Abstract
Background
Single-agent PD-1/PD-L1 inhibitors have shown limited efficacy in unselected mCRPC. The evidence of a survival benefit with sipuleucel-T and ipilimumab, provides a rationale to study further increasing immunogenicity in mCRPC through combinations.
Methods
Safety and efficacy avelumab plus carboplatin was investigated in a single-arm Phase Ib study in mCRPC, progressing to at least one taxane and one androgen-receptor inhibitor. The primary endpoint was safety. Secondary endpoints included PSA/radiographic responses, progression-free survival (PFS) and overall survival (OS). Germline/somatic mutation analysis was performed.
Results
In total, 26 patients were included. Patients were heavily pretreated: 76.9% received ≥3 and 42.3% ≥4 prior lines. A DNA damage repair (DDR) alteration was found in three patients (11.5%). The safety profile was acceptable with 73% Grade 3–4 treatment-related adverse events. PSA response rate ≥50% was seen in 7.7% of patients. The objective response rate was 17.6%, including one complete response (5.9%). Two of these responders had a known DDR alteration (one BRCA2, one ATM). The median response duration was 6 months. Median radiographic PFS was 6.6 months (95% CI 4.28–9.01), and median OS 10.6 months (95% CI 6.68–NR).
Conclusions
Avelumab plus carboplatin has an acceptable safety profile and was associated with a prolonged OS given the heavily pretreated population.
Similar content being viewed by others
Introduction
Prostate cancer (PC) is the most common cancer in men and the third most frequent cause of death from cancer in males [1]. Androgen-deprivation therapy with luteinizing hormone-releasing hormone analogues in combination with docetaxel chemotherapy or an androgen-receptor signalling inhibitor (ARSI) is the current standard of care for first-line treatment in patients with metastatic hormone-sensitive PC [2,3,4,5]. However, despite an initial response, most patients will ultimately experience disease progression after a median time of 20–33 months, developing metastatic castration-resistant prostate cancer (mCRPC) [2,3,4,5]. Several drugs, including two taxane chemotherapy agents [6,7,8], two ARSIs [9,10,11,12], an alpha-particle emitter [13] and a PSMA-guided beta-particle emitter [14] are approved for the treatment in this setting after showing improved survival in randomised clinical trials. However, invariably all patients will experience disease progression to these agents leading ultimately to limited survival.
In the last decade, cancer treatment has been revolutionised with the advent of immune-checkpoint inhibitors (ICI), namely thanks to agents targeting the programmed cell death-1 (PD-1) receptor pathway and its ligand PD-L1 and the cytotoxic T lymphocyte-associated protein-4 (CTLA-4) receptor. Several of these agents have been approved for the treatment of different solid tumours. However, their role in PC is still limited with initial data being not encouraging. Clinical trials testing the use of single-agent PD-1 or PD-L1 inhibitors for the treatment of advanced PC have shown very limited signs of efficacy with objective PSA response rates ranging between 8 and 9% and median progression-free survival (PFS) between 2.1 and 3.5 months [15,16,17]. This is probably partially due to the fact that PC has classically been classified as an immunologically cold tumour with a low PD-L1 expression, low tumour mutational burden (TMB) and an increase in immune-suppressive immune cells (such as tumour-associated macrophages, myeloid-derived suppressor cells) [18]. Select PC harbouring microsatellite instability (MSI), high TMB or specific genomic alterations such as mutations in DNA damage repair (DDR) genes or CDK12 loss may be associated with an increased immunotherapy response. Nonetheless, the evidence of a survival benefit seen with the cancer vaccine Sipuleucel-T [19] or the CTLA-4 inhibitor ipilimumab in combination with radiotherapy (final long-term analysis of CA184-043 Phase 3 trial) [20] in advanced PC patients provides a strong rationale supporting further research with the use of modern ICI in improved strategies, such as drug combinations directed to increase the tumour immunogenicity.
Conventional cytotoxic chemotherapy has been shown to induce an immunogenic type of cell death in tumour cells, resulting in the emission of specific signals that trigger phagocytosis of cell debris and promote the maturation of dendritic cells, ultimately resulting in the potential induction of immune-mediated antitumor responses [21]. Chemotherapy in combination with ICIs has already shown improved efficacy in other solid tumours such as lung cancer [22] or oesophageal cancer [23]. Carboplatin, as a known DNA-disrupting agent active in PC, could cause tumour cell destruction and tumour-antigens release leading to the presentation of neoepitopes and stimulation of the immune system. It has been hypothesised that chemotherapy-induced tumour-antigen release can act as an “autovaccination” which could be subsequently exploited and enhanced with the addition of an ICI. Thus, we hypothesised that the combination of carboplatin chemotherapy and cancer immunotherapy could have synergistic potential. Here, we report on a Phase Ib study conducted to evaluate the safety and efficacy of combining carboplatin chemotherapy with PD-L1 inhibitor avelumab in metastatic CRPC patients progressing after at least one line of taxane chemotherapy and one line of an ARSI.
