Abstract
Hemoglobin (Hb) and myoglobin (Mb) are heme proteins that capture and transport molecular oxygen (O2) in living organisms. Although mimicking the O2-binding function of Hb and Mb using synthetic iron-porphyrin has been extensively studied for over 40 years, mimicking the function of Hb/Mb in vivo or 100% aqueous solutions has been minimally studied. Hence, a supramolecular complex termed “hemoCD1” was constructed as the aqueous synthetic Hb/Mb model using a 1:1 inclusion complex of 5,10,15,20-tetrakis(4-sulfonatophenyl)porphinatoiron(II) (FeIITPPS) with a per-O-methylated β-cyclodextrin dimer with a pyridine linker (Py3CD). Selective carbon monoxide (CO) depletion in vivo is beneficial for studying the physiological roles of endogenous CO as a gaseous signal messenger. HemoCD1 reversibly binds O2 and CO in aqueous solution at ambient temperature. Hence, hemoCD1 was used as a selective CO scavenger in vivo due to its extremely high binding affinity to CO. In addition, hemoCD1 was utilized to quantify the accumulation of endogenous and exogenous CO in organs/tissues. Finally, hemoCD1 was employed as an antidote for CO poisoning in animals. Thus, recent developments in hemoCD1 have revealed that the aqueous biomimetic heme protein model has significant physiological and therapeutic application potential.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Heme (a protoporphyrin IX iron complex or its analog) is ubiquitous in living systems and an essential cofactor of heme proteins (Fig. 1) [1,2,3,4]. Heme bound to apoproteins forms highly functional heme proteins, such as myoglobin (Mb) in muscles, hemoglobin (Hb) in red blood cells, and cytochrome c oxidase (CcO) in mitochondria, which are primarily essential in the O2-dependent energy conversion process [1, 5,6,7]. However, heme itself (without a protein) is a nonfunctional and harmful molecule because it tends to self-aggregate in vivo owing to its hydrophobic nature and generates reactive oxygen species (ROS) from oxygen (O2) through a Fenton-type reaction [8,9,10,11,12]. Thus, a protein matrix provides appropriate environments for heme to exhibit physiologically important functions in living systems.
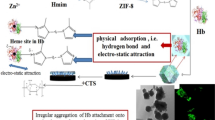
We constructed artificial biomimetic models of heme proteins using a porphyrin/cyclodextrin dimer supramolecular complex (Fig. 2) [13, 14]. A supramolecular 1:1 inclusion complex, hemoCD1, was constructed using 5,10,15,20-tetrakis(4-sulfonatophenyl)porphinatoiron(II) (FeIITPPS) and a per-O-methylated β-cyclodextrin dimer with a pyridine linker (Py3CD). FeIITPPS and Py3CD were utilized as alternatives for the heme molecule and Hb/Mb apoprotein matrix, respectively, and formed a stable supramolecular complex in water. Analogous to Hb and Mb, the iron(II) center of FeIITPPS is encapsulated and isolated by Py3CD from the aqueous bulk phase, which is essential for forming a stable O2 complex in water. Thus, hemoCD1 functions as a synthetic heme protein model in aqueous solution at room temperature [14, 15].
In this focused review, we overview the characteristics of hemoCD1 and its recent development as a unique artificial heme protein model that functions in aqueous biological media. Among the intriguing characteristics of hemoCD1, we focused on highly specific binding to carbon monoxide (CO), which can be utilized for physiological/therapeutic applications in vivo.
