Abstract
Treatment of relapsed/refractory acute lymphoblastic leukemia (RR-ALL) remains a clinical challenge with generally dismal prognosis. Allogeneic stem-cell transplantation using sequential conditioning (“FLAMSA”-like) has shown promising results in relapsed/refractory acute myeloid leukemia, but little is known about its efficacy in RR-ALL. We identified 115 patients (19–66 years) with relapsed (74%) or primary-refractory (26%) ALL allografted from matched related (31%), matched unrelated (58%), or haploidentical donor (11%). Median follow-up was 37 (13–111) months. At day 100, cumulative incidences of grade II–IV/III–IV acute graft-versus-host-disease (GVHD) were 30% and 17%, respectively. Two-year cumulative incidence of chronic GVHD was 25% with 11% extensive cases. Two-year relapse incidence (RI) was 45%, non-relapse mortality was 41%. Two-year leukemia free survival (LFS) was 14%, overall survival (OS) 17%, and GVHD relapse-free survival (GRFS) was 14%. In multivariable analysis, Karnofsky score <90 negatively affected RI, LFS, OS, and GRFS. Conditioning with chemotherapy alone, compared with total body irradiation (TBI) negatively affected RI (HR = 3.3; p = 0.008), LFS (HR = 1.94; p = 0.03), and OS (HR = 2.0; p = 0.03). These patients still face extremely poor outcomes, highlighting the importance of incorporating novel therapies (e.g., BITE antibodies, inotuzumab, CAR-T cells). Nevertheless, patients with RR-T-cell ALL remain with an unmet treatment need, for which TBI-based sequential conditioning could be one of few available options.
Similar content being viewed by others
Introduction
Relapsed/refractory ALL (RR-ALL) is associated with a dismal prognosis, with 5-year overall survival (OS) from first relapse of only 10% [1,2,3,4]. Despite recent advances in upfront ALL therapies demonstrating up to 85–90% complete remission (CR) rates with improved OS [5, 6], at least one-third of standard-risk and two-thirds of high-risk patients eventually relapse, posing a serious challenge. CR rates after the first relapse drop drastically to 30–44%, and even further to 20–25% after the second relapse [3, 7, 8]. While new treatment modalities such as CAR-T cells appear to offer unprecedented CR rates in heavily treated ALL patients, data suggest that such responses are not very durable in some patients [9]. Allogeneic stem-cell transplant (allo-SCT) remains the only curative approach for RR-ALL patients who achieve CR, but <50% of patients make it to transplant, with some reported rates as low as 10–30% [1, 2, 10, 11].
Sequential conditioning-based allo-SCT has long been established as an effective therapy approach for high-risk and relapsed refractory AML [12,13,14,15,16]. While some studies have looked into sequential conditioning in ALL patients [17], very few data are currently available, and little is known about its safety and efficacy in RR-ALL. The purpose of the present study is therefore to assess the outcomes of RR-ALL patients undergoing allo-SCT using sequential conditioning. Since most transplants in this setting currently include total body irradiation (TBI) due to its established advantages, the study aims at specifically comparing TBI-based regimens to standard chemotherapy [18].
Materials and methods
Study design and data collection
This was a retrospective, registry-based, multicenter analysis. Data were provided and approved by the EBMT Acute Leukemia Working Party. The EBMT is a voluntary collaborating working group of more than 600 transplant centers that are required to report all consecutive stem-cell transplantations and follow-up once a year, with regularly performed audits to determine the accuracy of the data. Since the 1st of January 2003, all transplantation centers have been required to obtain written informed consent prior to data registration with the EBMT, as per the Declaration of Helsinki of 1975.
Eligibility criteria for this analysis included adult patients (those aged >18 years) with primary refractory or relapsed ALL who received a first allo-SCT between 2000 and 2017 using sequential conditioning from an HLA-matched related, unrelated, or haploidentical donor with bone marrow or peripheral blood stem cells, with no ex-vivo stem-cell manipulation. Patients who received cord blood or mismatched stem cells were excluded.