Materials and methods
Patients
This was an investigator-initiated open-label single-arm Phase Ib study investigating the safety and efficacy of PD-L1 inhibitor avelumab plus carboplatin in patients with mCRPC. Patients were eligible for enrolment if they were aged 18 years or older, had histologically confirmed metastatic prostate adenocarcinoma, were castration-resistant and had progressed to at least one taxane chemotherapy and one ARSI treatment. Additional key inclusion criteria were Eastern Cooperative Oncology Group (ECOG) performance status (PS) 0–2, adequate organ function and evaluable disease as per the Prostate Cancer Clinical Trials Working Group 3 (PCWG3) [24], measurable or not as per the RECIST v1.1 criteria [25]. Eligible patients were also required to provide archival or newly obtained tumour sample for the assessment of PD-L1 expression and tumour sequencing. Prior therapy with radium-223, carboplatin or PARP inhibitors was allowed, and there was no limit in number of prior lines of therapy. Key exclusion criteria were prior treatment with ICIs, active autoimmune diseases, prior allogeneic stem cell or solid organ transplantation, high dose of systemic corticosteroids (more than 10 mg of prednisone or equivalent per day) and known history of active infection by HIV or hepatitis B and C viruses or tuberculosis.
Treatment schedule and procedures
Patients received two cycles of induction carboplatin (area under the curve [AUC] = 5) every 3 weeks, followed by two cycles of avelumab 10 mg/kg combined with carboplatin (AUC = 5) every 3 weeks, and then by maintenance 2-weekly avelumab 10 mg/kg for 2 years. Therapy was stopped in case of progressive disease, unacceptable toxicity or patient consent withdrawal. During the avelumab maintenance phase, patients could be treated beyond confirmed disease progression if the study investigator, in agreement with the sponsor, determined that the patient continued to derive clinical benefit. Figure 1 illustrates the trial schema. To prevent avelumab infusion-related reactions, a premedication with an antihistamine and paracetamol 30–60 min prior to each dose of avelumab was mandatory for the first four cycles. The use of G-CSF for prophylactic and therapeutic purposes was allowed following local clinical practice. Dose delays for adverse events (AE) were permitted. Dose reduction of carboplatin was allowed as per standard local practice. No dose reductions were allowed for avelumab.
mCRPC metastatic castration-resistant prostate cancer, ARSI androgen-receptor signalling inhibitor, ICI immune-checkpoint inhibitor, ECOG PS Eastern Cooperative Oncology Group Performance status, RECIST Response Evaluation Criteria in Solid Tumours, AUC area under the curve, G3-4 Grade 3 or 4, PSA prostate-specific antigen, PFS progression-free survival, PCWG Prostate Cancer Working Group.
Pre-treatment assessment included a complete medical history, physical examination, haematology and biochemistry test, thyroid function, testosterone, PSA, hepatitis B and C serology, ECG, and tumour evaluation by bone scan and chest, abdomen and pelvis CT scan. Tumour assessments were performed every 6 weeks (±2 weeks) during the carboplatin phase, and thereafter every 12 weeks when on avelumab maintenance phase. Recently acquired or archival (ideally <3 years old) formalin-fixed, paraffin-embedded tumour samples were used for PD-L1 immunohistochemical staining and additional genomic studies. PD-L1 expression was assessed at a central laboratory with the use of the commercially available PD-L1 IHC 22C3 pharmDx assay (Dako North America). PD-L1 expression was categorised as the PD-L1 combined positive score (CPS), defined as the number of PD-L1-expressing tumour and infiltrating immune cells multiplied by 100 and divided by the total number of tumour cells. Patients were considered PD-L1 positive if CPS was ≥1.
Trial design and endpoints
The trial had two stages: a Safety Phase and an Expansion Phase (Fig. 1). In the Safety Phase, the primary endpoint of safety and tolerability was assessed. In this phase, three patients were initially treated at full dose (carboplatin (AUC = 5) and avelumab 10 mg/kg). If two or more of the three patients experienced a Grade 3–4 AE during the first cycle of combination therapy, three extra patients were allowed to be treated at the reduced dose of carboplatin (AUC = 4) with avelumab 10 mg/kg. If only one or less patients experienced a Grade 3–4 AE, three extra patients were allowed to be treated at the standard dose of carboplatin (AUC = 5) with avelumab 10 mg/kg. If no more than two patients among the first six patients included presented a Grade 3–4 AE, the safety endpoint was met and the opening of the Expansion Phase was allowed. In the Expansion Phase, 20 patients were included and treated at the recommended dose level, which corresponds to the dose received by the last 3 patients in the Safety Phase. In this phase, antitumor efficacy was assessed in terms of PSA and radiographic objective responses, radiographic PFS (rPFS), biochemical PFS (bPFS) and overall survival (OS) as per the PCWG3 (secondary endpoints).
A PSA response was defined as a decrease of at least 50% from the baseline value confirmed by a second value 3 or more weeks later. Confirmed PSA reductions of at least 30% were also recorded. Radiographic objective response rate (ORR) was defined as the proportion of patients with a radiographically confirmed complete or partial response as per RECIST v1.1 among patients with measurable disease. Disease control rate was defined as the percentage of patients achieving a complete response, partial response and stable disease, as the best response. PFS was defined as the time from randomisation to death or progression based on local radiographic assessment. bPFS was defined as the time from randomisation to death or biochemical progression based on PSA assessments. Biochemical progression was defined as an increase in the PSA level of more than 50% above the nadir in case of PSA reduction or above the baseline value in case of no prior reduction, with two consecutive increases at least 2 weeks apart. OS was defined as the time from randomisation to death. Duration of response was defined as the time from first documented complete or partial response to radiographically confirmed disease progression or death from any cause, whichever occurred first.
Safety assessments consisted of monitoring and recording all AEs, as per the National Cancer Institute Common Toxicity Criteria Adverse event (NCI-CTCAE) version 4.03 [26] and codified according to MedDRA dictionary. Data on AEs and serious AEs were collected from the time the informed consent was signed up to 90 days after the last dose of study treatment.
