Abstract
This is the second part of a five-part series exploring the main ceramic materials used for the fabrication of all-ceramic restorations to aid clinicians in their selection. Feldspathic ceramics have been a desirable choice for over 200 years due to their favourable optical properties. However, the physical properties of the material have been its downfall, rendering it unsuitable in posterior regions. By going into further depth of feldspathic ceramic properties, clinicians will be able to gain a better understanding of their indications as they still have a place within modern dentistry.
Key points
-
Highlights the benefits of using feldspathic porcelain because of its optical properties.
-
Discusses the limitations of feldspathic porcelain based on its physical properties.
-
Explains the appropriate cementation technique for feldspathic ceramics.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
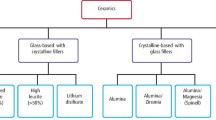
Despite porcelain being present for a thousand years, these feldspathic ceramics were first used within dentistry in 1723.1 Porcelain is a type of ceramic that has a composition including kaolin (Al2Si2O5[OH]4), quartz (SiO2)and feldspar (KaISi3O8-NaAlSi3O8-CaAl2Si2O8).2 Feldspathics are the most aesthetically pleasing yet weakest of the dental ceramic types; therefore, this material is mostly widely used as a veneering porcelain layered onto ceramic cores rather than monolithic restorations. The evolution of feldspathics has allowed the development of their optical properties and some improvement of the physical properties. In the second of our series on ceramics, feldspathic ceramics will be explored in greater depth to allow clinicians to obtain a better understanding according to research up to July 2020.
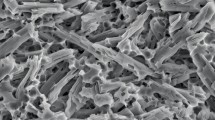
Microstructure
Conventional feldspathic porcelains, as mentioned in part one of the series, are of the glass-based ceramics. They are composed mainly of feldspar and also quartz, potash (K2O) and various metal oxides that impact the optical and physical properties, such as the coefficient of thermal expansion and melting temperature.1,3,4,5 Feldspar can be found naturally or produced synthetically to further improve aesthetics by removing all structural impurity.1,2 On heat treatment, feldspar readily forms leucite crystals which slightly increases the strength. Ceramics of majority glass phase have increased translucency, resulting in excellent aesthetics; however, the lack of crystalline fillers preludes to the brittle nature of the porcelain, making it undesirable.2 Therefore, leucite-reinforced feldspathic porcelain, containing a higher volume of leucite crystals (KAlSi3O6), was developed to help improve the physical properties. Along with the conventional feldspathic composition, premature microfine leucite crystals are dispersed into the matrix and crystalline fillers, such as alumina (Al2O3) and fluorapatite (Ca5[PO4]3F).1,2 Leucite-reinforced feldspathic porcelain is the most widely used feldspathic used within dentistry today and will be the main material referred to within this article.
Preparation design requirements
Porcelain veneers that are constructed via a layering technique can be fabricated very thinly, allowing for a highly conservative tooth preparation of 0.3-0.5 mm.6,7,8 Despite the ability to directly place veneers onto enamel, some enamel reduction is required to prevent the formation of an unnatural emergence profile and possible periodontal problems due to over-contouring. Porcelain veneers fabricated by computer-aided design and computer-aided manufacturing (CAD/CAM) are also suitable for preparations of 0.3 mm; however, for pressed veneers, a minimum of 0.75 mm of reduction is required.8
It is also important to consider the condition of the tooth/teeth to be veneered as a discoloured tooth would require a greater thickness of ceramic to mask the substrate, thus more tooth reduction would be needed.5 Various brands specify different tooth reduction and margin design requirements, so it is important to refer to these before tooth preparation.
Brands
There are various different feldspathic ceramics available (see Table 1) with different optical properties and allowing different processing techniques. Therefore, the choice may be decided on the restorative indication or the processing preference.
Optical properties
Traditionally, the metal oxides influenced the ceramic shade by acting as a pigment and on multiple firing cycles the shade would change as the metal oxide burnt out. Now, pre-sintered colourant crystals are used which do not vaporise during firing.1,5
Feldspathic porcelains may be used as the sole material for a restoration such as a veneer or inlay; however, their main use is as a veneering layer for ceramic frameworks such as zirconia or lithium disilicate to enhance the aesthetic result. The veneering layer may be placed directly on top of the coping, or a cut back technique can be used to reduce the coping thickness to allow for a larger veneering layer.
