Abstract
In order to identify cytomegalovirus (CMV)-seropositive patients who are at risk of developing CMV infection following first allogeneic hematopoietic cell transplantation (allo-HCT), we built up a scoring system based on patient/donor characteristics and transplantation modalities. To this end, 3690 consecutive patients were chronologically divided into a derivation cohort (2010–2012, n = 2180) and a validation cohort (2013–2014, n = 1490). Haploidentical donors were excluded. The incidence of first clinically significant CMV infection (CMV disease or CMV viremia leading to preemptive treatment) at 1, 3, and 6 months in the derivation cohort was 13.8%, 38.5%, and 39.6%, respectively. CMV-seropositive donor, unrelated donor (HLA matched 10/10 or HLA mismatched 9/10), myeloablative conditioning, total body irradiation, antithymocyte globulin, and mycophenolate mofetil significantly and independently affected the incidence of 3-month infection. These six factors were selected to build up the prognostic model. Four risk groups were defined: low, intermediate-low, intermediate-high, and high-risk categories, with a 3-month predicted incidence of first clinically significant CMV infection in the derivation cohort of 22.2%, 31.1%, 45.4%, and 56.9%, respectively. This score represents a framework for the evaluation of patients who are at risk of developing clinically significant CMV infection following allo-HCT. Prospective studies using this score may be of benefit in assessing the value of anti-CMV prophylaxis in well-defined patient cohorts.
Similar content being viewed by others
Introduction
Cytomegalovirus (CMV) infection is a major viral complication following allogeneic hematopoietic cell transplantation (allo-HCT) [1]. It is mostly observed in patients with a positive CMV serostatus and those with negative CMV serostatus receiving transplant from a positive CMV-serostatus donor [2]. Mainly occurring in the first 3 months, CMV infection is observed in over 60% of CMV-seropositive recipients, depending on the initial characteristics and posttransplant events [3]. CMV infection is associated with increased morbidity and mortality [4,5,6,7], especially in the case of CMV disease [8,9,10,11].
Preemptive therapy based on active monitoring of CMV in the blood long remained a standard of care [12,13,14]. The preemptive strategy improved the CMV-related outcome, mainly by decreasing the incidence of end-organ disease [15, 16], but did not fully prevent the emergence of breakthrough CMV disease. Until recently, no prophylactic strategy had been proven to be cost-effective, mainly because of the side effects of available drugs [17,18,19,20,21,22]. In a randomized phase 3 trial, prophylaxis with letermovir in CMV-seropositive adult allo-HCT patients was associated with a significantly lower risk of clinically significant CMV infection and improved survival, as compared to placebo, suggesting that universal prophylactic treatment could prove beneficial [23,24,25,26]. Many factors are known to be associated with a higher risk of developing CMV infection in CMV-seropositive patients, namely: CMV-seronegative donor, unrelated or HLA-mismatched donor, the use of immunosuppressive agents such as antithymocyte globulin (ATG) or calcineurin inhibitors, intensity and schedule of conditioning regimen, and development of GVHD [27, 28]. However, when considered separately, the predictive value of these factors is poor.
In order to estimate on an individual basis at the time of transplant the risk of developing clinically significant CMV infection, i.e., CMV disease or CMV viremia leading to preemptive treatment, we designed a scoring system considering and weighting the relevant baseline risk factors. This new score, based on large cohorts of CMV-seropositive patients, is designed to help evaluate the risk of CMV posttransplant infection in the era of primary CMV prophylaxis.
Material and methods
Study design and patients
Two distinct cohorts of patients were built up for the study, a derivation cohort and a validation cohort, both derived from the database of the Société Francophone de Greffe de Moelle et de Thérapie Cellulaire (SFGM-TC), with matching inclusion and exclusion criteria. All consecutive CMV-seropositive adult patients undergoing a first allo-HCT between January 2010 and December 2014 were retrospectively included in the study. They were divided into two consecutive cohorts according to the date of transplant: a derivation cohort from January 2010 to December 2012 and a validation cohort from January 2013 to December 2014. Haploidentical allo-HCT was excluded as few patients had received haploidentical transplant in France before 2014 mainly for nonmalignant disease.