Variables collected included recipient and donor age and gender, date of diagnosis, previous auto-transplants, disease status, and Karnofsky score at the time of transplant. Transplant-related factors included date, conditioning regimen, in vivo T-cell depletion, donor type, and patient and donor cytomegalovirus (CMV) status.
Definitions
Sequential conditioning was defined as any regimen that combines a short, intensive course of salvage chemotherapy to decrease leukemia cell burden followed by transplant conditioning [19]. Myeloablative conditioning (MAC) was defined as a regimen containing either TBI with a dose equal or greater than 8 Gy, a total dose of oral busulfan (Bu) greater than 8 mg/kg, or a total dose of intravenous Bu greater than 6.4 mg/kg. All other regimens were defined as reduced intensity conditioning (RIC) [20]. Diagnosis and grading of acute [21] and chronic GVHD [22] were performed by transplant centers using standard criteria. High-resolution HLA allele typing at loci A, B, C, DRB1, and DQ was retrieved from the EBMT registry for both the patient and the donor.
Endpoints
Endpoints included leukemia free survival (LFS), OS, non-relapse mortality (NRM), relapse incidence (RI), acute and chronic GVHD, and GVHD and relapse-free survival (GRFS), with all outcomes measured from the time of allo-SCT. LFS was defined as survival without leukemia relapse or progression, with patients censored at the time of last contact. OS was defined as the time until death from any cause occurred. NRM was defined as being alive until death with no previous leukemia relapse. GRFS was defined as being alive with neither grades 3–4 acute GVHD, extensive chronic GVHD, nor relapse [23]. Surviving patients were censored at the time of last contact.
Statistical analysis
The Kaplan–Meier method was used to calculate the probabilities of OS and LFS. Cumulative incidence functions were used to estimate RI and NRM in a competing risk setting. Death and relapse were considered as competing events for acute and chronic GVHD.
Patient, disease, and transplant-related characteristics were compared either by Wilcoxon signed rank tests or Mann–Whitney test for continuous variables, chi-square or McNemar test for categorical variables. Comparison of the outcome was performed using a Cox model. Results were expressed as hazard ratio (HR) with 95% confidence interval (CI). All tests were two sided. The type-1 error rate was fixed at 0.05 for determination of factors associated with time to event outcomes. All analyses were performed using SPSS 24.0 (SPSS Inc, Chicago, IL, USA) and R version 3.4.0 (R Core Team. R: a language for statistical computing. 2014. R Foundation for Statistical Computing, Vienna, Austria).
Results
Patient and transplantation characteristics
One hundred and fifteen patients (39% females; median age 38 years; range 18–66) met the eligibility criteria and were included in this study (Tables 1, 2 and Supplementary Table 1). Patients had either primary refractory (26%) or relapsed ALL (43% first relapse, 31% second relapse or more); out of 69 patients with reported diagnosis, 49% had T-ALL and 23% were Philadelphia chromosome positive. Six patients (5%) underwent previous auto-transplant. The Karnofsky score was above 90 in 52% of the patients. Conditioning was MAC with high dose TBI in 30% of the patients, RIC including low dose TBI in 22%, and with chemotherapy alone (MAC or RIC) in 48%, most commonly involving cytarabine, fludarabine, and cyclophosphamide-based regimens. In vivo T-cell depletion (TCD) was used in 77 patients (69%). Most patients (74%) and about half of the donors (47%) were CMV positive. Fourteen percent of patients were males who received a graft from a female donor. Patients were allografted from a matched related (31%), matched unrelated (58%), or haploidentical donor (11%). The median follow-up of alive patients was 37 months (IQR 13–111).
Transplant outcomes
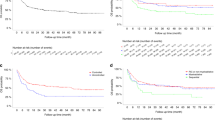
Day-100 acute GVHD grades II–IV and III–IV were encountered in 30% and 17% of patients, respectively, whereas the 2-year cumulative incidence of chronic GVHD was 25% with 11% developing extensive disease. The 2-year RI was 45% and NRM 41%. The 2-year LFS, OS, and GRFS were 14%, 17, and 12%, respectively. The main causes of death in 87 patients were the primary disease (31 patients; 37%), infections (26 patients; 31%), and GVHD (15 patients; 18%) (Table 3).
