Abstract
The predictive value of graft composition and plasma biomarkers on the outcome of allogeneic HSCT is well known for conventional GVHD prophylaxis based on calcineurin inhibitors with or without antithymocyte globulin. Currently, there is limited data whether these results could be translated to post transplantation cyclophosphamide (PTCy). The prospective extension cohort of NCT02294552 trial enrolled 79 adult patients with acute leukemia in CR. Twenty-six received matched-related bone marrow (BM) grafts with single-agent PTCy and 53 received unrelated peripheral blood stem cell graft (PBSC) with PTCy, tacrolimus, and MMF. The grafts were studied by the flow cytometry, and plasma samples were analyzed by ELISA. In the cluster and major component analysis, we determined that transplantation from donors with high content of CD3, NKT, and CD16-CD56 + subpopulations in the PBSC grafts was associated with poor immunological recovery and compromised event-free survival (50% vs. 80%, HR 2.93, p = 0.015) both due to increased relapse incidence and non-relapse mortality. The significant independent predictor of moderate and severe chronic GVHD was the high prevalence of and iNKT, Vβ11, and double-positive cells in the PBSC grafts from young donors (HR 2.75, p = 0.0483). No patterns could be identified for BM grafts and for plasma biomarkers.
Similar content being viewed by others
Introduction
Post transplantation cyclophosphamide (PTCy) is a platform for graft-versus-host disease (GVHD) prophylaxis, which was first implemented in haploidentical hematopoietic stem cell transplantations (HSCT) [1, 2]. Now it is gaining popularity in matched-related and unrelated HSCTs [3,4,5] due to lower immunosuppression burden and low incidence of chronic GVHD [6, 7]. Single-agent PTCy is predominantly used for matched-related bone marrow (BM) transplantations, while combinations with other immunosuppressive agents are used for the peripheral blood stem cell grafts [3, 8, 9].
Graft composition is a well known factor affecting the outcome of HSCT. While the number of CD34 + cells is the gold standard to assess the quality of HSCT grafts at least for peripheral blood stem cells (PBSC) [10], the other cell populations are assessed for the prognostic purposes. It was demonstrated that total number of CD3 + cells moderately increase the risk of acute GVHD [11], while for overall populations of CD4 + and CD8 + cells there are controversial results [12, 13]. Other studies characterizing lymphocyte subsets in the graft demonstrated the association between T-regulatory cells (Treg) [14], TCR alpha/beta cells [15], TCR Vbeta11 + T cells [16], iNKT cells [17], and acute GVHD. On the other hand, higher numbers of NK, NKT cells were reported to facilitate engraftment graft-versus leukemia (GVL) effect [18, 19]. However, all the above-mentioned studies were evaluating the predictive role of lymphocyte subpopulations in the setting of classical GVHD prophylaxis consisting of calcineurin inhibitors, methotrexate or mycophenolate mofetil as the second agent with or without antithymocyte globulin (ATG). PTCy has a different mechanisms of tolerance induction comparing to the classical GVHD prophylaxis [20]. Thus, the predictive value of lymphocyte subpopulations in the graft might be different comparing to classical GVHD prophylaxis. Only few studies of PTCy were published with analysis of only CD3 levels in the graft [21] and none solely focused on the related and unrelated transplantations.
In the previous study of cytokines in the plasma of patients after PTCy, our group demonstrated the reverse association of interleukin (IL)-8 and interferon (INF) gamma concentrations with GVHD: higher level of these cytokines was associated with reduced GVHD incidence [22]. Thus, we hypothesized that more prominent activation of lymphocytes and NK cells after graft infusion, which is characterized by higher cytokine levels, results in more profound depletion of lymphocytes. The extent of lymphodepletion by ATG was reported to predict relapse and mortality after transplantation [23]. In this prospective study, we evaluated whether the same effect is observed for PTCy due to excessive activation of lymphocytes. Owing to the limited information about the impact of graft composition on the outcome with PTCy a large number of parameters were screened to look for associations. We evaluated graft cellular subpopulations mentioned earlier [10,11,12,13,14,15,16,17,18,19] and immunological recovery. Additionally, most common inflammatory plasma biomarkers were studied, including ST2, IL-2, receptor, soluble receptor to TNF alpha (srTNFalpha), IL-8, IL-17, and VEGF A [24,25,26,27,28]. Extended information about the donors was obtained.