Feldspathics are known for their exceptional aesthetics resulting from the high degree of translucency and colour stability.6,9 The high glass content and fine leucite particles allow enhanced light transmission, hence its optical properties. The translucency allows for an aesthetically natural result as the existing tooth features can shine though.10 It is also important to note that the ceramic thickness can impact the light transmission and so its ability to mask discolouration of the tooth.7,11 Both the shade of the substrate and the ceramic will combine to determine the final restoration colour.11,12 Therefore, the restoration thickness needs to be carefully considered when planning treatment to ensure a successful outcome. It is advised that roughly 0.2-0.3 mm of space is required per shade change and up to 2 mm of porcelain may be required to mask underlying discolouration.8,13
Layered feldspathic porcelain involves the layering and firing of slurry several times, which enables multiple layers of different colours and customisation to be added (see Figure 1).6,8 The end result is a restoration with optical properties from both the surface and depth rather than simply the surface, as seen by restorations made of other materials.6 The problem with pressed and CAD/CAM restorations with superficial staining is that if any post-cementation adjustment is required or if tooth wear occurs then this can remove the aesthetic customisation.8
Even though the chemical properties and composition of feldspathics have a huge influence in the resulting aesthetic outcome, it is argued that the ability of the ceramist to manipulate the material has far more impact. Consequently, it is important to maintain clear communication with the ceramist in order to give them the necessary information to create their masterpiece.7
Physical properties
Feldspathic porcelain is known for its brittle nature and inherent weakness.3 During function, where tensile and shear stresses occur, microcracks can develop and they fracture.2 Traditional feldspathic porcelain has a far lower fracture toughness and flexural strength than any of the other dental ceramics, around 55-87 MPa. Whereas leucite-reinforced feldspathics have increased flexural strength by 17-19% to around 73-182 MPa and an increased fracture toughness of 3-64% compared to traditional feldspathic.14 The presence and size of leucite crystals has a huge impact on the physical strength of the material - increasing leucite crystal size and amount leads to an increase in fracture toughness.15 Nonetheless, when compared to other dental ceramics such as zirconia, the fracture toughness is still far weaker. The use of adhesive composite resin cement has been suggested to prevent crack propagation within porcelain and increase fracture resistance, which is enabled by the interlocking of the etched porcelain into the roughened tooth surface.7,9 This strengthening is much more evident in leucite-reinforced ceramics than in traditional feldspathic porcelain.16 Nonetheless, feldspathic ceramics are not suited for posterior restoration or areas where there is high masticatory exertion as the mechanical strength is not adequate.5 Studies have shown that there is a higher incidence of fractured leucite-reinforced feldspathic crowns that were placed on molars and premolars compared to those placed on anteriors.17 Furthermore, another study found that the feldspathic framework fracture rate after five years is 6.7% and the five year survival rate is 90.7%, the lowest compared to any other material.18 Despite functional loading reducing the fracture strength of feldspathic porcelain crowns, an in vitro study has determined them suitable for use anteriorly.19 Unless used as a veneering layer, feldspathic porcelain is not the ideal ceramic material of choice for fixed prostheses. Parafunctional habits increase the loading four to five times greater than functional loading and so, in these patients, feldspathic indirect restorations should not be provided unless some form of protection can be supplied, such as a soft occlusal splint.20
For layered restorations with a ceramic core and feldspathic layer, the overall strength of the restoration is dependent on the core-veneer bond. Furthermore, the ratio of ceramic core to veneering porcelain thickness influences the site of crack initiation as well as the aesthetics and so a good balance is required to allow the porcelain to be under compressive stresses and the core to be under tensile stress.13 In vitro studies have demonstrated that the core should be adequate to support a uniform layer of the porcelain veneer in the hope to prevent fractures of anterior crowns.21 It is the tensile stress that is the main cause for any observed chipping of the veneered layer.
The addition of leucite crystals also increases the coefficient of thermal expansion (CTE) which allows the veneering feldspathic to have a closer CTE to the ceramic coping, therefore reducing the risk of crack formation during restoration fabrication and hence potential chipping. Porcelain chipping has been one of the greatest causes of zirconia restoration failure and so is of a huge concern. The strength is also improved by preventing crack propagation as fracture energy is absorbed.14
Glazed feldspathic porcelain has the ability to erode the opposing enamel forty times more than a gold restoration and three times more than zirconia. In an in vitro study, the average amount of wear caused by feldspathic porcelain was 306.3 μm and 153.8 μm in the zirconia group.22 Therefore, it is recommended to ensure all restorative surfaces are polished.