Biomimetic chemistry of myoglobin in water
In 1973, Collman et al. reported the first synthetic Mb model, known as “Picket-fence porphyrin,” which reversibly binds O2 in absolute toluene [16, 17]. This compound has four o-pivalamidephenyl groups at the meso-positions of porphyrin, preventing the formation of a μ-oxo dimer of iron(III)porphyrin. Following this discovery, many synthetic metalloporphyrins with bulky meso-substituents have been reported as synthetic Hb/Mb models [5, 18,19,20,21,22,23,24,25]. However, these synthetic models capture O2 in anhydrous (absolute) organic solvents, and fewer models function in aqueous media, whereas native Hb/Mb can bind O2 in water. Furthermore, trace contamination with water must be eliminated from the solution to detect the O2 complexes of the synthetic porphyrins. Therefore, based on the molecular design of the picket-fence porphyrin, it was considered that preventing μ-oxo dimer formation is the key to constructing synthetic Hb/Mb model complexes in homogenous solutions. Nevertheless, few synthetic models can bind O2 stably in aqueous solutions [26,27,28,29]. Stable and reversible O2 complex formation in aqueous media has been realized by synthetic porphyrins embedded into hydrophobic lipid membranes, as demonstrated by Tsuchida, Komatsu, and their coworkers [30,31,32].
Tetrakis(4-sulfonatophenyl)porphyrin (TPPS) forms a very specific 2:1 inclusion complex with 2,3,6-tri-O-methyl-β-cyclodextrins (TMe-β-CD) in aqueous solution (Fig. 3) [33, 34]. The binding constant for the formation of this inclusion complex was estimated to be over 1016 M–2 (=K1K2). Furthermore, Kano et al. reported a significant decrease in the pKa of protonated TPPS when included by TMe-β-CD (ΔpKa = –5.4). This decrease in the pKa indicated that TPPS encapsulation by TMe-β-CD isolated the porphyrin ring to the hydrophobic cavity, thereby preventing protonation of the inner nitrogen of TPPS. Moreover, in 2004, complexation between TMe-β-CD and FeIIITPPS was characterized [35]. Interestingly, anion species such as azide (N3–) strongly bind to the iron(III) center of FeIIITPPS when complexed with TMe-β-CD in aqueous solutions. These anions do not coordinate with FeIIITPPS in the absence of TMe-β-CD because of strong hydration in water. The iron(III) center of the FeIIITPPS/TMe-β-CD inclusion complex was placed in the hydrophobic pocket and thus showed analogous anion-binding ability to native ferric Mb (met-Mb) [36]. Therefore, the FeIIITPPS/TMe-β-CD complex can be regarded as a biomimetic met-Mb model complex in water.
Our group was the first to report an aqueous biomimetic Mb model complex hemoCD1 composed of FeIITPPS and Py3CD (Figs. 2 and 4a) [13]. HemoCD1 reversibly binds O2 in aqueous solution at room temperature because of the tight encapsulation of FeIITPPS in the hydrophobic pocket of Py3CD. The O2 adduct of hemoCD1 (oxy-hemoCD1) formed in aqueous solution readily converted to its deoxy and CO-adduct (CO-hemoCD1) when the atmosphere of the solution was changed (Fig. 4b). The resonance Raman spectrum for oxy-hemoCD1 in water at room temperature showed the FeII–O2 bond stretching band at 569 cm−1, which is almost the same as that of the O2 complex of native Mb (horse hart Mb; 571 cm−1) [13, 37], indicating the formation of an O2-FeII complex similar to the native heme-O2 complex in Mb in water. Oxy-hemoCD1 gradually autoxidized to its iron(III) met-form (met-hemoCD1) with a half-life of 30 h in the pH 6–10 region at room temperature (Fig. 4c) [14]. Thus, hemoCD1 can be used as an artificial O2-carrying molecule at neutral pH in vivo.
