Abstract
Background
Dose-dense sequential chemotherapy with anthracyclines and taxanes achieved an 18% reduction of recurrence risk in early breast cancer (BC). The optimal chemotherapy schedule and interval between cycles remain under investigation.
Methods
Overall, 990 patients were randomised to receive either three cycles of epirubicin (E, 110 mg/m2) every 2 weeks followed by 3 cycles of paclitaxel (T, 200 mg/m2) every 2 weeks followed by three cycles of intensified CMF (Control Arm A, E-T-CMF) that was previously used in BC or three cycles of epirubicin followed by three cycles of CMF followed by nine consecutive weekly cycles of docetaxel (wD) 35 mg/m2 (Arm B, E-CMF-wD) or nine consecutive weekly cycles of paclitaxel (wT) 80 mg/m2 (Arm C, E-CMF-wT). Trastuzumab was administered for HER2-positive disease.
Results
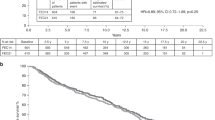
At a median follow-up of 13.3 years, 330 disease-free survival (DFS) events (33.3%) were reported. DFS and overall survival (OS) did not differ between patients in the combined B and C arms versus arm A either in the entire cohort (HR = 0.90, P = 0.38 and HR = 0.85, P = 0.20) or among trastuzumab-treated patients (HR = 0.69, P = 0.13 and HR = 0.67, P = 0.13). Thirty-four patients (3.4%) developed secondary neoplasms.
Conclusions
Overall, no significant differences in survival were found amongst the studied regimens after a long-term observational period.
Trial registration
Australian New Zealand Clinical Trials Registry ACTRN12610000151033.
Similar content being viewed by others
Background
Breast cancer (BC) remains the most common malignancy in the European Union (EU-28) [1] and in the United States of America (USA) [2] as well as in women worldwide, accounting for 2,261,419 new cases in 2020 [3]. However, screening programs and novel treatment options have resulted in a 41% decrease in BC-related mortality from 1989 to 2018 in the USA [2]. In early-stage disease, surgical treatment along with anthracycline and/or taxane-based adjuvant chemotherapy has essentially improved the clinical outcome. In particular, based on the National Surgical Adjuvant Breast and Bowel Project (NSABP) B-15 trial, which showed that the combination of cyclophosphamide with doxorubicin (AC) is equivalent to that of cyclophosphamide, methotrexate and fluorouracil (CMF), AC has become the standard-of-care in the adjuvant setting [4]. In node-negative disease, AC has been replaced by the equally effective and less toxic docetaxel and cyclophosphamide regimen (TC) [5]. In node-positive disease, however, taxanes have been currently added to anthracycline-based chemotherapy further reducing the mortality of early breast cancer by about one-third [6,7,8,9,10].
Another cornerstone of the adjuvant treatment has been the dosing schedule of adjuvant chemotherapy, which has been studied extensively since then. Higher dose intensity can be achieved either by increasing the dose administered per cycle or by reducing the intervals between cycles (i.e. dose density) [11]. Taking into account the Norton Simon hypothesis, which predicts that chemotherapy achieves tumour regression in a proportional relationship to the rate of tumour growth, the reduction of the intervals between chemotherapy cycles could potentially lead to a greater antineoplastic effect [12]. This hypothesis has been brought to clinical practice based on numerous Phase III clinical trials and thanks to the support with hemopoietic growth factors. More specifically, the Cancer and Leukemia Group B (CALGB) B9741 Phase III trial demonstrated that dose-dense adjuvant chemotherapy [doxorubicin (A), cyclophosphamide (C) and paclitaxel (T)] either in sequential (A—T—C) or concurrent administration (AC—T) significantly improves the disease-free survival (DFS) and overall survival (OS) [13]. Similarly, the AGO Phase III trial also reported a significantly prolonged DFS and OS in intense dose-dense adjuvant chemotherapy with sequential epirubicin, paclitaxel and cyclophosphamide every 2 weeks, compared to standard epirubicin/cyclophosphamide followed by paclitaxel (EC → P) every 3 weeks after 10 years of follow-up [14]. On the other hand, many Phase III clinical trials, such as PANTHER 3, the GIM2 trial, UK TACT2, NSABP B-38, GONO-MIG and GAIN, have reported conflicting results regarding the efficacy of dose-dense chemotherapy [15,16,17,18,19,20]. Recently, meta-analyses of randomised controlled trials have shown that the dose-density strategy of adjuvant chemotherapy further reduces the risk of recurrence, leading to improved DFS and OS [21,22,23].
In addition, sequential administration of chemotherapy, as we mentioned, is also of paramount importance for modern treatment options in BC. According to Phase III clinical trials, sequential dosing schedules were proven to be more effective since they allowed an increase in dose density [24, 25]. A recent meta-analysis showed that sequential administration of anthracycline and taxane regimens results in a 13% proportional reduction of the recurrence rate by achieving a dose-density ratio ranging from 1 to 1.5 [21]. When this sequential scheme was administered dose-intensely, a further reduction of 18% in recurrence was observed [21]. Another meta-analysis also confirmed the superiority of sequential chemotherapy [26]. The increased efficacy of sequential dosing schedules over alternating therapies has been further supported by numerous Phase III clinical trials [13, 14, 18, 27].
