Abstract
Warfarin has a very narrow therapeutic window and obvious interindividual variability in its effects, with many factors contributing to the body’s response. Algorithms incorporating multiple genetic, environment and clinical factors have been established to select a precision dose for each patient. A number of randomized controlled trials (RCTs) were conducted to explore whether patients could benefit from these algorithms; however, the results were inconsistent. Some questions remain to be resolved. Recently, new genetic and non-genetic factors have been discovered to contribute to variability in optimal warfarin doses. The results of further RCTs have been unveiled, and guidelines for pharmacogenetically guided warfarin dosing have been updated. Based on these most recent advancements, we summarize some open questions in this field and try to propose possible strategies to resolve them.
Similar content being viewed by others
Introduction
Warfarin is one of the most commonly prescribed oral anticoagulation drugs used for the treatment and prevention of thromboembolic disorders. It has a very narrow therapeutic window, and there is obvious interindividual variability in the body’s response to the drug. Warfarin dosing needs to be personalized for each patient in order to improve its efficacy and safety. Currently, genetic variation is widely recognized as a key contributor to optimal warfarin dosing and is used to guide warfarin treatment. A number of randomized controlled trials (RCTs) have assessed the benefit of genotype-guided warfarin dosing; however, they came to different conclusions. Although the pharmacogenetics of warfarin dosing has already been well reviewed and discussed, some questions remain unresolved [1,2,3].
Recently, both new genetic and non-genetic factors have been discovered to contribute to variability in optimal warfarin doses. The results of further RCTs have been unveiled, and guidelines for pharmacogenetically guided warfarin dosing have been updated. Based on these most recent advancements, we discuss the open questions regarding warfarin precision dosing and propose possible strategies to resolve them.
What new factors affect interindividual differences in warfarin response?
Many factors contribute to the response to warfarin and can be divided into two categories: genetic and non-genetic.
Genetic factors
Warfarin exerts anticoagulant effects by targeting the vitamin K epoxide reductase complex (VKORC1). Administered warfarin is predominantly metabolized by CYP2C9 to inactive products. Most of the current pharmacogenomics studies on the topic focus on CYP2C9 and VKORC1 polymorphisms. CYP2C9 encodes one of the major hepatic drug-metabolizing enzymes in humans. At least 60 variant alleles have been discovered, with remarkable ethnic differences. Two of the most commonly occurring SNPs are *2 (rs1799853) and *3 (rs1057910). In vitro studies in mammalian cells showed that both polymorphisms impaired CYP2C9 expression and decreased key kinetic parameters (Km, Vmax, and CLint) of S-warfarin metabolism [4, 5]. Compared with patients homozygous for the *1 allele, *2 and *3 carriers showed an increased risk of bleeding, a reduced maintenance dose and reduced international normalized ratio (INR) time in target range (TTR) [6]. VKORC1, the protein target of warfarin, catalyzes the conversion of epoxidized vitamin K to reduced vitamin K. Genetic variations altering VKORC1 activity may affect warfarin response. G-1639A (rs9923231) is the most studied polymorphism, and is located in the promoter. A luciferase reporter assay showed that this polymorphism decreased VKORC1 promoter activity [7]. Clinical trials also suggested that this SNP was associated with reduced maintenance drug dose, decreased INR TTR and increased risk of over-anticoagulation [6]. Additional SNPs of CYP2C9 and VKORC1 have also been investigated; however, their contribution to drug dose variability is limited due to either low frequency or weak correlation. CYP4F2 catalyzes the conversion of reduced vitamin K to hydroxyl-vitamin K, which removes vitamin K from the cycle. *3 (rs2108622), a non-synonymous SNP, is the most commonly investigated polymorphism of CYP4F2. Studies based on recombinant proteins and human liver microsomes showed that *3 decreases CYP4F2 protein expression and the capacity for vitamin K metabolism [8]. In patients, CYP4F2*3 showed a significant correlation with warfarin therapeutic dose, with carriers of the mutant allele required an increased dose [9].
CYP2C9, VKORC1 and CYP4F2 are well-recognized genes correlated with warfarin dosing; however, they explain only ~40% of the inter-individual differences in drug response [1, 6, 10] (Fig. 1). Thus, new genetic factors affecting warfarin efficacy and safety remain to be discovered. Some strategies can be proposed. First, new technologies can be utilized. With increases in genotyping throughput and decreases in sequencing cost, genome-wide association studies (GWAS) are becoming a robust tool to discover new genetic factors related to warfarin dosing. For example, CYP4F2*3 and CYP2C rs12777823 were discovered by GWAS [11,12,13,14,15]. Recently, next-generation sequencing (NGS) has been used in warfarin pharmacogenomic studies [15]. A targeted resequencing study of candidate regions in patients with an extreme quantitative phenotype found four novel mutations, namely, DNMT3A rs2304429, CYP1A1 rs3826041, STX1B rs72800847, and NQO1 rs10517, which were significantly correlated with warfarin maintenance dose [16]. However, a study employing whole-exome sequencing (WES) or whole-genome sequencing (WGS) is still lacking. Second, although we focus on common SNPs, rare or low-frequency variants should not be ignored. Some studies in the literature have unveiled the contribution of rare variants to warfarin response. Several non-synonymous mutations of VKORC1, namely, Val29Leu, Val45Ala, Arg58Gly, Arg98Trp, Leu128Arg, and Tyr139Cys, were identified to be associated with resistance to warfarin [17]. Their minor allele frequencies (MAFs) were all lower than 1%. A recent study further identified the significant association of rare variants in the COX15 and FGF5 genes with warfarin dose [18]. However, most of the current genetic studies are not designed to detect the contributions of rare variants. Using NGS, future investigations can sequence low-frequency variants in larger samples of patients to find these potential missing heritability. Finally, more clinical outcomes should be explored. Most of the existing studies have focused only on stable warfarin doses, and the factors contributing to other phenotypes remain largely unknown [6]. A GWAS analyzed warfarin maintenance dose and TTR in the same population. The results identified both CYP2C9 and VKORC1 as hits in the dose analysis; however, the only SNP that reached genome-wide significance in the TTR analysis was aspartate beta-hydroxylase (ASPH) rs4379440 [19]. This result indicated that genetic contribution may vary according to different clinical outcomes. To date, only CYP2C9 and VKORC1 polymorphisms were investigated in relation to the phenotypes of percent time in target range (PTTR), risk of bleeding events, time to achieve a stable INR and first INR in therapeutic range [6]. It is possible that additional genetic variations contributing to clinical outcomes other than stable doses can be discovered. An example is APOE ε variants, which were shown to increase the risk of intracerebral haemorrhage [20].