Indications
Feldspathic ceramics are mainly chosen to fabricate veneers or as a veneering layer for indirect restorations. Feldspathic veneers are more suitable for cases where the aims of treatment are to modify the tooth shape and only a slight change in colour is required, allowing for minimal tooth reduction to take place.7 The optical properties of the material make it unsuitable for cases where masking of the underlying tooth colour is desired.5 Furthermore, as the other dental ceramics are continuously developing, their optical properties are also being modified. This has meant that their strength and enhanced aesthetics makes them more desirable to be used in the anterior region and the need for a layered restoration is far less, as instead, stains can provide beautiful results.
Other indications for the use of feldspathic ceramics include anterior crowns, inlays and onlays; some brands have also advertised the use of their material for posterior crowns.6,13,14 Due to other ceramics having far stronger physical properties, it is wise to stick to such materials rather than the use of feldspathic ceramics for posterior crowns. It is important to do a risk assessment on possible tensile and shear stress before prescribing feldspathic ceramics. Considerations include:
-
Deep overbites
-
Identifying areas where there will be large areas of unsupported porcelain
-
If bonding will occur on dentine or composite (flexible substrates), it is better to bond on mainly enamel
-
The location of the restoration and how distal it is.2
Cementation
Veneering feldspathic layers do not require cementation to the underlying core as the bond created is purely mechanical when the porcelain is fired.
For successful bonding of feldspathic veneers, the following recommendations should be considered in preparation design:
-
50% of the preparation should be within enamel
-
50% or more of the enamel on the tooth surface should be remaining
-
70% or more of the preparation margin should be within enamel.8
Feldspathic ceramics are cemented only with resin cements to increase the shear strength of the overall restoration and the material is hydrofluoric acid (HF) etchable.9,13 It is important to not air-abrade the inner surface of the restoration to increase surface roughness due to the risk of volume reduction and radical changes to the morphology.13 Therefore, in order to enable resin cementation of feldspathic restorations, the following protocol is generally advised:
-
1.
The application of HF etch for 2-2.5 minutes on the cleaned restoration fit surface. The HF concentration indicated should be checked according to the specific brand used; however, it is recognised that a concentration between 5-9% is adequate to achieve the highest shear bond strength. This should then be washed and air dried. This allows micromechanical retention to be formed on cement application
-
2.
Silane coupling agent is then applied to the fit surface for one minute and is subsequently air dried.
-
3.
Dual-, light- or self-cure, self-adhesive composite resins can then be applied, following the specific instructions to ensure appropriate polymerisation. For anterior restorations, there are resin cements available that have various shades to ensure the most aesthetically pleasing result is achieved.9,23
Conclusion
Even though the physical properties of feldspathic ceramics will never be comparable to the other dental ceramics available, their use is still invaluable thanks to their optical properties. When used correctly, feldspathic ceramics can provide successful results for the patient and so should not be dismissed as an option. The development of transitional feldspathic into the formation of leucite-reinforced feldspathic ceramics has allowed wider usage and it would be a sensible suggestion that it may be further developed to improve its usability. However, for now, case assessment is essential before choosing to use this material as otherwise restoration failure is inevitable.
References
Chu S J, Ahmad I. A historical perspective of synthetic ceramic and traditional feldspathic porcelain. Pract Proced Aesthet Dent 2005; 17: 593-598.
Babu P J, Alla R K, Alluri V R, Datla S R, Konakanchi A. Dental Ceramics: Part I - An Overview of Composition, Structure and Properties. Am J Mat Eng Technol 2015; 3: 13-18.
Santander S A, Pelaez-Vargas A, Escobar J S, Monteiro F J, Tamayo L F R. Ceramics for Dental Restorations - An Introduction. Dyna (Columbia) 2010; 77: 26-36.
Lugwisha E H J, Siafu S I. The Properties Of Feldspathic Dental Porcelain From Tanzanian Aluminosilicate Materials. Int J Develop Res 2014; 4: 2260-2265.
Madhavan A, Dr Anand. Methods of Strengthening Ceramics. J Pharm Sci Res 2015; 7: 873-877.
De Almeida B A.R T, de Oliveira K F, Caldas R A. Mechanical and optical properties of feldspathic ceramics and lithium disilicate: literature review. Braz J Dent 2020; 77: 1-4.
Federizzi L, Gomes E A, Báratro S S P, Baratto-Filho F, Bacchi A, Spazzin A O. Use of Feldspathic Porcelain Veneers to Improve Smile Harmony: A 3-Year Follow-up Report. Braz Dent J 2016; DOI: 10.1590/0103-6440201602453.