Based on the aforementioned studies, the Hellenic Cooperative Oncology Group (HeCOG) has adopted, since 1997, both principles of contemporary chemotherapy for early breast cancer (EBC), i.e. dose-dense and sequential administration of anticancer drugs. In this context, we designed and conducted two randomised trials in patients with EBC, incorporating a taxane to epirubicin and ‘intensified’ CMF (E-T-CMF) [28,29,30]. Although CMF has been currently supplanted by anthracycline and taxane-containing regimens in the adjuvant setting, CMF has been considered the mainstay of adjuvant treatment for years. With the advent of trastuzumab in the adjuvant setting in 2005, we designed and completed a randomised trial (HE10/05) with dose-dense sequential chemotherapy with the above-mentioned agents plus trastuzumab for 1 year for patients with HER2-positive tumours. The results of the interim analysis of this trial were previously published [31]. In this trial, the E-T-CMF regimen served as the control arm based on the results on efficacy and safety from randomised trials published by our group [28,29,30]. Herein, we report the results of the final analysis of the HE10/05 trial upon collection of the required number of relapses, as prespecified, in the study design, as well as a prolonged period of follow-up.
Patients and methods
Study design and participants
Patient characteristics, methods and design of the ΗΕ10/05 trial have been previously reported [31]. Briefly, HE10/05 was a Greek, open-label, multicenter, Phase III, randomised clinical trial in patients with histologically confirmed node-positive BC or node-negative patients, with at least one of the following criteria: pT > 2 cm, or histological and/or nuclear Grade 2–3, or presence of peritumoral vascular invasion, or HER2 (human epidermal growth factor receptor 2) overexpression and/or amplification, or age <35 years, defined as “intermediate risk” according to the 2005 St. Gallen criteria [32].
Patients were to have undergone a breast-conserving surgery with tumour-free margins or modified radical mastectomy and an adequate bone marrow, hepatic, cardiac and renal function. The study was conducted at HeCOG affiliated departments of medical oncology upon the approval of Institutional Review Boards and the National Organization for Medicines; written informed consent was obtained from all patients before trial enrolment. The study was conducted in accordance with Good Clinical Practice guidelines and the Declaration of Helsinki [33].
Eligible patients were randomly assigned to receive one of the following three chemotherapeutic schedules: three cycles of epirubicin (E, 110 mg/m2) every 2 weeks followed by three cycles of paclitaxel (T, 200 mg/m2) every 2 weeks followed by three cycles of intensified CMF (cyclophosphamide 840 mg/m2, methotrexate 57 mg/m2 and fluorouracil 840 mg/m2) every 2 weeks (Control arm A, E-T-CMF), or three cycles of epirubicin followed by three cycles of CMF, as in Arm A, followed 3 weeks later by nine consecutive weekly cycles of docetaxel (wD) 35 mg/m2 (Experimental arm B, E-CMF-wD), or nine consecutive weekly cycles of paclitaxel (wT) 80 mg/m2 (experimental arm C, E-CMF-wT) with the support of G-CSF, following each cycle in Arm A and during the intensified phases of epirubicin and CMF treatments in Arms B and C.
Patients with HER2-positive tumours were treated with trastuzumab, initially at a dose of 8 mg/kg as a loading dose, and subsequently 6 mg/kg every 3 weeks for 1 year. Premenopausal patients with hormone receptor-positive status received oral tamoxifen 20 mg daily for 5 years and goserelin 10.8 mg subcutaneously every 3 months for 2 years. Postmenopausal patients with hormone receptor-positive status were treated daily with anastrozole 1 mg orally for 5 years. Postoperative radiation therapy (RT) was given to patients who underwent partial mastectomy or those with tumour size ≥5 cm and/or more than four positive lymph nodes, irrespective of the type of surgery. RT was initiated 3–4 weeks after the completion of chemotherapy.
Statistical analysis
The primary study endpoint was the invasive disease-free survival (DFS), estimated from the date of study entry to first locoregional recurrence, distant metastasis, contralateral BC, secondary neoplasm, death (from any cause) or last contact, whichever occurred first [34]. Overall survival (OS), measured from study entry until death (from any cause) or last contact, was a secondary endpoint. As previously reported, the study’s primary hypothesis was that since the sequential epirubicin, CMF and weekly docetaxel or paclitaxel schedules (Arms B and C) were equally effective in terms of DFS, a comparison of the combined Arms B and C to sequential epirubicin, paclitaxel and CMF administration (Arm A) would be of interest. For a 5% difference between the combined arms (Arms B and C) vs. the control arm (Arm A) and a power of 80%, 1000 patients had to be enrolled in the study given a 3-year DFS rate of 80% in arm A. The study recruitment was closed in November 2008 after the enrolment of 1001 patients. According to the statistical design, a total of 329 DFS events should be observed and an interim analysis was performed at approximately half of the events. In the current analysis, a total of 330 DFS events were reported in eligible participants after a median follow-up time of approximately 13 years.
All efficacy analyses were conducted according to the intent-to-treat (ITT) principle. OS and DFS survival rates were obtained via Kaplan–Meier analyses and compared between treatment arms with the log-rank test. Cox regression models were applied to estimate the prognostic effect of treatment on DFS and OS separately in the entire cohort and among patients treated with trastuzumab for their HER2-positive disease. In multivariate analysis, model choice with a backwards selection criterion of P < 0.10 was applied in the presence of the randomisation arm (combined arms B and C vs. A). The following parameters were included in the initial step of each model applied in the entire cohort: menopausal status (postmenopausal vs. premenopausal), tumour size (>2 vs. ≤2), histological grade (Grade III vs. I–II), number of positive nodes (≥4 and 1–3 vs. 0), ER (Oestrogen receptor)/PgR (Progesterone receptor) status (positive vs. negative) and HER2 status (positive vs. negative). In the subgroup of patients treated with trastuzumab the following parameters were included in the initial step of multivariate models: menopausal status (postmenopausal vs. premenopausal), tumour size (>2 vs. ≤2), histological grade (Grade III vs. I–II), number of positive nodes (≥4 and 1–3 vs. 0). All statistical analyses were performed using the SAS software (SAS version 9.3, SAS Institute Inc. Cary, NC, USA). Statistical significance was set at a two-sided P of 0.050.