Trial oversight
The study was carried out with the approval of the Institutional Ethics committee of all participating institutions. The study was conducted in accordance with the ethical principles pronounced in the Declaration of Helsinki (Amendment 64th of the World Medical Association General Assembly, Fortaleza, Brazil, October 2013). A signed informed consent was obtained from each participant prior to any study procedure. An independent Safety Data Monitoring Committee with three external Medical Oncologists was selected for assessing the Safety data and allowing or not the continuation of the Expansion phase. This study was registered at the European Union Drug Regulating Authorities Clinical Trials Database as EudraCT Number 2017-004552-39.
Statistical considerations
For sample size calculation, a clinical benefit endpoint was used. Clinical benefit was defined as disease response or absence of disease progression in terms of PSA and radiographic assessment as per the PCWG3 criteria at 4 months of treatment initiation. For that purpose, we established a null hypothesis that at 4 months of treatment initiation, less than 50% of patients would meet the endpoint of clinical benefit. In order to demonstrate that clinical benefit with the study treatment combination could be achieved in equal or greater than 50% of patients, we calculated that a sample of 26 patients was needed in order to estimate with a confidence interval of 95% (±15 percentage units, unilateral α error of 0.1 and a β error of 0.1) a percentage of clinical benefit in the real disease population of around 50%. No interim analysis was planned. For the efficacy variable of ORR, the relative frequency and respective 95% confidence interval (CI) were calculated. The analysis of all time-to-event endpoints (OS and PFS) was done by the Kaplan–Meier curve with the respective 95% CI.
Results
Patients
From June 2018 to January 2020, 28 patients were evaluated for eligibility, and 26 were enrolled. Patient baseline disease characteristics are summarised in Table 1. The median age was 70 years (range 55–83), 42.3% were ECOG PS0 and 57.7% PS1. Most patients had advanced disease: 38.5% of patients had visceral metastasis, 65.4% had a bone superscan, and 61.5% were de novo metastatic at first diagnosis. Patients were heavily pretreated: 76.9% received ≥3 and 42.3% ≥4 survival-prolonging treatment lines. PD-L1 CPS expression was positive in 11.5% of cases (n = 3), negative in 61.5% (n = 16) and unknown in 26.9% (n = 7). A somatic DDR molecular alteration was found in three patients (11.5%), including BRCA2 (n = 1), ATM (n = 1) and FANC (n = 1).
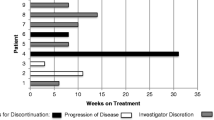
The primary reason for treatment discontinuation was disease progression (92.3%). Permanent treatment discontinuation due to AEs occurred in 1 patient (3.8%) who presented G4 thrombocytopenia and G2 urinary sepsis. The Median follow-up was 14.2 months (95% CI 12.7–17.9). The median treatment duration was 8.8 months (range 1.4–20.9). Four patients (15.4%) never received any cycle of avelumab due to rapid disease progression during the carboplatin induction phase but were included both in the safety and efficacy analyses.
Safety
In the Safety Phase, the first three patients were started on study treatment at full dose of the combination. Among these three patients, only one patient experienced a Grade 3 AE (anaemia and neutropenia) during the first combined cycle. Three extra patients were allowed at the same dose level, among which no Grade 3–4 AEs were observed. A Data Monitoring Committee with three external Medical Oncologists reviewed the Safety data and deemed the Safety endpoint had been met and that the recommended doses of the treatment combination were safe. The Expansion Phase was started at the recommended dose level of carboplatin (AUC = 5) plus avelumab 10 mg/kg.
AEs that occurred in at least 5% of patients (both Safety and Expansion phases) are summarised in Table 2. Treatment-emergent AEs (TEAE) of any grade were seen in 84.6% of patients. Grade 3 or worse TEAEs occurred in 73% of patients. Serious AEs of Grade 3–4 attributed to study treatment seen in 7.7% of patients. The most common TEAE of any grade were: thrombocytopenia (73%), anaemia (69.2%) and fatigue/asthenia (57.7%). The most frequent Grade 3 or worse TEAEs were: anaemia (61.5%), thrombocytopenia (53.8%), and neutropenia (26.9%). Only one patient experienced a febrile neutropenia (3.8%). There were no toxic deaths due to study treatment. Three patients (11.5%) presented immune-related TEAEs, including Grade 1 arthritis (n = 1), Grade 1 hypothyroidism (n = 1) and a Grade 4 neutropenia (n = 1, with confirmed antineutrophil autoantibodies). Eighteen patients (69.2%) temporarily interrupted or delayed therapy due to an AE. Carboplatin dose reductions occurred in 38.5% of patients.
