. 1993. https://doi.org/10.1001/jama.1993.03510010089036.Text
Braun M, Wassmer G, Klotz T, Reifenrath B, Mathers M, Engelmann U. Epidemiology of erectile dysfunction: results of the ‘Cologne Male Survey’. Int J Impot Res. 2000;12:305–11.
Philippou YA, Jung JH, Steggall MJ, O'Driscoll ST, Bakker CJ, Bodie JA, Dahm P. Penile rehabilitation for postprostatectomy erectile dysfunction. Cochrane Database Syst Rev. 2018;10:CD012414.
Buvat J, Maggi M, Gooren L, Guay AT, Kaufman J, Morgentaler A, Schulman C, et al. Torres LO. Endocrine aspects of male sexual dysfunctions. J Sex Med. 2010;7:1627–56
Jackson G, Montorsi P, Adams MA, Anis T, El-Sakka A, Miner M, et al. Cardiovascular aspects of sexual medicine. 2010;7:1608–26. https://doi.org/10.1111/j.1743-6109.2010.01779.x.
Deveci S, Palese M, Parker M, Guhring P, Mulhall JP. Erectile function profiles in men with Peyronie's disease. J Urol. 2006;175:1807–11
Besiroglu H, Otunctemur A, Ozbek E. The relationship between metabolic syndrome, its components, and erectile dysfunction: a systematic review and a meta-analysis of observational studies. J Sex Med. 2015;12:1309–18. https://doi.org/10.1111/jsm.12885
Shiri R, Koskimäki J, Häkkinen J, et al. Effects of age, comorbidity and lifestyle factors on erectile function: Tampere Ageing Male Urological Study (TAMUS). Eur Urol. 2004;45:628–33. https://doi.org/10.1016/j.eururo.2003.11.020
Sánchez-Cruz JJ, Cabrera-León A, Martín-Morales A, Fernández A, Burgos R, Rejas J. Male erectile dysfunction and health-related quality of life. Eur Urol. 2003;44:245–53. https://doi.org/10.1038/nrd893
Rotella DP. Phosphodiesterase 5 inhibitors: current status and potential applications. Nat Rev Drug Discov. 2002;1:674–82.
Carson CC, Burnett AL, Levine LA, Nehra A. The efficacy of sildenafil citrate (viagra®) in clinical populations: an update. Urology . 2002;60:12–27.
Hatzimouratidis K, Hatzichristou DG. A comparative review of the options for treatment of erectile dysfunction: which treatment for which patient? Drugs. 2005;65:1621–50.
Montorsi F, Verheyden B, Meuleman E, et al. Long-term safety and tolerability of Tadalafil in the treatment of erectile dysfunction. Eur Urol. 2004;45:339–45. https://doi.org/10.1016/j.eururo.2003.11.010
Corona G, Mondaini N, Ungar A, Razzoli E, Rossi A, Fusco F. Phosphodiesterase Type 5 (PDE5) inhibitors in erectile dysfunction: the proper drug for the proper patient. J Sex Med. 2011;8:3418–32. https://doi.org/10.1111/j.1743-6109.2011.02473.x
Hatzimouratidis K, Amar E, Eardley I, et al. Guidelines on male sexual dysfunction: erectile dysfunction and premature ejaculation. Eur Urol. 2010;57:804–14. https://doi.org/10.1016/j.eururo.2010.02.020
Hanson-Divers C, Jackson SE, Lue TF, Crawford SY, Rosen RC. Health outcomes variables important to patients in the treatment of erectile dysfunction. J Urol. 1998;159:1541–7.
Fode M, Hatzichristodoulou G, Serefoglu EC, Verze P, Albersen M. Low-intensity shockwave therapy for erectile dysfunction: Is the evidence strong enough? Nat Rev Urol. 2017;14:593–606. https://doi.org/10.1038/nrurol.2017.119
Vardi Y, Appel B, Jacob G, Massarwi O, Gruenwald I. Can low-intensity extracorporeal shockwave therapy improve erectile function? A 6-month follow-up pilot study in patients with organic erectile dysfunction. Eur Urol. 2010;58:243–8. https://doi.org/10.1016/j.eururo.2010.04.004
Cleveland RO, McAteer JA. Physics of shock-wave lithotripsy. In: Smith’s textbook of endourology Smith's Textbook of Endourology, I&II, 3rd Edition (Arthur D. Smith MD, Gopal H. Badlani MD, Glenn M. Preminger MD, Louis R. Kavoussi MD (eds.)) Blackwell Publishing Ltd, 2012. p. 527–58.