Patients and methods
Seventy-nine adult consecutive patients were included prospectively in the study during 2016–2017 (Supplement Fig. S1). The enrolled patients participated in the expansion phase of the NCT02294552 study of risk-adapted PTCy prophylaxis [27]. All patients signed informed consent for blood collection, graft analysis, and collection of clinical and personal data. The study was approved by the First Pavlov medical university ethical committee. Conditioning was performed with fludarabine 180 mg/m2 and oral busulfan 10–14 mg/kg according to the institutional operating procedures. Dose of busulfan 14 mg/kg is labeled as MAC in the analysis and dose 10 mg/kg is labeled as RIC. GVHD prophylaxis was performed with cyclophosphomide 50 mg/kg at day + 3, + 4. Recipients of the matched-related donor (MRD) grafts received no further immunosuppression. Recipients of matched unrelated donor (MUD) grafts received tacrolimus 0.03 mg/kg/day and MMF 30–45 mg/kg starting from day + 5. All clinical procedures and supportive care was performed as in the original study [28]. The criteria for inclusion in this biomarker study were the following: acute myeloid leukemia (AML) or acute lymphoblastic leukemia (ALL) as the indication for HSCT; complete remission at the time of HSCT; transplantation of either BM from MRD with single-agent PTCy or PBSC from MUD with PTCy, tacrolimus and MMF prophylaxis. Single-antigen HLA mismatch was allowed for MUD. Twenty-six patients had transplantation from MRD, and 53 from MUD (Table 1). The planned group size for the study was 75 patients, including 25 MRD and 50 MUD HSCTs. Four additional patients were enrolled for the possibility of flow cytometry analysis failure, which did not occur during the study. Planned median follow-up was 2 years. The group size was calculated based on the data from ATG studies where up to 40% of patients exhibit excessive lymphodepletion and slow recovery afterwards. The difference in survival for the excessively lymphodepleted patients was 20% [23]. The power of the study was 70%. Characteristics of patients enrolled in MRD and MUD were not significantly different, except higher percentage of CD34 cells in the graft due to the use of PBSC (Supplement Table S1).
Flow cytometry
The fresh non-frozen samples of BM and peripheral blood apheresis products were studied on the day of HSCT by flow cytometry (FACS Aria II, BD Biosciences, CA, USA; antibodies by Miltenyi biotec, Bergisch Gladbach, Germany). At least 300,000 events were collected. The following populations were analyzed: CD3, CD4, CD8, CD19, CD16CD56, NKT, iNKT (including CD4 and CD8 subpopulations), Treg (CD4 + CD25 + CD127 + ), double-positive T cells (CD4 + CD8 + ), double-negative T cells, TCR alpha/beta, TCR Vβ11 cells. The gating strategies are presented in Supplement Fig. S1. Immunological recovery was assessed with the same lymphocyte subpopulations in the peripheral blood at day + 30, + 60, and + 100 in 40 last consecutive patients from the study group. Total lymphocyte recovery was available for all patients.
Enzyme-linked immunoassay
Blood was collected from the central venous line after discarding the first draw in the EDTA-containing tubes at days 0, + 7, + 30. The selection of days was based on the previous study of cytokines after PTCy [22]. The samples were centrifuged at + 4 °C and 1000 × g for 15 min, aliquoted and stored at −80 °C until the day of the assay. The samples were studied for IL-6, soluble TNF receptor, IL-2 receptor, VEGF A, IL-17, IL-8 (eBioscience, CA, USA) and ST2 (Critical diagnostics, CA, USA) by commercially available kits according to the instructions of the manufacturer. Concentrations were determined without knowledge of clinical data. The sensitivities of IL-17, IL-6, IL-8, soluble TNF-α receptor, VEGF A and IL-2 receptor were 0.5–100, 0.92–100, 2.0–1000, 100–10000, 7.9–1000, 270–15000 pg/ml, respectively. VEGF A was measured on day 0. IL-6, IL-8, soluble TNF receptor, and IL-2 receptor were measured on day + 7. ST2, soluble TNF receptor, and IL-17 were measured on day + 30 (Supplement Fig. S2). Samples with concentrations above the calibration curves were re-tested in dilution.
Clinical definitions
Time to disease relapse incidence (RI), acute GVHD (aGVHD), moderate to severe chronic GVHD (cGVHD), non-relapse mortality (NRM), overall survival (OS), event-free survival (EFS), and GVHD-relapse free survival (GRFS) were defined as the time from transplantation to the event. Incidence of aGVHD was calculated at 125 days after HSCT, and the time frame for the other outcomes was 2 years. Events for EFS were relapse or death. Disease relapse was defined as morphologic or cytogenetic evidence of disease with pre-transplantation characteristics, or morphologic evidence without pre-transplantation characteristics. GVHD-related mortality was defined as any death without relapse in a patient within the time frame of 2 years. The Consensus Conference criteria and National Institutes of Health criteria were used for aGVHD and cGVHD grading, respectively [29, 30]. Measurable residual disease (MRD) was assessed before transplantation in all patients. In ALL MRD was measured by 8-color flow cytometry. In AML it was evaluated by combination of WT1, PCR, and FISH (for patients with chromosomal aberrations).