Efficacy
At the time of the database lock (November 29, 2021), 15 deaths had occurred (57.7%), all of them due to disease progression. The Median follow-up was 14.3 months (95% CI 12.7–17.9). The median treatment duration was 8.8 months (range 1.4–20.9). Efficacy results are summarised in Table 3. Confirmed PSA response rates ≥30% and ≥50% were 15.4% (4/26) and 7.7% (2/26), respectively (Fig. 2a). Any reduction of PSA was seen in 34.6% of patients. Rising PSA as the best response was seen in 65.4% (17/26). Confirmed PSA response rates ≥50% were 33.3% (1/3) among PD-L1 positive patients and 6.2% (1/16) for PD-L1 negative (Table 3). Among patients with measurable disease (n = 17), there were two partial responses (2/17, 11.8%) and one complete response (1/17, 5.9%) for an ORR of 17.6% (Fig. 2b). Median duration of response was 6 months (range 4.2–16.5). Of note, two of these responders had a known somatic DDR deleterious alteration (one BRCA2 mutation, one ATM mutation) (Supplementary Table 1). Eight patients (30.7%) experienced progressive disease as the best response. The disease control rate was 69.2% (18/26), including responses and stabilisations (both in measurable and no measurable patients). A clinical benefit, defined as disease response or absence of disease progression at 4 months of treatment initiation was seen in 73.1% (n = 19).
a Prostate-specific antigen responses waterfall plot. ^BRCA2 alteration; *FANC alteration; °ATM alteration. Best percentage change from baseline in PSA level. Each column represents one patient. Increases greater than 100% are truncated to 100%. PSA prostate-specific antigen, PD-L1 programmed death ligand 1. b Radiographic objective responses waterfall plot. ^BRCA2 alteration; *FANC alteration; °ATM alteration. Best percentage change from baseline in the sum of longest diameters of target lesions as assessed by RECIST v1.1 in the 17 patients with measurable disease. PD-L1 programmed death ligand 1.
ORR was 33.3% (1/3) and 10% (1/10) for PD-L1 positive and negative patients, respectively (Table 3). ORR in DDR-altered patients was 66.6% (2/3) while only 10% in DDR-negative patients (1/10). Median OS was 10.6 months (95% CI 6.68–NR) (Fig. 3a) for a 6- and 18-months survival rate of 80.4% (95% CI 59.2–91.4) and 36% (95% CI 17.4–55.0), respectively. Median OS was 21 and 9.3 months, for PD-L1 positive and negative patients, respectively. Median bPFS was 4.19 months (95% CI 3.52–4.38). Median rPFS was 6.6 months (95% CI 4.28–9.01) (Fig. 3b). Median rPFS was 3.75 and 7.25 months, for PD-L1-positive and -negative patients, respectively.
a Overall survival. Median OS: 10.6 months (95% CI 6.68–NR). One-year survival rate: 36% (95% CI 17.4–55). b Radiographic progression-free survival. Median rPFS: 6.6 months (95% CI 4.28–9.01). One-year PFS rate: 15.4% (95% CI 4.8–31.5). OS overall survival, PFS progression-free survival, CI confidence interval, NR not reached.
Following study treatment discontinuation, 40% of the patients received any subsequent life-prolonging anticancer therapy (Table 1). The median number of subsequent treatment lines was 1 (range 0–3).
Discussion
This is the first report on the safety and efficacy of the combination of avelumab and carboplatin chemotherapy in patients with mCRPC. Avelumab plus carboplatin had an acceptable safety profile with no greater toxicities with the combination than with each individual agent alone, meeting the prespecified primary endpoint of safety. Only one patient (3.8%) stopped study therapy due to AEs and there were no toxic deaths. Most Grade 3–4 TEAE were haematological toxicities (anaemia 61.5%, thrombocytopenia 53.8%, neutropenia 26.9%) and were related to carboplatin in an advanced patient population with significant volume of bone metastases (65.4% superscan) and probable bone marrow infiltration. We believe the high rate of haematological toxicities was mainly due to the AUC5 dosage of carboplatin and not to any additive effect of avelumab, since most of these toxicities improved with carboplatin dose reductions and did not reoccur during the avelumab maintenance phase. Our cohort of patients was heavily pretreated (42.3% of patients having received four or more survival-prolonging prior therapies) and had poor-prognosis features, including a high proportion of patients with visceral metastases, low haemoglobin and high alkaline phosphatase. In spite of that, avelumab plus carboplatin was associated with promising efficacy with an overall clinical benefit in 73% of patients and a prolonged median OS of 10.6 months. Treatment combination resulted in confirmed PSA response rates ≥50% in 7.7% of patients and an ORR of 17.6%, including one complete response in a patient with bulky lymph node-only disease. The clinical benefit with the combination was durable, with a median duration of response of 6 months and a 12-month survival rate of 36%.
Other combinations trials of PD-1/PD-L1 inhibitors in mCRPC have been reported so far. Ongoing trials include combinations with different drug agents, such as docetaxel chemotherapy [27, 28], ARSIs [29,30,31,32], CTLA-4 inhibitors [32, 33], antiangiogenic tyrosine-kinase inhibitors [34], PARP inhibitors [35,36,37] and radiopharmaceutical agents [38]. Most of these trials are small-sized Phase 1–2 trials in unselected mCRPC patients progressing to at least one line of ARSI and have reported so far mixed results, with signs of long-term efficacy in some subgroups of patients but overall, less activity than that observed in other cancers. To date, only one randomised Phase 3 trial, the Imbassador250 trial comparing atezolizumab with enzalutamide versus enzalutamide alone in mCRPC, has been published [29]. The study failed to show any benefit in terms of median OS of adding atezolizumab to enzalutamide compared to enzalutamide alone (15.2 versus 16.6 months, HR 1.12, 95% CI 0.91–1.37, P = 0.28) and the study was halted prematurely. Secondary endpoints, including rPFS (4.2 versus 4.1 months, HR 0.90, 95% CI 0.75–1.07), P = 0.28 and ORR (13.7% versus 7.4%) also failed to show a benefit for the treatment combination versus enzalutamide alone. Given the fact that the Imbassador250 trial included a much less pretreated population, with most patients only receiving one prior line of ARSI, our study showed encouraging efficacy with a numerically superior rPFS and ORR. Two Phase 2 trials have evaluated the combination of docetaxel chemotherapy with either pembrolizumab (KEYNOTE-365 cohort B) or nivolumab (CheckMate 9KD trial cohort B) in docetaxel-naïve mCRPC patients [27, 28]. These two studies have yielded signs of greater efficacy compared to our study, with a median OS of 20.2 and 18.2 months, a rPFS of 8.5 and 9.0 months and an ORR of 40% and 25%, for the pembrolizumab and nivolumab combination studies, respectively. Despite the fact that docetaxel chemotherapy is not a DNA-disrupting agent and that there is less evidence of his role as immunogenic cell death inducer than carboplatin [39], the known greatest antitumor efficacy of docetaxel monotherapy in mCRPC might in part explain the better outcomes of its combination with PD-1 inhibitors compared to our study. Other studies evaluating the use of carboplatin combined with ICI in mCRPC are also ongoing and are especially being focused in patients with aggressive variant prostate cancer (NCT02861573, NCT04592237, NCT02703623) [40].
