Abstract
Alcohol consumption is one of the major modifiable risk factors of hypertension. The aim of the present retrospective study was to assess the clinical impact of obesity on the association between alcohol consumption and the incidence of hypertension. The present study included 5116 male and 6077 female university employees with a median age of 32 (interquartile range 27–39) who underwent annual health checkups between January 2005 and March 2013. Self-reported drinking frequency was recorded at their first checkup and categorized into rarely and 1–3, 4–6, and 7 days/week. During the median observational period of 4.9 years (interquartile range 2.1–8.3), hypertension, defined as systolic/diastolic blood pressure of ≥140/90 mmHg and/or self-reported treatment for hypertension, was observed in 1067 (20.9%) men and 384 (6.3%) women. Poisson regression models adjusted for clinically relevant factors revealed a dose-dependent association between drinking frequency and the incidence of hypertension in men (adjusted incidence rate ratio [95% confidence interval] of men who drank rarely, 1–3, 4–6, and 7 days/week was 1.00 [reference], 1.12 [0.97–1.30], 1.42 [1.19–1.70], and 1.35 [1.14–1.59], respectively; Ptrend < 0.001). However, this association was not observed in women. The dose-dependent association was significant in nonobese men (body mass index (BMI) < 25 kg/m2), but not in obese men (BMI ≥25 kg/m2) (P for interaction between drinking frequency and BMI = 0.072). The present study provides clinically useful evidence to identify the drinkers who may reap the health benefits of abstinence from alcohol consumption.
Similar content being viewed by others
Introduction
Hypertension is one of the leading causes for the global burden of disease [1]. Its deleterious effect is largely mediated through cardiovascular diseases (CVD). In addition to genetic factors, a number of lifestyle factors affect the incidence of hypertension [2, 3]. Along with smoking, obesity, high salt intake, unhealthy diet, and physical inactivity, alcohol consumption is one of the leading factors contributing to hypertension [4,5,6], especially in the Asian population [7]. In Japan, 35% and 3% of cases of hypertension in men and women, respectively, may be attributed to alcohol consumption [8]. A systematic review of 36 randomized controlled trials demonstrated that a reduction in alcohol intake significantly lowered blood pressure [9].
Genetic and clinical characteristics of alcohol drinkers who are vulnerable to hypertension should be elucidated to prevent alcohol-associated hypertension. Besides sex [10], previous studies have suggested that gene polymorphism of key enzymes of alcohol metabolism, alcohol dehydrogenase [11], and aldehyde dehydrogenase [12], modified the association between alcohol consumption and the incidence of hypertension. In contrast to these genetic factors, little information is available regarding modifiable clinical factors that affect the association between alcohol consumption and the incidence of hypertension. Obesity might be a potential predictor of alcohol-associated hypertension, although conflicting results have been reported from a Japanese cohort study (N = 1310) [13] and a Chinese cohort study (N = 2778) [14].
The present retrospective cohort study aimed to assess the clinical impact of obesity on the association between frequency of alcohol consumption and the incidence of hypertension in 11,193 employees in a large national university in Japan. The present study provides clinically useful evidence to identify alcohol drinkers who may reap the health benefits of abstinence from alcohol consumption.
Methods
Participants
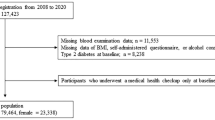
Participants who were enrolled in this study were 16,265 employees of Osaka University who visited Osaka University Health Care Center for annual health checkups between January 2005 and March 2013. Among 16,232 (99.8%) subjects aged 20–65 years, the following subjects were excluded: (i) 1189 (7.3%) subjects with hypertension, defined as systolic blood pressure ≥140 mmHg, diastolic blood pressure ≥90 mmHg, and/or self-reported treatment for hypertension; (ii) 64 (0.4%) subjects with missing baseline data at their first visit during the entry period; and (iii) 3786 (23.3%) subjects with no follow-up visit between their baseline visit and March 2019. Finally, the present study included 11,193 (68.8%) normotensive subjects (5116 men and 6077 women) with at least one follow-up visit. Because of the retrospective nature of the present study, sample size was determined by the number of employees of Osaka University who visited Osaka University Health Care Center for their annual health checkup during the entry period. The study protocol was approved by the ethics committee of Health and Counseling Center, Osaka University and Osaka University Hospital. Informed consent was not obtained from participants, according to the Japanese Ethical Guidelines for Medical and Health Research Involving Human Subjects.