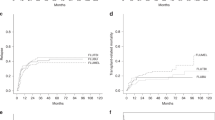
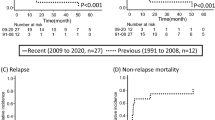
In univariate analysis, patient age, ALL subtype, status at transplant, year of transplant, donor type, patient and donor gender, female to male donor, patient CMV serology, and in vivo TCD did not affect any of the transplant outcomes (Supplementary Tables 2 and 3). On the other hand, the outcomes were affected by the Karnofsky score, donor CMV serology, and the choice of conditioning regimen. Patients with a Karnofsky score above 90 had a significantly better outcome as compared with those below, with relapse rates of 31% versus 59% (p < 0.005), 2-year LFS of 18% versus 3% (p < 0.005), 2-year OS of 21% versus 6% (p < 0.01), and 2-year GRFS of 17% versus 3%, respectively (p < 0.05) (Supplementary Tables 2 and 3). Finally, the choice of conditioning with MAC TBI, RIC TBI, and chemo alone was also associated with a significantly different 2-year LFS of 20, 25, and 7%, respectively (p < 0.001), OS of 34, 25, and 7%, respectively (p < 0.005), and GRFS of 16, 17, and 7% (p = 0.07) (Fig. 1 and Supplementary Tables 2 and 3). Of note, patients with T-ALL had better LFS, OS, and GRFS compared with B-ALL patients, although the differences did not achieve statistical significance, with no considerable differences between Philadelphia positive and negative patients in all outcomes (Supplementary Tables 2 and Fig. 2).
Multivariate analysis
In multivariate Cox analysis, a Karnofsky score above 90 positively affected relapse rates (HR = 0.21; p = 0.0001), LFS (HR = 0.47; p = 0.005), OS (HR = 0.48; p = 0.008), and GRFS (HR = 0.62; p = 0.06) (Table 4). Conversely, conditioning with chemotherapy alone compared with MAC TBI-based regimens negatively affected relapse rates (HR = 3.3; p = 0.008), LFS (HR = 1.94; p = 0.03), and OS (HR = 2.03; p = 0.03). Although there were no significant differences between MAC TBI and RIC TBI conditionings, the RIC TBI group had better outcomes across all endpoints (RI, NRM, LFS, OS, GRFS, aGVHD, and cGVHD) compared with MAC TBI group.
Discussion
In this study, we evaluated the predictive factors for post-transplant outcomes in a data set of 115 patients from the EBMT registry using sequential conditioning in RR-ALL. We found that RI, LFS, OS, and GRFS were significantly better in patients with Karnofsky scores above 90 at transplant, which is in agreement with previously published data [24]. Outcomes were also significantly better in patients who received TBI-based conditioning compared to chemotherapy alone. These results may help guide the treatment choice for RR-ALL.
There is much debate concerning the optimal pre-transplantation conditioning for ALL patients. While prospective randomized trials have yet to establish a definitive answer, many large multicenter retrospective studies suggest reduced relapse rates and a survival advantage with TBI-based regimens compared to chemotherapy alone [18, 25]. TBI was in fact shown as superior to many popular chemo-based conditionings, especially in young fit patients with T‐ALL and refractory disease [11, 26]. Despite the toxicities and long term complications associated with TBI, it appears to be mandatory in the setting of RR-ALL, even though results remain relatively poor in this population. However, new radiation-free strategies including thiotepa-based conditioning are emerging, with retrospective studies suggesting its noninferiority to TBI-based regimens in terms of survival and decreased overall long term toxicities [27]. Randomized trials are still needed to further explore the role of thiotepa in replacing TBI, especially in RR-ALL patients. Another TBI alternative could be the use of intravenous busulfan (Bu)-containing conditioning regimens [28]. Recently published data compared 819 ALL patients who received TBI with 299 patients with Bu-based regimens, and while Bu patients had higher risk of relapse in multivariate analysis, both groups had similar OS (TBI 53% versus Bu 57%) and DFS (TBI 48% versus Bu 45%) [28]. This further highlights the extreme toxicities associated with TBI which does not necessarily always improve patient survival. Another newly emerging approach with the evolution of radiation techniques is the focus of TBI dose solely to the skeleton sparing the rest of the body. This total marrow irradiation is able to deliver the same or even higher doses to the infiltrated marrow while reducing overall toxicity, thus further moving into ultra-personalized conditioning [29].