Results
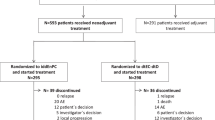
A total of 1001 patients with BC were recruited between July 2005 and November 2008. Eleven patients were considered ineligible and were excluded from the analysis. Among 990 eligible patients, 333 (33.6%) were randomised to receive E-T-CMF, 331 (33.4%) E-CMF-wD and 326 (32.9%) E-CMF-wT. All chemotherapy cycles were administered as per protocol in 91.9% of patients in arm A, 84.3% of arm B and 92% of arm C, respectively. Treatment compliance and reasons for early discontinuation have been previously reported [31].
Within a median follow-up of 13.3 years (95% CI 13.2–13.4, range 0.5–179.8 months), a total of 330 DFS events (33.3%) had been reported [113 DFS events in arm A (33.9%), 119 in arm B (36%) and 98 in arm C (30.1%)] and 272 patients (27.5%) had died [96 deaths in arm A (28.8%), 97 in arm B (29.3%) and 79 in arm C (24.2%)]. The minimum follow-up for alive patients (not lost to follow-up) was 11.3 years at the cut-off date for the analysis (October 2020). No significant differences were detected univariately between patients in the combined B and C arm and those in arm A with respect to DFS (combined B and C vs. control arm: HR = 0.95, 95% CI 0.76–1.20, Wald’s P = 0.68, Fig. 1a) or OS (HR = 0.91, 95% CI 0.71–1.17, P = 0.47, Fig. 1b). Arms B and C were equally effective in terms of DFS and OS (Fig. 1c, d). Upon multivariate analysis with backwards model selection, a higher number of positive lymph nodes, greater tumour size (>2 cm) and postmenopausal status were identified as independent unfavourable prognostic factors for both DFS and OS (Supplementary Table 1).
At the time of the analysis, 236 patients (23.8%) had experienced a disease progression [83 in arm A (24.9%), 83 in arm B (25.1%) and 70 in arm C (21.5%)]. Information on the site of the first documented disease progression was available for 219 of the patients (92.8%). Sites of relapse per subtype and randomisation arm are presented in Table 1 and Supplementary Table 2, respectively. Most relapses occurred within 5 years post randomisation/treatment initiation (159/236 relapses; 67.4%) and included 20 locoregional (83.3% of total locoregional relapses) and 138 distant relapses (68.3% of total distant relapses) (Fig. 2). Two patients experienced a locoregional relapse later than 10 years after the completion of dose-dense sequential chemotherapy; one of them had triple-negative BC and presented with locoregional relapse in the residual breast and the other patient, with a luminal A tumour, had locoregional breast skin relapse. Sixteen patients (1.6%) experienced distant relapses in bones (n = 6 patients), liver only (n = 3), lung/pleura only (n = 2), lung and liver (n = 2), brain and bones (n = 1), brain only (n = 1 TNBC patient) and nodes only (n = 1) later than 10 years post the last day of chemotherapy. Seven patients had both locoregional and distant relapses. The number of relapses per subtype is presented in Supplementary Fig. 1.
Thirty-four patients (3.4%) developed secondary neoplasms during the 10-year follow-up (Fig. 3). Haematologic neoplasms after adjuvant treatment for BC were observed in five patients and included myelodysplastic syndrome (MDS), (1 patient; 6.2 years post chemotherapy discontinuation), non-Hodgkin lymphoma (1 patient; 2 years post discontinuation of chemotherapy) and acute myeloid leukaemias (AML) (3 patients). In two patients, AML was diagnosed 3.3 and 5.5 years post chemotherapy completion, respectively, while for one patient the date of AML diagnosis was not available. In addition, three patients developed in situ BC later than 6 years post chemotherapy completion and one additional patient was presented with in situ colorectal cancer 5.8 years after the completion of all planned cycles of chemotherapy.
The majority of deaths were caused by tumour disease (181/272 deaths; 66.5%). In the subset of patients who died without a prior disease progression (N = 75), four patients (0.4% of the total cohort) died of toxicity, which developed within 7–32 days post the last day of chemotherapy, while ten patients (1% of the total cohort) died from the development of secondary tumours (Table 2). In addition, 18 patients (1.8%) developed cardiac events [6 (1.8%) in arm A, 5 (1.5%) in arm B and 7 (2.1%) in arm C] that led to death (Supplementary Fig. 2).
Among patients with HER2-positive disease that received trastuzumab (N = 255), a total of 69 DFS events (27.1%) had been reported at the time of the analysis and 56 patients had died (22%). Fifty-four women, treated with trastuzumab for their HER2-positive tumours, experienced a disease progression; four of them (1.6% of the trastuzumab-treated population for HER2-positive disease) had locoregional relapses and 50 (19.6% of the trastuzumab-treated cohort) experienced distant metastases (Table 3). The sites of relapse per randomisation arm for HER2-positive, trastuzumab-treated patients are depicted in Supplementary Table 3. Thirty-eight HER2-positive, trastuzumab-treated patients died of their disease (14.9%), whereas three patients (1.2%) died of other tumours (one patient due to AML, one due to lung and one due to vulvar cancer). In three additional patients (1.2%) death was caused by infection/sepsis. Two HER2-positive patients (0.8%) died of cardiac events 7.2 and 12.2 years post trastuzumab completion, respectively, while five patients (2%) died of other causes. Causes of death were not available for the remaining five patients.
Even though patients treated with weekly taxanes seemed to have longer DFS as compared to those treated with E-T-CMF after 2 years since randomisation (Fig. 1e), no significant difference was found between the two treatment groups (arm A vs. the combined B and C arms) during the long-term follow-up (HR = 0.68, 95% CI 0.42–1.09, P = 0.11) in contrast with the results previously obtained after ~5 years of follow-up. Likewise, patients in arm A had similar OS to those in the combined B and C arms (HR = 0.66, 95% CI 0.39–1.11, Wald’s P = 0.12). In multivariate analysis, using backwards selection, the number of positive lymph nodes was the only significant prognostic factor for both DFS (overall P = 0.001) and OS (overall P = 0.002), whereas the hazard ratio of patients in the combined B and C arms was of the same direction and magnitude for progression (HR = 0.69, 95% CI 0.43–1.10, P = 0.13) and death (HR = 0.67, 95% CI 0.39–1.13, P = 0.13) as those obtained from univariate analysis.