a Molecular oxygen (O2) and carbon monoxide (CO) binding and autoxidation of hemoCD1. b UV-vis spectra of deoxy-, oxy-, and CO-hemoCD1 in phosphate buffer at pH 7 and 25 °C. c The pH-rate profile for the autoxidation of oxy-hemoCD1 at 25 °C. Reproduced from ref. [15] with permission. Copyright (2006) American Chemical Society
Selective removal of CO in vivo
The injection of hemoCD1 into animals was first tested in rats [38]. This experiment was initiated to employ hemoCD1 as an alternative to Hb, which is a synthetic O2 carrier in blood; however, hemoCD1 acted as a selective CO scavenger in vivo. After intravenous injection of hemoCD1 into the vein of a rat, it was excreted in the urine within an hour. The excreted hemoCD1 contained the CO complex CO-hemoCD1 (Fig. 5a). Because the animals were not exposed to CO, the CO excreted with hemoCD1 must originate from an endogenous biological source. CO is endogenously produced in mammals during heme metabolic reactions catalyzed by heme oxygenase (HO) enzymes [2,3,4, 9,10,11,12]. Because the CO-binding affinity of hemoCD1 is much higher than that of Mb, Hb, and other heme proteins in living systems [15, 39], the injected hemoCD1 quantitatively eliminated endogenous CO from these heme proteins. Thus, the injection of hemoCD1 produced an endogenous CO-depleted state in the animals.
a Selective removal of endogenous carbon monoxide (CO) from the animal body by injecting oxy-hemoCD1. b Induction of heme oxygenase-1 mRNA (Hmox-1) upon injecting oxy-hemoCD1. Phosphate-buffered saline (PBS) and the iron-free complex (Fb-hemoCD1) were utilized as controls. Reproduced from ref. [49] with permission. Copyright (2016) American Chemical Society
CO is generally known as a toxic gas generated by incomplete combustion during fire accidents. However, CO produced endogenously is an important signaling gas molecule that exerts various physiological functions, such as anti-inflammatory, antiapoptotic, and antiproliferative effects [3, 40,41,42]. In addition, CO is regarded as a medical gas [43,44,45]. Recently, CO-releasing molecules (CORMs) have been used as therapeutic agents that can deliver appropriate amounts of CO into the body [45,46,47,48]. Moreover, the physiological functions of CO have been extensively studied using CORMs [46,47,48]. Nevertheless, there is no approach to selectively deplete endogenous CO; therefore, the removal of CO by hemoCD1 can contribute to the study of the biological function of endogenous CO in vivo.
When oxy-hemoCD1 was intraperitoneally injected into mice, a marked reduction in CO-Hb levels in blood from 0.2% to 0.02% was observed [49, 50]. Interestingly, the CO-Hb level quickly recovered to the normal level within 30 min after the excretion of endogenous CO by hemoCD1, indicating that the feedback system responded to maintain CO homeostasis. Consistently, the removal of endogenous CO by oxy-hemoCD1 significantly induced heme oxygenase-1 (HO-1) expression in the murine liver (Fig. 5b). Overexpressed HO-1 can produce additional endogenous CO via heme degradation, compensating for the temporary CO depletion caused by oxy-hemoCD1 injection. This is the first example that reveals feedback regulation for maintaining the homeostasis of endogenous CO in mammals, which was first revealed by a synthetic biomimetic heme protein model compound.
Some genes exhibit rhythmic expression in an approximately 24 h cycle in living systems, known as the “circadian clock.” Several transcription factors regulate the circadian clock. Among them, circadian locomotor output cycles kaput (CLOCK) and neuronal PAS domain protein 2 (NPAS2) are the main transcription factors, containing heme proteins that bind CO in its heme cofactor [3, 4, 51,52,53]. Therefore, endogenous CO has been considered to play a role in circadian clock regulation [53,54,55,56]. HemoCD1 was used to remove endogenous CO to show CO involvement in the circadian clock system, and the effect of CO depletion on clock genes was investigated [57]. A temporal decrease in endogenous CO by oxy-hemoCD1 injection in mice showed marked disruption of the main clock genes (Per1, Per2, Cry1, and Cry2). The disruption lasted over 19 h and subsequently returned to normal rhythmic expression. This disruption was ascribed to changes in the transcriptional activity of CLOCK and NPAS2. In addition, inflammation caused by a decrease in endogenous CO is also involved in circadian clock disruption. These findings support the hypothesis that endogenous CO participates in circadian clock regulation in the mammalian body.