Measurements
The baseline parameters of each participant, including age; sex; drinking frequency; smoking status; body mass index (BMI) (=body weight [kg]/height2 [m2]); systolic and diastolic blood pressure; hemoglobin A1c level; serum concentrations of total cholesterol, triglycerides, and creatinine; dipstick urinary protein of a random spot urine sample; and self-reported treatments for hypertension, diabetes, dyslipidemia, and kidney disease were recorded at the initial visit during the entry period. All participants were told to visit after an overnight fast. Estimated glomerular filtration rate (eGFR) was calculated using a three-variable equation modified for the Japanese: eGFR (mL/min/1.73 m2) = 194 × age (year)−0.287 × serum creatinine (mg/dL)−1.094 (×0.739 for women) [15]. Dipstick urinary protein was categorized as negative, trace, and 1+ or more. Drinking frequency, smoking history, and current treatments for hypertension, diabetes, dyslipidemia, and kidney disease were obtained from self-reported standard questionnaires. Drinking frequency was ascertained by the question “How often do you drink per a week?” with responses of rarely, 1–3 days, 4–6 days, or every day. Smoking status was classified into non-, past-, and current smokers according to the question, “Do you smoke?” with possible answers “I do not smoke”, “I quit smoking”, or “I smoke”. Current treatments for hypertension, diabetes, dyslipidemia, and kidney disease were determined according to a positive answer to the question “Are you under treatment for hypertension, diabetes, hyperlipidemia, or kidney disease?”
The outcome measure of the present study was the incidence of hypertension, defined as systolic blood pressure ≥140 mmHg, diastolic blood pressure ≥90 mmHg, and/or self-reported treatment for hypertension. The observational period was defined as the time from the baseline visit to the incidence of hypertension or to the last visit before March 2019, whichever came first.
To assess the degree to which the baseline drinking frequency reflected the drinking frequency during the follow-up period, answers to the question of drinking frequency closest to 730, 1461, and 2191 days after the baseline visit, with a window period of ±185 days, were retrieved. The data of the drinking frequency were missing after March 2013 because the question of alcohol drinking was changed thereafter.
All data were retrieved from the electronic database in the Health and Counseling Center, Osaka University.
Statistical analyses
Baseline characteristics of 11,193 included subjects and 3786 excluded subjects with no follow-up visit were compared using the unpaired t-test, Wilcoxon rank-sum test, or chi-square test, as appropriate. Baseline characteristics stratified by drinking frequency (rarely, 1–3 days, 4–6 days, 7 days) were compared using ANOVA, the Kruskal–Wallis test, the chi-square test, or Fisher’s exact test, as appropriate. Reproducibility of the baseline drinking frequency 2, 4, and 6 years after the baseline visit was assessed using the weighted Cohen's kappa statistic. Reproducibility with a kappa of <0.00, 0.00–0.20, 0.21–0.40, 0.41–0.60, 0.61–0.80, or 0.81–1.00 was regarded as poor, slight, fair, moderate, substantial, or almost perfect, respectively [16].
Cumulative probabilities of the incidence of hypertension were calculated using the Kaplan–Meier method. The association between drinking frequency and the incidence of hypertension was assessed using the log-rank test for trend and unadjusted and multivariable-adjusted Poisson regression models. The adjusted incidence rate ratio of drinking frequency was calculated after adjusting for age (year), smoking status (non-, past-, vs. current smokers), BMI (kg/m2), systolic blood pressure (mmHg), hemoglobin A1c level (%), serum concentrations of total cholesterol (mg/dL) and triglycerides (Log mg/dL), eGFR (mL/min/1.73 m2), dipstick urinary protein (negative, trace, vs. 1+ or more), and current treatments for diabetes, dyslipidemia, and kidney disease. The appropriateness of Poisson regression models was tested with a goodness-of-fit test using deviance statistics. Robust (Huber–White) sandwich-based standard errors were used to validate inferences for estimates in Poisson regression models. To assess the dose-dependent association between drinking frequency and incidence of hypertension in Poisson regression models, Ptrend for drinking frequency was calculated, including drinking frequency as a continuous independent variable.