Discussion
During recent decades, numerous studies have documented the clinical benefit from the addition of taxanes in the anthracycline-based adjuvant chemotherapy in BC. The NSABP B-28 Phase III trial demonstrated that the addition of paclitaxel to adjuvant treatment with doxorubicin and cyclophosphamide significantly prolongs DFS [7]. Similarly, the CALGB 9344 Phase III trial has shown that the addition of paclitaxel (175 mg/m2 every 21 days) to adjuvant treatment with doxorubicin and cyclophosphamide resulted in a 17 and 18% reduction of recurrence and death risk, respectively [9]. In addition, the Breast Cancer International Research Group (BCIRG) 001 Phase III trial, which compared adjuvant treatment with TAC (doxorubicin, cyclophosphamide, docetaxel) to FAC (doxorubicin, fluorouracil, cyclophosphamide) combination, showed that the taxane-containing regimen was associated with a 28% decrease in relapse risk [8]. In line with previous studies, a recent meta-analysis documented that the addition of taxane to a fixed anthracycline-based control regimen reduces BC mortality [6]. Although the role of taxanes in the treatment of EBC is well documented, more data are needed regarding the most effective and safe treatment regimen as well as the long-term efficacy.
In this study, we present the most recent analysis of the HE10/05 study after a long-term observational period (median follow-up of 13.3 years). Similar to the initial analysis after the first 5 years of follow-up [31], this updated analysis of the HE10/05 trial further supports our hypothesis that weekly administration of taxanes (docetaxel or paclitaxel), compared to biweekly administration, and in combination with epirubicin is a clinically valid option in patients with intermediate or high-risk operable BC showing a trend for improved clinical outcome. As previously noted, CMF has been currently replaced by “next-generation” regimens containing anthracyclines and taxanes. In addition, the introduction of neoadjuvant treatment regimens in intermediate and high-risk HER2-positive breast cancer has decreased the need for aggressive adjuvant treatment and has changed current clinical practice. Although the regimens studied above are considered obsolete these days, they remained clinically meaningful during previous decades. A key strength of this study is the long-term follow-up period. Long-term observation is a pivotal issue in clinical trials, since it allows the evaluation of late recurrences and side effects as well as the long-term benefit from the studied regimens [35]. Especially for BC, long-term observation is significant given that treatment-related harm may be clinically detected years later, with the most representative example being the side effects from radiotherapy and tamoxifen [36,37,38].
One of the most important findings of our study is that no statistically significant difference was observed between the control arm (E-T-CMF, biweekly administration of paclitaxel) and the combined B (E-CMF-wD, weekly docetaxel) and C (E-CMF-wT, weekly paclitaxel) arms in terms of DFS or OS. In most randomised trials, paclitaxel and docetaxel have been given every three weeks, however, alternative schedules may favourably affect the therapeutic ratio. In the present study, we compared the sequential administration of dose-dense paclitaxel after dose-dense epirubicin with the administration of either weekly docetaxel or paclitaxel after dose-dense epirubicin and intensified CMF. Our long-term analysis revealed no difference between the two dosing schedules in the entire cohort in terms of DFS or OS. In the CALBG 9741 Phase III study, an increase in DFS and OS rates by dose-dense dosing schedules of both anthracycline and taxane compared with 3-weekly schedules were reported [13]. Phase III studies evaluating the administration of taxanes in a dose-dense manner mostly used the 3-weekly administration schedule as the control group (PANTHER 3, GIM2 trial, UK TACT2, NSABP B-38, GONO-MIG, GAIN) [15,16,17,18,19,20]. These trials reported conflicting results regarding the differences in efficacy between different dosing schedules. However, the interstudy heterogeneity in the risk profile of the patients enrolled (number of positive lymph nodes, HR-positive population) and the dose administered might be responsible for this controversy. CALBG 9741, GIM2 and AGO III displayed a clinical benefit from the dose-dense administration of adjuvant chemotherapy, while in UK TACT2, GONO-MIG, NSABP B-38 and PANTHER 3 Phase III trials the positive effect of dose density on DFS and OS failed to reach statistical significance [15,16,17,18,19,20].
There was no difference observed between the docetaxel and paclitaxel treatment arms (arms B and C). Comparing docetaxel with paclitaxel, although the first appears to be more effective in the metastatic setting [39], here we report that the administration of weekly paclitaxel or weekly docetaxel after dose-dense epirubicin followed by intensified CMF is equally effective in terms of DFS and OS in the adjuvant setting. In line with our findings, the Eastern Cooperative Oncology Group (ECOG) E1199 trial, which was designed to compare the taxanes (paclitaxel versus docetaxel) and the dosing schedule of adjuvant treatment, has shown that, after a median follow-up of 12.1 years, although weekly paclitaxel and the every-3-week docetaxel were superior to the standard 3-week paclitaxel arm in terms of DFS and OS, no difference was detected between the two taxanes [40].