Seidl M, Steinbach P, Wörle K, Hofstädter F. Induction of stress fibres and intercellular gaps in human vascular endothelium by shock-waves. Ultrasonics. 1994;32:397–400. https://doi.org/10.1016/j.eururo.2010.04.004
Apfel R. Acoustic cavitation: a possible consequence of biomedical uses of ultrasound. Br J Cancer Suppl. 1982;5:140–6.
Ciampa AR, De Prati AC, Amelio E, et al. Nitric oxide mediates anti-inflammatory action of extracorporeal shock waves. FEBS Lett. 2005;579:6839–45. https://doi.org/10.1016/j.febslet.2005.11.023
Gotte G, Amelio E, Russo S, Marlinghaus E, Musci G, Suzuki H. Short-time non-enzymatic nitric oxide synthesis from L-arginine and hydrogen peroxide induced by shock waves treatment. FEBS Lett. 2002;520:153–5. https://doi.org/10.1016/S0014-5793(02)02807-7
Gruenwald I, Appel B, Vardi Y. Low-intensity extracorporeal shock wave therapy—a novel effective treatment for erectile dysfunction in severe ED patients who respond poorly to PDE5 inhibitor therapy. J Sex Med. 2012;9:259–64. https://doi.org/10.1111/j.1743-6109.2011.02498.x
Bechara A, Casabé A, De Bonis W, Ciciclia PG. Twelve-month efficacy and safety of low-intensity shockwave therapy for erectile dysfunction in patients who do not respond to phosphodiesterase type 5 inhibitors. Sex Med. 2016;4:e225–e232. https://doi.org/10.1016/j.esxm.2016.06.001
Tsai CC, Wang CJ, Lee YC, et al. Low-intensity extracorporeal shockwave therapy can improve erectile function in patients who failed to respond to phosphodiesterase type 5 inhibitors. Am J Mens Health. 2017;11:1781–90. https://doi.org/10.1177/1557988317721643
Kitrey ND, Gruenwald I, Appel B, Shechter A, Massarwa O, Vardi Y. Penile low intensity shock wave treatment is able to shift PDE5i nonresponders to responders: a double-blind, sham controlled study. J Urol. 2016;195:1550–5. https://doi.org/10.1016/j.juro.2015.12.049
Burnett AL, Nehra A, Breau RH, et al. Erectile dysfunction: AUA guideline. J Urol. 2018;200:633–41. https://doi.org/10.1016/j.juro.2018.05.004
Kalyvianakis D, Memmos E, Mykoniatis I, Kapoteli P, Memmos D, Hatzichristou D. Low-intensity shockwave therapy for erectile dysfunction: a randomized clinical trial comparing 2 treatment protocols and the impact of repeating treatment. J Sex Med. 2018:1–12. https://doi.org/10.1016/j.jsxm.2018.01.003
Reisman Y, Hind A, Varaneckas A, Motil I. Initial experience with linear focused shockwave treatment for erectile dysfunction: a 6-month follow-up pilot study. Int J Impot Res. 2014;27:108–12. https://doi.org/10.1038/ijir.2014.41
Pelayo-Nieto M, Linden-Castro E, Alias-Melgar A, et al. Linear shock wave therapy in the treatment of erectile dysfunction. Actas Urol Esp. 2015;39:456–9. https://doi.org/10.1016/j.acuro.2014.09.010
Hisasue S, China T, Horiuchi A, et al. Impact of aging and comorbidity on the efficacy of low-intensity shock wave therapy for erectile dysfunction. Int J Urol. 2016;23:80–4. https://doi.org/10.1111/iju.12955
Chung E, Cartmill R. Evaluation of clinical efficacy, safety and patient satisfaction rate after low-intensity extracorporeal shockwave therapy for the treatment of male erectile dysfunction: an Australian first open-label single-arm prospective clinical trial. BJU Int. 2015;115(S5):46–9. https://doi.org/10.1111/bju.13035