DDR alterations have been associated with increased benefit to ICIs in several solid tumours due to increased genomic instability and novel neoantigens potentially enhancing immune-mediated antitumor responses [41]. Platinum chemotherapy has also been demonstrated to induce synthetic lethality in patients harbouring alterations in DDR genes, resulting in increased benefit to this therapy [42]. While the activity of the avelumab–carboplatin combination was apparent in all patient subgroups in our Phase 1 trial, our data indicate a potential greater efficacy in DDR-altered patients and PD-L1-positive tumours. ORR in DDR-altered patients was 66.6% (2/3) compared to only 10% in DDR-negative patients (1/10). Similarly, PD-L1-positive had an ORR of 33.3% while negative patients only 10%. Median OS was also longer for PD-L1-positive patients (21 months) compared to negative patients (9.3 months). The role of DDR alterations and PD-L1 expression as potential predictive biomarkers of benefit to PD-1 blockade has been assessed in several clinical trials in mCRPC with conflicting results. In both the Imbassador250 Phase 3 trial and CheckMate 9KD Phase 2 trial, the presence of DDR alterations was not associated with better outcomes in patients treated with the combinations [27, 29]. On the other hand, in the CheckMate 650 Phase 2 trial of nivolumab-ipilimumab in mCRPC patients, DDR alterations significantly correlated with greater OS, rPFS and ORR [33]. Similarly, in two PARP inhibitors combination Phase 2 trials of nivolumab-rucaparib (CheckMate 9KD trial cohort A2) and durvalumab-olaparib in molecularly unselected mCRPC, the presence of DDR alterations was associated with increased efficacy [35, 37]. However, given the proven predictive role of DDR alterations to benefit with PARP inhibitors [43], it is impossible to discern whether this increased efficacy is solely due to the PARP inhibitor or whether the addition of the PD-1 inhibitor is also playing a role. Regarding PD-L1 expression, only in the CheckMate 650 Phase 2 trial, the efficacy of ICI combination was enriched in patients with high PD-L1 expression [33], while no such correlation was seen among the other clinical trials mentioned above. Taken together, the inconsistency surrounding the role of DDR alterations and PD-L1 expression as predictive biomarkers to ICIs questions their clinical utility in mCRPC. Other potential molecular biomarkers such as the presence of biallelic CDK12 loss, MSI status, TMB, tumour indel burden and TGF-beta signature are currently being investigated as potentially predictive biomarkers of ICIs [44, 45]. Other strategies currently under investigation for harnessing the immune system against prostate cancer include using PSMA as a tumour-associated antigen as a target for bi-specific T-cell engager (BiTE) therapy or CAR-T cells [46, 47].
Our study has several limitations, including the small patient population and the non-randomised single-arm design of the study. The lack of a molecular DDR analysis and PD-L1 status in a significant proportion of patients also limits our ability to establish a conclusive role of these as potential predictive biomarkers. In this small patient cohort, biomarker analysis is exploratory and only hypothesis-generating. The poor-prognosis and heavily pretreated population included in our trial also limited our ability to assess the potential synergy of avelumab and carboplatin as well as our possibility to test the hypothesis of carboplatin-induced immune cell death and autovaccination. Four patients (15.4%) included in our study never received any cycle of avelumab due to rapid disease progression during the first two cycles of induction carboplatin monotherapy, highlighting the advanced state of the disease in our cohort. Nevertheless, these four patients were also included in the efficacy analysis. Testing this combination in a less pretreated mCRPC cohort, could have been a more adequate strategy in order to reduce the risk of rapid disease progressions. Administering upfront avelumab in combination with carboplatin without an induction carboplatin phase could also have been an alternative trial design for better assessing their potential synergy, especially in such an advanced patient population.
In spite of these limitations, avelumab combined with carboplatin demonstrated encouraging efficacy in a heavily pretreated mCRPC cohort, with durable disease control in nearly 70% of patients and a prolonged overall survival. These results do not appear to be explained by an enrichment of DDR-altered or PD-L1 positive cases. The avelumab–carboplatin combination warrants further examination in future randomised clinical trials.
Data availability
The datasets generated and/or analysed during this study are available from the corresponding author upon reasonable request.
References
Bray F, Lortet-Tieulent J, Ferlay J, Forman D, Auvinen A. Prostate cancer incidence and mortality trends in 37 European countries: an overview. Eur J Cancer. 2010;46:3040–52.