HemoCD1 was conjugated with octaarginine (R8) as a cell-penetrating peptide to capture CO inside the cells (Fig. 6) [58]. Maleimide-modified hemoCD1 (mal-hemoCD1) was conjugated with Cys-R8 peptide through a 1,4-Michael addition reaction in water. The resulting compound (R8-hemoCD1) was internalized into living cells, resulting in selective depletion of CO in the cells. Furthermore, the removal of endogenous CO in the cells significantly increased intracellular ROS levels, suggesting a relationship between endogenous CO levels and inflammation caused by ROS, although a detailed mechanistic study has not yet been performed.
Selective removal of endogenous CO was achieved in vivo using hemoCD1, contributing to the elucidation of the unknown physiological roles of CO in living systems. This “pseudoknockdown” approach using synthetic compounds is a novel concept researching the roles of biologically related small molecules. Thus, highly specific molecular recognition in vivo by synthetic models will be in high demand to further determine regulatory mechanisms involving small molecules in living systems.
Therapeutic approaches to CO poisoning
It is generally believed that exogenously inhaled CO prevents the O2 transportation of Hb in red blood cells. However, this finding may be controversial. In a study published in 1975 [59], a CO poisoning animal model using dogs was reported. When dogs were exposed to 13% CO gas for 15 min, they died within an hour. In contrast, they survived when CO-Hb-saturated blood was transfused into healthy recipient dogs. In both cases, the CO-Hb levels reached 60–70%. Moreover, only CO gas exerted significant toxicity, whereas CO-Hb did not show any toxic effect. Therefore, the diffusion of gaseous CO to organs/tissues might be the direct cause of lethal toxicity. Hence, it is essential to determine the distribution of gaseous CO into organs/tissues in the body to understand the true mechanism of CO poisoning.
As mentioned above, hemoCD1 showed the highest CO-binding affinity among the reported CO-binding heme proteins. Therefore, hemoCD1 can remove CO from other heme proteins present in organs/tissues. Moreover, the amount of CO can be quantified using hemoCD1 [39, 58]. The protocol for CO quantification in the tissues using hemoCD1 is shown in Fig. 7. The hemoCD1 solution was mixed with the tissue sample and homogenized by sonication. A clear filtrate was obtained after removing the insoluble materials by centrifugation and filtration. Excess Na2S2O4 acted as a reducing agent for hemoCD1 and a precipitant for soluble proteins. Therefore, only the absorbance owing to hemoCD1 was detected, and the amount of endogenous CO was determined simply based on the Lambert–Beer law [39]. The amount of CO in animal tissues was previously determined using gas chromatography (GC) [60, 61]. Comparing the amount of CO determined by GC to that determined by hemoCD1 showed that more CO was detected by hemoCD1, indicating that the assay using hemoCD1 was more sensitive than GC. Thus, the assay using hemoCD1 could become a powerful and convenient tool for sensitive CO quantification in animal tissues and organs, thereby contributing to the elucidation of the CO poisoning mechanism.
a Experimental procedure describing the various steps in the hemoCD1 assay for measuring carbon monoxide (CO) in tissue samples. b Typical spectra for supernatant solutions of the liver sample and control obtained at the end of the hemoCD1 assay. c Amounts of CO quantified in liver tissue without (–) or following flushing with 25–200 mL saline. Adapted from ref. [39] with permission
CO diffused into the blood and tissues of the rats exposed to CO gas. The amount of CO in tissues before and after CO exposure was quantified by the assay using hemoCD1, revealing that CO contained in the tissues first significantly increased and then reached a plateau. After ventilation by air or O2, the amount of CO in the tissues decreased; however, a significant amount of CO was detected in the tissues, and it was difficult to remove it by ventilation in the brain tissues alone. Thus, the residual CO in the brain quantified by the assay using hemoCD1 could cause sequelae after CO poisoning.