Effect modification between drinking frequency and BMI was assessed by incorporating their interaction term into multivariable-adjusted models. A P value of <0.10 for interaction was regarded as statistically significant. To elucidate the interaction between drinking frequency and BMI in men, we first assessed the association between drinking frequency and the incidence of hypertension in three subgroups, with BMI of <22.0, 22.0–24.9, and ≥25.0 kg/m2, separately, and we then calculated incidence rate ratios of 12 categories based on the 4 categories of drinking frequency and the 3 categories of BMI.
Continuous variables are expressed as mean ± standard deviation or median (interquartile range), as appropriate, and categorical variables as number (proportion). Statistical significance was set at P < 0.05, if not specified. Statistical analyses were performed using Stata, version 15.0 (StataCorp LLC, College Station, TX) and R, version 3.6.0 (The R Foundation for Statistical Computing, www.r-project.org).
Results
The baseline characteristics of 11,193 included subjects and 3786 excluded subjects with no follow-up visit are listed in the Supplementary Table. Despite statistically significant differences in age, smoking status, systolic and diastolic blood pressure, and urinary protein, their differences did not reach clinically meaningful levels, suggesting that their baseline characteristics were comparable. The baseline characteristics of 5116 men and 6077 women, stratified by the four categories of drinking frequency, are listed in Tables 1 and 2, respectively. The men who drank more frequently were likely to have older age; current smoker status; a negative result of dipstick urinary protein; higher BMI, systolic blood pressure, and diastolic blood pressure; higher levels of hemoglobin A1c, total cholesterol, and triglycerides; and a lower eGFR than those who rank rarely (P < 0.05). The women who drank more frequently were likely to have older age; current smoker status; a negative result of dipstick urinary protein; higher systolic and diastolic blood pressure; and lower hemoglobin A1c and eGFR than those who drank rarely (P < 0.05).
During the median observational period of 4.9 (interquartile range 2.1–8.3) years, the onset of hypertension was observed in 1067 (20.9%) men (Table 3) and 384 (6.3%) women (Table 4). Subjects with higher drinking frequency were at a higher risk of developing hypertension among both men and women (Ptrend < 0.001 in both men and women) (Fig. 1). Unadjusted Poisson regression models showed significant linear associations in both men and women (Ptrend < 0.001 and 0.001 in men and women, respectively) (Fig. 2a). Even after adjusting for clinically relevant factors, men who drank ≥4 days/week were at significantly higher risk of hypertension in a dose-dependent manner (adjusted incidence rate ratio of men who drank rarely, 1–3, 4–6, and 7 days/week: 1.00 [Reference], 1.12 [0.97–1.30], 1.42 [1.19–1.70], and 1.35 [1.14–1.59], respectively; Ptrend < 0.001). In contrast, no significant linear association was observed in women (adjusted incidence rate ratio of women who drank rarely, 1–3, 4–6, and 7 days/week: 1.00 [Reference], 1.06 [0.84–1.33], 1.09 [0.72–1.65], and 1.29 [0.93–1.77], respectively; Ptrend = 0.140).
Drinking frequency and the incidence of hypertension in 5116 men and 6077 women (a) and in male subgroups stratified by body mass index (b). Overall effect modification between drinking frequency and body mass index in men (c). Incidence rates were calculated using Poisson regression models unadjusted and adjusted for age (years), smoking status (non-, past-, vs. current smoking), body mass index (kg/m2) (in a and b, not c), systolic blood pressure (mmHg), total cholesterol (mg/dL), triglycerides (log mg/dL), hemoglobin A1c (%), estimated glomerular filtration rate (ml/min/1.73 m2), dipstick urinary protein (negative, trace, vs. 1+ or more), and self-reported current treatments for dyslipidemia, diabetes, and kidney disease. The Ptrend for drinking frequency in adjusted models has been described in a and b. The P value for the interaction between drinking frequency and body mass index in adjusted models in a was 0.072 and 0.910 in men and women, respectively