The baseline parameters assessed included those of the recipient (age, sex, diagnosis, disease status), those of the donor (age, sex, CMV serostatus, type of donor), and transplantation modalities (stem cell source, intensity of the conditioning regimen, use of total body irradiation [TBI], ATG, GVHD prophylaxis). HLA-matched (10/10) and HLA-mismatched (9/10) donors were defined using high-resolution four-digit 10/10. Given that subhazard ratios (SHRs) were very similar in univariate analyses (Table 2 and Fig. S1, Supplementary Material), all unrelated donors were merged into one category named “unrelated” in multivariate analysis. Cord blood transplants were regarded as CMV seronegative [29]. Conditioning intensity was defined according to standard criteria [30]. Thus, TBI–cyclophosphamide, busulfan–cyclophosphamide, thiotepa–busulfan–fludarabine, fludarabine–busulfan ≥ 8 mg/kg days were considered myeloablative conditioning (MAC) regimens, whereas other conditioning regimens were classified as reduced intensity conditioning regimens. Only the first clinically significant CMV infection was considered [14, 31, 32].
This study was conducted according to the Declaration of Helsinki and was approved by the SFGM-TC scientific board. All patients gave consent for data recovery.
CMV monitoring and treatment
All patients were placed on a surveillance and treatment protocol based on the guidelines issued by SFGM-TC and periodically updated [33]. No CMV prophylactic treatment was given during the study period. According to risk factors and local policy, weekly or biweekly monitoring for CMV was performed from day 0 to at least day 100, using a real-time polymerase chain reaction. The threshold for the initiation of anti-CMV treatment followed local criteria based on the national SFGM-TC guidelines cited above. Treatment was mainly based on ganciclovir or foscarnet at recommended doses, according to the patient profile.
Statistical analysis
The median time from transplantation to last follow-up was estimated using the reverse Kaplan–Meier method [34]. Predictions of the first episode of clinically significant CMV infection were based on Fine–Gray models for survival, considering death as a competing event [35]. The cumulative incidence of the first episode of clinically significant CMV infection was estimated using the approach of Kalbfleisch and Prentice [36].
Firstly, candidate predictors were analyzed using bivariate Fine–Gray regression models; SHRs were reported as effect size with their 95% confidence intervals (CIs). For each continuous predictor (recipient and donor age), the log-linearity assumption was assessed using the restricted cubic spline functions [37]. Since we found no evidence of non-log-linear relationship, continuous predictors were introduced as linear terms in analyses. For each candidate predictor, we assessed proportional hazards assumption by plotting the Schoenfeld residuals against the rank of event time [38]. To develop the prognostic model, all candidate predictors were considered for entrance into the multivariable Fine–Gray regression model irrespective of the bivariate analyses. The full model was then simplified with a backward selection procedure by using a removal criterion of 0.05. The proportional hazards assumption for the prognostic index of the selected model was also assessed by plotting the Schoenfeld residuals against the rank of event time.
To avoid case deletion in univariate and multivariate analyses, missing data for candidate predictors (ranged from 0 to 4.7%) were imputed by simple imputation using the regression-switching approach [39], with the predictive mean-matching method for continuous variables and logistic regression (binary, ordinal, or multinomial) models for categorical variables.
The performance of the selected model was examined by assessing discrimination and calibration. Discrimination was assessed using the c-statistic adapted to the presence of competing risks [40], which indicates to what extent the model distinguishes between patients who will reactivate the CMV from those who will not. To address the overestimation issues in developing prognostic model [37], we performed an internal validation by using bootstrap resampling method (200 resamples) to correct the c-statistic for overoptimism and to calculate the shrinkage factor. Calibration (i.e., the predicted-to-observed incidence function agreement) was evaluated by comparing the predicted mean cumulative incidences (predicted from selected model) to the Kalbfleisch and Prentice cumulative incidences (observed) in four risk groups determined as the 16th, 50th, and 84th percentiles of the prognostic index’s distribution [41].
For clinical purpose, a point-scoring system was determined using regression coefficients of the selected Fine–Gray model; the number of points was determined by multiplying the regression coefficient by 10 and rounding to the nearest integer [42].
For the external validation, calibration and discrimination performances were assessed for continuous and discreet point score models in the validation dataset. The predicted survival probabilities calculated within the validation dataset were issued from the coefficient estimates (after applying the shrinkage factor) and the baseline survival estimate from the derivation dataset.
Statistical testing was performed at the two-tailed α level of 0.05. Data were analyzed using the SAS software package, release 9.4 (SAS Institute, Cary, NC, USA).
Results
Characteristics of the patients
Between January 2010 and December 2014, 10,484 patients received an allo-HCT in any of the SFGM-TC centers, 5343 (51.0%) of them being seropositive for CMV. A total of 1673 patients (16.0% of the entire population) were excluded from the analysis because of age < 18 years (n = 735; 7.0%), second allo-HCT (n = 395; 3.8%), haploidentical allo-HCT (n = 161; 1.5%), and missing data on survival status, CMV infection status or time of CMV infection (n = 382; 3.6%) (Fig. 1).