Finally, we tested hemoCD1 as an antidote for CO poisoning (Fig. 8a) [39]. After exposure to 400 ppm CO gas for 5 min, oxy-hemoCD1 solution (3.5 mM, 1.0 mL) was intravenously injected into the rats during O2 ventilation. The increased CO-Hb levels (60%) in the rats returned to normal more rapidly in the hemoCD1-injected rats, with excretion of CO in the urine as CO-hemoCD1. Residual CO in the brain tissue was considered the cause of serious sequelae after CO poisoning [62, 63]. After CO exposure, a significant amount of CO accumulated in the brain tissue of the rat and was present even after 30 min of O2 ventilation (Fig. 8b). In contrast, the amount of residual CO in the brain decreased markedly in hemoCD1-injected rats (Fig. 8b). Thus, this finding suggests that hemoCD1 can be used as an effective antidote to reduce CO in blood and brain tissues, although the removal mechanism of CO in brain tissues needs to be further investigated. Nevertheless, the development of a novel antidote to CO poisoning based on hemoCD1 is currently in progress in our laboratory.
a Experimental procedure for the test of hemoCD1 as an antidote for carbon monoxide (CO, 400 ppm)-exposed animal models. b Changes in CO levels detected in the cerebrum samples before (0 min) and after CO exposure without (–) and with hemoCD1 injection (+). Adapted from ref. [39] with permission
Conclusion and outlook
This review focuses on the synthesis and recent development of our biomimetic Hb/Mb model complex hemoCD1. HemoCD1 is continuously synthesized in our laboratory using FeII/IIITPPS and Py3CD for several biomedical applications. HemoCD1 is used for the following purposes: (1) selective removal of endogenous CO in vivo to study endogenous CO as a gaseous signal mediator, (2) quantification of endogenous/exogenous CO accumulated in organs/tissues to study the CO biodistribution, and (3) the creation of an injectable antidote for CO poisoning, which frequently occurs in fire accidents.
References
Reedy CJ, Gibney BR. Heme protein assemblies. Chem Rev. 2004;104:617–49.
Kühl T, Imhof D. Regulatory FeII/III heme: the reconstruction of a molecule’s biography. Chembiochem. 2014;15:2024–35.
Shimizu T, Huang D, Yan F, Stranava M, Bartosova M, Fojtíková V, et al. Gaseous O2, NO, and CO in signal transduction: structure and function relationships of heme-based gas sensors and heme-redox sensors. Chem Rev. 2015;115:6491–533.
Shimizu T, Lengalova A, Martínek V, Martínková M. Heme: emergent roles of heme in signal transduction, functional regulation and as catalytic centres. Chem Soc Rev. 2019;48:5624–57.
Collman JP, Boulatov R, Sunderland CJ, Fu L. Functional analogues of cytochrome c oxidase, myoglobin, and hemoglobin. Chem Rev. 2004;104:561–88.
Huang X, Groves JT. Oxygen activation and radical transformations in heme proteins and metalloporphyrins. Chem Rev. 2018;118:2491–553.
Adam SM, Wijeratne GB, Rogler PJ, Diaz DE, Quist DA, Liu JJ, et al. Synthetic Fe/Cu complexes: toward understanding heme-copper oxidase structure and function. Chem Rev. 2018;118:10840–1022.
Wagener FADTG, Eggert A, Boerman OC, Oyen WJG, Verhofstad A, Abraham NG, et al. Heme is a potent inducer of inflammation in mice and is counteracted by heme oxygenase. Blood. 2001;98:1802–11.
Balla J, Vercellotti GM, Jeney V, Yachie A, Varga Z, Eaton JW, et al. Heme, heme oxygenase and ferritin in vasculae endothelial cell injury. Mol Nutr Food Res. 2005;49:1030–43.
Kumar S, Bandyopadhyay U. Free heme toxicity and its detoxification systems in human. Toxicol Lett. 2005;157:175–88.
Gozzelino R, Jeney V, Soares MP. Mechanisms of cell protection by heme oxygenase-1. Annu Rev Pharm Toxicol. 2010;50:323–54.