BMI modified the association between drinking frequency and the incidence of hypertension in the adjusted model in men, but not in women (P value for interaction between drinking frequency and BMI = 0.072 and 0.910 in men and women, respectively). To elucidate the male effect modification, 5116 men were categorized into three subgroups stratified by BMI (<22.0, 22.0–24.9, and ≥25.0 kg/m2), in whom the incidence rate of each drinking frequency was calculated (Fig. 2b). A dose-dependent association between drinking frequency and the incidence of hypertension was evident in nonobese men (BMI < 22.0 and 22.0–24.9 kg/m2), even after adjusting for clinically relevant factors (Ptrend = 0.012 and <0.001, respectively), whereas this association was not evident in obese men (BMI of ≥25.0 kg/m2) (Ptrend = 0.178). To clarify any overall effect modification between drinking frequency and BMI, men were classified into 12 categories (4 drinking frequencies × 3 BMIs), and their incidence rate ratios were calculated, regarding rare drinkers with BMI < 22.0 kg/m2 as a reference (Fig. 2c). In an unadjusted model, men with BMI ≥25 kg/m2 were at markedly higher risk of the incidence of hypertension compared with those with BMI < 22.0 kg/m2 and drinking frequency of 4–7 days/week. However, after multivariable adjustment, the incidence rate ratio of men with BMI ≥25 kg/m2 was comparable with the ratio of those with BMI < 22.0 kg/m2 and drinking frequency of 4–7 days/week (rarely, 1–3, 4–6, 7 days/week drinking frequency with BMI < 22.0 kg/m2: 1.00 [reference], 1.34 [1.01–1.78], 1.71 [1.20–2.41], 1.61 [1.21–2.15]; rarely, 1–3, 4–6, 7 days/week drinking frequency with BMI 22.0–24.9 kg/m2: 1.18 [0.2–1.51], 1.29 [1.00–1.68], 1.72 [1.29–2.29], 1.85 [1.41–2.43]; rarely, 1–3, 4–6, 7 days/week drinking frequency with BMI ≥25.0 kg/m2: 1.87 [1.47–2.39], 1.90 [1.45–2.49], 2.30 [1.63–3.25], 1.75 [1.26–2.43]).
To assess whether the baseline drinking frequency reflected the drinking frequency during the observational period, we assessed the reproducibility of drinking frequency 2, 4, and 6 years after the baseline visit (Tables 3 and 4). Among 4034 (78.9%) men who were at risk 2 years after the baseline visit, the data of drinking frequency at 2 years after the baseline visit were available in 2543 (63.0%) men. Their reproducibility of drinking frequency was almost perfect (weighted Cohen's kappa statistics = 0.82). The reproducibility at 4 and 6 years after the baseline visit was substantial (weighted Cohen's kappa statistics = 0.78 and 0.76, respectively), suggesting that the baseline drinking frequency reflected the drinking frequency during the observational period in men. Substantial reproducibility was also observed in women (weighted Cohen's kappa statistics at 2, 4, and 6 years after the baseline visit = 0.74, 0.71, and 0.70, respectively) (Table 4).
Discussion
The present study identified drinking frequency as a predictor of hypertension in men, especially in nonobese men. The results of the current study suggest that a reduction in alcohol consumption might be more effective in nonobese men than obese men. One of the advantages of the present study was a large sample size (5116 men and 6077 women), which enabled statistically meaningful analyses in men and women separately to elucidate a sex-dependent association between drinking frequency and the incidence of hypertension. Other advantages were the inclusion of an Asian population, who are vulnerable to alcohol-induced hypertension [7], and a robust assessment showing the substantial reproducibility of the baseline drinking frequency during the observational period (Tables 3 and 4). The results of the present study might provide clinically useful evidence to establish an effective strategy to prevent the incidence of hypertension, which is one of the major risk factors of CVD.
Conflicting effect modifications between alcohol consumption and obesity have been reported in Asian cohort studies. A Chinese cohort study, the Prevention of Metabolic Syndrome and Multimetabolic disorders in Jiangsu Province of China Study, including 1097 men and 1681 women, showed an additive interaction of current drinking and abdominal obesity (waist ≥90 and 80 cm for men and women, respectively) on the incidence of hypertension [14], suggesting that abdominal obesity might substantially enhance the risk of alcohol-induced hypertension. In contrast, a Japanese cohort study, including 1310 men who were office workers, reported a significant linear association between alcohol consumption and the incidence of hypertension in nonobese men with BMI < 24.2 kg/m2, whereas such an association was not observed in obese men with BMI ≥24.2 kg/m2 [13]. This cohort study suggested that obesity might attenuate the risk of alcohol-induced hypertension in men. The present study, with a larger sample size, confirmed the results of the previous Japanese male cohort study. In contrast to previous studies including only men, the present study found a sex-specific association between alcohol consumption and the incidence of hypertension. However, the results of this study, including 11,193 employees of a national university and 1310 office workers in a company in Japan, should be verified in a larger cohort with higher generalizability.
