Abstract
Comparative data of fludarabine, cytarabine and amsacrine (FLAMSA) chemotherapy followed by busulfan (Bu)-based reduced-intensity conditioning (RIC) (FLAMSA-Bu) versus RIC regimens are lacking in patients with active relapsed/refractory (R/R) acute myeloid leukemia (AML) at the time of allogeneic hematopoietic stem cell transplantation (alloSCT). Here, we retrospectively analyzed outcomes after FLAMSA-Bu versus fludarabine/busulfan (FluBu2) conditioning in this patient population. A total of 476 patients fulfilled the inclusion criteria, of whom 257 received FluBu2 and 219 FLAMSA-Bu. Median follow-up was 41 months. Two-year non-relapse mortality (21%), graft-versus-host disease-free, relapse-free survival (24%) and chronic graft-versus-host disease (GVHD) (29%) were not statistically different between cohorts. FLAMSA-Bu was associated with lower 2-year relapse incidence (RI) (38 vs 49% after FluBu2, p = 0.004), and increased leukemia-free survival (LFS) (42 vs 29%, p = 0.001), overall survival (47 vs 39%, p = 0.008) and grades II-IV acute GVHD (36 vs 20%, p = 0.001). In the multivariate analysis, FLAMSA-Bu remained associated with lower RI (HR 0.69, p = 0.042), increased LFS (HR 0.74, p = 0.048) and a higher risk of acute GVHD (HR 2.06, p = 0.005). Notwithstanding the limitations inherent in this analysis, our data indicate that FLAMSA-Bu constitutes a tolerable conditioning strategy, resulting in a long-term benefit in a subset of patients reaching alloSCT with active disease.
Similar content being viewed by others
Introduction
Despite unprecedented developments in the therapeutic landscape of acute myeloid leukemia (AML), patients with relapsed or refractory (R/R) disease still face a dismal prognosis [1,2,3,4,5,6,7]. In this challenging clinical scenario, allogeneic stem cell transplantation (alloSCT) remains to this date the only treatment modality offering a potential long-term survival benefit [8,9,10]. Salvage cytotoxic chemotherapy, and more recently emerging targeted or immune-based therapies, can be employed to bridge patients to alloSCT in remission [3,4,5,6,7], but a substantial proportion of patients may only reach transplantation in the setting of uncontrolled active disease. In those R/R patients not candidates for a myeloablative alloSCT, suboptimal leukemic burden control after reduced-intensity conditioning (RIC) may hinder the generation of clinically meaningful graft-versus-leukemia (GVL) effects before overt disease relapse, resulting in poor transplant outcomes [11]. Thus, major efforts have been directed at the development of intensified RIC strategies that may offer superior cytoreductive properties in the absence of excessive added toxicity. In this respect, the use of sequential regimens comprising fludarabine, cytarabine and amsacrine (FLAMSA) followed by a conventional RIC incorporating total body irradiation (TBI) or busulphan (Bu) has experienced a widespread expansion based on promising results from uncontrolled studies in high-risk AML patients [12,13,14]. Yet, while this approach could be particularly appealing in patients with active disease at the time of alloSCT, comparative data of sequential FLAMSA-based versus standard RIC regimens are lacking in this specific population.
In this retrospective analysis, we compared transplant outcomes in a large series of patients with active R/R AML who underwent alloSCT after either sequential FLAMSA-Bu or FluBu2 RIC conditioning.
Material/Subjects and methods
Data collection and patients
This was a retrospective, multicentre, registry-based analysis performed by the Acute Leukemia Working Party (ALWP) of the European Society for Blood and Marrow Transplantation (EBMT). The EBMT is a nonprofit scientific society representing more than 600 transplant centers, mainly but not exclusively located in Europe. EBMT collaborating centers are required to report all stem cell transplantations and to provide follow-up data once a year. Audits are routinely undertaken to establish the accuracy of the data. All transplantation centers obtained patient written informed consent before data registration with the EBMT in accordance with the 1975 Declaration of Helsinki. The study was approved by the scientific board of the ALWP of the EBMT.