Another interesting finding of this study is that no significant difference was observed regarding DFS and OS between the arms A and B or C (E-T-CMF vs E-CMF-wD or E-CMF-wT) in the trastuzumab-treated population. In most trials, which have evaluated dose-intense treatment schedules, the majority of women did not receive the current standard of treatment with trastuzumab [13,14,15,16,17,18,19,20]. Therefore, it is difficult to evaluate the real clinical benefit provided by dose-intense chemotherapy in HER2-positive breast cancer patients. Indeed, this is one of the few trials evaluating dose-dense treatment regimens in conjunction with trastuzumab treatment. In the GIM2 trial, patients with BC were randomised to receive FEC (fluorouracil, epirubicin, cyclophosphamide followed by dose-dense or 3-weekly paclitaxel) [41]. After trastuzumab approval in 2006, HER2-positive patients with BC received additional treatment with trastuzumab. Lambertini et al. conducted an exploratory analysis in which they concluded that the clinical benefit of dose density is limited in HER2-positive patients who receive trastuzumab, despite the survival benefit observed in high-risk BC [41]. Before the introduction of trastuzumab, dose-dense chemotherapy offered significant benefits in HER2-positive BC patients [42]. In the trastuzumab-treated HER-positive patients, however, neither DFS (68.7 vs 72.3%) nor OS (84.9 vs 86.1%) did differ significantly between dose-dense and standard chemotherapy groups [41]. Consistently, a recent secondary analysis of the PANTHER Phase III trial demonstrated that the BC relapse-free survival was not significantly prolonged in patients receiving dose-dense chemotherapy and trastuzumab compared to standard chemotherapy and trastuzumab [43]. Moreover, the EBCTCG meta-analysis reported similar benefits from dose density among HER2-positive and HER2-negative patients, however, most patients were not treated with trastuzumab [6]. In addition, our results are compatible with the results from the final (after 11 years of follow-up) analysis of the HERceptin Adjuvant (HERA) trial, regarding DFS events after 1-year adjuvant trastuzumab (27.1% in the current study vs 29.7% in the HERA trial) [44].
Also, intriguing was the finding regarding the long-term incidence of secondary cancers in our cohort. Interestingly, thirty-four patients (3.4%) developed secondary neoplasms during the follow-up period. Haematologic neoplasms accounted for 0.5% of the cases (5/990) including one patient with MDS, one patient with non-Hodgkin lymphoma and three patients with AML. Overall, 0.4% of patients developed MDS/AML in our study which is consistent with the rate reported in previous studies and meta-analyses [16, 23]. Previous studies have reported an increased incidence of MDS/AML development in dose-dense regimens [16, 23]. Del Mastro et al. have reported two cases (0.4%; 2/496) of MDS/AML both occurring in the dose-dense regimen (q2EC-P) [16]. Citron et al. have also reported a 0.4% (2/495) rate of MDS/AML in the dose-dense concurrent treatment regimen of doxorubicin, cyclophosphamide and taxane [13]. Indeed, patients who receive standard cumulative doses of epirubicin and cyclophosphamide (≥ 720 and ≥ 6300 mg/m2, respectively) have an 8-year risk of AML/MDS of 0.37%, which rises up to 0.6% in dose-dense regimens [45]. Of note, dose-dense schemes require support with granulocyte colony-stimulating factor (G-CSF) which has been accused of a leukemogenic effect. Indeed, some studies have associated the administration of G-CSF with an almost doubling of the risk of AML/MDS [45].
Fatal cardiotoxicity, another serious side effect, was reported in 18 patients (1.8%) in the entire cohort [6 (1.8%) in arm A, 5 (1.5%) in arm B and 7 (2.1%) in arm C]. It has been reported that late development of cardiac dysfunction may occur after dose-dense adjuvant anthracycline and taxane-based chemotherapy for BC [46]. Most of the cardiac events are asymptomatic reductions in the left ventricle ejection fraction (LVEF) [47]. Cardiac events, including LVEF decline, heart failure and myocardial ischaemia, affect approximately 15% of patients receiving dose-dense chemotherapy. However, a statistically significant LVEF decline was reported not only in BC patients receiving dose-dense anthracycline compounds but also in patients receiving standard chemotherapy at 4-year follow-up, although the mean LVEF was significantly lower in the dose-dense subgroup at 6 years [15]. PANTHER trial did not report any differences in LVEF decline between dose-dense and standard chemotherapy groups among the HER2-positive patients.
Despite the very promising observations, we have to acknowledge some limitations of the current study. First, in HER2-positive patients, concurrent administration of trastuzumab with a taxane was not used since at the time of the study design there were not adequate data available regarding this strategy. Finally, more conclusive results may have been obtained if we had used the dose-dense doxorubicin and cyclophosphamide followed by the paclitaxel regimen, which is widely used today, as the control arm instead of E-T-CMF, especially with concurrent CMF.
Conclusions
Collectively, we report here the final long-term analysis of the HE10/05 Phase III clinical trial. DFS and OS were not significantly different between patients with BC receiving weekly taxane-containing regimens (docetaxel or paclitaxel) and the control arm at a median follow-up of 13.3 years. In the HER2-positive trastuzumab-treated population, no difference was observed between the control and the combined weekly taxane-containing experimental arm (combined B and C arm), despite the initial superiority of the weekly taxane regimen for DFS at 5 years of follow-up [31]. Although the treatment regimens studied are obsolete, we conclude that the combination of dose-dense adjuvant chemotherapy with one year of trastuzumab treatment is well-tolerated and safe.
Data availability
All data are available upon request.
References
Ferlay J, Colombet M, Soerjomataram I, Dyba T, Randi G, Bettio M, et al. Cancer incidence and mortality patterns in Europe: Estimates for 40 countries and 25 major cancers in 2018. Eur J Cancer. 2018;103:356–87.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA Cancer J Clin. 2021;71:7–33.
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49.
Fisher B, Brown AM, Dimitrov NV, Poisson R, Redmond C, Margolese RG, et al. Two months of doxorubicin-cyclophosphamide with and without interval reinduction therapy compared with 6 months of cyclophosphamide, methotrexate, and fluorouracil in positive-node breast cancer patients with tamoxifen-nonresponsive tumors: results from the National Surgical Adjuvant Breast and Bowel Project B-15. J Clin Oncol. 1990;8:1483–96.