The analysis included the data from 3670 patients, chronologically divided according to the date of transplant into a derivation cohort (2010–2012, n = 2180) and a validation cohort (2013–2014, n = 1490). The baseline characteristics of the two cohorts are presented in Table 1. The mean age (standard derivation) was respectively 49.9 (13.2) and 51.2 (13.3) years, with 54.3 and 55.2% males. The median time from transplantation to last follow-up was 42.4 months (interquartile range [IQR], 26.6–53.3) in the derivation cohort, 18.8 months (11.8–25.7) in the validation cohort. Acute myeloid leukemia was the most frequent diagnosis (43.0 and 44.5%) and most patients were in complete remission (67.6 and 66.5%) in the derivation and validation cohorts, respectively. The donor was an identical sibling in 43.3 and 41.1% and unrelated in 56.7 and 58.9% of patients (including matched 10/10 in 27.5% and 32.8%, mismatched 9/10 in 18.3 and 17.7% and without precision in 10.9 and 8.3%) in the derivation and validation cohorts, respectively. Half of the donors were seronegative for CMV (52.5 and 46.8%). Source of stem cells was peripheral blood in 73.1% (70.4 and 77.8%), bone marrow in 18.1% (19.9 and 15.4%), and cord blood in 8.3% of transplantations (9.7 and 6.8%). A MAC was used in 35.7% of patients (35.7 and 35.6%), including TBI in 27.0% (32.2 and 19.4%) of the cases and in vivo T-cell depletion with ATG in 64.1% (60.0 and 73.7%). GVHD prophylaxis was mainly based on a combination of calcineurin inhibitor and methotrexate (40.6 and 38.4%) or mycophenolate mofetil (MMF) (38.5 and 38.0%). The other characteristics of each cohort are given in Table 1.
CMV infection
In the derivation cohort, 864 episodes of clinically significant CMV infection requiring first-line treatment occurred, within 1–180 days (median 36 days; IQR 26–49), leading to an incidence of 13.8% (95% CI, 12.4–15.2) at 1 month, 38.5% (95% CI, 36.5–40.5) at 3 months, and 39.7% (95% CI, 37.6–41.7) at 6 months. In the validation cohort, 625 first clinically significant CMV infection events occurred during the follow-up, within 1 day to 13.5 months (median 36 days; IQR 27–49), leading to an incidence of 15.5% (95% CI, 13.7–17.3) at 1 month, 41.1% (95% CI, 38.6–43.6) at 3 months, and 42.8% (95% CI, 40.2–45.3) at 6 months.
Prognostic model
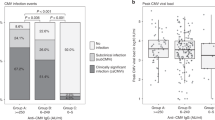
Univariate analyses of potential predictors of first CMV infection at transplant are presented in Table 2. Multivariable model screening (using backward-stepwise selection procedure including all potential predictors) selected six predictors of first clinically significant CMV infection: CMV serostatus of the donor, type of donor, intensity of the conditioning regimen, TBI, ATG, and MMF (Table 3). There was no deviation from proportional hazard assumptions for the prognostic index of selected prognostic continuous model. One-, three-, and six-month risk predictions computed by the prognostic continuous model (after shrinking the regression coefficients to improve the prediction in future patients) are available in Appendix. After correcting for overoptimism, the c-index of the prognostic continuous model was 0.610 (95% CI, 0.591–0.628). As shown in Table 4 and Fig. 2, the prediction of first clinically significant CMV infection incidence rate at 1, 3, and 6 months were close to the observed incidences, which indicated a good calibration of the prognostic continuous model. In the validation cohort, the c-index was 0.583 (95% CI, 0.560–0.606); after the shrinkage of the coefficients, the calibration remained satisfactory despite a slight underestimation observed (Table 4).
A point-scoring system was built from the prognostic continuous model (Table 3), the total number of points ranging from 0 to 20. The bounds of low, intermediate-low, intermediate-high, and high-risk categories were 0–4, 5–10, 11–14, and 15–20 respectively. At 3 months, the predicted incidence of first clinically significant CMV infection for the four categories in the derivation cohort was 22.2, 31.1, 45.4, and 56.9%. The predicted 1-, 3-, and 6-month incidence by classes of risk are reported in Table 5.