Treating RR-ALL remains a clinical challenge. Its prognosis is generally dismal, with cure rates barely reaching 10% [1,2,3,4]. Achieving CR with chemotherapy alone is usually very difficult in these patients, making sequential based conditioning an acceptable alternative. Recent advances in targeted and immune therapies could potentially offer more options for treating RR-ALL. Inotuzumab ozogamicin, for instance, has been shown to increase the likelihood of reaching CR and to improve OS compared with standard chemotherapy in patients with RR B-cell precursor ALL [30]. Blinatumomab has shown similar advantages in the RR setting, with increased CR rates and an OS advantage [31]. The combination of blinatumomab and tyrosine kinase inhibitors, namely ponatinib, for the treatment of Philadelphia positive RR-ALL has produced very encouraging results [32, 33]. Treatment with these drugs could also potentially be useful as a bridge for transplant, thus allowing more patients to undergo the only curative measure for RR-ALL, allo-SCT. The use of inotuzumab in this setting however could increase the risk of veno-occlusive disease, making blinatumomab a better choice. For patients who relapse after transplant, offering a second allo-SCT is an option. However, recent data by the EBMT Acute Leukemia Working Party showed poor outcomes with OS and GRFS at 5 years of only 14% and 7%, respectively, with very high relapse rates [34]. Chimeric antigen receptor (CAR) T-cells have also emerged as another option for the treatment of RR-ALL—tisagenlecleucel, a CD19-directed CAR-T, yielded unprecedented results, with CR rates reaching 80% in heavily pretreated, mostly pediatrics’ ALL [35]. This led to its recent approval by the FDA as salvage therapy for young (≤25 years), fit RR-ALL patients, with studies yet to investigate its role in older, frailer patients [36].
An important aspect to consider when evaluating patients with RR-ALL for the optimal treatment strategy is the ALL subtype. As previously discussed, patients with B-cell RR-ALL have many alternatives to standard chemotherapy with the inclusion of novel agents, tyrosine kinase inhibitors when appropriate for Philadelphia positive patients, and even the use of CAR-T cells. Little progress, however, has been achieved for T-ALL patients, for whom an unmet need of better treatment remains. Nelarabine was granted accelerated approval by the U.S. Food and Drug Administration in 2005 for the treatment of patients with T-cell RR-ALL, and remains the only agent approved for this subpopulation [37]. Venetoclax is another promising option, with pre-clinical studies suggesting good response in T-ALL patients, particularly with immature or early T-cell precursor phenotype [38, 39]. Sequential conditioning-based therapy with the inclusion of TBI is therefore one of the few options currently available for this challenging subpopulation with few alternatives, further highlighting its importance.
The study was limited by its sample size, its lack of homogeneity in used conditionings across centers and its retrospective nature. Prospective clinical trials are required to fully understand the role of sequential conditioning in this population.
Conclusion
Allo-SCT using a sequential conditioning regimen can be proposed in RR-ALL, especially when considering a TBI-based regimen in patients with good Karnofsky score. However, the overall 2-year LFS of 14% suggests that these patients still face extremely poor outcomes, highlighting that other therapies (e.g., BITE antibodies, inotuzumab, CAR-T cells) need to be used. Ideally, these agents need to be combined with allo-SCT as patients can still relapse post novel agents use, possibly making allo-SCT the last available salvage treatment [40]. The need for novel strategies is also particularly crucial for T-ALL patients, for whom TBI-based sequential conditioning followed by allo-SCT is one of the few options currently available.
References
Fielding AK, Richards SM, Chopra R, Lazarus HM, Litzow MR, Buck G, et al. Outcome of 609 adults after relapse of acute lymphoblastic leukemia (ALL); an MRC UKALL12/ECOG 2993 study. Blood. 2007;109:944–50.