Adult patients (aged ≥18 years) with a diagnosis of primary refractory, first or second relapsed AML with active disease at the time of transplant and who had received a first alloSCT from a matched sibling donor (MSD) or a 10/10 matched unrelated donor (MUD) after fludarabine/busulfan RIC (FluBu2) or sequential FLAMSA followed by busulfan/cyclophosphamide RIC (FLAMSA-Bu) between 2005 and 2019, were included in the study. Patients who had received ex-vivo T-cell depletion were excluded.
Endpoints and definitions
The primary endpoint of the study was leukemia-free survival (LFS). The secondary endpoints were relapse incidence (RI), non-relapse mortality (NRM), overall survival (OS), acute graft-versus-host disease (aGVHD), chronic graft-versus-host disease (cGVHD) and graft-versus-host disease-free, relapse-free survival (GRFS). LFS was defined as the time to first documentation of active disease or death from any cause. Relapse incidence was defined as the time to first documentation of active disease. NRM was defined as time to death from any cause in the absence of prior documentation of active disease. OS was defined as the time to death from any cause. GRFS was defined as the time to grades III–IV aGVHD, extensive cGVHD, relapse, or death, whichever came first [15]. aGVHD and cGVHD were graded according to the modified Glucksberg criteria and the revised Seattle criteria, respectively [16, 17]. Neutrophil engraftment was defined as the achievement of an absolute neutrophil count ≥0.5 × 109/L for 3 consecutive days. The starting point for time-to-event analyses was the date of transplantation. Patients with no event were censored at the date of their last follow-up.
Primary refractory or relapsed patients with active disease at the time of transplantation were included in the study as reported by the participating centers, but details on prior therapy or leukemia burden at the time of alloSCT were not available in the registry. Cytogenetic risk stratification was based on data at diagnosis according to the Medical Research Council (MRC) classification [18]. The FLAMSA-based regimen consisted of fludarabine (Flu) 30 mg/m2, cytarabine 2 g/m2 and amsacrine 100 mg/m2 from days −12 to −9, followed after 3 days of rest by RIC with cyclophosphamide (Cy) and Bu 6.4 mg/kg (intravenous, i.v.) or 8 mg/kg (oral). Cy dosing was not available in the registry database. Of note, the FLAMSA-BU strategy typically includes the use of prophylactic donor lymphocyte infusions (DLI). Patients undergoing FluBu2 RIC received a median Flu dose of 150 mg/m2 and Bu 6.4 mg/kg (i.v.) or 8 mg/kg (oral).
Statistical analysis
Characteristics of the two study groups were compared using the Mann–Whitney U test for continuous variables and the Chi-square test for categorical variables. Median follow-up was calculated using the reverse Kaplan-Meier method. Probabilities of OS, LFS and GRFS were calculated using the Kaplan-Meier method. Cumulative incidence functions were used to estimate RI, NRM, aGVHD, and cGVHD rates in the setting of competing risks. To study aGVHD and cGVHD, both relapse and death were considered to be competing events. Univariate analyses were performed using the log-rank test for LFS, OS, and GRFS, and the Gray’s test for RI, NRM, aGVHD and cGVHD. A Cox proportional hazards regression model was constructed for each study endpoint. Those variables differing between the two cohorts or associated with at least one endpoint in the univariate analysis (p value < 0.05) were included in the multivariate models. Results were reported as the hazard ratio (HR) with the 95% confidence interval (CI). A random effect or frailty was introduced for each center into the models in order to account for center effects [19, 20]. A prespecified per protocol subanalysis in patients aged above 50 years was also performed. All tests were two-sided. The type-1 error rate was fixed at 0.05 for the determination of factors associated with time-to-event endpoints. The statistical analyses were conducted in R 4.1.0 (R Core Team 2020).
Results
Patient, disease and transplant characteristics
Characteristics according to conditioning regimen are summarized in Table 1. A total of 476 patients were included in the study, of whom 257 received FluBu2 and 219 FLAMSA-Bu conditioning. Bu was administered i.v. in the majority of patients (66% in the FluBu2 group and 89% in the FLAMSA-Bu group). The median age at the time of transplant was 59 years (range 18–76), and the median follow-up was 41 months. Patients in the FLAMSA-Bu group were more likely to harbor adverse-risk cytogenetics (38 vs 25%) and to have received in vivo T-cell depletion with antithymocyte globulin (ATG) (95 vs 75%). Conversely, a higher proportion of patients in the FluBu2 group had a Karnofsky performance status (KPS) score <90 (46 vs 37%). Cyclosporin/ mycophenolate (34%) and cyclosporin/methotrexate (28%) were the most frequently used GVHD prophylaxis regimens in the FluBu2 group, whereas the cyclosporin/mycophenolate combination was employed in a large majority (77%) of patients in the FLAMSA-Bu group. The distributions of donor type, secondary AML, and disease status at transplantation were comparable in the two groups. Data regarding preemptive DLI were only reported in 50% of the patients. Among patients with available data, only a minority received DLI prophylactically (14% after FluBu2 and 23% after FLAMSA-Bu).