Statistical analysis
In the group description overall survival (OS) and event-free survival (EFS) were calculated using Kaplan–Meier methodology. The comparisons were made using the log-rank test. Cumulative incidence analysis was used for aGVHD, cGVHD, relapse incidence, and NRM. The comparisons were made using Gray test. The competing risks for acute and chronic GVHD were relapse and donor lymphocyte infusion (DLI). No prophylactic DLIs were used in the study group. NRM and RI were also analyzed as competing risks. Multivariate analysis of EFS was performed with Cox regression. Non-parametric data was analyzed with Chi-square, Fisher exact and Mann–Whitney tests according the type of data in each group.
The methodology of the laboratory data analysis included several steps. First, the preliminary univariate Cox regression screening was performed for initial features extraction. The cluster analysis was performed for visualization of patterns in graft composition and cytokine profiles. Further identification of patterns in graft composition and cytokine profiles was performed with principle components analysis (PCA) [31]. Based on PCA results, the clusters extraction analysis was performed. The identified clusters were further characterized and evaluated against the outcomes highlighted in the initial screening [32]. Based on the experience with the selected patient population, the expected number of NRM and aGVHD events was to be <10 and produce low statistical power, thus the main focus in the statistical plan was made on EFS and chronic GVHD. Based on the results of clustering, the whole group was split and cumulative incidence or Kaplan–Meier curves were plotted. Data processing and visualization was implemented with use of the R statistical packages.
Results
Clinical results
Median follow-up was 22 months (range 15–33). In the whole group overall survival (OS) was 77%, event-free survival (EFS) 73%, grade II–IV aGVHD 13%, moderate and severe (m&s) chronic GVHD 20%, NRM 6%, RI−20%. The major cause of NRM were severe bacterial infections. There was no difference between BM/related and PBSC/unrelated grafts in the OS, EFS, incidence of aGVHD, cGVHD, NRM, and RI (p > 0.11, Supplement Fig. S3). Also there was no differences in the outcomes between ALL and AML patients (p > 0.09, Supplement Fig. S4). RI in the study group was not affected by the remission number (p = 0.1941), but was negatively impacted by cytogenetic risk (p = 0.0032) and presence of MRD (p = 0.0411).
Predictors of HSCT outcome
The cluster analysis of graft composition revealed two major groups of grafts. One with high prevalence of CD3 and NK effector subpopulations and low concentration of regulatory subpopulations. The other, on the contrary, contained higher prevalence of regulatory populations (iNKT, Treg) and lower number of CD16-CD56 + , TCR alpha/beta (Supplement Fig. S5). The graft variant with high effector prevalence was observed in 35% of cases with comparable frequency in the BM and PBSC group (p = 0.3). None of the donor characteristics, including age, gender, or donor white blood cell differential count before stimulation were associated with graft composition clusters (p > 0.4). No distinct groups of patients were identified based on cytokine cluster analysis (Supplement Fig. S6). Also there was no association between cytokines and graft cluster (p > 0.2), thus further analysis was focused on graft composition.
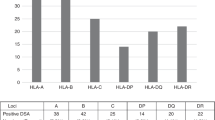
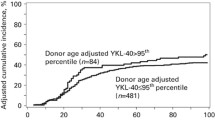
Based on cluster discrimination patients who received the graft with high levels of CD3 and NK cells had significantly lower EFS (85% vs. 61%, p = 0.0393, Supplement Fig. S7) due to higher relapse incidence (36% vs. 12%, p = 0.0105). The regression screening (Fig. 1a) identified possible association with lower EFS not only for effector subpopulations, but also for the early lymphocyte recovery. Thus, levels of CD3, NK, and NKT cells in the graft along with absolute lymphocyte count (ALC) on day + 30 were analyzed in principle component analysis, which identified the group of patients where high levels of CD3, NK, and NKT were associated with poor ALC recovery at day + 30 and reduced EFS (80% vs. 50%, p = 0.0106, Fig. 1b, c). The differences were due to both increased NRM (17% vs. 3%, p = 0.0437) and relapse (33% vs. 16%, p = 0.1330). No such association was observed for the BM grafts. Further characterization of this subgroup revealed that it was solely restricted to PBSC grafts (34%) with no cases in BM group (0%). The number of CD34 + cells was not different between the clusters (5.6 vs. 4.8 × 106/kg, p = 0.06). There was also no association with the level of cytokines measured (p > 0.39). Incidence if aGVHD (p = 0.9) and cGVHD (p = 0.6) was not different between these two groups.
a “Heat” plot of univariate p-values of the predictive parameters from Cox regression analyses. p-values > 0.1 are marked in white. More significant p-values a marked with darker colors. b Results of principal component analysis. The highlighted area comprises patients with high proportion of CD3, CD16-CD56 + , NKT cells in the graft, slow engraftment, and lymphocyte recovery. c Event-free survival in patients with high proportion of CD3, CD16-CD56 + , NKT cells in the graft and with lower proportion of these cells
In the multivariate analysis, the above-mentioned phenotype of the graft was still significantly predictive for EFS (HR 2.93, 95% CI 1.23–6.97, p = 0.015) along with the MRD-positive status before HSCT (HR 3.32, 95% CI 1.37–8.05, p = 0.008). Remission number (HR 1.7, 95% CI 0.81–3.37, p = 0.168) and cytogenetic risk (HR 2.57, 95% CI 0.83–4.34, p = 0.128) did not reach statistical significance.