Tavernier E, Boiron JM, Huguet F, Bradstock K, Vey N, Kovacsovics T, et al. Outcome of treatment after first relapse in adults with acute lymphoblastic leukemia initially treated by the LALA-94 trial. Leukemia. 2007;21:1907–14.
Gokbuget N, Stanze D, Beck J, Diedrich H, Horst HA, Huttmann A, et al. Outcome of relapsed adult lymphoblastic leukemia depends on response to salvage chemotherapy, prognostic factors, and performance of stem cell transplantation. Blood. 2012;120:2032–41.
Forman SJ, Rowe JM. The myth of the second remission of acute leukemia in the adult. Blood. 2013;121:1077–82.
Bassan R, Hoelzer D. Modern therapy of acute lymphoblastic leukemia. J Clin Oncol. 2011;29:532–43.
Gokbuget N, Hoelzer D. Treatment of adult acute lymphoblastic leukemia. Semin Hematol. 2009;46:64–75.
Gokbuget N, Dombret H, Ribera JM, Fielding AK, Advani A, Bassan R, et al. International reference analysis of outcomes in adults with B-precursor Ph-negative relapsed/refractory acute lymphoblastic leukemia. Haematologica. 2016;101:1524–33.
O’Brien S, Thomas D, Ravandi F, Faderl S, Cortes J, Borthakur G, et al. Outcome of adults with acute lymphocytic leukemia after second salvage therapy. Cancer. 2008;113:3186–91.
Enrico M, Francesco S, Francesco L. Treatment of adult patients with relapsed/refractory b-cell philadelphia-negative acute lymphoblastic leukemia. Clin Hematol Int. 2019;1:85–93.
Oriol A, Vives S, Hernandez-Rivas JM, Tormo M, Heras I, Rivas C, et al. Outcome after relapse of acute lymphoblastic leukemia in adult patients included in four consecutive risk-adapted trials by the PETHEMA study group. Haematologica. 2010;95:589–96.
Pavlu J, Labopin M, Zoellner AK, Sakellari I, Stelljes M, Finke J, et al. Allogeneic hematopoietic cell transplantation for primary refractory acute lymphoblastic leukemia: a report from the Acute Leukemia Working Party of the EBMT. Cancer. 2017;123:1965–70.
Sheth V, Labopin M, Canaani J, Volin L, Brecht A, Ganser A, et al. Comparison of FLAMSA-based reduced intensity conditioning with treosulfan/fludarabine conditioning for patients with acute myeloid leukemia: an ALWP/EBMT analysis. Bone Marrow Transplant. 2018;54:531–9.
Fraccaroli A, Prevalsek D, Fritsch S, Haebe S, Bucklein V, Schulz C, et al. Sequential HLA-haploidentical transplantation utilizing post-transplantation cyclophosphamide for GvHD prophylaxis in high-risk and relapsed/refractory AML/MDS. Am J Hematol. 2018;93:1524–31.
Decroocq J, Itzykson R, Vigouroux S, Michallet M, Yakoub-Agha I, Huynh A, et al. Similar outcome of allogeneic stem cell transplantation after myeloablative and sequential conditioning regimen in patients with refractory or relapsed acute myeloid leukemia: a study from the societe Francophone de Greffe de Moelle et de Therapie Cellulaire. Am J Hematol. 2018;93:416–23.
Ringden O, Labopin M, Schmid C, Sadeghi B, Polge E, Tischer J, et al. Sequential chemotherapy followed by reduced-intensity conditioning and allogeneic haematopoietic stem cell transplantation in adult patients with relapse or refractory acute myeloid leukaemia: a survey from the Acute Leukaemia Working Party of EBMT. Br J Haematol. 2017;176:431–9.
Malard F, Labopin M, Stuhler G, Bittenbring J, Ganser A, Tischer J, et al. Sequential intensified conditioning regimen allogeneic hematopoietic stem cell transplantation in adult patients with intermediate- or high-risk acute myeloid leukemia in complete remission: a study from the acute leukemia working party of the european group for blood and marrow transplantation. Biol Blood Marrow Transpl. 2017;23:278–84.