Analysis of transplantation outcomes
The results of the univariate analysis are reported in Table 2, and the results of the multivariate analysis in Table 3.
Engraftment and complete remission
The cumulative incidence of neutrophil engraftment at 60 days was 97%. A complete remission (CR) after transplantation was achieved in 73% of the patients, without significant differences between conditioning groups.
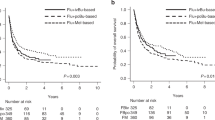
LFS and OS
The 2-year estimate of LFS was 29 and 42% in the FluBu2 and FLAMSA-Bu groups, respectively (p = 0.001). Similarly, FLAMSA-Bu was associated with increased 2-year OS in the univariate analysis (47 vs. 39% for FluBu2, p = 0.008) (Fig. 1 and Table 2). LFS and OS rates did not differ according to primary refractory or relapsed pretransplantation disease status. After multivariate adjustment, FLAMSA-Bu remained associated with improved LFS (HR: 0.74, 95% CI: 0.55–1, p = 0.048), but not OS (HR: 0.81, 95% CI: 0.59–1.11, p = 0.18). A KPS score ≥ 90 was also associated with higher LFS and OS in this analysis (Table 3).
RI and NRM
The 2-year cumulative RI was 49% after FluBu2 and 38% after FLAMSA-Bu (p = 0.004). There were no significant differences in terms of NRM between the two groups, with a 2-year estimate of 21% after either conditioning strategy (p = 0.76) (Fig. 1 and Table 2). These associations were maintained in the multivariate analysis (HR for RI: 0.69, 95% CI: 0.48–0.99, p = 0.042; HR for NRM: 0.93, 95% CI: 0.58–1.49, p = 0.76; FluBu2 as reference). Additionally, adverse-risk cytogenetics and transplant from an MSD were identified as predictors of increased RI, while a KPS score <90 and transplant from a 10/10 MUD were associated with a higher NRM in the multivariate models (Table 3). Rates of RI and NRM were similar in patients with primary refractory or relapsed disease at the time of alloSCT. Disease progression (57%) was the most frequent cause of death, followed by infections (17%), and GVHD (13%) (Table 4).
GVHD and GRFS
The risk of grades II-IV aGVHD was higher in the FLAMSA-Bu group, with an estimated cumulative incidence of 36% as compared to 20% after FluBu2 conditioning (p = 0.001). Similarly, the incidence of grades III-IV aGVHD was increased after FLAMSA-Bu (20 vs 10% after FluBu2; p = 0.003). On the other hand, the cumulative incidence of cGVHD did not significantly differ between the two groups (26% after FluBu2 vs 33% after FLAMSA-Bu, p = 0.09) (Table 2 and Supplementary material). No significant differences were noted in GRFS according to the conditioning regimen. The two-year GRFS was 21 and 28% after FluBu2 and FLAMSA-Bu, respectively (p = 0.17). In the multivariate analysis, FLAMSA-Bu was associated with a higher risk of grades II-IV aGVHD (HR: 2.06, 95% CI: 1.24–3.41, p = 0.005), but conditioning choice did not have an impact on cGVHD (HR: 1.07, 95% CI: 0.65–1.76, p = 0.78) or on GRFS (HR: 0.96, 95% CI: 0.73–1.27, p = 0.78) (Table 3).
Subgroup analysis of transplant outcomes in patients over the age of 50
Patients over 50 years of age represented 76% of the total study population. Two hundred and three patients received FluBu2 and 161 received FLAMSA-Bu in this patient subgroup. In the univariate analysis, FLAMSA-Bu remained associated with a lower 2-year RI (36 vs 46%, p = 0.013), improved 2-year LFS (39 vs 31%, p = 0.033) and increased rates of grades II-IV aGVHD (38 vs 20%, p = 0.001) as compared to FluBu2. No significant differences were observed at 2 years in terms of NRM, OS, GRFS or cGVHD between the two conditioning groups. In the multivariate analysis, FLAMSA-Bu only maintained a statistically significant association with an increased risk of grades II-IV aGVHD (HR: 2.07, 95% CI: 1.18–3.61, p = 0.011) (Supplementary material).