No significant predictors for aGVHD were determined, however a subgroup of patients (25% from the whole group) with young donors and high prevalence of CD4 + CD8 + cells, iNKT cells, and TCR Vβ11 cells was identified in the principal component analysis (Supplement Fig. S8). With correction for previous grade III–IV aGVHD (HR 6.441, 95% CI 1.400–22.544, p = 0.0007), patients in this cluster had significantly higher incidence of moderate and severe cGVHD (HR 2.754, 95% CI 0.965–7.679, p = 0.0483). The median donor age was 24 years compared to 31 in the rest of the study group (p = 0.010). The phenotype with high prevalence of double-positive, iNKT, and TCR Vβ11 cells was significantly more often observed with PBSC grafts than with BM grafts (36% vs. 4%, p = 0.002). The cGVHD clusters and adverse EFS clusters significantly overlapped (p < 0.0001). None of the other donor characteristics, including gender, CMV serostatus, and steady-state differential WBC count were associated with the above-mentioned phenotype.
The confidence intervals of lymphocyte subsets in the graft determining adverse EFS and cGVHD are presented in Supplement Table S2.
Immunological recovery
Since the screening for predictive biomarkers identified the link between graft composition, lymphocyte recovery, and survival, additional analysis of immunologic recovery was performed in the subgroup of consecutive patients to determine the synchronicity of subpopulation recovery. Engraftment was faster in the PBSC group (median 20 vs. 22 days for neutrophils, p = 0.015 and 14 vs. 21 days for platelets, p < 0.001), however by day + 30 there was no significant differences in the level of WBC (p = 0.80) and lymphocytes (p = 0.49) between the groups. Also no differences between the PBSC and BM groups was observed in overall lymphocyte count by days + 60–180 (p > 0.1).
The absolute number of lymphocytes, CD3, CD8, TCR alpha/beta, and NK cells recovered rather rapidly after PTCy reaching normal range in the majority of patients by day + 60 [33]. However, CD4 + T-cell and B-cell recovery was significantly delayed (Fig. 2a). The cluster analysis demonstrated that there are four sets of populations according to the pace of recovery from day + 30 to day + 100: CD3, CD8, and TCR alpha/beta cells, CD4 and NKT cells, NK cell subpopulations, Treg and iNKT cells. All the subpopulations within the first three clusters significantly correlated with each over, while there was no correlation with the Treg and iNKT cells (Fig. 2b and Supplement Table S3). Although the size of the reconstitution cohort was small, there was a trend to the higher levels of iNKT cells (2.6 ± 3.1 vs. 0.9 ± 1.3 × 106/ml, p = 0.002) and Treg cells (32 ± 10 vs. 6 ± 1, p = 0.082), lower Day + 30 levels of CD3 + (100 ± 100 vs. 400 ± 680 × 106/ml, p = 0.053) and NKT (0.8 ± 0.8 vs. 12.0 ± 23.7 × 106/ml, p = 0.027) in the cluster of patients with initial high prevalence of CD3, NKT, and CD16-CD56 + cells in the graft.
a Recovery of lymphocytes in patients with relapse, non-relapse mortality, and alive without relapse. b Cluster analysis of the immunologic reconstitution. The color represents the mean absolute values for each time point normalized to the highest absolute level of reconstitution. Lighter colors indicate lower levels, darker colors indicate higher levels of reconstitution. The clusters demonstrate the synchronicity of reconstitution
Despite differences in the pace of reconstitution between lymphocyte subtypes, ALC on day + 30 with the cut off level 400 × 106/ml had very high predictive power for both RI (p = 0.0059) and NRM (p = 0.0074). Only 18% of relapses and one case of non-relapse mortality was documented in patients with day 30 ALC > 400 106/ml (Supplement Fig. S9). The difference in the EFS with this cutoff was 91% vs. 53% (p < 0.0001). Thirty-eight percent of patients had day + 30 ALC below this level and 10% were in the cluster with high prevalence of effector lymphocyte populations in the graft.