The mechanism of the smaller impact of alcohol consumption on hypertension in obese men is unknown. The variability in first-pass metabolism of alcohol might affect the effect modification between alcohol consumption and obesity. Several randomized crossover trials have demonstrated that food intake before alcohol consumption significantly decreases the bioavailability of alcohol compared with alcohol consumption on the empty stomach [17, 18]. Thus, excessive food intake in obese men may suppress the detrimental effects of high alcohol consumption. Another potential link between obesity and the bioavailability of alcohol may be delayed gastric emptying, which results in an enhanced first-pass metabolism of alcohol [19]. Several studies have reported that higher BMI is associated with delayed gastric emptying [20, 21], suggesting lower bioavailability of alcohol in obese subjects. After the first-pass metabolism, the distribution volume of alcohol is strongly correlated with total water volume [22]. Thus, obese subjects are more likely to have lower blood alcohol concentrations than nonobese subjects [23]. Many other factors may contribute to the effect modification between alcohol consumption and obesity, which should be elucidated in further studies.
In the present study, in contrast to men, no significant association between frequency of alcohol consumption and the incidence of hypertension was observed in women after adjusting for clinically relevant factors. Several cohort studies have also reported that the association between alcohol consumption and the incidence of hypertension was stronger in men than women [24, 25]. A systematic review including 16 cohort studies (33,904 men and 193,752 women) reported similar results [26]. A smaller number of subjects and no information on daily alcohol consumption (g/day) in the present study might have underestimated the association between alcohol consumption and the incidence of hypertension in women, leading to no significant association between drinking frequency and the incidence of hypertension. Because inflammation and adipocytokines are associated with blood pressure in different manners between men and women [27], the sex difference in the association between alcohol consumption and the incidence of hypertension should be assessed in further studies.
Besides the lack of information on daily alcohol consumption described above, the present study has several limitations. First, self-reported drinking frequency may be biased, especially in obese subjects. Many studies have reported that dietary intake is likely to be underreported in obese subjects [28, 29]. The lack of a linear association between drinking frequency and the incidence of hypertension in obese men might be partly due to biased answers. Some potential biomarkers of chronic alcohol consumption [30] will be helpful in estimating the unbiased association in obese men in a future study. Second, the association between drinking frequency and the incidence of hypertension might be confounded by salt intake, one of the major nutritional determinants of hypertension [31]. A large Japanese cohort study has reported that men with higher salt intake had a higher prevalence of alcohol drinkers [32, 33], suggesting a positive association between alcohol consumption and salt intake. In contrast, no association between salt intake and the prevalence of daily alcohol consumers was observed in women. The sex difference in the present study might be partly due to an effect modification between sex and salt intake with alcohol consumption. Their association should be assessed in a well-designed cohort study. Third, although several cohort studies have shown that wine, beer, and liquor have different effects on the incidence of hypertension [34, 35], the present study had no information on each type of alcoholic beverage. Fourth, information on past drinking was not available in the present study. Sick quitters, the past smokers who quit drinking due to medical problems, might have affected the association between drinking frequency and the incidence of hypertension. Given that these sick quitters are at a higher risk of cardiometabolic diseases, including hypertension, the association between drinking frequency and the incidence of hypertension was biased toward the null hypothesis. If we consider past drinkers, the association between drinking frequency and the incidence of hypertension is probably stronger than that observed in the present study.
In conclusion, the present study identified a higher frequency of alcohol consumption as a significant predictor of incident hypertension in nonobese men but not in obese men, whereas no association between the frequency of alcohol consumption and the incidence of hypertension in women was observed. These results suggest that the reduction of alcohol consumption may be effective in nonobese men for the prevention of hypertension. Its efficacy should be evaluated in well-designed randomized controlled trials.
References
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–60.
Warren HR, Evangelou E, Cabrera CP, Gao H, Ren M, Mifsud B, et al. Genome-wide association analysis identifies novel blood pressure loci and offers biological insights into cardiovascular risk. Nat Genet. 2017;49:403–15.
Lennon SL, DellaValle DM, Rodder SG, Prest M, Sinley RC, Hoy MK, et al. 2015 evidence analysis library evidence-based nutrition practice guideline for the management of hypertension in adults. J Acad Nutr Diet. 2017;117:1445–58.