Discussion
After decades-long stagnation in the development of novel strategies to mitigate relapse risk after RIC, FLAMSA-based sequential regimens have been eagerly adopted by transplant centers worldwide based on results from single-arm studies showing encouraging antileukemic activity together with a favorable tolerability profile [12,13,14]. Recently, the FIGARO trial compared sequential FLAMSA-Bu versus fludarabine-based RIC in the first-ever randomized study of sequential conditioning [21]. Disappointingly, relapse risk did not differ between treatment arms, irrespective of pretransplantation measurable residual disease (MRD) status. Of note, however, is that 94% of the AML patients included in the study were in remission at the time of randomization, thus leaving open the question as to whether sequential conditioning may improve transplant outcomes in the setting of active R/R disease, where the addition of debulking chemotherapy before RIC could conceivably offer a differential impact.
In this context, our study represents the first comparative analysis to report evidence for a lower relapse risk after a sequential FLAMSA-based regimen versus standard RIC in patients with active R/R AML. Contrasting with the results of the FIGARO trial, augmented cytoreduction through sequential conditioning may have conferred a distinct advantage in our patient population, in which buying additional time for the emergence of GVL effects could prove particularly critical. In line with prior studies [22], a lower relapse incidence was also observed after MUD, suggesting more potent GVL effects as compared to transplant from MSD. Also notably, conditioning intensification with FLAMSA-Bu was associated with a significant long-term LFS benefit in the absence of increased NRM. In prior work from our group, FLAMSA followed by TBI-free RIC (over half of the patients having received FLAMSA-Bu) was associated with lower transplant-related mortality and higher OS as compared to MAC in younger patients with active R/R AML [23]. Taken together, these results are consistent with the assignment of FLAMSA-Bu to an intermediate transplant conditioning intensity category in a recent EBMT analysis, differentiating sequential regimens from standard RIC schemes [24].
Concerns on unacceptably high relapse rates have undermined the use of RIC alloSCT in patients with active R/R AML, and may serve as a rationale favoring the exhaustion of available salvage therapies before embarking on transplantation. Nonetheless, patients following this approach risk failing to reach transplant due to intercurrent complications or disease progression while on the quest to a disease response. Successive salvage therapies may also impose selective pressures resulting in clonal evolution with a potential deleterious impact on leukemia sensitivity to subsequent conditioning [13]. In a scenario where clinical decision-making is hampered by a scarce evidence base, this is to our knowledge the largest reported series of patients undergoing RIC alloSCT with active R/R AML. Although sequential FLAMSA-Bu was associated with improved outcomes in this analysis, a remarkable 2-year OS of 39% (as compared to 47% after FLAMSA-Bu) was observed after FluBu2 conditioning, and both platforms achieved long-term remissions in a non-negligible subset of patients. In fact, these results are not dissimilar to those reported in patients undergoing RIC alloSCT with pretransplantation MRD positivity in the BMT-CTN 0901 and FIGARO trials, being consistent with the presence of potent GVL effects after RIC [25, 26]. Ultimately, these data challenge the notion that RIC may only provide marginal clinical value in the setting of active disease, and emphasize the role of RIC alloSCT as possibly the best available therapy for patients not candidates for MAC. While the optimal timing of alloSCT in this patient population remains to be defined, our results suggest that alloSCT should be a prioritised treatment option.
A higher incidence of aGVHD, but not cGVHD, was observed after FLAMSA-Bu, despite a more frequent use of ATG-based T-cell depletion in patients receiving this regimen. The association between conditioning intensity and GVHD risk has been previously reported, although this finding has been disputed in other studies [27,28,29,30,31]. To what extent, if any, additional tissue damage induced by FLAMSA sequential regimens may prime the risk for subsequent aGVHD remains to be elucidated. Conversely, no relevant differences in GVHD rates were found in FIGARO. Of note, the use of prophylactic DLI constitutes an integral component of the original FLAMSA-based sequential conditioning strategy. The higher incidence of aGVHD observed after FLAMSA-Bu could be thus related to a more frequent DLI administration in this patient group. However, the evaluation of the potential impact of DLI on patient outcomes was hampered by missing data in our study, and multivariate analyses could not account for differences in the distribution of GVHD immunoprophylactic schemes between conditioning groups. This precluded the ability to isolate the effect of the conditioning chemotherapy itself on GVHD risk.