Discussion
The clinical results in the study population was comparable to the previously published for MRD [6] and MUD [3, 9] HSCTs with PTCy. There was some heterogeneity in the study population; it included both AML and ALL patients in CR, both MRD donors with single-agent PTCy and MUD/MMUD donors with PTCy-tacrolimus-MMF regimen. However, heterogenic patient populations are used in the majority of biological studies in HSCT recipients [25]. Nonetheless, in the current study the outcome of ALL and AML patients was not significantly different, which is in line with the CIBMTR data [34]. Also PTCy-based prophylaxis produced comparable results for MRD and MUD donors just like in the previous study [28]. So the presence of clinical heterogeneity might have not significantly impacted the results. On the other hand, relatively small study size might have prevented certain thoroughly validated biomarkers from reaching statistical significance.
The main conclusion of the study is that, like ATG [23, 35], PTCy in a subgroup of patients can cause excessive depletion of lymphocyte subpopulations, leading to delayed immunological recovery and adverse clinical outcome. Moreover, poor immunological recovery is the long known factor of dismal prognosis [36, 37]. However, unlike ATG, this effect of PTCy was not dependant on the increased exposure but rather on the composition of the graft. We have determined that in one-third of donors there is an “activated” phenotype of the graft with high prevalence of CD3, NKT, and CD16-CD56 + cell populations and low prevalence of Treg populations. It is equally observed in BM and PBSC grafts, however the significant clinical impact was observed only for PBSC. Patients who received grafts with this phenotype had higher risk of relapse and worse EFS. This observation is supported by the mechanism of action of PTCy when only activated cells undergo apoptosis due to differences in aldehyde dehydrogenase expression in activated lymphocytes [20].
This phenomenon seems to be unique for PTCy-based prophylaxis. The efficacy of classical prophylaxis is dependent on suppression of cytokine production [35, 38, 39, 40] and subsequent T-cell activation. Thus, this “activated” phenotype of donor immune system only increases the risk of aGVHD what was demonstrated in the previous studies [11, 15] or increases GVL in case of high NK cell population prevalence [18]. In our study, we observed that NK cell subpopulations play a completely opposite role. It was demonstrated that CD16-CD56 + are more prone to rapid activation compared to the other NK-subtypes [41, 42]. Along with that it was demonstrated that NK cells is one of the drivers of lymphocyte proliferation after graft infusion and before PTCy administration [43]. Since donors with high prevalence of NK cells also had increased numbers of T cells in the graft it is unclear which cell population determines the degree of activation after graft infusion. Further elucidation of these aspects in preclinical models might be complicated as the majority of them utilize bone marrow as the graft source [44].
The previous study of immunological recovery after haploidentical transplantation with PTCy identified delayed recovery of CD3 cells compared to MRD with classical prophylaxis [45], while in MRD setting with single-agent PTCy and BM as the graft source there was a relatively rapid recovery [46]. The probable explanation might be that this effect of “over-activation” and profound depletion by PTCy might be more prominent after haploidentical transplantation than after MRD and MUD. As in the previous study by Kanakry et al. [47], we observed that cell populations recovery after PTCy was relatively synchronous. So ALC is a parameter that could be assessed easily and predict the majority of adverse events after HSCT.
The identified subpopulations responsible for cGVHD represent the cells of thymic origin. Imbalance in CD4 + CD8 + [48, 49], Vbeta11 cells [50], and iNKT cells [51] was reported during chronic T-cell activation and autoimmune diseases, like lupus or rheumatoid arthritis. Thus, these expanded subpopulations in graft might represent the predisposition of donor immune system to autoimmune disease, which translates into cGVHD after HSCT.
While PTCy has been used for more than a decade, there might be several explanations why the reported associations have not been reported previously. First, there was relatively small number of studies looking at graft composition. Mussetti et al. [21] reported no impact of higher number of CD3 + cells in the graft on the outcome of haploidentical transplantations with PTCy. This might be due to differences in the protocol: cyclosporine A was given starting day + 1, which could have prevented the hyperactivation of lymphocytes. Also, as described previously, after haploidentical transplantation the effects of over-activation might affect more patients. Second, the studies that evaluated cytokine proteomics started the assessment by day 30, when the consequences of day + 1 and + 2 events might not be so easily captured [47]. The fact that cytokines tested in this study had low predictive value for the prognosis highlights the importance of blood sampling before graft infusion, before and after PTCy administration.
In conclusion, the study demonstrated that high concentrations of effector populations in the graft negatively impact the outcome after MRD and MUD PBSC transplantations with PTCy due to compromised immunological recovery. Confirmatory multicenter studies are required to confirm this observation and determine the safe cut offs. Also it should be studied if this “activation” phenotype could be captured by analysis of lymphocyte subpopulations in a donor peripheral blood at steady-state.
