Abstract
Aims
To evaluate presenting features of patients with orbital solitary fibrous tumours (SFTs), based on histological phenotype.
Methods
A retrospective case-note review was performed for demographics and presenting features for patients with orbital SFTs. The tumours were classified as “Group IA” hypocellular SFT phenotype, “Group IB” haemangiopericytoma phenotype and low mitotic activity, and high-grade “Group II” haemangiopericytoma phenotype with high mitotic activity.
Results
Sixty-four patients (34 female; 53%) presented at a mean age of 42.2 years (median 38; range 19–82), with Group II patients presenting at an older age (mean 53 years). Median symptom duration was 12 months for Groups IA and IB, compared to 4 months for Group II, the commonest symptoms being proptosis (53%), diplopia (41%), periorbital swelling (31%), and altered vision (19%). Mean LogMAR was 0.17 (median 0.0; range −0.2–4), and 14% had ipsilateral optic neuropathy, with no significant difference between the three groups. Non-axial displacement was noted in 69%, a palpable mass in 45%, and reduced eye movements in 59%; choroidal folds and optic disc swelling were recorded in 12% and 9%. SFTs were mostly extraconal (59%), within the superior and superonasal quadrants (44%), with an average estimated tumour volume of 4.9 ml (median 3.6; range 0.31–14.5 ml).
Conclusion
SFTs may present with impaired visual function (∼15%), fundal abnormalities (a fifth), globe displacement (two-thirds), and reduced ocular motility (over a half). High-grade tumours tend to present more than a decade later, with a shorter duration of symptoms.
Similar content being viewed by others
Introduction
Originally described in the pleura, solitary fibrous tumours (SFTs) are rare spindle cell tumours that can also affect extrapleural tissues, such as the orbit [1,2,3]. Previously thought to be distinct entities, fibrous histiocytoma, haemangiopericytoma and giant cell angiofibroma have been shown (with advances in immunohistochemistry, cytogenetics, and molecular biology) to be a spectrum of morphologically-similar mesenchymal fibroblastic tumours that are now grouped as “SFTs” [1,2,3,4]. Various grading systems have been developed to classify SFTs, based on tumour phenotype or multivariate risk-stratification models [1, 2, 5].
SFTs account for ∼1% of orbital masses [6, 7] and can affect any part of the orbit, conjunctiva, caruncle, eyelids, or lacrimal drainage system [3,4,5, 8,9,10,11,12]. Rarely, the orbit may be secondarily involved by tumours arising in the sinonasal [13] or intracranial [14] spaces, or by distant metastases [15]. The spectrum of orbital SFTs ranges from benign to malignant variants, the vast majority having a relatively “low-grade” and indolent course, although recurrent lesions can be locally aggressive or display malignant behaviour with extraorbital spread [3].
In this study, we compare the clinical characteristics of orbital SFTs, based on three main tumour phenotypes.
Patients and methods
Patients who presented between 1971 and 2022 with a histologically-confirmed diagnosis of SFT were identified from diagnostic orbital and pathological databases.
The tumours were classified based on a phenotypic grading adapted from the World Health Organization Classification of Tumours of the Central Nervous System [2] into: “Group IA” hypocellular SFT phenotype (hypocellular collagenized tumour) with no necrosis, and <5 mitosis/10 high-power fields (HPF), “Group IB” haemangiopericytoma (densely cellular and higher vascular pattern) with no necrosis and <5 mitosis/10 HPF, and “Group II” haemangiopericytoma phenotype, with necrosis and/or >5 mitosis/10 HPF. Group IA and IB tumours were considered “low-grade” SFTs, and Group II tumours as “high-grade”. Immunostaining for STAT6 was applied only to tumours since 2014.
Details of gender, age at presentation, symptoms and their duration, orbital functions, and tumour location were recorded from a retrospective review of clinical and imaging records. The study only included tumours that were histologically confirmed to be “haemangiopericytoma” or “solitary fibrous tumour,” and any other SFT-related spindle cell lesions such as “fibrous histiocytoma” or “giant cell angiofibroma” were excluded. Cases secondarily involving the orbit from the paranasal sinuses or intracranial space were also excluded.
The SFT volume was estimated from three orthogonal dimensions (“A,” “B,” and “C”; in cm) drawn from pathology reports (where excision was in toto) or imaging (CT or MRI); the volume “V” (ml) was presumed to be that of an ellipsoid with “V = 0.524 × A × B × C”.
One-way analysis of variance (ANOVA) or independent two-tail Student’s t tests were applied for continuous variables and the Fisher exact test for discrete variables, with an α-risk of 0.05 being considered clinically significant. The relationship between age at presentation and estimated tumour volume was investigated using linear regression, with Pearson’s correlation coefficient being used to quantify linearity.