Discussion
Implementation of strategies to prevent CMV infection and disease after allo-HCT entails substantial commitment of resources, especially laboratory tests and drugs. Tailoring the strategy to the recipient risk profile appears to be justified. For this purpose, we studied in a large population of patients the correlation between baseline risk factors and the incidence of CMV infection.
Clinically significant CMV infection in our population of CMV-seropositive recipients of a first allo-HCT occurred mainly within the first 3 months post transplant, and the global incidence at 3 months in the total population was 39.6%, consistent with published data [43, 44]. Using multivariate analysis, we found six independent predictors of new-onset clinically significant CMV infection: CMV-seronegative donor, unrelated donor, MAC regimen, TBI, ATG, and MMF. These risk factors were previously described to be associated with CMV infection, but their respective prognostic importance had not yet been fully determined [45,46,47,48,49,50]. In transplant preparation, use of ATG (SHR 1.52; 1.27–1.81), TBI (SHR 1.35; 1.14–1.59), and MAC regimen (SHR 1.22; 1.05–1.43) was associated with a significant increase of the risk of CMV infection [51,52,53,54,55,56]. Regarding the GVHD prophylaxis, the use of MMF was associated in our study, as previously described [57], with a significant increase of the risk of CMV infection (SHR 1.34; 1.15–1.56). Contrary to many published data [58,59,60], cord blood transplant in our study was associated to CMV infection only in univariate, but not in multivariate analysis, most likely because of confounding factors correlated with this stem cell source (CMV-seronegative status of cord blood graft, unrelated transplant and frequent use of ATG and of MMF). To allow for the development of a risk score based on pretransplant characteristics of patient/donor and transplantation modalities, GVHD was deliberately excluded from the analysis.
The present study was based on a very large population of patients undergoing a first allo-HCT, with numbers of 2180 in the derivation cohort and 1490 in the validation cohort, which strengthen the validity of our results. George et al. previously described a three-class risk score for early CMV infection after allogeneic HCT. However, their study was based on 335 patients only, and more than half of them were CMV-seronegative recipients, whose risk and pathogenesis of CMV infection are distinct [50]. Our point-scoring system was calculated from the derivation cohort and confirmed in a validation cohort of CMV-seropositive patients with similar characteristics. It allowed the classification of patients into four risk groups, namely low, intermediate low, intermediate high, and high risk, with scores 0–4, 5–10, 11–14, and 15–20, respectively. These four classes were associated with clearly distinct predicted rates of infection at every point of time. In particular, the 3-month infection predicted risk was 22.2%, 31.1%, 45.4%, and 56.9%, respectively.
Our point-scoring system is very simple to implement in routine practice and will help clinicians to more accurately predict the probability of CMV infection in a CMV-seropositive patient who is not on anti-CMV prophylaxis. However, recent years have seen the more widespread use of letermovir prophylaxis following randomized trial evidence of clinical benefit. In this context, it should be noted that although the prevention of clinically significant CMV infection by letermovir was consistent in both high-risk and low-risk patients, the lower mortality seen in letermovir recipients was more pronounced in high-risk patients. This latter group was defined by the presence of one or more of the following criteria: HLA-mismatched related or unrelated donors, haploidentical donors, cord blood, ex vivo T-cell-depleted grafts, and GVHD requiring systemic immunosuppression. This high-risk cohort made up 31% of trial participants [24]. Many of these patients would have been classified as either high or very high risk by our score. Given the lesser benefit seen with the use of letermovir in the 69% of patients classified as low risk in the trial, and the greater discrimination of very low-risk patients allowed by the four subcategories in our study, this scoring system could potentially allow for the identification of a very low-risk group in whom there is no significant benefit to letermovir prophylaxis. However, this remains to be shown and, at present, our score offers a potential structure to allow this hypothesis to be formally tested in trials.
The avoidance of unnecessary prophylactic drugs and any associated drug interactions is clearly preferable in stem cell transplant recipients and letermovir is a substrate of OATP1B1/3 transporters and a moderate inhibitor of CYP3A. Possible future dynamic prophylactic strategies meriting investigation would include, for example, the prescribing of letermovir when patients develop GVHD requiring systemic corticosteroids, a complication which is known to greatly increase the risk of CMV infection [61, 62]. Obviously, these more nuanced approaches would need to be evaluated in prospective studies.