Mclaren E A, LeSage B. Feldspathic Veneers: what are their indications? Compend Contin Educ Dent 2011; 32: 44-49.
Strassler H E, Morgan R J. Cements for Today's All-Ceramic Materials. Inside Dentistry 2013. Available at https://www.aegisdentalnetwork.com/id/2013/12/cements-for-all-ceramic-materials (accessed January 2022).
Dentistry IQ. All veneers are not created equal. 2005. Available at https://www.dentistryiq.com/dentistry/restorative-cosmetic-and-whitening/article/16348210/all-veneers-are-not-created-equal (accessed July 2020).
Sari T, Ural C, Yüzbasioglu E, Duran I, Cengiz S, Kavut I. Colour match of a feldspathic ceramic CAD-CAM material for ultrathin laminate veneers as a function of substrate shade, restoration colour, and thickness. J Prosthet Dent 2018; 119: 455-460.
Barizon K T L. Relative translucency of ceramic systems for porcelain veneers. Iowa: University of Iowa, 2011. MS Thesis.
Mizrahi B. The anterior all-ceramic crown: a rationale for the choice of ceramic and cement. Br Dent J 2008; 205: 251-255.
Byeon S-M, Song J-J. Mechanical Properties and Microstructure of the Leucite-Reinforced Glass-Ceramics for Dental CAD/CAM. J Dent Hyg Sci 2018; 18: 42-49.
Drummond J L, King T J, Bapna M.S, Koperski R D. Mechanical property evaluation of pressable restorative ceramics. Dent Mater 2000; 16: 226-233.
Burke F J. Fracture resistance of teeth restored with dentin-bonded crowns constructed in a leucite-reinforced ceramic. Dent Mater 1999; 15: 359-362.
Sjögren G, Lantto R, Granberg A, Sundström B O, Tillberg A. Clinical examination of leucite-reinforced glass-ceramic crowns (Empress) in general practice: a retrospective study. Int J Prosthodont 1999; 12: 122-128.
Sailer I, Makarov N A, Thoma D S, Zwahlen M, Pjetursson B E. All-ceramic or metal-ceramic tooth-supported fixed dental prostheses (FDPs)? A systematic review of the survival and complication rates Part I: Single crowns (SCs). Dent Mater 2015; 31: 603-623.
Strub J R, Beschnidt S M. Fracture strength of 5 different all-ceramic crown systems. Int J Prosthodont 1998; 11: 602-609.
Torcato L B, Pellizzer E P, Verri F R, Falcon-Antenucci R M, de Souza Batista V E, de Toledo Piza Lopes L F. Effect of the parafunctional occlusal loading and crown height on stress distribution. Braz Dent J 2014; 25: 554-560.
Badran N, Kader S A, Alabbassy F. Effect of Incisal Porcelain Veneering Thickness on the Fracture Resistance of CAD/CAM Zirconia All-Ceramic Anterior Crowns. Int J Dent 2019; DOI: 10.1155/2019/6548519.
Ahmadzadeh A, Ashtiani A R H, Epakchi S et al. Comparison of the Effect of Feldspathic Porcelain and Zirconia on Natural Tooth Wear. J Islam Dent Assoc Iran 2014; 26: 170-176.
Santos Jr G C, Santos M J M C, Rizkalla A S. Adhesive Cementation of Etchable Ceramic Esthetic Restorations. J Can Dent Assoc 2009; 75: 379-384.
Acknowledgements
Fine Art Studio Dental Lab, Birmingham produced the ceramic work in Figure 1 and we thank them for all of their support.
Author information
Authors and Affiliations
Contributions
Mojgan Talibi: lead author; conceptualisation; drafting the manuscript; reviewing and editing of the manuscript to create the final version; photographing images and producing figures. Kiran Kaur: second author; conceptualisation; reviewing and editing of the manuscript to create the final manuscript and referencing. Hiten Parmar: supervisor and reviewing the manuscript.
Corresponding author
Ethics declarations
The authors declare no conflicts of interest.
Rights and permissions
About this article
Cite this article
Talibi, M., Kaur, K. & Parmar, H. Do you know your ceramics? Part 2: feldspathic ceramics. Br Dent J 232, 80–83 (2022). https://doi.org/10.1038/s41415-022-3874-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-022-3874-x
- Springer Nature Limited
This article is cited by
-
Ceramics overview
British Dental Journal (2022)
-
Preparation and mechanical properties of polymer infiltrated feldspar ceramic for dental restoration materials
Journal of Polymer Research (2022)