Non-genetic factors
Clinical and environmental factors have well-established correlations with warfarin response, including age, height, weight, race, gender, medicine interactions, smoking and age (Fig. 1). Some of those factors have already been incorporated into the dose prediction algorithms and have been well reviewed elsewhere [1]. Here, we discuss pharmacomicrobiomic and pharmacoepigenetic factors, which are emerging as important influences [21]. With increasing recognition of the importance of the microbiome to human health and disease, a growing number of studies have reported the contribution of the gut microbiome to drug response [22,23,24]. Data released by the Human Microbiome Project (HMP) showed remarkable inter-individual diversity in the human microbiome, which may explain inter-individual differences in drug response [25, 26]. Clinically, the anticoagulant effect of warfarin is strongly affected by diet. Warfarin can be metabolized in the intestine by CYP2C9, which is one of the major CYPs expressed in the gut [27]. Furthermore, a recent study showed that warfarin significantly reduced the growth of certain strains of gut bacteria [28]. It is reasonable to propose that gut microbiome diversity contributes to warfarin metabolism in the gut, which, in turn, influences drug response.
Pharmacoepigenetics investigates the epigenetic basis of interindividual differences in drug response [29]. Current studies are focused on DNA methylation and microRNA (miRNA) regulation; some such biomarkers have already been used to guide clinical drug treatment [30]. It was reported that both CYP2C9 and VKORC1 can be regulated by a number of miRNAs, including miR-130, miR-128, miR-133 and miR-137 [31,32,33,34]. A few studies reported that miR-133 polymorphisms were correlated with variability in optimal warfarin dosing [35, 36]. These results need to be further validated in different populations.
How can the performance of dose prediction algorithms be improved?
The efficacy and safety of warfarin are affected by multiple genetic, environmental and clinical factors. Thus, algorithms incorporating those factors are indispensable for predicting drug response and adverse reaction events.
Current algorithms
Two major algorithm types are initial and revision dose prediction algorithms. Age, height, weight, race, medicine interactions, and genetic variation in CYP2C9 and VKORC1 are the major factors included in them. Initial dose prediction algorithms are the most extensively investigated type, and at least 20 algorithms of this class have been reported [37]. It was reported that CYP2C9 affected the elimination rate of S-warfarin but not initial drug sensitivity [38, 39]. Some studies established initial dose prediction algorithms without CYP2C9 genotypes, which is the most notable difference among them [40, 41]. The most frequently used mathematical model for algorithm establishment is multivariate linear regression (MLR), while a few studies employ the machine learning methods of Bayesian forecasting, random forest regression, boosted regression trees, support vector regression and artificial neural networks [42,43,44,45,46]. In 2009, the International Warfarin Pharmacogenetics Consortium (IWPC) established an algorithm in a total of 5700 patients and proposed a well-known evaluation criterion for prediction accuracy [47]. The consortium suggested that an algorithm should be considered successful when the predicted dose was within 20% of the actual value. The IWPC model is available as a free app called iWarfarin. Another widely used algorithm was developed by Gage et al. [48]. The therapeutic doses calculated by the algorithm are based on data from over 1000 patients. This algorithm can be accessed on a free website (www.WarfarinDosing.org), which facilitates its use by clinicians. Dose revision algorithms are utilized to adjust warfarin dosing after initial treatment. In addition to the factors in the initial dose algorithm, this type incorporates INR values and initial doses [40, 49, 50]. As with initial dose algorithms, dose adjustment algorithms are established by MLR using multiple genetic, environmental and clinical factors [49, 50].
Improvement of prediction accuracy
For initial dose prediction algorithms, the included genetic and clinical factors explain approximately 55% of the dose variation, while the predictive accuracy is less than 70% in most studies. In a previous RCT, patients in two arms received an initial dose based on the IWPC algorithm, while subsequent doses were adjusted according to either MLR dose revision or standard INR-based algorithms [40]. The outcomes of the percentage of out-of-range INR (POOR) and PTTR were similar between the two arms. Thus, the accuracy of dose revision algorithms also needs to be improved.