References
Luznik L, O’Donnell PV, Symons HJ, Chen AR, Leffell MS, Zahurak M, et al. HLA-haploidentical bone marrow transplantation for hematologic malignancies using nonmyeloablative conditioning and high-dose, posttransplantation cyclophosphamide. Biol Blood Marrow Transplant. 2008;14:641–50.
Raiola AM, Dominietto A, Ghiso A, Di Grazia C, Lamparelli T, Gualandi F, et al. Unmanipulated haploidentical bone marrow transplantation and posttransplantation cyclophosphamide for hematologic malignancies after myeloablative conditioning. Biol Blood Marrow Transplant. 2013;19:117–22.
Ruggeri A, Labopin M, Bacigalupo A, Afanasyev B, Cornelissen JJ, Elmaagacli A, et al. Post-transplant cyclophosphamide for graft-versus-host disease prophylaxis in HLA matched sibling or matched unrelated donor transplant for patients with acute leukemia, on behalf of ALWP-EBMT. J Hematol Oncol. 2018;11:40.
Luznik L, Bolaños-Meade J, Zahurak M, Chen AR, Smith BD, et al. High-dose cyclophosphamide as single-agent, short-course prophylaxis of graft-versus-host disease. Blood. 2010;115:3224–30.
Mielcarek M, Furlong T, O’Donnell PV, Storer BE, McCune JS, Storb R, et al. Posttransplantation cyclophosphamide for prevention of graft-versus-host disease after HLA-matched mobilized blood cell transplantation. Blood. 2016;127:1502–8.
Kanakry CG, O’Donnell PV, Furlong T, de Lima MJ, Wei W, Medeot M, et al. Multi-institutional study of post-transplantation cyclophosphamide as single-agent graft-versus-host disease prophylaxis after allogeneic bone marrow transplantation using myeloablative busulfan and fludarabine conditioning. J Clin Oncol. 2014;32:3497–505.
Kanakry CG, Bolaños-Meade J, Kasamon YL, Zahurak M, Durakovic N, Furlong T, et al. Low immunosuppressive burden after HLA-matched related or unrelated BMT using posttransplantation cyclophosphamide. Blood. 2017;129:1389–93.
Moiseev IS, Pirogova OV, Babenko EV, Gindina TL, Darskaya EI, Morozova EV, et al. Single-agent post-transplantation cyclophosphamide versus calcineurin-based graft-versus-host disease prophylaxis in matched related bone marrow transplantation. Cell Ther Transplant (CTT). 2017;6:52–9.
Mehta RS, Saliba RM, Chen J, Rondon G, Hammerstrom AE, Alousi A, et al. Post-transplantation cyclophosphamide versus conventional graft-versus-host disease prophylaxis in mismatched unrelated donor haematopoietic cell transplantation. Br J Haematol. 2016;173:444–55.
Roscoe RA, Rybka WB, Winkelstein A, Houston AM, Kiss JE. Enumeration of CD34+ hematopoietic stem cells for reconstitution following myeloablative therapy. Cytometry. 1994;16:74–9.
Saad A, Lamb L, Wang T, Hemmer MT, Spellman S, Couriel D, et al. Impact of T-cell dose on the outcome of T-cell replete HLA matched allogeneic peripheral blood stem cell transplantation. Biol Blood Marrow Transplant. 2019;S1083-8791:30291–5. https://doi.org/10.1016/j.bbmt.2019.05.007.
Waller EK, Logan BR, Harris WA, Devine SM, Porter DL, Mineishi S, et al. Improved survival after transplantation of more donor plasmacytoid dendritic or naïve T cells from unrelated-donor marrow grafts: results from BMTCTN 0201. J Clin Oncol. 2014;32:2365–72.
Reshef R, Huffman AP, Gao A, Luskin MR, Frey NV, Gill SI, et al. High graft CD8 cell dose predicts improved survival and enables better donor selection in allogeneic stem-cell transplantation with reduced-intensity conditioning. J Clin Oncol. 2015;33:2392–8.
Edinger M, Hoffmann P, Ermann J, Drago K, Fathman CG, Strober S, et al. CD4+CD25+ regulatory T cells preserve graft-versus-tumor activity while inhibiting graft-versus-host disease after bone marrow transplantation. Nat Med. 2003;9:1144–50.
Locatelli F, Bauquet A, Palumbo G, Moretta F, Bertaina A. Negative depletion of α/β+ T cells and of CD19+ B lymphocytes: a novel frontier to optimize the effect of innate immunity in HLA-mismatched hematopoietic stem cell transplantation. Immunol Lett. 2013;155:21–3.
DiRienzo CG, Murphy GF, Friedman TM, Korngold R. T-cell receptor V(alpha) usage by effector CD4+Vbeta11+ T cells mediating graft-versus-host disease directed to minor histocompatibility antigens. Biol Blood Marrow Transplant. 2007;13:265–76.