Sweeney CJ, Chen YH, Carducci M, Liu G, Jarrard DF, Eisenberger M, et al. Chemohormonal therapy in metastatic hormone-sensitive prostate cancer. N Engl J Med. 2015;373:737–46.
Fizazi K, Tran N, Fein L, Matsubara N, Rodriguez-Antolin A, Alekseev BY, et al. Abiraterone plus prednisone in metastatic, castration-sensitive prostate cancer. N Engl J Med. 2017;377:352–60.
Davis ID, Martin AJ, Stockler MR, Begbie S, Chi KN, Chowdhury S, et al. Enzalutamide with standard first-line therapy in metastatic prostate cancer. N Engl J Med. 2019;381:121–31.
Chi KN, Agarwal N, Bjartell A, Chung BH, Pereira de Santana Gomes AJ, Given R, et al. Apalutamide for metastatic, castration-sensitive prostate cancer. N Engl J Med. 2019;381:13–24.
de Bono JS, Oudard S, Ozguroglu M, Hansen S, Machiels JP, Kocak I, et al. Prednisone plus cabazitaxel or mitoxantrone for metastatic castration-resistant prostate cancer progressing after docetaxel treatment: a randomised open-label trial. Lancet. 2010;376:1147–54.
Petrylak DP, Tangen CM, Hussain MH, Lara PN, Jones JA, Taplin ME, et al. Docetaxel and estramustine compared with mitoxantrone and prednisone for advanced refractory prostate cancer. N Engl J Med. 2004;351:1513–20.
Tannock IF, de Wit R, Berry WR, Horti J, Pluzanska A, Chi KN, et al. Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. N Engl J Med. 2004;351:1502–12.
de Bono JS, Logothetis CJ, Molina A, Fizazi K, North S, Chu L, et al. Abiraterone and increased survival in metastatic prostate cancer. N Engl J Med. 2011;364:1995–2005.
Ryan CJ, Smith MR, de Bono JS, Molina A, Logothetis CJ, de Souza P, et al. Abiraterone in metastatic prostate cancer without previous chemotherapy. N Engl J Med. 2013;368:138–48.
Scher HI, Fizazi K, Saad F, Taplin ME, Sternberg CN, Miller K, et al. Increased survival with enzalutamide in prostate cancer after chemotherapy. N Engl J Med. 2012;367:1187–97.
Beer TM, Armstrong AJ, Rathkopf DE, Loriot Y, Sternberg CN, Higano CS, et al. Enzalutamide in metastatic prostate cancer before chemotherapy. N Engl J Med. 2014;371:424–33.
Parker C, Nilsson S, Heinrich D, Helle SI, O’Sullivan JM, Fosså SD, et al. Alpha emitter radium-223 and survival in metastatic prostate cancer. N Engl J Med. 2013;369:213–23.
Sartor O, de Bono J, Chi KN, Fizazi K, Herrmann K, Rahbar K, et al. Lutetium-177-PSMA-617 for metastatic castration-resistant prostate cancer. N Engl J Med. 2021;385:1091–103.
Petrylak DP, Loriot Y, Shaffer DR, Braiteh F, Powderly J, Harshman LC, et al. Safety and clinical activity of atezolizumab in patients with metastatic castration-resistant prostate cancer: a phase I study. Clin Cancer Res. 2021;27:3360–9.
Hansen AR, Massard C, Ott PA, Haas NB, Lopez JS, Ejadi S, et al. Pembrolizumab for advanced prostate adenocarcinoma: findings of the KEYNOTE-028 study. Ann Oncol. 2018;29:1807–13.
Antonarakis ES, Piulats JM, Gross-Goupil M, Goh J, Ojamaa K, Hoimes CJ, et al. Pembrolizumab for treatment-refractory metastatic castration-resistant prostate cancer: multicohort, open-label phase II KEYNOTE-199 study. J Clin Oncol. 2020;38:395–405.
Palicelli A, Croci S, Bisagni A, Zanetti E, De Biase D, Melli B, et al. What do we have to know about PD-L1 expression in prostate cancer? A systematic literature review. Part 3: PD-L1, intracellular signaling pathways and tumor microenvironment. Int J Mol Sci. 2021;22:12297.
Kantoff PW, Higano CS, Shore ND, Berger ER, Small EJ, Penson DF, et al. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N Engl J Med. 2010;363:411–22.
Fizazi K, Drake CG, Beer TM, Kwon ED, Scher HI, Gerritsen WR, et al. Final analysis of the ipilimumab versus placebo following radiotherapy phase III trial in postdocetaxel metastatic castration-resistant prostate cancer identifies an excess of long-term survivors. Eur Urol. 2020;78:822–30.
Bracci L, Schiavoni G, Sistigu A, Belardelli F. Immune-based mechanisms of cytotoxic chemotherapy: implications for the design of novel and rationale-based combined treatments against cancer. Cell Death Differ. 2014;21:15–25.
Rodríguez-Abreu D, Powell SF, Hochmair MJ, Gadgeel S, Esteban E, Felip E, et al. Pemetrexed plus platinum with or without pembrolizumab in patients with previously untreated metastatic nonsquamous NSCLC: protocol-specified final analysis from KEYNOTE-189. Ann Oncol. 2021;32:881–95.
Doki Y, Ajani JA, Kato K, Xu J, Wyrwicz L, Motoyama S, et al. Nivolumab combination therapy in advanced esophageal squamous-cell carcinoma. N Engl J Med. 2022;386:449–62.