Some strategies can be considered in pursuit of improved accuracy. First, the prediction performance needs to be stratified and analyzed. A comparison of the predicted and clinically observed doses showed that the bias existed mainly in patients who required higher or lower doses than the average value [51]. Further analysis showed that bias was more serious in patients with lower doses than in those with higher doses, and more than 86% of the lower-dose patients received overestimates [52]. The poor prediction accuracy in these patients with extreme doses lowered the overall performance of the algorithms. This is a possible reason for the unsatisfactory results of some genotype-guided RCTs. Second, the contribution of variants to the initial and stable doses may be different. Considering drug safety and tolerance, a patient’s stable dose may not be the best initial dose. The initial dose is normally much lower than the stable dose, and the contribution of factors to them may not be the same. Recently, genetic variants included in the initial dose prediction algorithm have emerged as being associated with stable doses. Theoretically, these variants are appropriate for predicting the stable dose rather than initial dose and, if used for the latter purpose, may cause side effects due to overdosing. This may account for the low prediction performance of algorithms. Third, ethnic differences should be considered in the generation of algorithms. The allelic frequencies of CYP2C9, VKORC1 and CYP4F2 SNPs vary greatly among populations with different ancestry. They are the major genetic factors included in most algorithms and should be weighted differently according to race. In both the COAG and GIFT trials, the PTTR achieved with genotype-guided dosing varied obviously between Black and other races when the same algorithms were used [53, 54]. We compared the predictive ability of the algorithms based on different mathematical models and found that MLR was the best model in Chinese patients, while machine learning methods including Bayesian additive regression trees and multivariate adaptive regression splines had better performance in Caucasian and Black patients [52, 55]. These results indicated that establishing algorithms based on ethnic differences can improve their performance. Finally, more factors affecting warfarin efficacy and safety should be integrated into the algorithms. The currently known genetic and clinical factors explained only ~55% of the dose variation. As discussed above, more factors contributing to optimal warfarin doses are awaiting discovery, including rare genetic variants, pharmacomicrobiomic and pharmacoepigenetic biomarkers. Incorporating these novel factors can improve algorithm performance.
What is behind the inconsistent results of RCTs?
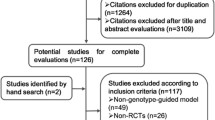
The goal of genetic variant discovery and algorithm development is to guide the clinical use of warfarin. At least 19 published RCTs explored whether patients with indications for warfarin could benefit from pharmacogenetically guided dosing, including three large clinical trials (EU-PACT, COAG and GIFT) [54, 56,57,58]. In addition, seven meta-analyzes were conducted based on these trials [59,60,61,62,63,64,65]. However, neither RCTs nor meta-analyzes obtained a consistent conclusion.
Comparison of the EU-PACT, COAG and GIFT trials
Until recently, the most intensively discussed results of warfarin dosing RCTs were those of EU-PACT and COAG, which were two major RCTs conducted in Europe and the USA [1, 2]. Although both were well-designed trials with large sample sizes, their results were contradictory. EU-PACT showed that pharmacogenetically guided dosing improved PTTR during the first 12 weeks after warfarin initiation, while COAG did not find any difference between the two arms. There were many differences between the two studies that might explain their inconsistent results, including dosing algorithm, control arm, use of loading doses, blinding, patient ethnicity and recruitment area [1, 2]. It is difficult to compare these two trials with each other.
Recently, the results of the GIFT trial were published, revealing that genotype-guided dosing reduced adverse events and improved the PTTR achieved with warfarin, which was also inconsistent with COAG [54]. GIFT was very similar to COAG, and most of the differences between EU-PACT and COAG did not exist between these two trials. Thus, it is possible to explain the contradictory results by comparing the three trials (Table 1). First, the dosing algorithms of the three trials were different. The most important differences came from the control patients. Both GIFT and COAG employed clinical algorithms, while EU-PACT used traditional dosing. It has been reported that an algorithm incorporating clinical factors is more predictive than a fixed dose [66]. In addition, there are differences between genotype-guided dosing algorithms. EU-PACT used the IWPC algorithm, while both GIFT and COAG employed the Gage algorithm. The major difference came from CYP4F2*3. The GIFT trial incorporated CYP4F2*3, which was not included in COAG and EU-PACT. CYP4F2*3 has been widely reported to be significantly correlated with warfarin dose in non-African populations, explaining 1.5–7% of the inter-individual dose difference [9, 11, 67, 68]. In addition, algorithms incorporating CYP4F2*3 increased warfarin dosing predicting accuracy by ~1–2% [69]. Most of the patients in GIFT were non-African, and genotyping CYP4F2*3 may have helped them benefit from pharmacogenetics-guided dosing. Second, the duration of genotype-guided dosing was extended to 11 days in GIFT [70]. By contrast, in the COAG trial design, there were 4 or 5 days of genotype-guided dosing. Patients received their initial dose in the first 3 days based on the initiation algorithm, followed by dose adjustment on the 4th and/or 5th day based on the revision algorithm, while GIFT extended this period to 11 days. Patients have the lowest PTTR in the initial stage of treatment, which means a high risk of bleeding and thromboembolic events [71,72,73]. Genotype-guided dosing showed the greatest effect in improving PTTR and lowering adverse events during the early stage of therapy. Thus, extending the duration of genotype-guided dosing after the beginning of warfarin treatment could further reduce adverse events and improve the PTTR. Third, the ethnic composition was different. Of the patients, 91% in GIFT were White, while the population in COAG was composed of 73% White and 27% Black individuals. Due to this difference, the frequencies of CYP2C9 and VKORC1 variants were lower in COAG than in GIFT. It has been reported that patients with higher frequencies of VKORC1 and CYP2C9 polymorphisms benefit more from genotype-guided dosing, which could explain the better clinical outcome in GIFT [74]. In addition, the correlation of genetic polymorphisms with warfarin dosing is different among ethnicities [6]. For example, CYP4F2*3 has no effect on warfarin dose requirements in people of African descent [75]. In contrast, CYP2C rs12777823 is associated with warfarin dosing in African Americans [15]. Thus, guiding warfarin dosing in patients of different ethnicities using the same genetic factors would affect the performance of the genotype-guided dosing algorithm. Based on the ethnic stratification analysis in the COAG trial, PTTR was lower for Black and higher for non-Black patients in the genotype-guided group than in the control group [56]. Similar results were also obtained in the GIFT trial [54]. Based on these analyses, ethnicity-specific genotyping strategies should be employed to improve algorithm performance [76]. In addition to the dosing algorithm, genetic panel and ethnic composition, other differences in the GIFT trial included older patients, open-label drug doses and different indications.