Ruffo A, Capece M, Prezioso D, et al. Safety and efficacy of low intensity shockwave (LISW) treatment in patients with erectile dysfunction. Int Braz J Urol. 2015;41:967–74. https://doi.org/10.1590/S1677-5538.IBJU.2014.0386
Frey A, Sønksen J, Fode M. Low-intensity extracorporeal shockwave therapy in the treatment of postprostatectomy erectile dysfunction: a pilot study. Scand J Urol. 2016;50:123–7. https://doi.org/10.3109/21681805.2015.1100675
Rosen RC, Allen KR, Ni X, Araujo AB. Minimal clinically important differences in the erectile function domain of the international index of erectile function scale. Eur Urol. 2011;60:1010–6. https://doi.org/10.1016/j.eururo.2011.07.053
Katz JE, Molina ML, Clavijo R, Prakash NS, Ramasamy R. A phase 2 randomized trial to evaluate different dose regimens of low-intensity extracorporeal shockwave therapy for erectile dysfunction: clinical trial update. Eur Urol Focus. 2018;4:336–7. https://doi.org/10.1016/j.euf.2018.07.011
Kitrey ND, Vardi Y, Appel B, et al. Low intensity shock wave treatment for erectile dysfunction—how long does the effect last? J Urol. 2018;200:167–70. https://doi.org/10.1016/j.juro.2018.02.070
Mulhall JP, Carlsson M, Stecher V, Tseng LJ. Predictors of erectile function normalization in men with erectile dysfunction treated with placebo. J Sex Med. 2018;15:866–72. https://doi.org/10.1016/j.jsxm.2018.03.089
de Araujo AC, da Silva FG, Salvi F, Awad MC, da Silva EA, Damião R. The management of erectile dysfunction with placebo only: does it work? J Sex Med. 2009;6. https://www.jsm.jsexmed.org/article/S1743-6095(15)32350-X/fulltext.
Fojecki GL, Tiessen S, Osther PJS. Effect of low-energy linear shockwave therapy on erectile dysfunction—a double-blinded, sham-controlled, randomized clinical trial. J Sex Med. 2016;14:106–12. https://doi.org/10.1016/j.jsxm.2016.11.307
Fojecki GL, Tiessen S, Sloth Osther PJ. Effect of linear low-intensity extracorporeal shockwave therapy for erectile dysfunction-12-month follow-up of a randomized, double-blinded, sham-controlled study. Sex Med. 2018;6:1–7. https://doi.org/10.1016/j.esxm.2017.09.002
Yee C-H, Chan ES, Hou SS-M, Ng C-F. Extracorporeal shockwave therapy in the treatment of erectile dysfunction: a prospective, randomized, double-blinded, placebo controlled study. Int J Urol. 2014;21:1041–5. https://doi.org/10.1111/iju.12506
Olsen AB, Persiani M, Boie S, Hanna M, Lund L. Can low-intensity extracorporeal shockwave therapy improve erectile dysfunction? A prospective, randomized, double-blind, placebo-controlled study. Scand J Urol. 2015;49:329–33. https://doi.org/10.3109/21681805.2014.984326
Motil I, Kubis I, Sramkova T. Treatment of vasculogenic erectile dysfunction with Piezowave 2 device. Application of low intensity shockwaves using novel linear shockwave tissue coverage (LSTC-ED®) technique. A prospective, multicentric, placebo-controlled study. Adv Sex Med. 2016;6:15–8.
Srini VS, Reddy RK, Shultz T, Denes B. Low intensity extracorporeal shockwave therapy for erectile dysfunction: a study in an Indian population. Can J Urol. 2015;22:7614–22.