The study was approved by the Institutional Review Board (MEH #1089) and adhered to the tenets of the Declaration of Helsinki. The basic data set for this investigation is not available in the public domain.
Results
Sixty-four patients (34 female; 53%) were identified, 27 (42.2%) having Group IA tumours, 28 (48.4%) Group IB and 5 (9.4%) Group II, high-grade tumours. STAT6 immunohistochemistry was carried out in 23 cases (36%), all of which showed strong immunoreactivity. The mean presenting age for each tumour group was 42.8, 43.1 and 53.2 years, respectively (p = 0.23) (Table 1), although the average presenting age for low-grade tumours (Groups IA and IB; 41.7 years) was somewhat lower than that for high-grade, Group II tumours (53.2 years) (p = 0.11) (Table 1).
The average symptom duration was 24.5 months (median 12; range 1–180), with a median duration of 12 months for Groups IA and IB, as compared to 4 months for Group II tumours (Table 1). The commonest symptoms were proptosis (34/64; 53%), diplopia (26/64; 41%), periorbital swelling (20/64; 31%), subjectively palpable lump (15/64; 23%), and altered vision (12/64; 19%) with no statistically significant difference between the 3 groups, although patients with Group II tumours had a somewhat greater rate of subjective globe dystopia (5/6; 83%) but no diplopia (Table 1).
In affected orbits, the mean LogMAR was 0.17 (median 0.0; range −0.2–4), with 13% (8/64) having LogMAR acuity of 0.5 or worse, 12% (6/52) had abnormal Ishihara colour testing, and 14% (9/64) an ipsilateral relative afferent pupillary defect (Table 2).
There was 4.7 mm relative exophthalmos (median 4 mm; range −1–15 mm), a non-axial displacement in 44 (69%), a palpable mass in 29 (45%), and reduced eye movements in 38 (59%) orbits, the latter being found in every patient with Group II tumours. Choroidal folds, optic disc swelling, and disc pallor were noted in 12%, and 9% of patients, respectively (Table 2).
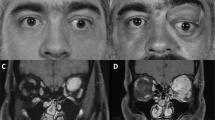
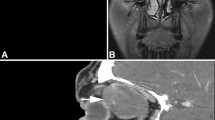
All patients had imaging findings that favoured a diagnosis of SFT, with almost all of them showing avid enhancement on CT or MRI (unlike the patchy and slower enhancement of orbital cavernous venous malformations), and many having flow-voids on MRI due to arterioles within the tumour (or clearly-defined contrast-enhancing vessels on CT) (Fig. 1A–D). SFTs were usually centred on the anterior (22/64; 34%) or mid-orbital spaces (24/64; 38%), with 59% (38/64) being predominantly extraconal and most commonly affecting the superior and nasal quadrants (Table 3). SFTs were centred on the lacrimal gland in 6% (4/64) of cases and the lacrimal sac in 5% (8/64). Pressure remodelling or scalloping of the adjacent orbital bone (typically orbital roof or lamina papyracea) was evident in 50% (29/58) (Table 3 and Fig. 1E, F), and one patient in Group II had bony erosion. Where data was available, the mean estimated tumour volume was 4.9 ml (median 3.6; range 0.3–14.5), with the largest dimension averaging 2.6 cm (median 2.5; range 1.1–3.8 cm) (Table 2). There was a weak positive correlation between age and tumour volume (r = 0.287; p = 0.032) (Fig. 2).
A Non-contrast axial T1-weighted magnetic resonance image (MRI) showing a large right-sided isointense lateral intraconal mass, extending into an expanded superior orbital fissure, with (B) avid post-gadolinium contrast enhancement. C T2-weighted coronal MRI showing flow-void (arrow) within a superior extraconal SFT, and D post-contrast T1-weighted axial image of the same mass, shows enhancement of the lesion that contains a tortuous hypointense flow-void (arrow). E Coronal CT shows a superonasal quadrant SFT with remodelling of the orbital roof. F Axial MRI for a large, avidly enhancing superomedial SFT, with marked smooth deformation of the lamina papyracea.