Malard F, Labopin M, Chevallier P, Guillaume T, Duquesne A, Rialland F, et al. Larger number of invariant natural killer T cells in PBSC allografts correlates with improved GVHD-free and progression-free survival. Blood. 2016;127:1828–35.
Panse JP, Heimfeld S, Guthrie KA, Maris MB, Maloney DG, Baril BB, et al. Allogeneic peripheral blood stem cell graft composition affects early T-cell chimaerism and later clinical outcomes after non-myeloablative conditioning. Br J Haematol. 2005;128:659–67.
Vela-Ojeda J, García-Ruiz Esparza MA, Reyes-Maldonado E, Jiménez-Zamudio L, García-Latorre E, Moreno-Lafont M, et al. Clinical relevance of NK, NKT, and dendritic cell dose in patients receiving G-CSF-mobilized peripheral blood allogeneic stem cell transplantation. Ann Hematol. 2006;85:113–20.
Luznik L, O’Donnell PV, Fuchs EJ. Post-transplantation cyclophosphamide for tolerance induction in HLA-haploidentical bone marrow transplantation. Semin Oncol. 2012;39:683–93.
Mussetti A, De Philippis C, Carniti C, Bastos-Oreiro M, Gayoso J, Cieri N, et al. CD3+ graft cell count influence on chronic GVHD in haploidentical allogeneic transplantation using post-transplant cyclophosphamide. Bone Marrow Transplant. 2018;53:1522–31.
Pirogova OV, Moiseev IS, Surkova EA, Lapin SV, Bondarenko SN, Kulagin AD, et al. Profiles of pro-inflammatory cytokines in allogenic stem cell transplantation with post-transplant cyclophosphamide. Cytokine. 2017;99:148–53.
Admiraal R, Nierkens S, de Witte MA, Petersen EJ, Fleurke GJ, Verrest L, et al. Association between anti-thymocyte globulin exposure and survival outcomes in adult unrelated haemopoietic cell transplantation: a multicentre, retrospective, pharmacodynamic cohort analysis. Lancet Haematol. 2017;4:e201.
Paczesny S, Krijanovski OI, Braun TM, Choi SW, Clouthier SG, Kuick R, et al. A biomarker panel for acute graft-versus-host disease. Blood. 2009;113:273–8.
Vander Lugt MT, Braun TM, Hanash S, Ritz J, Ho VT, Antin JH, et al. ST2 as a marker for risk of therapy-resistant graft-versus-host disease and death. N Engl J Med. 2013;369:529–39.
Berger M, Signorino E, Muraro M, Quarello P, Biasin E, Nesi F, et al. Monitoring of TNFR1, IL-2Rα, HGF, CCL8, IL-8 and IL-12p70 following HSCT and their role as GVHD biomarkers in paediatric patients. Bone Marrow Transplant. 2013;48:1230–6.
Levine JE, Braun TM, Harris AC, Holler E, Taylor A, Miller H, et al. Blood and marrow transplant clinical trials network. A prognostic score for acute graft-versus-host disease based on biomarkers: a multicentre study. Lancet Haematol. 2015;2:e21–9.
Moiseev IS, Pirogova OV, Alyanski AL, Babenko EV, Gindina TL, Darskaya EI, et al. Risk-adapted GVHD prophylaxis with post-transplantation cyclophosphamide in adults after related, unrelated, and haploidentical transplantations. Eur J Haematol. 2018;100:395–402.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. 1994 consensus conference on acute GVHD grading. Bone Marrow Transplant. 1995;15:825–8.
Filipovich AH, Weisdorf D, Pavletic S, Socie G, Wingard JR, Lee SJ, et al. National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. Diagnosis and staging working group report. Biol Blood Marrow Transplant. 2005;11:945–56.
Wing K, Fung, Hong Gu, Liming X, et al. Assessing local influence in principal component analysiswith application to haematology study data. Stat Med. 2007;26:2730–44. https://doi.org/10.1002/sim.2747
Joseph FH, Rolph AE, Ronald LT, William CB. Multivariate data analysis, 5th ed. Pearson Education; 2003.
Santagostino A, Garbaccio G, Pistorio A, Bolis V, Camisasca G, Pagliaro P, et al. An Italian national multicenter study for the definition of reference ranges for normal values of peripheral blood lymphocyte subsets in healthy adults. Haematologica. 1999;84:499–504.
Forman SJ, Rowe JM. The myth of the second remission of acute leukemia in the adult. Blood. 2013;121:1077–82.
Mohty M. Mechanisms of action of antithymocyte globulin: T-cell depletion and beyond. Leukemia. 2007;21:1387–94.
Klyuchnikov E, Asenova S, Kern W, Kilinc G, Ayuk F, Wiedemann B, et al. Post-transplant immune reconstitution after unrelated allogeneic stem cell transplant in patients with acute myeloid leukemia. Leuk Lymphoma. 2010;51:1450–63.