Kokubo Y. Prevention of hypertension and cardiovascular diseases: a comparison of lifestyle factors in Westerners and East Asians. Hypertension. 2014;63:655–60.
Kawabe H, Azegami T, Takeda A, Kanda T, Saito I, Saruta T, et al. Features of and preventive measures against hypertension in the young. Hypertens Res. 2019;42:935–48.
Iwama N, Metoki H, Nishigori H, Mizuno S, Takahashi F, Tanaka K, et al. Association between alcohol consumption during pregnancy and hypertensive disorders of pregnancy in Japan: the Japan Environment and Children’s Study. Hypertens Res. 2019;42:85–94.
Taylor B, Irving HM, Baliunas D, Roerecke M, Patra J, Mohapatra S, et al. Alcohol and hypertension: gender differences in dose-response relationships determined through systematic review and meta-analysis. Addiction. 2009;104:1981–90.
Nakamura K, Okamura T, Hayakawa T, Hozawa A, Kadowaki T, Murakami Y, et al. The proportion of individuals with alcohol-induced hypertension among total hypertensives in a general Japanese population: NIPPON DATA90. Hypertens Res. 2007;30:663–8.
Roerecke M, Kaczorowski J, Tobe SW, Gmel G, Hasan OSMM, Rehm J. The effect of a reduction in alcohol consumption on blood pressure: a systematic review and meta-analysis. Lancet Public Health. 2017;2:e108–20.
Roerecke M, Tobe SW, Kaczorowski J, Bacon SL, Vafaei A, Hasan OSM, et al. Sex-specific associations between alcohol consumption and incidence of hypertension: a systematic review and meta-analysis of cohort studies. J Am Heart Assoc. 2018;7:e008202.
Sen Zhang W, Xu L, Mary Schooling C, Jiang CQ, Keung Cheng K, Liu B, et al. Effect of alcohol and aldehyde dehydrogenase gene polymorphisms on alcohol-associated hypertension: the Guangzhou Biobank Cohort Study. Hypertens Res. 2013;36:741–6.
Chang YC, Chiu YF, Lee ITe, Ho LT, Hung YJ, Hsiung CA, et al. Common ALDH2 genetic variants predict development of hypertension in the SAPPHIRe prospective cohort: gene-environmental interaction with alcohol consumption. BMC Cardiovasc Disord. 2012;12:58.
Nakanishi N, Yoshida H, Nakamura K, Suzuki K, Tatara K. Alcohol consumption and risk for hypertension in middle-aged Japanese men. J Hypertens. 2001;19:851–5.
Luo W, Guo Z, Hao C, Yao X, Zhou Z, Wu M, et al. Interaction of current alcohol consumption and abdominal obesity on hypertension risk. Physiol Behav. 2013;122:182–6.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Kundel HL, Polansky M. Measurement of observer agreement. Radiology. 2003;228:303–8.
Fraser A, Rosalki S, Gamble G, Pounder R. Inter-individual and intra-individual variability of ethanol concentration-time profiles: comparison of ethanol ingestion before or after an evening meal. Br J Clin Pharm. 1995;40:387–92.
Jones AW, Jönsson KÅ, Kechagias S. Effect of high-fat, high-protein, and high-carbohydrate meals on the pharmacokinetics of a small dose of ethanol. Br J Clin Pharm. 2003;44:521–6.
Oneta CM, Simanowski UA, Martinez M, Allali-Hassani A, Parés X, Homann N, et al. First pass metabolism of ethanol is strikingly influenced by the speed of gastric emptying. Gut. 1998;43:612–9.
Jackson SJ, Leahy FE, McGowan AA, Bluck LJC, Coward WA, Jebb SA. Delayed gastric emptying in the obese: an assessment using the non-invasive 13C-octanoic acid breath test. Diabetes Obes Metab. 2004;6:264–70.
Brogna A, Ferrara R, Bucceri AM, Catalano F, Natoli G, Leocata V. Gastric emptying rates of solid food in relation to body mass index: an ultrasonographic and scintigraphic study. Eur J Radio. 1998;27:258–63.
Norberg A, Jones AW, Hahn RG, Gabrielsson JL. Role of variability in explaining ethanol pharmacokinetics: research and forensic applications. Clin Pharmacokinet. 2003;42:1–31.