Unresolved questions
Despite the growing body of RCT results, some questions remain to be answered. First, it is not yet known to what extent patients can benefit from genotype-guided warfarin dosing. Based on the results of EU-PACT and GIFT, genotype-guided dosing showed the most significant effect in reducing instances of INR ≥ 4. Thirty-five and 11 patients needed to be genotyped to prevent one instance of INR ≥ 4 in GIFT and EU-PACT, respectively. Bleeding and thromboembolism are also important adverse events that can occur during warfarin therapy, and they may result in hospitalization. Although genotype-guided dosing reduced these two events slightly, no significant difference was observed between the two arms in either trial. Another important outcome is PTTR, which is recognized as a surrogate of adverse responses to warfarin. Patients with higher values showed a lower risk of bleeding and thromboembolic events [71,72,73]. Genotype-guided dosing significantly improved PTTR by 7.4 and 3.4% in EU-PACT and GIFT, respectively. It was reported that a 6.9% improvement in PTTR prevented one major bleeding event per 100 patient-years, while an 11.9% improvement in PTTR prevented one thromboembolic event per 100 patient-years [77]. Theoretically, genotyping prevented the occurrence of 1.07 events of major bleeding and 0.62 events of thromboembolism per 100 patient-years in EU-PACT, while the corresponding values in GIFT were 0.49 events of major bleeding and 0.29 events of thromboembolism. Collectively, the improvement of PTTR and prevention of adverse events by genotyping was limited, especially compared with the standard dosing regimen. In addition, some RCTs showed that genotype-guided dosing did not improve patient outcomes. Thus, the benefit of genotype-guided dosing still needs to be supported by further clinical trials. Second, the benefit of genotype-guided dosing in some races of patients is unclear. Existing RCTs have mainly been performed in White patients. Although the results concerning treatment benefits are conflicting, there are no data showing a harmful effect of genotype-guided dosing. Thus, using genetic data on CYP2C9*2 and *3, VKORC1 G-1639A and CYP4F2*3 during treatment is recommended for White patients by some guidelines. For Black patients, the results are controversial. Data from the COAG trial showed that using the same algorithm applied to non-Black patients is harmful to Black patients. Thus, genotype-guided dosing algorithms incorporating only CYP2C9*2, *3 and VKORC1 G-1639A should not be used for them. Instead, some other polymorphisms could be considered, including CYP2C9*5, *6, *8, and *11 as well as CYP2C rs12777823. These polymorphisms are correlated with lower required warfarin doses in this race. However, the performance of dosing algorithms incorporating these SNPs in the clinic still needs to be tested by RCTs. For Asian patients, more data are needed. Except for CYP2C9*2 and *3 and VKORC1 G-1639A, no genetic variations are well established to be correlated with warfarin dosing in the Asian population. Although several novel mutations were recently identified in Chinese patients, they accounted for only 2.2% of the dose discrepancy and still need to be validated [16, 78]. Several RCTs in patients of Asian descent have been reported, and the results conflict with each other [79,80,81,82,83]. One recently completed RCT (NCT02211326) enrolled 660 patients in 15 centres in Hunan Province, China. This study will provide further insight into the benefit of genotype-guided warfarin dosing in Chinese patients. Third, future clinical trials need new genotype-guided dosing strategies. Currently, pharmacogenetically guided dosing is designed to be applied only in the first 4 to 5 days in most studies. A number of clinical trials showed that the INR gradually increased in the first 2 weeks and peaked on approximately the 15th day after the initial dose. Patients in this period have increased susceptibility to overdose. Compared with control patients, those who received genotype-guided dosing group had reduced INR peak values [56,57,58, 79, 84]. Theoretically, extending pharmacogenetically guided dosing to span the first 2 weeks could improve outcomes. This is supported by the results of GIFT, which extended pharmacogenetically guided dosing across the first 11 days. Another strategy is to employ new dosing algorithms with better performance. Dosing regimens largely determine clinical outcomes; however, their prediction accuracy still needs to be improved. As discussed above, algorithms that incorporate more factors contributing to warfarin dose requirements remain to be developed. Clinical outcomes could be better in the future trials using newly developed dosing prediction algorithms.
Why is genotype-guided dosing not wildly implemented in the clinic?
Although warfarin is one of the most actionable drugs for genotype-guided dosing, genetic testing is still not routine for physicians and patients.