Bartelink IH, Belitser SV, Knibbe CA, Danhof M, de Pagter AJ, Egberts TC, et al. Immune reconstitution kinetics as an early predictor for mortality using various hematopoietic stem cell sources in children. Biol Blood Marrow Transplant. 2013;19:305–13.
Cutolo М, Sulli A, Pizzorni C. Anti-inflammatory mechanisms of methotrexate in rheumatoid arthritis. Ann Rheum Dis. 2001;60:729–35.
Allison AC, Eugui EM. Mycophenolate mofetil and its mechanisms of action. Immunopharmacology. 2000;47:85–118.
Matsuda S, Koyasu S. Mechanisms of action of cyclosporine. Immunopharmacology. 2000;47:119–25.
Alter G, Teigen N, Davis BT, Addo MM, Suscovich TJ, Waring MT et al. Sequential deregulation of NK cell subset distribution and function starting in acute HIV-1 infection. Blood. 2005;106:3366–9.
Forconi CS, Cosgrove CP, Saikumar-Lakshmi P, Nixon CE, Foley J, Ong'echa JM et al. Poorly cytotoxic terminally differentiated CD56negCD16pos NK cells accumulate in Kenyan children with Burkitt lymphomas. Blood Adv. 2018;2:1101–14.
Russo A, Oliveira G, Berglund S, Greco R, Gambacorta V, Cieri N et al. NK cell recovery after haploidentical HSCT with posttransplant cyclophosphamide: dynamics and clinical implications. Blood. 2018;131:247–262.
Ferrara J, Deeg H, Cooke K, Ferrara J, Cooke K, Deeg H (eds.). Graft vs. host disease. Boca Raton: CRC Press;2004.
Di Stasi A, Milton DR, Poon LM, Hamdi A, Rondon G, Chen J, et al. Similar transplantation outcomes for acute myeloid leukemia and myelodysplastic syndrome patients with haploidentical versus 10/10 human leukocyte antigen-matched unrelated and related donors. Biol Blood Marrow Transplant. 2014;20:1975–81.
Kanakry CG, Coffey DG, Towlerton AM, Vulic A, Storer BE, Chou J, et al. Origin and evolution of the T cell repertoire after posttransplantation cyclophosphamide. JCI Insight. 2016;1:e86252. epub Apr 21 2016
Kanakry CG, Bakoyannis G, Perkins SM, McCurdy SR, Vulic A, Warren EH, et al. Plasma-derived proteomic biomarkers in human leukocyte antigen-haploidentical or human leukocyte antigen-matched bone marrow transplantation using post-transplantation cyclophosphamide. Haematologica. 2017;102:932–40.
Nascimbeni M, Shin EC, Chiriboga L, Kleiner DE, Rehermann B. Peripheral CD4(+)CD8(+) T cells are differentiated effector memory cells with antiviral functions. Blood. 2004;104:478–86.
Quandt D, Rothe K, Scholz R, Baerwald CW, Wagner U. Peripheral CD4CD8 double positive T cells with a distinct helper cytokine profile are increased in rheumatoid arthritis. PLoS ONE. 2014;9:e93293.
van der Vliet HJ, von Blomberg BM, Nishi N, Reijm M, Voskuyl AE, van Bodegraven AA, et al. Circulating V(alpha24+) Vbeta11+ NKT cell numbers are decreased in a wide variety of diseases that are characterized by autoreactive tissue damage. Clin Immunol. 2001;100:144–8.
Smith E, Croca S, Waddington KE, Sofat R, Griffin M, Nicolaides A, et al. Cross-talk between iNKT cells and monocytes triggers an atheroprotective immune response in SLE patients with asymptomatic plaque. Sci Immunol. 2016;1:eaah4081.
Acknowledgements
The study was supported by the RFBR grant 16–34–60142 mol_а_dk and RSF grant №17–75–20145. We express our deep gratitude to the unrelated donor registries’ employees who provided the extended information about the unrelated donors: Tigran Torosian and Jan Markert from DKMS, Andreas Heu from Stefan Morsch Stiftung, Malisheva Natalia from Kirov registry, and Marina Teterina from Saint-Petersburg registry. We thank Valerii Beklenischev for performing the biobanking and handling of the frozen samples and our nurses for the collection of the samples.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Moiseev, I.S., Babenko, E.V., Epifanovskaya, O.S. et al. High prevalence of CD3, NK, and NKT cells in the graft predicts adverse outcome after matched-related and unrelated transplantations with post transplantation cyclophosphamide. Bone Marrow Transplant 55, 544–552 (2020). https://doi.org/10.1038/s41409-019-0665-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-019-0665-3
- Springer Nature Limited