Yamaçake KGR, Carneiro F, Cury J, Lourenço R, Françolin PC, Piovesan AC, et al. Low-intensity shockwave therapy for erectile dysfunction in kidney transplant recipients. A prospective, randomized, double blinded, sham-controlled study with evaluation by penile Doppler ultrasonography. Int J Impot Res. 2018. https://doi.org/10.1038/s41443-018-0062-2
Vardi Y, Appel B, Kilchevsky A, Gruenwald I. Does low intensity extracorporeal shock wave therapy have a physiological effect on erectile function? Short-term results of a randomized, double-blind, sham controlled study. J Urol. 2012;187:1769–75. https://doi.org/10.1016/j.juro.2011.12.117
Kalyvianakis D, Hatzichristou D. Low-intensity shockwave therapy improves hemodynamic parameters in patients with vasculogenic erectile dysfunction: a triplex ultrasonography-based sham-controlled trial. J Sex Med. 2017;14:891–7. https://doi.org/10.1016/j.jsxm.2017.05.012
Zewin TS, El A, Ahmed A, et al. Efficacy and safety of low-intensity shock wave therapy in penile rehabilitation post nerve-sparing radical cystoprostatectomy: a randomized controlled trial. Int Urol Nephrol. 2018;50:2007–14. https://doi.org/10.1007/s11255-018-1987-6
Lu Z, Lin G, Reed-Maldonado A, Wang C, Lee YC, Lue TF. Low-intensity extracorporeal shock wave treatment improves erectile function: a systematic review and meta-analysis. Eur Urol. 2017;71:223–33. https://doi.org/10.1016/j.eururo.2016.05.050
Man L, Li G. Low-intensity extracorporeal shock wave therapy for erectile dysfunction: a systematic review and meta-analysis. Amsterdam: Elsevier Inc.; 2017.
Clavijo RI, Kohn TP, Kohn JR, Ramasamy R. Effects of low-intensity extracorporeal shockwave therapy on erectile dysfunction: a systematic review and meta-analysis. J Sex Med. 2016;14:27–35. https://doi.org/10.1016/j.jsxm.2016.11.001
Zou Z, Tang L, Liu Z, et al. Short-term efficacy and safety of low-intensity extracorporeal shock wave therapy in erectile dysfunction: a systematic review and meta-analysis. Int Braz J Urol. 2017;43:805–21. https://doi.org/10.1590/s1677-5538.ibju.2016.0245
Angulo J, Arancea B, Heras, et al. Efficacy of low-intensity shock wave therapy for erectile dysfunction: a systematic review and meta-analysis. Actas Urol Esp. 2017;41:479–90.
Feldman R, Denes B, Appel B, Vasan SS, Shultz T, Burnett A. Pd45-10 the safety and efficacy of Li-Eswt in 604 patients for erectile dysfunction: summary of current and evolving evidence. J Urol. 2015;193:e905–e906. https://doi.org/10.1016/j.juro.2015.02.2582
Rizk PJ, Krieger JR, Kohn TP, Pastuszak AW. Low-intensity shockwave therapy for erectile dysfunction. Sex Med Rev. 2018:1–7. https://doi.org/10.1016/j.sxmr.2018.01.002
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Schoofs, E., Fode, M., Capogrosso, P. et al. Current guideline recommendations and analysis of evidence quality on low-intensity shockwave therapy for erectile dysfunction. Int J Impot Res 31, 209–217 (2019). https://doi.org/10.1038/s41443-019-0132-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-019-0132-0
- Springer Nature Limited
This article is cited by
-
Low-intensity extracorporeal shock wave therapy among urologist practitioners: how the opinion of urologists changed between 2016 and 2019
International Journal of Impotence Research (2022)
-
Penile low intensity shock wave treatment for PDE5I refractory erectile dysfunction: a randomized double-blind sham-controlled clinical trial
World Journal of Urology (2021)
-
European association of urology guidelines for sexual and reproductive health 2020: what is new?
International Journal of Impotence Research (2020)
-
Penile prosthesis infection—moving the needle forward: a commentary on risk factors associated with penile prosthesis infection: systematic review and meta-analysis
International Journal of Impotence Research (2020)
-
Low-intensity shockwave therapy (LiST) for erectile dysfunction: a randomized clinical trial assessing the impact of energy flux density (EFD) and frequency of sessions
International Journal of Impotence Research (2020)