Recommendation from databases and guidelines
The Pharmacogenomics Knowledgebase (PharmGKB) is a database on the impact of human genetic variation on drug responses, providing clinical annotation regarding levels of evidence for variation-drug combinations [85]. Level 1 is the highest grade and is applied in CPIC guidelines or known clinical implementations. The clinical annotation evidence for CYP2C9*2, *3 and VKORC1 G-1639A in PharmGKB is recognized as level 1A, while CYP4F2*3 is listed as 1B. CYP2C9 and VKORC1 are labelled as actionable pharmacogenomic biomarkers of warfarin response by the U.S. Food and Drug Administration (FDA). Some in vitro companion diagnostic genetic test kits designed for their genotyping have been approved by the FDA as an aid to warfarin dosing [https://www.fda.gov/medicaldevices/productsandmedicalprocedures/invitrodiagnostics/ucm330711.htm]. There are at least three clinical guidelines regarding pharmacogenetics-guided warfarin dosing. All of them give the recommendations based on CYP2C9, VKORC1 and CYP4F2 genotypes. However, there are some substantial differences (Table 2). The evidence-based clinical practice guidelines of the American College of Chest Physicians (ACCP) recommend routine genetic testing of CYP2C9 and VKORC1 for patients initiating therapy [86]. The guidelines of the Canadian Pharmacogenomics Network for Drug Safety (CPNDS) suggested testing CYP2C9*2 and *3 as well as VKORC1 G-1639A for all warfarin-naive patients (including paediatric patients) within the first 2 weeks of therapy, while CYP2C9*5, *6, *8 and *11 as well as CYP4F2*3 was not recommended. In patients who reached a stable INR, no genetic testing was recommended [87]. The CPIC guidelines were updated recently, recommending pharmacogenetically guided warfarin dosing only when the genotype is available [6]. For adult patients of non-African ancestry, a strong recommendation was given to conduct dose calculations based on pharmacogenetic algorithms using the CYP2C9*2, *3 and VKORC1 G-1639A genotypes. For patients of African ancestry, the same recommendation was deemed moderate rather than strong. In addition, patients of African descent carrying CYP2C9*5, *6, *8 and *11 and African American carrying CYP2C rs12777823 in were moderately recommended to decrease the calculated dose.
Considerations for clinical implementation
One of the most important considerations is cost-effectiveness. Although a number of pharmacoeconomics investigations have compared the cost-effectiveness of genotype-guided and standard dosing, but no consistent conclusion could be obtained [88, 89]. Most of the studies showed that genotyping increased both the cost and the quality-adjusted life-year (QALY) gain to different degrees. However, the results of incremental cost-effectiveness ratio (ICER) per QALY analysis were different. Some were below the willingness-to-pay threshold, while others exceeded the accepted cost. Factors contributing to cost-effectiveness include the predictive accuracy of algorithms, adverse events reduced by genotype-guided dosing, cost and turnaround time (TAT) of genetic tests. With the development of sequencing and genotyping technology, genetic testing can be accomplished with increased throughput, decreased time and decreased cost [90, 91]. In addition, identification of additional genetic and other factors correlated with warfarin dosing and improvement of the algorithms can increase the prediction accuracy. Thus, more recent studies found that genotype-guided dosing was cost effective compared with standard dosing [92,93,94]. However, this conclusion is still uncertain and requires further investigation. Currently, CPIC guidelines recommend genotype-guided dosing only when the genotype is available. Based on this strategy, the cost-effectiveness could be improved. However, many patients are unable to access the benefit because only a few patients have their pharmacogenomic data available at present. The second consideration for widespread clinical implementation is the lack of data and guidelines for some subpopulations. Although two guidelines recommended genetic testing in paediatric patients, the benefit of genotype-guided dosing in children remains unknown. In addition, there are no guidelines for patients from some ancestral backgrounds. For example, guidelines are available for Asian patients. These questions should be answered by future clinical trials in patients from corresponding subpopulations.
Conclusion and future directions
Warfarin ranks as one of the most successfully opportunities for pharmacogenetics-guided dosing; however, a number of open questions remain to be answered (Fig. 2). At present, the correlation between genetic variations and warfarin dose requirements is well recognized. Algorithms incorporating multiple genetic, environmental and clinical factors have been established to predict both initial and revision doses. Based on these investigations, genotype-guided dosing of warfarin is recommended in several guidelines. In the future, the remaining factors affecting the efficacy and safety warfarin should be ascertained, and new dose calculation algorithms need to be developed. Most importantly, new dosing strategies should be designed in further clinical trials to improve the benefit to patients receiving genotype-guided dosing. In addition, exploring the performance of pharmacogenetics-guided dosing in a real-world setting is an emerging topic of research [95].
References
Pirmohamed M, Kamali F, Daly AK, Wadelius M. Oral anticoagulation: a critique of recent advances and controversies. Trends Pharmacol Sci. 2015;36:153–63.
Johnson JA, Cavallari LH. Warfarin pharmacogenetics. Trends Cardiovasc Med. 2015;25:33–41.
Cavallari LH, Nutescu EA. Warfarin pharmacogenetics: to genotype or not to genotype, that is the question. Clin Pharmacol Ther. 2014;96:224.
Niinuma Y, Saito T, Takahashi M, Tsukada C, Ito M, Hirasawa N, et al. Functional characterization of 32 CYP2C9 allelic variants. Pharm J. 2014;14:107–14.
Hiratsuka M. In vitro assessment of the allelic variants of cytochrome P450. Drug Metab Pharmacokinet. 2012;27:68–84.
Johnson JA, Caudle KE, Gong L, Whirl-Carrillo M, Stein CM, Scott SA, et al. Clinical Pharmacogenetics Implementation Consortium (CPIC) Guideline for Pharmacogenetics-Guided Warfarin Dosing: 2017 Update. Clin Pharmacol Ther. 2017;102:397–404.
Yuan HY, Chen JJ, Lee MT, Wung JC, Chen YF, Charng MJ, et al. A novel functional VKORC1 promoter polymorphism is associated with inter-individual and inter-ethnic differences in warfarin sensitivity. Human Mol Genet. 2005;14:1745–51.
McDonald MG, Rieder MJ, Nakano M, Hsia CK, Rettie AE. CYP4F2 is a vitamin K1 oxidase: An explanation for altered warfarin dose in carriers of the V433M variant. Mol Pharmacol. 2009;75:1337–46.