Jones SE, Savin MA, Holmes FA, O’Shaughnessy JA, Blum JL, Vukelja S, et al. Phase III trial comparing doxorubicin plus cyclophosphamide with docetaxel plus cyclophosphamide as adjuvant therapy for operable breast cancer. J Clin Oncol. 2006;24:5381–7.
Peto R, Davies C, Godwin J, Gray R, Pan HC, Clarke M, et al. Comparisons between different polychemotherapy regimens for early breast cancer: meta-analyses of long-term outcome among 100,000 women in 123 randomised trials. Lancet. 2012;379:432–44.
Henderson IC, Berry DA, Demetri GD, Cirrincione CT, Goldstein LJ, Martino S, et al. Improved outcomes from adding sequential Paclitaxel but not from escalating Doxorubicin dose in an adjuvant chemotherapy regimen for patients with node-positive primary breast cancer. J Clin Oncol. 2003;21:976–83.
Martin M, Pienkowski T, Mackey J, Pawlicki M, Guastalla JP, Weaver C, et al. Adjuvant docetaxel for node-positive breast cancer. N. Engl J Med. 2005;352:2302–13.
Mamounas EP, Bryant J, Lembersky B, Fehrenbacher L, Sedlacek SM, Fisher B, et al. Paclitaxel after doxorubicin plus cyclophosphamide as adjuvant chemotherapy for node-positive breast cancer: results from NSABP B-28. J Clin Oncol. 2005;23:3686–96.
Jacquin JP, Jones S, Magné N, Chapelle C, Ellis P, Janni W, et al. Docetaxel-containing adjuvant chemotherapy in patients with early stage breast cancer. Consistency of effect independent of nodal and biomarker status: a meta-analysis of 14 randomized clinical trials. Breast Cancer Res Treat. 2012;134:903–13.
Hryniuk W, Levine MN. Analysis of dose intensity for adjuvant chemotherapy trials in stage II breast cancer. J Clin Oncol. 1986;4:1162–70.
Simon R, Norton L. The Norton-Simon hypothesis: designing more effective and less toxic chemotherapeutic regimens. Nat Clin Pract Oncol. 2006;3:406–7.
Citron ML, Berry DA, Cirrincione C, Hudis C, Winer EP, Gradishar WJ, et al. Randomized trial of dose-dense versus conventionally scheduled and sequential versus concurrent combination chemotherapy as postoperative adjuvant treatment of node-positive primary breast cancer: first report of Intergroup Trial C9741/Cancer and Leukemia Group B Trial 9741. J Clin Oncol. 2003;21:1431–9.
Möbus V, Jackisch C, Lück HJ, du Bois A, Thomssen C, Kuhn W, et al. Ten-year results of intense dose-dense chemotherapy show superior survival compared with a conventional schedule in high-risk primary breast cancer: final results of AGO phase III iddEPC trial. Ann Oncol: Off J Eur Soc Med Oncol. 2018;29:178–85.
Papakonstantinou A, Matikas A, Bengtsson NO, Malmström P, Hedayati E, Steger G, et al. Efficacy and safety of tailored and dose-dense adjuvant chemotherapy and trastuzumab for resected HER2-positive breast cancer: Results from the phase 3 PANTHER trial. Cancer. 2020;126:1175–82.
Del Mastro L, De Placido S, Bruzzi P, De Laurentiis M, Boni C, Cavazzini G, et al. Fluorouracil and dose-dense chemotherapy in adjuvant treatment of patients with early-stage breast cancer: an open-label, 2 × 2 factorial, randomised phase 3 trial. Lancet. 2015;385:1863–72.
Cameron D, Morden JP, Canney P, Velikova G, Coleman R, Bartlett J, et al. Accelerated versus standard epirubicin followed by cyclophosphamide, methotrexate, and fluorouracil or capecitabine as adjuvant therapy for breast cancer in the randomised UK TACT2 trial (CRUK/05/19): a multicentre, phase 3, open-label, randomised, controlled trial. Lancet Oncol. 2017;18:929–45.
Venturini M, Del Mastro L, Aitini E, Baldini E, Caroti C, Contu A, et al. Dose-dense adjuvant chemotherapy in early breast cancer patients: results from a randomized trial. J Natl Cancer Inst. 2005;97:1724–33.
Swain SM, Tang G, Geyer CE Jr, Rastogi P, Atkins JN, Donnellan PP, et al. Definitive results of a phase III adjuvant trial comparing three chemotherapy regimens in women with operable, node-positive breast cancer: the NSABP B-38 trial. J Clin Oncol. 2013;31:3197–204.
Möbus V, von Minckwitz G, Jackisch C, Lück HJ, Schneeweiss A, Tesch H, et al. Node-positive Study (GAIN): a phase III trial comparing two dose-dense regimens (iddEPC versus ddEC-PwX) in high-risk early breast cancer patients. Ann Oncol. 2017;28:1803–10.
(EBCTCG) EBCTCG. Increasing the dose intensity of chemotherapy by more frequent administration or sequential scheduling: a patient-level meta-analysis of 37 298 women with early breast cancer in 26 randomised trials. Lancet. 2019;393:1440–52.
Bonilla L, Ben-Aharon I, Vidal L, Gafter-Gvili A, Leibovici L, Stemmer SM. Dose-dense chemotherapy in nonmetastatic breast cancer: a systematic review and meta-analysis of randomized controlled trials. J Natl Cancer Inst. 2010;102:1845–54.
Petrelli F, Cabiddu M, Coinu A, Borgonovo K, Ghilardi M, Lonati V, et al. Adjuvant dose-dense chemotherapy in breast cancer: a systematic review and meta-analysis of randomized trials. Breast Cancer Res Treat. 2015;151:251–9.