Roumenina LT, Rayes J, Lacroix-Desmazes S, Dimitrov JD. Heme: modulator of plasma systems in hemolytic diseases. Trends Mol Med. 2016;22:200–13.
Kitagishi H, Kano K. Synthetic heme protein models that function in aqueous solution. Chem Commun. 2021;57:148–73.
Kano K, Kitagishi H, Kodera M, Hirota S. Dioxygen binding to a simple myoglobin model in aqueous solution. Angew Chem Int Ed. 2005;44:435–8.
Kano K, Kitagishi H, Dagallier C, Kodera M, Matsuo T, Hayashi T, et al. Iron porphyrin-cyclodextrin supramolecular complex as a functional model of myoglobin in aqueous solution. Inorg Chem. 2006;45:4448–60.
Collman JP, Gagne RR, Halbert TR, Marchon JC, Reed CA. Reversible oxygen adduct formation in ferrous complexes derived from a picket fence porphyrin. A model for oxymyoglobin. J Am Chem Soc. 1973;9:7868–70.
Collman JP, Gagne RR, Reed CA, Robinson WT, Rodley GA. Structure of an iron(II) dioxygen complex; a model for oxygen carrying hemeproteins. Proc Natl Acad Sci USA. 1974;71:1326–9.
Collman JP. Synthetic models for the oxygen-binding hemoproteins. Acc Chem Res. 1977;10:265–72.
Collman JP, Fu L. Synthetic models for hemoglobin and myoglobin. Acc Chem Res. 1999;32:455–63.
Jameson GB, Ibers JA. Biological and synthetic dioxygen carriers. In: Bertini I, Gray HB, Lippard SJ, Valentine JS, editors. Bioinorganic chemistry. Mill Valley, CA: University Science Books; 1994. p. 167–251.
Momenteau M, Reed CA. Synthetic heme dioxygen complexes. Chem Rev. 1994;94:659–98.
Rose E, Lecas A, Quelquejeu M, Kossanyi A, Boitrel B. Synthesis of biomimetic heme precursors. Coord Chem Rev. 1998;180:1407–31.
Lombardi A, Nastri F, Pavone V. Peptide-based heme-protein models. Chem Rev. 2001;101:3165–89.
Boitrel B, Le, Gac S. Stabilization of synthetic heme-superoxo complexes by hydrogen bonding: a still on-going quest. N J Chem. 2018;42:7516–21.
Zaragoza JPT, Goldberg DP. Dioxygen binding and activation mediated by transition metal porphyrinoid complexes. In: Ikeda-Saito M, Raven E, editors. Dioxygen-dependent heme enzymes. Cambridge, UK: The Royal Society of Chemistry; 2018. p. 1–36.
Jiang D-J, Aida T. A dendritic iron porphyrin as a novel haemoprotein mimic: effects of the dendrimer cage on dioxygen-binding activity. Chem Commun. 1996;1523;1523–4.
Komatsu T, Hayakawa S, Tsuchida E, Nishide H. meso-Tetrakis[o-(N-methyl)pyridinium]porphyrin ensembles with axially coordinated cyclodextrin-penetrating phenethylimidazole: reversible dioxygen-binding in aqueous DMF solution. Chem Commun. 2003;50–1.
Collman JP, Fu L, Zingg A, Diederich F. Dioxygen and carbon monoxide binding in dendritic iron(ii)porphyrins. Chem Commun. 1997;193–4.
Zingg A, Felber B, Gramlich V, Fu L, Collman JP, Diederich F. Dendritic iron(II) porphyrins as models for hemoglobin and myoglobin: specific stabilization of O2 complexes in dendrimers with H-bond-donor centers. Helv Chim Acta. 2002;85:333–50.
Tsuchida E, Komatsu T, Arai K, Yamada K, Nishide H, Furhop J. Self-assembled lipidporphyrin bilayer vesicles. Microstructure and dioxygen binding in aqueous medium. Langmuir. 1995;11:1877–84.