Considering the limitations inherent in any registry comparative analysis, caution should be exerted when interpreting the results of this study. Most notably, the reasons underlying conditioning regimen choice were unknown. In this respect, data on variables that may have influenced both transplant outcomes and allocation to a specific conditioning regimen, such as the hematopoietic cell transplantation-specific comorbidity index [32] (HCT-CI), the baseline leukemia burden (i.e. blast percentage) or the treatments received prior to transplant, were not available in the registry. Thus, the persistence of residual confounding after multivariate analysis cannot be completely dismissed. Additionally, the lack of data on therapy before alloSCT made not possible the identification of any patients having undergone suboptimal salvage treatment. This patient subgroup would be expected to show better outcomes after alloSCT than truly refractory patients, and could have biased transplant results to an uncertain extent.
In the absence of randomized studies, and notwithstanding the aforementioned limitations, our data provide robust evidence that sequential FLAMSA-Bu constitutes a tolerable conditioning strategy for patients reaching alloSCT with active disease, and suggest that this regimen may have superior antileukemic activity as compared to standard fludarabine-based RIC, resulting in a long-term benefit in a significant subset of patients in this very high-risk setting. Optimized use of prophylactic DLI [33], as well as the incorporation of post-transplant maintenance therapy [34,35,36], may further reduce relapse risk after FLAMSA-based conditioning and warrant evaluation in future studies.
References
Kurosawa S, Yamaguchi T, Miyawaki S, Uchida N, Sakura T, Kanamori H, et al. Prognostic factors and outcomes of adult patients with acute myeloid leukemia after first relapse. Haematologica. 2010;95:1857–64.
Ravandi F, Cortes J, Faderl S, O’Brien S, Garcia-Manero G, Verstovsek S, et al. Characteristics and outcome of patients with acute myeloid leukemia refractory to 1 cycle of high-dose cytarabine-based induction chemotherapy. Blood. 2010;116:5818–23.
Wattad M, Weber D, Döhner K, Krauter J, Gaidzik VI, Paschka P, et al. Impact of salvage regimens on response and overall survival in acute myeloid leukemia with induction failure. Leukemia. 2017;31:1306–13.
Cortes JE, Khaled S, Martinelli G, Perl AE, Ganguly S, Russell N, et al. Quizartinib versus salvage chemotherapy in relapsed or refractory FLT3-ITD acute myeloid leukaemia (QuANTUM-R): a multicentre, randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2019;20:984–97.
Perl AE, Martinelli G, Cortes JE, Neubauer A, Berman E, Paolini S, et al. Gilteritinib or chemotherapy for relapsed or refractory FLT3-mutated AML. N Engl J Med. 2019;381:1728–40.
Uy GL, Aldoss I, Foster MC, Sayre PH, Wieduwilt MJ, Advani AS, et al. Flotetuzumab as salvage immunotherapy for refractory acute myeloid leukemia. Blood. 2021;137:751–62.
Stahl M, Menghrajani K, Derkach A, Chan A, Xiao W, Glass J, et al. Clinical and molecular predictors of response and survival following venetoclax therapy in relapsed/refractory AML. Blood Adv. 2021;5:1552–64.
Duval M, Klein JP, He W, Cahn JY, Cairo M, Camitta BM, et al. Hematopoietic stem-cell transplantation for acute leukemia in relapse or primary induction failure. J Clin Oncol. 2010;28:3730–8.
Othus M, Appelbaum FR, Petersdorf SH, Kopecky KJ, Slovak M, Nevill T, et al. Fate of patients with newly diagnosed acute myeloid leukemia who fail primary induction therapy. Biol Blood Marrow Transpl. 2015;21:559–64.
Nagler A, Savani BN, Labopin M, Polge E, Passweg J, Finke J, et al. Outcomes after use of two standard ablative regimens in patients with refractory acute myeloid leukaemia: A retrospective, multicentre, registry analysis. Lancet Haematol. 2015;2:e384–92.