Discussion
This series describes the presentation of patients with primary orbital SFTs and, as with other reports, there was no gender predilection. Most patients present in the 4th to 6th decades [4, 5, 8, 9], with a peak incidence in the 4th; on average, however, our Group II patients (with high-grade SFTs) presented over a decade later than those with low-grade tumours. The median age of 38 years in our study is very similar to the median of 42 years reported in a recent major review [5], suggesting that many orbital SFTs present earlier than the 5th to 7th decade that is common for those at other anatomical sites. They can, however, affect any age group, with rare cases of haemangiopericytoma being reported in infancy or at birth [16,17,18]
SFTs usually present with slowly progressive symptoms related to a mass effect, depending on the size and anatomical position of the tumour within the orbit. Similar to prior studies [4, 5, 8,9,10], almost half of our patients had subjective “facial asymmetry” or globe displacement, although we found higher rates of diplopia (41%) and impaired vision (19%), compared to a reported 17% prevalence of visual symptoms (blurred vision and diplopia) [5]. Whilst the average 24.5-month duration of symptoms in our study is almost identical to the 23–29.5 months in earlier publications [4, 5], more than half of our patients had symptoms for less than a year, with over one-quarter having symptoms for less than 6 months. The median symptom duration with Group II high-grade tumours was much shorter (4 months vs. 12 months in Groups IA and IB), and these patients also had a higher rate of subjective globe dystopia and altered vision, which probably reflected the more rapid onset of symptoms.
Visual impairment is reported in 10–17% of patients with SFTs [4, 5, 8, 9]. In the current study, impaired visual function due to compressive optic neuropathy (with relative afferent pupillary defect and impaired colour perception) was present in 14%, while choroidal folds due to globe indentation was also noted in 12% of the patients (Table 2). Overall, more than a half of the patients had varying degrees of limited ocular duction, although this was seen in almost all of the Group II patients.
Imaging usually shows SFTs as well-defined, homogenous or heterogenous, and strongly-enhancing ovoid soft-tissue masses, often with vascular flow-voids; the tumour may be located in any part of the orbit and associated with displacement of normal orbital structures or bone remodelling, the latter being noted in half of our cases [1]. Several studies have revealed a predilection for the superior extraconal orbit [8,9,10, 19], whereas another found that the medial orbit was most commonly involved [20]. Compatible with these reports, this study found that most SFTs (59%) were predominantly extraconal, with nearly half of the tumours involving them upper quadrants, and nearly a quarter involving the nasal and inferonasal quadrants.
Unlike other anatomical sites (where SFTs can be very large; >15 cm), those of the head and neck are much smaller (mostly ≤5 cm) and, due to spatial limitations of the orbit, detected much earlier with clinical signs of a mass [21]. A study of 41 orbital SFTs [4] found a median size of 2.2 cm (mean 1.3; range 0.4–5.0), while a major review found a median size of 2.6 cm (mean 2.9; range 0.4–15) [5]. We found similar median dimension of 2.6 cm (mean 2.5; range 1.1–3.8), with a median estimated tumour volume of 3.6 ml (mean 4.9; range 0.31–14.5), and a weakly positive correlation with age (r = 0.287).
In summary, primary orbital SFTs can affect all ages with a peak incidence in the fourth decade and no gender predilection. The presentation varies depending on the size, anatomical position within the orbit, and biological behaviour of the tumour—with high-grade tumours presenting a decade later with shorter symptom duration, and having higher rates of subjective proptosis, change in vision, and reduced ocular motility. SFTs, regardless of histological phenotype, may present with significantly impaired visual functions (about 15%), fundus abnormalities (one-fifth), globe displacement (two-thirds), and reduced ocular motility (over a half).
Summary
What was known before
-
Solitary fibrous tumours (SFTs) are a spectrum of mesenchymal neoplasms that include tumours previously classified as haemangiopericytoma, giant cell angiofibroma, and fibrous histiocytoma.
-
SFTs account for ~1% of orbital masses and can affect any part of the ocular adnexa.
-
Although most cases have a relatively “benign” course, malignant variants have been described, and distant metastasis can rarely occur.
What this study adds
-
About 15% solitary fibrous tumours (SFTs) impair vision, two-thirds displace the globe, and more than a half impair motility.
-
Malignant or “high-grade” SFTs tend to present more than a decade later (median age 52 years vs. 38 years), with a shorter duration of symptoms than “low-grade” forms (median 4 months vs. 12 months).
-
This study found no significant difference between “low-grade” and “high-grade” SFTs in terms of clinical symptoms and signs, orbital location, or tumour size.
Data availability
The basic data set for this investigation is not available in the public domain.
References
Demmico EG, Fritchie KJ, Han A. Solitary fibrous tumours. In: The WHO Classification of Tumours Editorial Board, editor. WHO classification of tumours of soft-tissue and bone. 5th ed. Lyon, France: IARC; 2020. p. 104-8.