Caldwell MD, Awad T, Johnson JA, Gage BF, Falkowski M, Gardina P, et al. CYP4F2 genetic variant alters required warfarin dose. Blood. 2008;111:4106–12.
Johnson JA, Gong L, Whirl-Carrillo M, Gage BF, Scott SA, Stein CM, et al. Clinical Pharmacogenetics Implementation Consortium Guidelines for CYP2C9 and VKORC1 genotypes and warfarin dosing. Clin Pharmacol Ther. 2011;90:625–9.
Takeuchi F, McGinnis R, Bourgeois S, Barnes C, Eriksson N, Soranzo N, et al. A genome-wide association study confirms VKORC1, CYP2C9, and CYP4F2 as principal genetic determinants of warfarin dose. PLoS Genet. 2009;5:e1000433.
Cha PC, Mushiroda T, Takahashi A, Kubo M, Minami S, Kamatani N, et al. Genome-wide association study identifies genetic determinants of warfarin responsiveness for Japanese. Human Mol Genet. 2010;19:4735–44.
Cooper GM, Johnson JA, Langaee TY, Feng H, Stanaway IB, Schwarz UI, et al. A genome-wide scan for common genetic variants with a large influence on warfarin maintenance dose. Blood. 2008;112:1022–7.
Parra EJ, Botton MR, Perini JA, Krithika S, Bourgeois S, Johnson TA, et al. Genome-wide association study of warfarin maintenance dose in a Brazilian sample. Pharmacogenomics. 2015;16:1253–63.
Perera MA, Cavallari LH, Limdi NA, Gamazon ER, Konkashbaev A, Daneshjou R, et al. Genetic variants associated with warfarin dose in African-American individuals: a genome-wide association study. Lancet. 2013;382:790–6.
Luo Z, Li X, Zhu M, Tang J, Li Z, Zhou X, et al. Identification of novel variants associated with warfarin stable dosage by use of a two-stage extreme phenotype strategy. J Thromb Haemost: JTH. 2017;15:28–37.
Rost S, Fregin A, Ivaskevicius V, Conzelmann E, Hortnagel K, Pelz HJ, et al. Mutations in VKORC1 cause warfarin resistance and multiple coagulation factor deficiency type 2. Nature. 2004;427:537–41.
Liu N, Irvin MR, Zhi D, Patki A, Beasley TM, Nickerson DA, et al. Influence of common and rare genetic variation on warfarin dose among African-Americans and European-Americans using the exome array. Pharmacogenomics. 2017;18:1059–73.
Eriksson N, Wallentin L, Berglund L, Axelsson T, Connolly S, Eikelboom J, et al. Genetic determinants of warfarin maintenance dose and time in therapeutic treatment range: a RE-LY genomics substudy. Pharmacogenomics. 2016;17:1425–39.
Falcone GJ, Radmanesh F, Brouwers HB, Battey TW, Devan WJ, Valant V, et al. APOE epsilon variants increase risk of warfarin-related intracerebral hemorrhage. Neurology. 2014;83:1139–46.
Ivanov M, Barragan I, Ingelman-Sundberg M. Epigenetic mechanisms of importance for drug treatment. Trends Pharmacol Sci. 2014;35:384–96.
Routy B, Le Chatelier E, Derosa L, Duong CPM, Alou MT, Daillere R, et al. Gut microbiome influences efficacy of PD-1-based immunotherapy against epithelial tumors. Science. 2017;359:91–7.
Gopalakrishnan V, Spencer CN, Nezi L, Reuben A, Andrews MC, Karpinets TV, et al. Gut microbiome modulates response to anti-PD-1 immunotherapy in melanoma patients. Science. 2017;359:97–103.
Geller LT, Barzily-Rokni M, Danino T, Jonas OH, Shental N, Nejman D, et al. Potential role of intratumor bacteria in mediating tumor resistance to the chemotherapeutic drug gemcitabine. Science. 2017;357:1156–60.
Schloissnig S, Arumugam M, Sunagawa S, Mitreva M, Tap J, Zhu A, et al. Genomic variation landscape of the human gut microbiome. Nature. 2013;493:45–50.
Lloyd-Price J, Mahurkar A, Rahnavard G, Crabtree J, Orvis J, Hall AB, et al. Strains, functions and dynamics in the expanded Human Microbiome Project. Nature. 2017;550:61–6.
Thelen K, Dressman JB. Cytochrome P450-mediated metabolism in the human gut wall. J Pharm Pharmacol. 2009;61:541–58.
Maier L, Pruteanu M, Kuhn M, Zeller G, Telzerow A, Anderson EE, et al. Extensive impact of non-antibiotic drugs on human gut bacteria. Nature. 2018;555:623–8.
Majchrzak-Celinska A, Baer-Dubowska W. Pharmacoepigenetics: an element of personalized therapy? Expert Opin Drug Metab Toxicol. 2017;13:387–98.
Hegi ME, Diserens AC, Gorlia T, Hamou MF, de Tribolet N, Weller M, et al. MGMT gene silencing and benefit from temozolomide in glioblastoma. New Engl J Med. 2005;352:997–1003.
Rieger JK, Reutter S, Hofmann U, Schwab M, Zanger UM. Inflammation-associated microRNA-130b down-regulates cytochrome P450 activities and directly targets CYP2C9. Drug Metab Dispos: Biol fate Chem. 2015;43:884–8.
Yu D, Green B, Marrone A, Guo Y, Kadlubar S, Lin D, et al. Suppression of CYP2C9 by microRNA hsa-miR-128-3p in human liver cells and association with hepatocellular carcinoma. Sci Rep. 2015;5:8534.