Scher HI, Morris MJ, Stadler WM, Higano C, Basch E, Fizazi K, et al. Trial design and objectives for castration-resistant prostate cancer: updated recommendations from the prostate cancer clinical trials working group 3. J Clin Oncol. 2016;34:1402–18.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–47.
Common Terminology Criteria for Adverse Events (CTCAE) Version 4.0. (v4.03: June 14, 2010). https://www.eortc.be/services/doc/ctc/ctcae_4.03_2010-06-14_quickreference_5x7.pdf. Accessed February 2022.
Fizazi K, González Mella P, Castellano D, Minatta JN, Rezazadeh Kalebasty A, Shaffer D, et al. Nivolumab plus docetaxel in patients with chemotherapy-naïve metastatic castration-resistant prostate cancer: results from the phase II CheckMate 9KD trial. Eur J Cancer. 2022;160:61–71.
Fizazi K, González Mella P, Castellano D, Minatta JN, Rezazadeh A, Shaffer DR, et al. CheckMate 9KD arm B final analysis: efficacy and safety of nivolumab plus docetaxel for chemotherapy-naïve metastatic castration-resistant prostate cancer. J Clin Oncol. 2021;39.6(suppl):12.
Powles T, Yuen KC, Gillessen S, Kadel EE, Rathkopf D, Matsubara N, et al. Atezolizumab with enzalutamide versus enzalutamide alone in metastatic castration-resistant prostate cancer: a randomized phase 3 trial. Nat Med. 2022;28:144–53.
Graff JN, Beer TM, Alumkal JJ, Slottke RE, Redmond WL, Thomas GV, et al. A phase II single-arm study of pembrolizumab with enzalutamide in men with metastatic castration-resistant prostate cancer progressing on enzalutamide alone. J Immunother Cancer. 2020;8.
Hoimes CJ, Graff JN, Tagawa ST, Hwang C, Kilari D, Tije AJT, et al. KEYNOTE-199 cohorts 4 and 5: Phase II study of pembrolizumab plus enzalutamide for Enza-resistant metastatic castration-resistant prostate cancer (mCRPC). J Clin Oncol. 2020;38(15_suppl):5543.
Shenderov E, Boudadi K, Fu W, Wang H, Sullivan R, Jordan A, et al. Nivolumab plus ipilimumab, with or without enzalutamide, in AR-V7-expressing metastatic castration-resistant prostate cancer: a phase-2 nonrandomized clinical trial. Prostate. 2021;81:326–38.
Sharma P, Pachynski RK, Narayan V, Fléchon A, Gravis G, Galsky MD, et al. Nivolumab plus ipilimumab for metastatic castration-resistant prostate cancer: preliminary analysis of patients in the CheckMate 650 trial. Cancer Cell. 2020;38:489–99.e3.
Agarwal N, McGregor BA, Maughan BL, Dorff T, Kelly W, Fang B, et al. Cabozantinib in combination with atezolizumab in patients with metastatic castration resistant prostate cancer mCRPC): results of expanded cohort 6 of the COSMIC 021 study. Ann Oncol. 2021;32:S1283–346.
Karzai F, VanderWeele D, Madan RA, Owens H, Cordes LM, Hankin A, et al. Activity of durvalumab plus olaparib in metastatic castration-resistant prostate cancer in men with and without DNA damage repair mutations. J Immunother Cancer. 2018;6:141.
Yu E, Piulats JM, Gravis G, Fong PC, Todenhöfer T, Laguerre B, et al. Pembrolizumab plus olaparib in patients with docetaxel-pretreated metastatic castration-resistant prostate cancer: update of KEYNOTE-365 cohort a with a minimum of 11 months of follow-up for all patients. Ann Oncol. 2021;32:S652–3.
Petrylak DP, Perez-Gracia JL, Lacombe L, Bastos DA, Mahammedi H, Kwan EM, et al. CheckMate 9KD cohort A2 final analysis: nivolumab plus rucaparib for chemotherapy naïve metastatic castration resistant prostate cancer. Ann Oncol. 2021;32:S626–77.
Fong L, Morris MJ, Sartor O, Higano CS, Pagliaro L, Alva A, et al. A phase Ib study of atezolizumab with radium-223 dichloride in men with metastatic castration-resistant prostate cancer. Clin Cancer Res. 2021;27:4746–56.
Flieswasser T, Van Loenhout J, Freire Boullosa L, Van den Eynde A, De Waele J, Van Audenaerde J, et al. Clinically relevant chemotherapeutics have the ability to induce immunogenic cell death in non-small cell lung cancer. Cells. 2020;9:1474.
De Bono JS, Joshua AM, Shore ND, Kramer G, Tong Li X, Poehlein CH, et al. KEYNOTE-365 cohort I: phase 1b/2 study of pembrolizumab combined with platinum-containing chemotherapy and chemotherapy alone for treatment-emergent neuroendocrine prostate carcinoma (t-NE). J Clin Oncol. 2022;(suppl 6; abstr TPS218):40.
Zhang J, Shih DJH, Lin SY. Role of DNA repair defects in predicting immunotherapy response. Biomark Res. 2020;8:23.
Mota JM, Barnett E, Nauseef JT, Nguyen B, Stopsack KH, Wibmer A, et al. Platinum-based chemotherapy in metastatic prostate cancer with DNA repair gene alterations. JCO Precis Oncol. 2020;4:355–66.