One of the potential limitations to the implementation of our score is the exclusion of haploidentical transplants. The inclusion of these patients was not possible because of the limited numbers and the heterogeneity of GVHD prophylaxis in those patients. Indeed, some patients had received ex vivo T-cell depletion plus ATG, while others received posttransplant cyclophosphamide with or without ATG. In addition, many of these patients received haploidentical transplants for nonmalignant diseases. Given the increasing use of this type of transplant, validation of our scoring system in this context would be desirable. Another limitation of our study is that all unrelated donors are four-digit HLA-matched (10/10) or mismatched (9/10). Therefore, a potential effect of another degree of HLA-matching could not be investigated. However, given that the SHR was as high as 2, such an effect would probably be insignificant.
In conclusion, this new score may help in evaluating the risk of clinically significant CMV infection in CMV-seropositive recipient who are being managed with a preemptive anti-CMV strategy. Although there is more use of letermovir, this remains a widely used strategy. In the coming years, the score could be used in prospective clinical trials to allow for the further refining of patient populations most likely to benefit from prophylactic anti-CMV treatment.
References
Ljungman P, Boeckh M, Hirsch HH, Josephson F, Lundgren J, Nichols G, et al. Definitions of cytomegalovirus infection and disease in transplant patients for use in clinical trials. Clin Infect Dis. 2017;64:87–91.
Ljungman P, Brand R, Einsele H, Frassoni F, Niederwieser D, Cordonnier C. Donor CMV serologic status and outcome of CMV-seropositive recipients after unrelated donor stem cell transplantation: an EBMT megafile analysis. Blood. 2003;102:4255–60.
Takenaka K, Gondo H, Tanimoto K, Nagafuji K, Fujisaki T, Mizuno S, et al. Increased incidence of cytomegalovirus (CMV) infection and CMV-associated disease after allogeneic bone marrow transplantation from unrelated donors. The Fukuoka Bone Marrow Transplantation Group. Bone Marrow Transplant. 1997;19:241–8.
Schmidt-Hieber M, Labopin M, Beelen D, Volin L, Ehninger G, Finke J, et al. CMV serostatus still has an important prognostic impact in de novo acute leukemia patients after allogeneic stem cell transplantation: a report from the Acute Leukemia Working Party of EBMT. Blood. 2013;122:3359–64.
Broers AE, van Der Holt R, van Esser JW, Gratama JW, Henzen-Logmans S, Kuenen-Boumeester V, et al. Increased transplant-related morbidity and mortality in CMV-seropositive patients despite highly effective prevention of CMV disease after allogeneic T-cell-depleted stem cell transplantation. Blood. 2000;95:2240–5.
Teira P, Battiwalla M, Ramanathan M, Barrett AJ, Ahn KW, Chen M, et al. Early cytomegalovirus reactivation remains associated with increased transplant-related mortality in the current era: a CIBMTR analysis. Blood. 2016;127:2427–38.
Ghobadi A, Milton DR, Gowda L, Rondon G, Chemaly RF, Hamdi A, et al. HLA-DP mismatch and CMV reactivation increase risk of aGVHD independently in recipients of allogeneic stem cell transplant. Curr Res Transl Med. 2019;67:51–5.
Hakimi Z, Ferchichi S, Aballea S, Odeyemi I, Toumi M, English M, et al. Burden of cytomegalovirus disease in allogeneic hematopoietic cell transplant recipients: a national, matched cohort study in an inpatient setting. Curr Res Transl Med. 2018;66:95–101.
Green ML, Leisenring W, Xie H, Mast TC, Cui Y, Sandmaier BM, et al. Cytomegalovirus viral load and mortality after haemopoietic stem cell transplantation in the era of pre-emptive therapy: a retrospective cohort study. Lancet Haematol. 2016;3:e119–27.
van Burik JA, Lawatsch EJ, DeFor TE, Weisdorf DJ. Cytomegalovirus enteritis among hematopoietic stem cell transplant recipients. Biol Blood Marrow Transplant. 2001;7:674–9.
Machado CM, Dulley FL, Boas LS, Castelli JB, Macedo MC, Silva RL, et al. CMV pneumonia in allogeneic BMT recipients undergoing early treatment of pre-emptive ganciclovir therapy. Bone Marrow Transplant. 2000;26:413–7.
Boeckh M, Ljungman P. How we treat cytomegalovirus in hematopoietic cell transplant recipients. Blood. 2009;113:5711–9.
Ljungman P. CMV infections after hematopoietic stem cell transplantation. Bone Marrow Transplant. 2008;42:S70–2.