Perez-Andreu V, Teruel R, Corral J, Roldan V, Garcia-Barbera N, Salloum-Asfar S, et al. miR-133a regulates vitamin K 2,3-epoxide reductase complex subunit 1 (VKORC1), a key protein in the vitamin K cycle. Mol Med. 2013;18:1466–72.
Shomron N. MicroRNAs and pharmacogenomics. Pharmacogenomics. 2010;11:629–32.
Ciccacci C, Rufini S, Politi C, Novelli G, Forte V, Borgiani P. Could MicroRNA polymorphisms influence warfarin dosing? A pharmacogenetics study on mir133 genes. Thromb Res. 2015;136:367–70.
Tang XY, Zhang J, Peng J, Tan SL, Zhang W, Song GB, et al. The association between GGCX, miR-133 genetic polymorphisms and warfarin stable dosage in Han Chinese patients with mechanical heart valve replacement. J Clin Pharm Ther. 2017;42:438–45.
Hillman MA, Wilke RA, Caldwell MD, Berg RL, Glurich I, Burmester JK. Relative impact of covariates in prescribing warfarin according to CYP2C9 genotype. Pharmacogenetics. 2004;14:539–47.
Schwarz UI, Ritchie MD, Bradford Y, Li C, Dudek SM, Frye-Anderson A, et al. Genetic determinants of response to warfarin during initial anticoagulation. New Engl J Med. 2008;358:999–1008.
Voora D, Eby C, Linder MW, Milligan PE, Bukaveckas BL, McLeod HL, et al. Prospective dosing of warfarin based on cytochrome P-450 2C9 genotype. Thromb Haemost. 2005;93:700–5.
Anderson JL, Horne BD, Stevens SM, Woller SC, Samuelson KM, Mansfield JW, et al. A randomized and clinical effectiveness trial comparing two pharmacogenetic algorithms and standard care for individualizing warfarin dosing (CoumaGen-II). Circulation. 2012;125:1997–2005.
Pirmohamed M, Burnside G, Eriksson N, Jorgensen AL, Toh CH, Nicholson T, et al. A randomized trial of genotype-guided dosing of warfarin. New Engl J Med. 2013;369:2294–303.
Sasaki T, Tabuchi H, Higuchi S, Ieiri I. Warfarin-dosing algorithm based on a population pharmacokinetic/pharmacodynamic model combined with Bayesian forecasting. Pharmacogenomics. 2009;10:1257–66.
Cosgun E, Limdi NA, Duarte CW. High-dimensional pharmacogenetic prediction of a continuous trait using machine learning techniques with application to warfarin dose prediction in African Americans. Bioinformatics. 2011;27:1384–9.
Hu YH, Wu F, Lo CL, Tai CT. Predicting warfarin dosage from clinical data: a supervised learning approach. Artif Intell Med. 2012;56:27–34.
Isma’eel HA, Sakr GE, Habib RH, Almedawar MM, Zgheib NK, Elhajj IH. Improved accuracy of anticoagulant dose prediction using a pharmacogenetic and artificial neural network-based method. Eur J Clin Pharmacol. 2014;70:265–73.
Pavani A, Naushad SM, Kumar RM, Srinath M, Malempati AR, Kutala VK. Artificial neural network-based pharmacogenomic algorithm for warfarin dose optimization. Pharmacogenomics. 2016;17:121–31.
Consortium TIWP. Estimation of the warfarin dose with clinical and pharmacogenetic data. New Engl J Med. 2009;360:753–64.
Gage BF, Eby C, Johnson JA, Deych E, Rieder MJ, Ridker PM, et al. Use of pharmacogenetic and clinical factors to predict the therapeutic dose of warfarin. Clin Pharmacol Ther. 2008;84:326–31.
Millican EA, Lenzini PA, Milligan PE, Grosso L, Eby C, Deych E, et al. Genetic-based dosing in orthopedic patients beginning warfarin therapy. Blood. 2007;110:1511–5.
Lenzini P, Wadelius M, Kimmel S, Anderson JL, Jorgensen AL, Pirmohamed M, et al. Integration of genetic, clinical, and INR data to refine warfarin dosing. Clin Pharmacol & Ther. 2010;87:572–8.
Yan H, Yin JY, Zhang W, Li X. Possible strategies to make warfarin dosing algorithm prediction more accurately in patients with extreme dose. Clin Pharmacol Ther. 2018;103:184.
Li X, Liu R, Luo ZY, Yan H, Huang WH, Yin JY, et al. Comparison of the predictive abilities of pharmacogenetics-based warfarin dosing algorithms using seven mathematical models in Chinese patients. Pharmacogenomics. 2015;16:583–90.
Kimmel SE, French B, Kasner SE, Johnson JA, Anderson JL, Gage BF, et al. A pharmacogenetic versus a clinical algorithm for warfarin dosing. New Engl J Med. 2013;369:2283–93.
Gage BF, Bass AR, Lin H, Woller SC, Stevens SM, Al-Hammadi N, et al. Effect of genotype-guided warfarin dosing on clinical events and anticoagulation control among patients undergoing hip or knee arthroplasty: the GIFT randomized clinical trial. J Am Med Assoc. 2017;318:1115–24.
Liu R, Li X, Zhang W, Zhou HH. Comparison of nine statistical model based warfarin pharmacogenetic dosing algorithms using the racially diverse international warfarin pharmacogenetic consortium cohort database. PloS ONE. 2015;10:11.
Kimmel SE, French B, Kasner SE, Johnson JA, Anderson JL, Gage BF, et al. A pharmacogenetic versus a clinical algorithm for warfarin dosing. New Engl J Med. 2013;369:2283–93.