Arita K, Kondo T, Sugita J, Shigematsu A, Shiratori S, Wakasa K, et al. Sequential chemotherapy and myeloablative allogeneic hematopoietic stem cell transplantation for refractory acute lymphoblastic leukemia. Int J Hematol. 2011;94:291–5.
Giebel S, Labopin M, Socie G, Beelen D, Browne P, Volin L, et al. Improving results of allogeneic hematopoietic cell transplantation for adults with acute lymphoblastic leukemia in first complete remission: an analysis from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. Haematologica. 2017;102:139–49.
Mohty M, Malard F, Blaise D, Milpied N, Socie G, Huynh A, et al. Sequential regimen of clofarabine, cytosine arabinoside and reduced-intensity conditioned transplantation for primary refractory acute myeloid leukemia. Haematologica. 2017;102:184–91.
Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V, et al. Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transpl. 2009;15:1628–33.
Glucksberg H, Storb R, Fefer A, Buckner CD, Neiman PE, Clift RA, et al. Clinical manifestations of graft-versus-host disease in human recipients of marrow from HL-A-matched sibling donors. Transplantation. 1974;18:295–304.
Terwey TH, Vega-Ruiz A, Hemmati PG, Martus P, Dietz E, le Coutre P, et al. NIH-defined graft-versus-host disease after reduced intensity or myeloablative conditioning in patients with acute myeloid leukemia. Leukemia. 2012;26:536–42.
Ruggeri A, Labopin M, Ciceri F, Mohty M, Nagler A. Definition of GvHD-free, relapse-free survival for registry-based studies: an ALWP-EBMT analysis on patients with AML in remission. Bone Marrow Transpl. 2016;51:610–1.
Ringden O, Boumendil A, Labopin M, Canaani J, Beelen D, Ehninger G, et al. Outcome of allogeneic hematopoietic stem cell transplantation in patients over 69 years of age with acute myeloid leukemia: on behalf of the acute leukemia working party of the Ebmt. Biol Blood Marrow Transplant. 2019. pii: S1083-8791(19)30362-3. https://doi.org/10.1016/j.bbmt.2019.05.037. [Epub ahead of print].
Mitsuhashi K, Kako S, Shigematsu A, Atsuta Y, Doki N, Fukuda T, et al. Comparison of cyclophosphamide combined with total body irradiation, oral busulfan, or intravenous busulfan for allogeneic hematopoietic cell transplantation in adults with acute lymphoblastic leukemia. Biol Blood Marrow Transpl. 2016;22:2194–200.
Cahu X, Labopin M, Giebel S, Aljurf M, Kyrcz-Krzemien S, Socie G, et al. Impact of conditioning with TBI in adult patients with T-cell ALL who receive a myeloablative allogeneic stem cell transplantation: a report from the acute leukemia working party of EBMT. Bone Marrow Transpl. 2016;51:351–7.
Eder S, Canaani J, Beohou E, Labopin M, Sanz J, Arcese W, et al. Thiotepa-based conditioning versus total body irradiation as myeloablative conditioning prior to allogeneic stem cell transplantation for acute lymphoblastic leukemia: a matched-pair analysis from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. Am J Hematol. 2017;92:997–1003.
Kebriaei P, Anasetti C, Zhang MJ, Wang HL, Aldoss I, de Lima M, et al. Intravenous Busulfan compared with total body irradiation pretransplant conditioning for adults with acute lymphoblastic leukemia. Biol Blood Marrow Transpl. 2018;24:726–33.
Rashmika RP, Sorab G, Sebastian G, Bipin NS, Gabor V, Arnon N, et al. Current status and perspectives of irradiation-based conditioning regimens for patients with acute leukemia undergoing hematopoietic stem cell transplantation. Clin Hematol Int. 2019;1:19–27.
Kantarjian HM, DeAngelo DJ, Stelljes M, Liedtke M, Stock W, Gokbuget N, et al. Inotuzumab ozogamicin versus standard of care in relapsed or refractory acute lymphoblastic leukemia: final report and long-term survival follow-up from the randomized, phase 3 INO-VATE study. Cancer. 2019;125:2474–87.