Ljungman P, de la Camara R, Robin C, Crocchiolo R, Einsele H, Hill JA, et al. Guidelines for the management of cytomegalovirus infection in patients with haematological malignancies and after stem cell transplantation from the 2017 European Conference on Infections in Leukaemia (ECIL 7). Lancet Infect Dis. 2019;19:e260–72.
El Chaer F, Shah DP, Chemaly RF. How I treat resistant cytomegalovirus infection in hematopoietic cell transplantation recipients. Blood. 2016;128:2624–36.
Salzberger B, Bowden RA, Hackman RC, Davis C, Boeckh M. Neutropenia in allogeneic marrow transplant recipients receiving ganciclovir for prevention of cytomegalovirus disease: risk factors and outcome. Blood. 1997;90:2502–8.
Boeckh M, Nichols WG, Chemaly RF, Papanicolaou GA, Wingard JR, Xie H, et al. Valganciclovir for the prevention of complications of late cytomegalovirus infection after allogeneic hematopoietic cell transplantation: a randomized trial. Ann Intern Med. 2015;162:1–10.
Gagelmann N, Ljungman P, Styczynski J, Kröger N. Comparative efficacy and safety of different antiviral agents for cytomegalovirus prophylaxis in allogeneic hematopoietic cell transplantation: a systematic review and meta-analysis. Biol Blood Marrow Transplant. 2018;24:2101–9.
Marty FM, Winston DJ, Chemaly RF, Mullane KM, Shore TB, Papanicolaou GA, et al. A randomized, double-blind, placebo-controlled phase 3 trial of oral brincidofovir for cytomegalovirus prophylaxis in allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2019;25:369–81.
Marty FM, Winston DJ, Rowley SD, Vance E, Papanicolaou GA, Mullane KM, et al. CMX001 to prevent cytomegalovirus disease in hematopoietic-cell transplantation. N Engl J Med. 2013;369:1227–36.
Marty FM, Ljungman P, Papanicolaou GA, Winston DJ, Chemaly RF, Strasfeld L, et al. Maribavir prophylaxis for prevention of cytomegalovirus disease in recipients of allogeneic stem-cell transplants: a phase 3, double-blind, placebo-controlled, randomised trial. Lancet Infect Dis. 2011;11:284–92.
Winston DJ, Young J-AH, Pullarkat V, Papanicolaou GA, Vij R, Vance E, et al. Maribavir prophylaxis for prevention of cytomegalovirus infection in allogeneic stem cell transplant recipients: a multicenter, randomized, double-blind, placebo-controlled, dose-ranging study. Blood. 2008;111:5403–10.
Ljungman P, Schmitt M, Marty FM, et al. A mortality analysis of letermovir prophylaxis for cytomegalovirus (CMV) in CMV-seropositive recipients of allogeneic hematopoietic cell transplantation. Clin Infect Dis. 2020;70:1525–33. https://doi.org/10.1093/cid/ciz490
Marty FM, Ljungman P, Chemaly RF, Maertens J, Dadwal SS, Duarte RF, et al. Letermovir prophylaxis for cytomegalovirus in hematopoietic-cell transplantation. N Engl J Med. 2017;377:2433–44.
Chemaly RF, Ullmann AJ, Stoelben S, Richard MP, Bornhäuser M, Groth C, et al. Letermovir for cytomegalovirus prophylaxis in hematopoietic-cell transplantation. N Engl J Med. 2014;370:1781–9.
Foolad F, Aitken SL, Chemaly RF. Letermovir for the prevention of cytomegalovirus infection in adult cytomegalovirus-seropositive hematopoietic stem cell transplant recipients. Expert Rev Clin Pharm. 2018;11:931–41.
Emery V, Zuckerman M, Jackson G, Aitken C, Osman H, Pagliuca A, et al. Management of cytomegalovirus infection in haemopoietic stem cell transplantation. Br J Haematol. 2013;162:25–39.
Ljungman P, Brandan R. Factors influencing cytomegalovirus seropositivity in stem cell transplant patients and donors. Haematologica. 2007;92:1139–42.
Boland GJ, Vlieger AM, Ververs C, De, Gast GC. Evidence for transfer of cellular and humoral immunity to cytomegalovirus from donor to recipient in allogeneic bone marrow transplantation. Clin Exp Immunol. 1992;88:506–11.
Spyridonidis A, Labopin M, Savani BN, Niittyvuopio R, Blaise D, Craddock C, et al. Redefining and measuring transplant conditioning intensity in current era: a study in acute myeloid leukemia patients. Bone Marrow Transplant. 2020. https://doi.org/10.1038/s41409-020-0803-y.