Loke J, Malladi R, Moss P, Craddock C. The role of allogeneic stem cell transplantation in the management of acute myeloid leukaemia: a triumph of hope and experience. Br J Haematol. 2020;188:129–46.
Schmid C, Schleuning M, Ledderose G, Tischer J, Kolb HJ. Sequential regimen of chemotherapy, reduced-intensity conditioning for allogeneic stem-cell transplantation, and prophylactic donor lymphocyte transfusion in high-risk acute myeloid leukemia and myelodysplastic syndrome. J Clin Oncol. 2005;23:5675–87.
Schmid C, Schleuning M, Schwerdtfeger R, Hertenstein B, Mischak-Weissinger E, Bunjes D, et al. Long-term survival in refractory acute myeloid leukemia after sequential treatment with chemotherapy and reduced-intensity conditioning for allogeneic stem cell transplantation. Blood. 2006;108:1092–9.
Malard F, Labopin M, Stuhler G, Bittenbring J, Ganser A, Tischer J, et al. Sequential intensified conditioning regimen allogeneic hematopoietic stem cell transplantation in adult patients with intermediate- or high-risk acute myeloid leukemia in complete remission: a study from the acute leukemia working party of the European Group for Blood and Marrow Transplantation. Biol Blood Marrow Transpl. 2017;23:278–84.
Ruggeri A, Labopin M, Ciceri F, Mohty M, Nagler A. Definition of GvHD-free, relapse-free survival for registry-based studies: An ALWP-EBMT analysis on patients with AML in remission. Bone Marrow Transpl. 2016;51:610–1.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows JTE. 1994 consensus conference on acute GVHD grading. Bone Marrow Transpl. 1995;15:825–8.
Lee SJ, Vogelsang G, Flowers MED. Chronic graft-versus-host disease. Biol Blood Marrow Transpl. 2003;9:215–33.
Grimwade D, Hills RK, Moorman AV, Walker H, Chatters S, Goldstone AH, et al. Refinement of cytogenetic classification in acute myeloid leukemia: determination of prognostic significance of rare recurring chromosomal abnormalities among 5876 younger adult patients treated in the United Kingdom Medical Research Council trials. Blood. 2010;116:354–66.
Hougaard P. Frailty models for survival data. Lifetime Data Anal. 1995;1:255–73.
Andersen P, Klein J, Zhang M. Testing for centre effects in multi-centre survival studies: a Monte Carlo comparison of fixed and random effects tests. Stat Med. 1999;18:1489–500.
Craddock C, Jackson A, Loke J, Siddique S, Hodgkinson A, Mason J, et al. Augmented reduced-intensity regimen does not improve postallogeneic transplant outcomes in acute myeloid leukemia. J Clin Oncol. 2021;39:768–78.
Ruggeri A, Battipaglia G, Labopin M, Ehninger G, Beelen D, Tischer J, et al. Unrelated donor versus matched sibling donor in adults with acute myeloid leukemia in first relapse: An ALWP-EBMT study. J Hematol Oncol. 2016;9:1–8.
Rodríguez-Arbolí E, Labopin M, Tischer J, Brecht A, Ganser A, Finke J, et al. FLAMSA-based reduced-intensity conditioning versus myeloablative conditioning in younger patients with relapsed/refractory acute myeloid leukemia with active disease at the time of allogeneic stem cell transplantation: an analysis from the acute leukemia. Biol Blood Marrow Transpl. 2020;26:2165–73.
Spyridonidis A, Labopin M, Savani BN, Niittyvuopio R, Blaise D, Craddock C, et al. Redefining and measuring transplant conditioning intensity in current era: a study in acute myeloid leukemia patients. Bone Marrow Transpl. 2020;55:1114–25.
Hourigan CS, Dillon LW, Gui G, Logan BR, Fei M, Ghannam J, et al. Impact of conditioning intensity of allogeneic transplantation for acute myeloid leukemia with genomic evidence of residual disease. J Clin Oncol. 2020;38:1273–83.
Craddock C, Nagra S, Peniket A, Brookes C, Buckley L, Nikolousis E, et al. Factors predicting long-term survival after T-cell depleted reduced intensity allogeneic stem cell transplantation for acute myeloid leukemia. Haematologica. 2010;95:989–95.