Komatsu T, Yanagimoto T, Furubayashi Y, Wu J, Tsuchida E. Self-assembled fibers made of lipidporphyrinato–zinc(II) and –iron(II) complexes with an intramolecular coordinated axial imidazole. Langmuir. 1999;15:4427–33.
Tsuchida E, Komatsu T, Arai K, Yamada K, Nishide H, Böttecher C, et al. Monolayered octopus-porphyrin vesicle: microstructure and oxygen-binding in aqueous medium. J Chem Soc Chem Commun. 1995:10634.
Kano K, Tanaka N, Minamizono H, Kawakita Y. Tetraarylporphyrins as probes for studying mechanism of inclusion-complex formation of cyclodextrins. Effect of microscopic environment on inclusion of ionic guests. Chem Lett. 1996;925–6.
Kano K, Nishiyabu R, Asada T, Kuroda Y. Static and dynamic behavior of 2:1 inclusion complexes of cyclodextrins and charged porphyrins in aqueous organic media. J Am Chem Soc. 2002;124:9937–44.
Kano K, Kitagishi H, Tamara S, Yamada A. Anion binding to a ferric porphyrin complexed with per-O-methylated β-cyclodextrin in aqueous solution. J Am Chem Soc. 2004;126:15202–10.
De Rosa MC, Bertonati C, Giardina B, Di Stasio E, Brancaccio A. The effect of anions on azide binding to myoglobin: an unusual functional modulation. Biochim Biophys Acta. 2002;1594:341–52.
Hirota S, Ogura T, Appelman EH, Shinzawa-Itoh K, Yoshikawa S, Kitagawa T. Observation of a new oxygen-isotope-sensitive Raman band for oxyhemoproteins and its implications in heme pocket structures. J Am Chem Soc. 1994;116:10564–70.
Kitagishi H, Negi S, Kiriyama A, Honbo A, Sugiura Y, Kawaguchi AT, et al. A diatomic molecule receptor that removes CO in a living organism. Angew Chem Int Ed. 2010;49:1312–5.
Mao Q, Kawaguchi AT, Mizobata S, Motterlini R, Foresti R, Kitagishi H. Sensitive quantification of carbon monoxide in vivo reveals a protective role of circulating hemoglobin in CO intoxication. Commun Biol. 2021;4:425.
Ryter SW, Otterbein LE. Carbon monoxide in biology and medicine. Biossays. 2004;26:270–80.
Ryter SW, Alam J, Choi AMK. Haem oxygenase-1/carbon monoxide: from basic science to therapeutic applications. Physiol Rev. 2006;86:583–650.
Wu L, Wang R. Carbon monoxide: endogenous production, physiological functions, and pharmacological applications. Pharm Rev. 2005;57:585–630.
Mustafa AK, Gadalla MM, Snyder SH. Signaling by gasotransmitters. Sci Signal. 2009;2:re2.
Fukuto JM, Carrington SJ, Tantillo DJ, Harrison JG, Ignarro LJ, Freeman BA, et al. Small molecule signaling agents: the integrated chemistry and biochemistry of nitrogen oxides, oxides of carbon, dioxygen, hydrogen sulfide, and their derived species. Chem Res Toxicol. 2012;25:769–93.
Mann BE, Motterlini R, Foresti R. CO and NO in medicine. Chem Commun. 2007;4197–208.
Motterlini R, Otterbein LE. The therapeutic potential of carbon monoxide. Nat Rev Drug Disco. 2010;9:728–43.
Motterlini R, Foresti R. Biological signaling by carbon monoxide and carbon monoxide-releasing molecules. Am J Physiol Cell Physiol. 2017;312:C302.
Ling K, Men F, Wang W-C, Zhou Y-Q, Zhang H-W, Ye D-W. Carbon monoxide and its controlled release: therapeutic application, detection, and development of carbon monoxide releasing molecules (CORMs). J Med Chem. 2018;61:2611–35.