Lilleri D, Gerna G, Furione M, Bernardo ME, Giorgiani G, Telli S, et al. Use of a DNAemia cut-off for monitoring human cytomegalovirus infection reduces the number of preemptively treated children and young adults receiving hematopoietic stem-cell transplantation compared with qualitative pp65 antigenemia. Blood. 2007;110:2757–60.
Gerna G, Lilleri D, Caldera D, Furione M, Zenone Bragotti L, Alessandrino EP. Validation of a DNAemia cutoff for preemptive therapy of cytomegalovirus infection in adult hematopoietic stem cell transplant recipients. Bone Marrow Transplant. 2008;41:873–9.
Brissot E, Alsuliman T, Gruson B, Hermet E, Tirefort Y, Yakoub-Agha I. et al. How to manage EBV reactivation and EBV-PTLD, CMV and human herpesvirus 6 reactivation and infection after allogeneic stem cell transplantation: A report of the SFGM-TC (update). Bull Cancer. 2017;104:S181–7.
Schemper M, Smith TL. A note on quantifying follow-up in studies of failure time. Control Clin Trials. 1996;17:343–6.
Gray RJ, Fine JP. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94:496–509.
Prentice RL, Kalbfleisch JD, Peterson AV, Flournoy N, Farewell VT, Breslow NE. The analysis of failure times in the presence of competing risks. Biometrics. 1978;34:541–54.
Harrell FE, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15:361–87.
Schoenfeld D. Partial residuals for the proportional hazards regression model. Biometrika. 1982;69:239–41.
Buuren S, van, Groothuis-Oudshoorn K. mice: multivariate imputation by chained equations in R. J Stat Softw. 2011;45:1–67.
Wolbers M, Koller MT, Witteman JCM, Steyerberg EW. Prognostic models with competing risks: methods and application to coronary risk prediction. Epidemiology. 2009;20:555–61.
Royston P, Moons KGM, Altman DG, Vergouwe Y. Prognosis and prognostic research: developing a prognostic model. BMJ. 2009;338:b604.
Austin PC, Lee DS, D’Agostino RB, Fine JP. Developing points-based risk-scoring systems in the presence of competing risks. Stat Med. 2016;35:4056–72.
Rowe J, Grim SA, Peace D, Lai C, Sweiss K, Layden JE, et al. The significance of cytomegalovirus viremia at day 100 or more following allogeneic hematopoietic stem cell transplantation. Clin Transplant. 2013;27:510–6.
Ozdemir E, Saliba RM, Champlin RE, Couriel DR, Giralt SA, de Lima M, et al. Risk factors associated with late cytomegalovirus reactivation after allogeneic stem cell transplantation for hematological malignancies. Bone Marrow Transplant. 2007;40:125–36.
Ljungman P, Brand R, Hoek J, de la Camara R, Cordonnier C, Einsele H, et al. Donor cytomegalovirus status influences the outcome of allogeneic stem cell transplant: a study by the European group for blood and marrow transplantation. Clin Infect Dis. 2014;59:473–81.
Ugarte-Torres A, Hoegh-Petersen M, Liu Y, Zhou F, Williamson TS, Quinlan D, et al. Donor serostatus has an impact on cytomegalovirus-specific immunity, cytomegaloviral disease incidence, and survival in seropositive hematopoietic cell transplant recipients. Biol Blood Marrow Transplant. 2011;17:574–85.
Junghanss C, Storb R, Maris MB, Carter RA, Sandmaier BM, Maloney DG, et al. Impact of unrelated donor status on the incidence and outcome of cytomegalovirus infections after non-myeloablative allogeneic stem cell transplantation. Br J Haematol. 2003;123:662–70.
Goldsmith SR, Slade M, DiPersio JF, Westervelt P, Lawrence SJ, Uy GL, et al. Cytomegalovirus viremia, disease, and impact on relapse in T-cell replete peripheral blood haploidentical hematopoietic cell transplantation with post-transplant cyclophosphamide. Haematologica. 2016;101:e465–8.
Servais S, Dumontier N, Biard L, Schnepf N, Resche-Rigon M, Peffault de Latour R, et al. Response to antiviral therapy in haematopoietic stem cell transplant recipients with cytomegalovirus (CMV) reactivation according to the donor CMV serological status. Clin Microbiol Infect. 2016;22:289.e1–7.