Aoudjhane M, Labopin M, Gorin NC, Shimoni A, Ruutu T, Kolb HJ, et al. Comparative outcome of reduced intensity and myeloablative conditioning regimen in HLA identical sibling allogeneic haematopoietic stem cell transplantation for patients older than 50 years of age with acute myeloblastic leukaemia: a retrospective survey. Leukemia. 2005;19:2304–12.
Luger SM, Ringdén O, Zhang M-J, Perez WS, Bishop MR, Bornhäuser M, et al. Similar outcomes using myeloablative versus reduced intensity allogeneic transplant. Bone Marrow Transpl. 2012;47:203–11.
Ringdén O, Labopin M, Ehninger G, Niederwieser D, Olsson R, Basara N, et al. Reduced intensity conditioning compared with myeloablative conditioning using unrelated donor transplants in patients with acute myeloid leukemia. J Clin Oncol. 2009;27:4570–7.
Couriel DR, Saliba RM, Giralt S, Khouri I, Andersson B, de Lima M, et al. Acute and chronic graft-versus-host disease after ablative and nonmyeloablative conditioning for allogeneic hematopoietic transplantation. Biol Blood Marrow Transpl. 2004;10:178–85.
Bornhäuser M, Kienast J, Trenschel R, Burchert A, Hegenbart U, Stadler M, et al. Reduced-intensity conditioning versus standard conditioning before allogeneic haemopoietic cell transplantation in patients with acute myeloid leukaemia in first complete remission: a prospective, open-label randomised phase 3 trial. Lancet Oncol. 2012;13:1035–44.
Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG, et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood. 2005;106:2912–9.
Schmid C, Labopin M, Schaap N, Veelken H, Schleuning M, Stadler M, et al. Prophylactic donor lymphocyte infusion after allogeneic stem cell transplantation in acute leukaemia—a matched pair analysis by the Acute Leukaemia Working Party of EBMT. Br J Haematol. 2019;184:782–7.
Burchert A, Bug G, Fritz LV, Finke J, Stelljes M, Röllig C, et al. Sorafenib maintenance after allogeneic hematopoietic stem cell transplantation for acute myeloid leukemia with FLT3-internal tandem duplication mutation (SORMAIN). J Clin Oncol. 2020;38:2993–3002.
Xuan L, Wang Y, Huang F, Fan Z, Xu Y, Sun J, et al. Sorafenib maintenance in patients with FLT3-ITD acute myeloid leukaemia undergoing allogeneic haematopoietic stem-cell transplantation: an open-label, multicentre, randomised phase 3 trial. Lancet Oncol. 2020;21:1201–12.
Bug G, Burchert A, Wagner EM, Kröger N, Berg T, Güller S, et al. Phase I/II study of the deacetylase inhibitor panobinostat after allogeneic stem cell transplantation in patients with high-risk MDS or AML (PANOBEST trial). Leukemia. 2017;31:2523–5.
Acknowledgements
ERA is a recipient of a Río Hortega academic clinical fellowship (CM19/00194) from the Instituto de Salud Carlos III, Spain. We thank all the patients included in the study and their families, as well as the investigators and data managers from the participating EBMT sites.
Author information
Authors and Affiliations
Contributions
ERA and MM conceived and designed the study. ML performed the statistical analyses. ERA wrote the draft version of the manuscript. BS, AS, AB, SG, EB, CS, AN, and MM reviewed the manuscript and contributed to its final version. ME, AB, IWB, AH, EF, JT, WB, SB, MV, CEB, HE, and FS were the principal investigators at the centers recruiting the highest number of patients for the study. All authors critically reviewed the manuscript and approved its final version.
Corresponding author
Ethics declarations
Competing interests
ERA and CS have received speaker fees from Eurocept Pharmaceuticals. The remaining authors declare no competing financial interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Rodríguez-Arbolí, E., Labopin, M., Eder, M. et al. Augmented FLAMSA-Bu versus FluBu2 reduced-intensity conditioning in patients with active relapsed/refractory acute myeloid leukemia: an EBMT analysis. Bone Marrow Transplant 57, 934–941 (2022). https://doi.org/10.1038/s41409-022-01611-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-022-01611-y
- Springer Nature Limited