Davies BT, Bowen CK. Total body water and peak alcohol concentration: a comparative study of young, middle-age, and older females. Alcohol Clin Exp Res. 1999;23:969–75.
Sesso HD, Cook NR, Buring JE, Manson JE, Gaziano JM. Alcohol consumption and the risk of hypertension in women and men. Hypertension. 2008;51:1080–7.
Okubo Y, Sairenchi T, Irie F, Yamagishi K, Iso H, Watanabe H, et al. Association of alcohol consumption with incident hypertension among middle-aged and older Japanese population. Hypertension. 2014;63:41–7.
Briasoulis A, Agarwal V, Messerli FH. Alcohol consumption and the risk of hypertension in men and women: a systematic review and meta-analysis. J Clin Hypertens. 2012;14:792–8.
Yang Yde, Zheng CJ, Dong Yhui, Zou Zyong, Lv Y, Wang Zhe, et al. Sex difference in the mediation roles of an inflammatory factor (hsCRP) and adipokines on the relationship between adiposity and blood pressure. Hypertens Res. 2019;42:903–11.
Zhang J, Temme EHM, Sasaki S, Kesteloot H. Under- and overreporting of energy intake using urinary cations as biomarkers: Relation to body mass index. Am J Epidemiol. 2000;152:453–62.
Murakami K, Sasaki S, Takahashi Y, Uenishi K, Yamasaki M, Hayabuchi H, et al. Misreporting of dietary energy, protein, potassium and sodium in relation to body mass index in young Japanese women. Eur J Clin Nutr. 2008;62:111–8.
Viel G, Boscolo-Berto R, Cecchetto G, Fais P, Nalesso A, Ferrara SD. Phosphatidylethanol in blood as a marker of chronic alcohol use: a systematic review and meta-analysis. Int J Mol Sci. 2012;13:14788–812.
Wolf M, Ewen S, Mahfoud F, Böhm M. Hypertension: history and development of established and novel treatments. Clin Res Cardiol. 2018;107:16–29.
Tsugane S, Sasazuki S, Kobayashi M, Sasaki S. Salt and salted food intake and subsequent risk of gastric cancer among middle-aged Japanese men and women. Br J Cancer. 2004;90:128–34.
Imaizumi T, Ando M, Nakatochi M, Maruyama S, Yasuda Y, Honda H, et al. Association of interactions between dietary salt consumption and hypertension-susceptibility genetic polymorphisms with blood pressure among Japanese male workers. Clin Exp Nephrol. 2017;21:457–64.
Thadhani R, Camargo CA Jr, Stampfer MJ, Curhan GC, Willett WC, Rimm EB. Prospective study of moderate alcohol consumption and risk of hypertension in young women. Arch Intern Med. 2002;162:569–74.
Núñez-Córdoba JM, Martínez-González MA, Bes-Rastrollo M, Toledo E, Beunza JJ, Alonso A. Alcohol consumption and the incidence of hypertension in a Mediterranean cohort: the SUN study. Rev Esp Cardiol. 2009;62:633–41.
Acknowledgements
We thank Michiko Akashi and all the staff of the Health and Counseling Center, Osaka University, Toyonaka, Japan, for managing the health checkup data in the database.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Grants covering the research: None
Supplementary information
Rights and permissions
About this article
Cite this article
Nishigaki, D., Yamamoto, R., Shinzawa, M. et al. Body mass index modifies the association between frequency of alcohol consumption and incidence of hypertension in men but not in women: a retrospective cohort study. Hypertens Res 43, 322–330 (2020). https://doi.org/10.1038/s41440-019-0382-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-019-0382-8
- Springer Nature Singapore Pte Ltd.
Keywords
This article is cited by
-
Meta-analytic evidence for a sex-diverging association between alcohol use and body mass index
Scientific Reports (2022)
-
Annual reports on hypertension research 2020
Hypertension Research (2022)
-
Evaluation of serum ATX and LPA as potential diagnostic biomarkers in patients with pancreatic cancer
BMC Gastroenterology (2021)
-
Association of sleep-disordered breathing and alcohol consumption with hypertension among Japanese male bus drivers
Hypertension Research (2021)
-
Effect of body mass index on the association between alcohol consumption and the development of chronic kidney disease
Scientific Reports (2021)