George B, Kerridge IH, Gilroy N, Huang G, Hertzberg MS, Bradstock KF, et al. A risk score for early cytomegalovirus reactivation after allogeneic stem cell transplantation identifies low-, intermediate-, and high-risk groups: reactivation risk is increased by graft-versus-host disease only in the intermediate-risk group. Transpl Infect Dis. 2012;14:141–8.
Kanda Y, Mineishi S, Nakai K, Saito T, Tanosaki R, Takaue Y. Frequent detection of rising cytomegalovirus antigenemia after allogeneic stem cell transplantation following a regimen containing antithymocyte globulin. Blood. 2001;97:3676–7.
Meijer E, Dekker AW, Verdonck LF. Influence of antithymocyte globulin dose on outcome in cytomegalovirus-seropositive recipients of partially T cell-depleted stem cell grafts from matched-unrelated donors. Br J Haematol. 2003;121:473–6.
Cohen L, Yeshurun M, Shpilberg O, Ram R. Risk factors and prognostic scale for cytomegalovirus (CMV) infection in CMV-seropositive patients after allogeneic hematopoietic cell transplantation. Transpl Infect Dis. 2015;17:510–7.
Nakamae H, Kirby KA, Sandmaier BM, Norasetthada L, Maloney DG, Maris MB, et al. Effect of conditioning regimen intensity on CMV infection in allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2009;15:694–703.
Kalpoe JS, van der Heiden PLJ, Vaessen N, Claas ECJ, Barge RM, Kroes ACM. Comparable incidence and severity of cytomegalovirus infections following T cell-depleted allogeneic stem cell transplantation preceded by reduced intensity or myeloablative conditioning. Bone Marrow Transplant. 2007;40:137–43.
Junghanss C, Boeckh M, Carter RA, Sandmaier BM, Maris MB, Maloney DG, et al. Incidence and outcome of cytomegalovirus infections following nonmyeloablative compared with myeloablative allogeneic stem cell transplantation, a matched control study. Blood. 2002;99:1978–85.
Hambach L, Stadler M, Dammann E, Ganser A, Hertenstein B. Increased risk of complicated CMV infection with the use of mycophenolate mofetil in allogeneic stem cell transplantation. Bone Marrow Transplant. 2002;29:903–6.
Walker CM, van Burik J-AH, De For TE, Weisdorf DJ. Cytomegalovirus infection after allogeneic transplantation: comparison of cord blood with peripheral blood and marrow graft sources. Biol Blood Marrow Transplant. 2007;13:1106–15.
Sauter C, Abboud M, Jia X, Heller G, Gonzales A-M, Lubin M, et al. Serious infection risk and immune recovery after double-unit cord blood transplantation without antithymocyte globulin. Biol Blood Marrow Transplant. 2011;17:1460–71.
Mikulska M, Raiola AM, Bruzzi P, Varaldo R, Annunziata S, Lamparelli T, et al. CMV infection after transplant from cord blood compared to other alternative donors: the importance of donor-negative CMV serostatus. Biol Blood Marrow Transplant. 2012;18:92–9.
Melendez-Munoz R, Marchalik R, Jerussi T, Dimitrova D, Nussenblatt V, Beri A, et al. Cytomegalovirus infection incidence and risk factors across diverse hematopoietic cell transplantation platforms using a standardized monitoring and treatment approach: a comprehensive evaluation from a single institution. Biol Blood Marrow Transplant. 2019;25:577–86.
Ljungman P, Perez-Bercoff L, Jonsson J, Avetisyan G, Sparrelid E, Aschan J, et al. Risk factors for the development of cytomegalovirus disease after allogeneic stem cell transplantation. Haematologica. 2006;91:78–83.
Acknowledgements
The authors would like to thank Nicole Raus, the SFGM-TC data manager. The authors wish to acknowledge all our medical teams for their dedication and involvement in daily patient care. A special thanks to Dr. Martine Lenoble for her help in writing and proofreading this article.
Funding
This study was supported in part by a research grant from Biotest.
Author information
Authors and Affiliations
Contributions
DB, ED, AD, and IY-A designed the study, reviewed the data, analyzed results, and made the figures. All authors wrote and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
IY-A received honorarium from MSD and Biotest, both are selling anti-CMV drugs. The other authors have no conflicts of interest to declare.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Beauvais, D., Drumez, E., Blaise, D. et al. Scoring system for clinically significant CMV infection in seropositive recipients following allogenic hematopoietic cell transplant: an SFGM-TC study. Bone Marrow Transplant 56, 1305–1315 (2021). https://doi.org/10.1038/s41409-020-01178-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-020-01178-6
- Springer Nature Limited