Giannini C, Rushing EJ, Hainfellner JA, Bouvier C, Figarella-Branger D, von Deimling A, et al. Solitary fibrous tumour/Haemangiopericytoma. In: Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Ellison DW, Figarella‐Branger D, et al. editors. WHO classification of tumours of the central nervous system. 4th ed. Lyon, France: IARC; 2016. p. 249–54.
René C, Scollo P, O’Donovan D. A review of solitary fibrous tumours of the orbit and ocular adnexa. Eye. 2022. https://doi.org/10.1038/s41433-022-02160-w.
Furusato E, Valenzuela IA, Fanburg-Smith JC, Auerbach A, Furusato B, Cameron JD, et al. Orbital solitary fibrous tumour: encompassing terminology for haemangiopericytoma, giant cell angiofibroma, and fibrous histiocytoma of the orbit: reappraisal of 41 cases. Hum Pathol. 2011;42:120–8.
Thompson LDR, Liou SS, Feldman KA. Orbit solitary fibrous tumour: a proposed risk prediction model based on a case series and comprehensive literature review. Head Neck Pathol. 2021;15:138–52.
Bonavolontà G, Strianese D, Grassi P, Comune C, Tranfa F, Uccello G, et al. An analysis of 2,480 space-occupying lesions of the orbit from 1976 to 2011. Ophthalmic Plast Reconstr Surg. 2013;29:79–86.
Goto H, Yamakawa N, Komatsu H, Asakage M, Tsubota K, Ueda S-I, et al. Clinico-epidemiological analysis of 1000 cases of orbital tumours. Jpn J Ophthalmol. 2021;65:704–23.
Blessing NW, Bermudez-Magner JA, Fernandez MP, Rosenberg AE, Dubovy SR, Johnson TE. Solitary fibrous tumour of the orbit: a case series with clinicopathologic correlation and evaluation of STAT6 as a diagnostic marker. Ophthalmic Plast Reconstr Surg. 2020;36:164–71.
Croxatto JO, Font RL. Haemangiopericytoma of the orbit: a clinicopathologic study of 30 cases. Hum Pathol. 1982;13:210–8.
Sullivan TJ, Wright JE, Wulc AE, Garner A, Moseley I, Sathananthan N. Haemangiopericytoma of the orbit. Aust N Z J Ophthalmol. 1992;20:325–32.
Bonaffini SG, Patel S, Zhou J, Carrasco J. Solitary fibrous tumour of the caruncle: a solitary location. Orbit. 2020;41:250–2.
Vahdani K, Gupta T, Verity DH, Rose GE. Extension of masses involving the lacrimal sac to above the medial canthal tendon. Ophthalmic Plast Reconstr Surg. 2021;37:556–9.
Zeitler D, Kanowitz S, Har-El G. Malignant solitary fibrous tumour of the nasal cavity. Skull Base. 2007;17:239–46.
Ahn JY, Shim JY, Yang WI, Kim TS. Meningeal solitary fibrous tumour as an unusual cause of exophthalmos: case report and review of the literature. Neurosurgery. 2001;48:1362–6.
Patel MM, Jakobiec FA, Zakka FR, Du R, Annino DJ, Borboli-Gerogiannis S, et al. Intraorbital metastasis from solitary fibrous tumour. Ophthalmic Plast Reconstr Surg. 2013;29:e76–9.
Rose AM, Kabiru J, Rose GE. A rare case of orbital haemangiopericytoma arising in childhood. Orbit. 2013;32:384–6.
Arshad AR, Normala B. Infantile malignant haemangiopericytoma of the orbit. Ophthalmic Plast Reconstr Surg. 2008;24:147–8.
Boyle J, Kennedy C, Berry J, Mott MG. Congenital haemangiopericytoma. J R Soc Med. 1985;78:10–12.
Yang BT, Wang YZ, Dong JY, et al. MRI study of solitary fibrous tumour in the orbit. Am J Roentgenol. 2012;199:W506–11.
Alkatan HM, Alsalamah AK, Almizel A, et al. Orbital solitary fibrous tumours: a multi-centered histopathological and immunohistochemical analysis with radiological description. Ann Saudi Med. 2020;40:227–33.
Smith SC, Gooding WE, Elkins M, et al. Solitary fibrous tumours of the head and neck. Am J Surg Pathol. 2017;41:1642–56.
Author information
Authors and Affiliations
Contributions
GER initiated the work and both authors contributed to data acquisition and writing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vahdani, K., Rose, G.E. Presentation of orbital solitary fibrous tumours. Eye 37, 3406–3411 (2023). https://doi.org/10.1038/s41433-023-02519-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02519-7
- Springer Nature Limited