Buzzoni R, Bonadonna G, Valagussa P, Zambetti M. Adjuvant chemotherapy with doxorubicin plus cyclophosphamide, methotrexate, and fluorouracil in the treatment of resectable breast cancer with more than three positive axillary nodes. J Clin Oncol. 1991;9:2134–40.
Perloff M, Norton L, Korzun AH, Wood WC, Carey RW, Gottlieb A, et al. Postsurgical adjuvant chemotherapy of stage II breast carcinoma with or without crossover to a non-cross-resistant regimen: a Cancer and Leukemia Group B study. J Clin Oncol. 1996;14:1589–98.
Shao N, Wang S, Yao C, Xu X, Zhang Y, Zhang Y, et al. Sequential versus concurrent anthracyclines and taxanes as adjuvant chemotherapy of early breast cancer: a meta-analysis of phase III randomized control trials. Breast. 2012;21:389–93.
Bonadonna G, Zambetti M, Valagussa P. Sequential or alternating doxorubicin and CMF regimens in breast cancer with more than three positive nodes. Ten-year results. J Am Med Assoc.1995;273:542–7.
Fountzilas G, Skarlos D, Dafni U, Gogas H, Briasoulis E, Pectasides D, et al. Postoperative dose-dense sequential chemotherapy with epirubicin, followed by CMF with or without paclitaxel, in patients with high-risk operable breast cancer: a randomized phase III study conducted by the Hellenic Cooperative Oncology Group. Ann Oncol. 2005;16:1762–71.
Gogas H, Dafni U, Karina M, Papadimitriou C, Batistatou A, Bobos M, et al. Postoperative dose-dense sequential versus concomitant administration of epirubicin and paclitaxel in patients with node-positive breast cancer: 5-year results of the Hellenic Cooperative Oncology Group HE 10/00 phase III Trial. Breast Cancer Res Treat. 2012;132:609–19.
Fountzilas G, Dafni U, Gogas H, Linardou H, Kalofonos HP, Briasoulis E, et al. Postoperative dose-dense sequential chemotherapy with epirubicin, paclitaxel and CMF in patients with high-risk breast cancer: safety analysis of the Hellenic Cooperative Oncology Group randomized phase III trial HE 10/00. Ann Oncol. 2008;19:853–60.
Fountzilas G, Dafni U, Papadimitriou C, Timotheadou E, Gogas H, Eleftheraki AG, et al. Dose-dense sequential adjuvant chemotherapy followed, as indicated, by trastuzumab for one year in patients with early breast cancer: first report at 5-year median follow-up of a Hellenic Cooperative Oncology Group randomized phase III trial. BMC Cancer. 2014;14:515.
Goldhirsch A, Glick JH, Gelber RD, Coates AS, Thürlimann B, Senn HJ. Meeting highlights: international expert consensus on the primary therapy of early breast cancer 2005. Ann Oncol. 2005;16:1569–83.
World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. Bulletin of the World Health Organization. 2001;79:373–4.
Hudis CA, Barlow WE, Costantino JP, Gray RJ, Pritchard KI, Chapman JA, et al. Proposal for standardized definitions for efficacy end points in adjuvant breast cancer trials: the STEEP system. J Clin Oncol. 2007;25:2127–32.
Cuzick J. Statistical controversies in clinical research: long-term follow-up of clinical trials in cancer. Ann Oncol. 2015;26:2363–6.
Darby SC, Ewertz M, McGale P, Bennet AM, Blom-Goldman U, Brønnum D, et al. Risk of ischemic heart disease in women after radiotherapy for breast cancer. N. Engl J Med. 2013;368:987–98.
van Leeuwen FE, Benraadt J, Coebergh JW, Kiemeney LA, Gimbrère CH, Otter R, et al. Risk of endometrial cancer after tamoxifen treatment of breast cancer. Lancet. 1994;343:448–52.
Early Breast Cancer Trialists' Collaborative Group. Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;365:1687–717.
Jones SE, Erban J, Overmoyer B, Budd GT, Hutchins L, Lower E, et al. Randomized phase III study of docetaxel compared with paclitaxel in metastatic breast cancer. J Clin Oncol. 2005;23:5542–51.
Sparano JA, Zhao F, Martino S, Ligibel JA, Perez EA, Saphner T, et al. Long-Term follow-up of the E1199 Phase III trial evaluating the role of taxane and schedule in operable breast cancer. J Clin Oncol. 2015;33:2353–60.
Lambertini M, Poggio F, Bruzzone M, Conte B, Bighin C, de Azambuja E, et al. Dose-dense adjuvant chemotherapy in HER2-positive early breast cancer patients before and after the introduction of trastuzumab: exploratory analysis of the GIM2 trial. Int J Cancer. 2020;147:160–9.
Del Mastro L, Bruzzi P, Nicolò G, Cavazzini G, Contu A, D’Amico M, et al. HER2 expression and efficacy of dose-dense anthracycline-containing adjuvant chemotherapy in breast cancer patients. Br J Cancer. 2005;93:7–14.
Foukakis T, Papakonstantinou A, Matikas A, Bengtsson N-O, Malmström P, Hedayati E, et al. Tailored dose-dense chemotherapy in combination with trastuzumab as adjuvant therapy for HER2-positive breast cancer: a secondary analysis of the phase III PANTHER trial. J Clin Oncol. 2019;37:553.
Cameron D, Piccart-Gebhart MJ, Gelber RD, Procter M, Goldhirsch A, de Azambuja E, et al. 11 years’ follow-up of trastuzumab after adjuvant chemotherapy in HER2-positive early breast cancer: final analysis of the HERceptin Adjuvant (HERA) trial. Lancet. 2017;389:1195–205.
Dong C, Chen L. Second malignancies after breast cancer: the impact of adjuvant therapy. Mol Clin Oncol. 2014;2:331–6.