Kantarjian H, Stein A, Gokbuget N, Fielding AK, Schuh AC, Ribera JM, et al. Blinatumomab versus chemotherapy for advanced acute lymphoblastic leukemia. N Engl J Med. 2017;376:836–47.
Assi R, Kantarjian H, Short NJ, Daver N, Takahashi K, Garcia-Manero G, et al. Safety and efficacy of blinatumomab in combination with a tyrosine kinase inhibitor for the treatment of relapsed philadelphia chromosome-positive leukemia. Clin Lymphoma Myeloma Leuk. 2017;17:897–901.
El Chaer F, Holtzman NG, Sausville EA, Law JY, Lee ST, Duong VH, et al. Relapsed philadelphia chromosome-positive Pre-B-ALL after CD19-directed CAR-T cell therapy successfully treated with combination of blinatumomab and ponatinib. Acta Haematol. 2019;141:107–10.
Nagler A, Labopin M, Dholaria B, Finke J, Brecht A, Schanz U, et al. Second allogeneic stem cell transplantation in patients with acute lymphoblastic leukaemia: a study on behalf of the Acute Leukaemia Working Party of the European Society for Blood and Marrow Transplantation. Br J Haematol. 2019;186:767–76.
Maude SL, Laetsch TW, Buechner J, Rives S, Boyer M, Bittencourt H, et al. Tisagenlecleucel in Children and Young Adults with B-Cell Lymphoblastic Leukemia. N Engl J Med. 2018;378:439–48.
O’Leary MC, Lu X, Huang Y, Lin X, Mahmood I, Przepiorka D, et al. FDA approval summary: tisagenlecleucel for treatment of patients with relapsed or refractory b-cell precursor acute lymphoblastic leukemia. Clin Cancer Res. 2019;25:1142–6.
Cohen MH, Johnson JR, Justice R, Pazdur R. FDA drug approval summary: nelarabine (Arranon) for the treatment of T-cell lymphoblastic leukemia/lymphoma. Oncologist. 2008;13:709–14.
Peirs S, Matthijssens F, Goossens S, Van de Walle I, Ruggero K, de Bock CE, et al. ABT-199 mediated inhibition of BCL-2 as a novel therapeutic strategy in T-cell acute lymphoblastic leukemia. Blood. 2014;124:3738–47.
El-Cheikh J, Moukalled NM, El Darsa H, Massoud R, Kanj SS, Mahfouz R, et al. Feasibility of the combination of venetoclax and asparaginase-based chemotherapy for adult patients with relapsed/refractory acute lymphoblastic leukemia. Clin Lymphoma Myeloma Leuk. 2018;18:e441–e4.
Elad J. Relapse and resistance to CAR-T cells and blinatumomab in hematologic malignancies. Clin Hematol Int. 2019;1:79–84.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Bazarbachi, A.H., Al Hamed, R., Labopin, M. et al. Allogeneic stem-cell transplantation with sequential conditioning in adult patients with refractory or relapsed acute lymphoblastic leukemia: a report from the EBMT Acute Leukemia Working Party. Bone Marrow Transplant 55, 595–602 (2020). https://doi.org/10.1038/s41409-019-0702-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-019-0702-2
- Springer Nature Limited
This article is cited by
-
Upfront allogeneic hematopoietic stem cell transplantation for adult T-cell acute lymphoblastic leukemia/lymphoma in first complete remission: a single-center study
Annals of Hematology (2024)
-
Thiotepa, busulfan and fludarabine conditioning-regimen is a promising approach for older adult patients with acute lymphoblastic leukemia treated with allogeneic stem cell transplantation
Bone Marrow Transplantation (2023)
-
Azacitidine in Combination with Venetoclax Maintenance Post-allogeneic Hematopoietic Stem Cell Transplantation in T Cell Acute Lymphoblastic Leukemia
Clinical Hematology International (2023)
-
Wnt/β-catenin signaling mediates the abnormal osteogenic and adipogenic capabilities of bone marrow mesenchymal stem cells from chronic graft-versus-host disease patients
Cell Death & Disease (2021)
-
Prognostic factors for survival after allogeneic transplantation in acute lymphoblastic leukemia
Bone Marrow Transplantation (2021)