Mateo J, Porta N, Bianchini D, McGovern U, Elliott T, Jones R, et al. Olaparib in patients with metastatic castration-resistant prostate cancer with DNA repair gene aberrations (TOPARP-B): a multicentre, open-label, randomised, phase 2 trial. Lancet Oncol. 2020;21:162–74.
Wu YM, Cieślik M, Lonigro RJ, Vats P, Reimers MA, Cao X, et al. Inactivation of CDK12 delineates a distinct immunogenic class of advanced prostate. Cancer Cell. 2018;173:1770–82.e14.
Le DT, Durham JN, Smith KN, Wang H, Bartlett BR, Aulakh LK, et al. Mismatch repair deficiency predicts response of solid tumors to PD-1 blockade. Science. 2017;357:409–13.
Narayan V, Barber-Rotenberg J, Fraietta J, Hwang WT, Lacey SF, Plesa G, et al. A phase I clinical trial of PSMA-directed/TGFβ-insensitive CAR-T cells in metastatic castration-resistant prostate cancer. J Clin Oncol. 2021;39:125–125.
De Bono JS, Fong L, Beer TM, Gao X, Geynisman DM, Burris HA, et al. Results of an ongoing phase 1/2a dose escalation study of HPN424, a tri-specific half-life extended PSMA-targeting T-cell engager, in patients with metastatic castration-resistant prostate cancer (mCRPC). J Clin Oncol. 2021;(suppl 15; abstr 5013):39.
Acknowledgements
Study was carried out by Pivotal CRO. Statistical analyses were performed by Tania San José. The Sponsor of the study was APRO (Associació per la recerca oncològica, Spanish Oncology Research Group).
Funding
Funding for this study was jointly provided through an unrestricted educational grant from Pfizer, Inc, New York, NY, USA and Merck KGaA, Darmstadt, Germany, as part of an alliance between Merck (CrossRef Funder ID: 10.13039/100009945) and Pfizer. Pfizer and Merck reviewed the manuscript for medical accuracy only before journal submission. The authors are fully responsible for the content of this manuscript, and the views and opinions described in the publication reflect solely those of the authors.
Author information
Authors and Affiliations
Contributions
All authors conceived and/or designed the work that led to the submission, acquired data and/or played an important role in interpreting the results; drafted or revised the manuscript; approved the final version and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was carried out with the approval of the Institutional Ethics committee of all participating institutions. The study was conducted in accordance with the ethical principles pronounced in the Declaration of Helsinki (Amendment 64th of the World Medical Association General Assembly, Fortaleza, Brazil, October 2013). This study was registered at the European Union Drug Regulating Authorities Clinical Trials Database as EudraCT Number 2017-004552-39.
Consent to publish
A signed informed consent was obtained from each participant prior to any study procedure.
Competing interests
Dr. JB reports serving in an advisory role to Genentech, MSD, Pfizer, GSK, BMS, AstraZeneca, Pierre-Fabre, Sanofi Aventis, Astellas, OncoGenex, and Janssen; receiving honoraria or travel expenses from Pfizer, MSD, GSK, Novartis, Pierre-Fabre, Astellas, and BMS; and receiving research funding from Takeda, Pfizer, Novartis, and Sanofi Aventis. Dr. AR-V reports serving in an advisory role for MSD, Pfizer, BMS, Astellas, Janssen, Bayer, Clovis and Roche; receiving honoraria or travel expenses from Pfizer, MSD, Astellas, BMS, Janssen, AstraZeneca, Roche, Bayer, and Sanofi Aventis; and receiving research funding from Takeda, Pfizer, and Merck. Dr. PM reports serving in advisory board for Pfizer, Ipsen, and BMS. Dr. AF reports serving in an advisory role to Janssen, Astellas, Sanofi, Eusa; and receiving research funding from AstraZeneca. Dr. BM has received consulting fees from Pfizer, Roche, AstraZeneca, Bayer, Astellas Pharma, and Janssen, support for attending meetings or travel from Janssen-Cilag; and other financial or non-financial interests from Roche, Janssen, and Bayer. Dr. AT reports personal fees and non-financial support from Roche, BMS, MSD, GSK, AstraZeneca and Pfizer. Dr. AC reports receiving honoraria or travel expenses from Astellas, BMS, Janssen, and Merck. Dr. RQ repots Personal fees and non-financial support from Merck, Sanofi Aventis, Roche, Pfizer, Jansen, Amgen and Astellas. Dr. OJ declares being an employee of Pivotal SLU. Dr. MM-G reports serving in an advisory role for Roche, Seagen and Pierre-Fabre; receiving honoraria or travel expenses from Roche and Pfizer. Dr. NJ reports serving in an advisory role for AstraZeneca; and receiving honoraria or travel expenses from Roche and MSD. Dr. Oscar Reig, Dr. AR-H, Dr. MO and Dr. CM report no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rodriguez-Vida, A., Maroto, P., Font, A. et al. Safety and efficacy of avelumab plus carboplatin in patients with metastatic castration-resistant prostate cancer in an open-label Phase Ib study. Br J Cancer 128, 21–29 (2023). https://doi.org/10.1038/s41416-022-01991-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-022-01991-4
- Springer Nature Limited
This article is cited by
-
Unlocking ferroptosis in prostate cancer — the road to novel therapies and imaging markers
Nature Reviews Urology (2024)
-
Therapeutic cancer vaccines: advancements, challenges and prospects
Signal Transduction and Targeted Therapy (2023)