Abu-Khalaf MM, Juneja V, Chung GG, DiGiovanna MP, Sipples R, McGurk M, et al. Long-term assessment of cardiac function after dose-dense and -intense sequential doxorubicin (A), paclitaxel (T), and cyclophosphamide (C) as adjuvant therapy for high risk breast cancer. Breast Cancer Res Treat. 2007;104:341–9.
Dent SF, Botros J, Rushton M, Aseyev O, Levine MN, Parulekar WR, et al. Anthracycline-induced cardiotoxicity in patients with early-stage breast cancer: the Canadian Cancer Trials Group (CCTG) MA.21 experience. Breast Cancer Res Treat. 2020;184:733–41.
Acknowledgements
The authors are grateful to all patients and their families for their trust and participation in the trial. The authors wish to thank Dimitra Katsala for monitoring the study, Maria Moschoni for coordinating the data management and Stella Dallidou for secretarial assistance. This work has been presented in part at the 2021 San Antonio Breast Cancer Symposium, Texas, US.
Funding
The study was supported by a Hellenic Cooperative Oncology Group internal research grant (HE TRANS_BR).
Author information
Authors and Affiliations
Contributions
Flora Zagouri: conceptualisation, resources and writing—original draft. Georgia-Angeliki Koliou: formal analysis and writing—original draft. Foteinos Dimitrakopoulos: resources and writing—original draft. Christos Papadimitriou: resources and writing—review and editing. Ioannis Binas: resources and writing—review and editing. Angelos Koutras: resources and writing—review and editing. Pavlos Papakostas: resources and writing—review and editing. Christos Markopoulos: resources and writing—review and editing. Vasileios Venizelos: resources and writing—review and editing. Grigorios Xepapadakis: resources and writing—review and editing. Angeliki Andrikopoulou: resources and writing—review and editing. Charisios Karanikiotis: resources and writing—review and editing. Amanda Psyrri: resources and writing—review and editing. Dimitrios Bafaloukos: resources and writing—review and editing. Paris Kosmidis: resources and writing—review and editing. Gerasimos Aravantinos: resources and writing—review and editing. Eleni Res: resources and writing—review and editing. Davide Mauri: resources and writing—review and editing. Anna Koumarianou: resources and writing—review and editing. Kalliopi Petraki: resources and writing—review and editing. Anna Tsipoura: resources and writing—review and editing. Dimitrios Pectasides: resources and writing—review and editing. Helen Gogas: resources and writing—review and editing. George Fountzilas: conceptualisation, supervision and writing—original draft.
Corresponding author
Ethics declarations
Competing interests
FZ: Honoraria and advisory role: AstraZeneca, Daiichi, Eli-Lilly, Merck, Novartis, Pfizer and Roche. CP: Honoraria and advisory role: Novartis, AstraZeneca, Genesis, MSD, Amgen, Pfizer, Merck and Roche. Research grants: BMS and Roche. AK: consulting or advisory role: Novartis, Roche, Genesis, AstraZeneca. Speaker’s bureau: GSK. Travel: Sanofi-Aventis, Astellas, Genesis, Amgen, BMS, Merck Serono. PP: advisory role: Roche, Merck, Genesis Pharmaceuticals, Honoraria: Roche, Merck. AP: consulting or advisory role: Amgen, Merck Serono, Roche, BMS, AstraZeneca, MSD, Honoraria: Amgen, Merck Serono, Roche, BMS, AstraZeneca, MSD. Research funds: BMS Kura. PK: Honoraria: Novartis, MSD, Pfizer. Travel: Pfizer, MSD, Genesis. GA: advisory boards: Novartis, BMS, Roche Hellas, Astra Zeneca, Sanofi, Amgen, Genesis Pharma, Merck, Pfizer. ER: consulting or advisory role: Novartis; Honoraria: Novartis; Travel: Genesis Pharmaceuticals, Pfizer, Roche, Bristol-Myers Squibb, Genekor. AK: Advisory Role: Genesis Pharma. Honoraria: Pfizer. Speaker’s bureau: Roche. Research funding: Merck. Travel: MSD. Educational grants: Novartis, Pfizer, Merck, Roche, BMS, MSD, Genesis, and Ipsen. DP: advisory role: Roche, MSD, Astellas. Honoraria: Roche, MSD, Astellas. HG: Advisory Role: Bristol-Myers Squibb, MSD Oncology, Amgen, Novartis, Roche, Pierre-Fabre, Honoraria: Bristol-Myers Squibb, MSD Oncology, Roche, Amgen, Novartis, research funding (institution): Bristol-Myers Squibb, Roche, MSD Oncology, Travel: Roche, Bristol-Myers Squibb. George Fountzilas: Advisory Board of Pfizer, Sanofi and Roche. Honoraria from AstraZeneca. Stock ownership: Genprex, Daiichi Sankyo, RFL Holdings, Formycon. The remaining authors declare no competing interests.
Ethics approval and consent to participate
All patients provided written informed consent before participating in the study. The clinical protocol was approved by the Institutional Review Boards in participating centres, by the National Organization for Medicines and by the National Ethics Committee and was registered in the Australian New Zealand Clinical Trials Registry (ACTRN12610000151033). The study was conducted in accordance with the ethical principles that have their origins in the Declaration of Helsinki.
Consent to publish
Not applicable.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41416_2022_1846_MOESM4_ESM.jpg
Swimmer plot showing the time to death caused by cardiac events. Each bar represents one patient in study who experienced a cardiac event that led to death. Bar lengths represent study follow-up time
Rights and permissions
About this article
Cite this article
Zagouri, F., Koliou, GA., Dimitrakopoulos, F. et al. Dose-dense sequential adjuvant chemotherapy in the trastuzumab era: final long-term results of the Hellenic Cooperative Oncology Group Phase III HE10/05 Trial. Br J Cancer 127, 695–703 (2022). https://doi.org/10.1038/s41416-022-01846-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-022-01846-y
- Springer Nature Limited