Kitagishi H, Minegishi S, Yumura A, Negi S, Taketani S, Amagase Y, et al. Feedback response to selective depletion of endogenous carbon monoxide in the blood. J Am Chem Soc. 2016;138:5417–25.
Kitagishi H, Minegishi S. Iron(II)porphyrin–cyclodextrin supramolecular complex as a carbon monoxide-depleting agent in living organisms. Chem Pharm Bull. 2017;65:336–40.
Freeman SL, Kwon H, Portolano N, Parkin G, Venkatraman Girija U, Basran J, et al. Heme binding to human CLOCK affects interactions with the E-box. Proc Natl Acad Sci USA. 2019;116:19911–6.
Dioum EM, Rutter J, Tuckerman JR, Gonzalez G, Gilles-Gonzalez M-A, McKnight SL. NPAS2: a gas-responsive transcription factor. Science. 2003;298:2385–7.
Lukat-Rodgers GS, Correia C, Botuyan MV, Mer G, Rodgers KR. Heme-based sensing by the mammalian circadian protein CLOCK. Inorg Chem. 2010;49:6349–65.
Klemz R, Reischl S, Wallach T, Witte N, Jürchott K, Klemz S, et al. Reciprocal regulation of carbon monoxide metabolism and the circadian clock. Nat Struct Mol Biol. 2017;24:15–22.
Bass J, Lazar MA. Circadian time signatures of fitness and disease. Science. 2016;354:994–9.
Boehning D, Snyder SH. Carbon monoxide and clocks. Science. 2002;298:2339–40.
Minegishi S, Sagami I, Negi S, Kano K, Kitagishi H. Circadian clock disruption by selective removal of endogenous carbon monoxide. Sci Rep. 2018;8:11996.
Minegishi S, Yumura A, Miyoshi H, Negi S, Taketani S, Motterlini R, et al. Detection and removal of endogenous carbon monoxide by selective and cell-permeable hemoprotein-model complexes. J Am Chem Soc. 2017;139:5984–91.
Goldbaum LR, Ramirez RG, Absalon KB. What is the mechanism of carbon monoxide toxicity? Aviat Space Environ Med. 1975;46:1289–91.
Vreman HJ, Wong RJ, Kadotani T, Stevenson TK. Determination of carbon monoxide (CO) in rodent tissue: effect of heme administration and environmental CO exposure. Anal Biochem. 2005;341:280–9.
Chaves-Ferreira M, Albuquerque IS, Matak-Vinkovic D, Coelho AC, Carvalho SM, Saraiva LM, et al. Release from RuII(CO)2–protein complexes in aqueous solution, cells, and mice. Angew Chem Int Ed. 2015;54:1172–5.
Brown SD, Piantadosi CA. In vivo binding of carbon monoxide to cytochrome c oxidase in rat brain. J Appl Physiol. 1985;68:604–10.
Piantadosi CA, Zhang J, Levin ED, Folz RJ, Schmechel DE. Apoptosis and delayed neuronal damage after carbon monoxide poisoning in the rat. Exp Neurol. 1997;147:103–14.
Acknowledgements
This work was financially supported by JSPS KAKENHI Grant Numbers 20H02871, 20H04540, 19K22972, and 18KK0156, the MEXT-Supported Program for the Strategic Research Foundation at Private Universities (2015–2019), the Takeda Science Foundation, the NOVARTIS Foundation (Japan) for the Promotion of Science, the Suntory Foundation for Life Sciences, and the JGC-S Scholarship Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kitagishi, H., Mao, Q. Capture of carbon monoxide using a heme protein model: from biomimetic chemistry of heme proteins to physiological and therapeutic applications. Polym J 54, 465–472 (2022). https://doi.org/10.1038/s41428-021-00591-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41428-021-00591-y
- Springer Nature Limited
This article is cited by
-
Special issue: Fundamentals and applications of carbohydrate polymers
Polymer Journal (2022)