Pirmohamed M, Burnside G, Eriksson N, Jorgensen AL, Toh CH, Nicholson T, et al. A randomized trial of genotype-guided dosing of warfarin. New Engl J Med. 2013;369:2294–303.
Verhoef TI, Ragia G, de Boer A, Barallon R, Kolovou G, Kolovou V, et al. A randomized trial of genotype-guided dosing of acenocoumarol and phenprocoumon. New Engl J Med. 2013;369:2304–12.
Shi C, Yan W, Wang G, Wang F, Li Q, Lin N. Pharmacogenetics-based versus conventional dosing of warfarin: a meta-analysis of randomized controlled trials. PloS ONE. 2015;10:e0144511.
Tang Q, Zou H, Guo C, Liu Z. Outcomes of pharmacogenetics-guided dosing of warfarin: a systematic review and meta-analysis. Int J Cardiol. 2014;175:587–91.
Xu H, Xie X, Wang B, Chen Y, Meng T, Ma S, et al. Meta-analysis of efficacy and safety of genotype-guided pharmacogenetic dosing of warfarin. Int J Cardiol. 2014;177:654–7.
Stergiopoulos K, Brown DL. Genotype-guided vs clinical dosing of warfarin and its analogues: meta-analysis of randomized clinical trials. JAMA Intern Med. 2014;174:1330–8.
Franchini M, Mengoli C, Cruciani M, Bonfanti C, Mannucci PM. Effects on bleeding complications of pharmacogenetic testing for initial dosing of vitamin K antagonists: a systematic review and meta-analysis. J Thromb Haemost: JTH. 2014;12:1480–7.
Li X, Yang J, Wang X, Xu Q, Zhang Y, Yin T. Clinical benefits of pharmacogenetic algorithm-based warfarin dosing: meta-analysis of randomized controlled trials. Thromb Res. 2015;135:621–9.
Dahal K, Sharma SP, Fung E, Lee J, Moore JH, Unterborn JN, et al. Meta-analysis of randomized controlled trials of genotype-guided vs standard dosing of warfarin. Chest. 2015;148:701–10.
Klein TE, Altman RB, Eriksson N, Gage BF, Kimmel SE, Lee MT, et al. Estimation of the warfarin dose with clinical and pharmacogenetic data. New Engl J Med. 2009;360:753–64.
Cen HJ, Zeng WT, Leng XY, Huang M, Chen X, Li JL, et al. CYP4F2rs2108622: a minor significant genetic factor of warfarin dose in Han Chinese patients with mechanical heart valve replacement. Br J Clin Pharmacol. 2010;70:234–40.
Borgiani P, Ciccacci C, Forte V, Sirianni E, Novelli L, Bramanti P, et al. CYP4F2 genetic variant (rs2108622) significantly contributes to warfarin dosing variability in the Italian population. Pharmacogenomics. 2009;10:261–6.
Zhang JE, Klein K, Jorgensen AL, Francis B, Alfirevic A, Bourgeois S, et al. Effect of genetic variability in the CYP4F2, CYP4F11, and CYP4F12 genes on liver mRNA levels and warfarin response. Front Pharmacol. 2017;8:323.
Do EJ, Lenzini P, Eby CS, Bass AR, McMillin GA, Stevens SM, et al. Genetics informatics trial (GIFT) of warfarin to prevent deep vein thrombosis (DVT): rationale and study design. Pharm J. 2012;12:417–24.
Lee A, Crowther M. Practical issues with vitamin K antagonists: elevated INRs, low time-in-therapeutic range, and warfarin failure. J Thromb Thrombolysis. 2011;31:249–58.
Connolly SJ, Pogue J, Eikelboom J, Flaker G, Commerford P, Franzosi MG, et al. Benefit of oral anticoagulant over antiplatelet therapy in atrial fibrillation depends on the quality of international normalized ratio control achieved by centers and countries as measured by time in therapeutic range. Circulation. 2008;118:2029–37.
Rose AJ, Hylek EM, Ozonoff A, Ash AS, Reisman JI, Berlowitz DR. Risk-adjusted percent time in therapeutic range as a quality indicator for outpatient oral anticoagulation: results of the Veterans Affairs Study to Improve Anticoagulation (VARIA). Circ Cardiovasc Qual Outcomes. 2011;4:22–9.
Bader LA, Elewa H. The impact of genetic and non-genetic factors on warfarin dose prediction in MENA region: a systematic review. PloS ONE. 2016;11:e0168732.
Danese E, Montagnana M, Johnson JA, Rettie AE, Zambon CF, Lubitz SA, et al. Impact of the CYP4F2 p.V433M polymorphism on coumarin dose requirement: systematic review and meta-analysis. Clin Pharmacol Ther. 2012;92:746–56.
Hernandez W, Gamazon ER, Aquino-Michaels K, Patel S, O’Brien TJ, Harralson AF, et al. Ethnicity-specific pharmacogenetics: the case of warfarin in African Americans. Pharm J. 2014;14:223–8.
Wan Y, Heneghan C, Perera R, Roberts N, Hollowell J, Glasziou P, et al. Anticoagulation control and prediction of adverse events in patients with atrial fibrillation: a systematic review. Circ Cardiovasc Qual Outcomes. 2008;1:84–91.
Liu J, Jiang HH, Wu DK, Zhou YX, Ye HM, Li X, et al. Effect of gene polymorphims on the warfarin treatment at initial stage. Pharm J. 2017;17:47–52.
Wen MS, Chang KC, Lee TH, Chen YF, Hung KC, Chang YJ, et al. Pharmacogenetic dosing of warfarin in the Han-Chinese population: a randomized trial. Pharmacogenomics. 2017;18:245–53.
Wang M, Lang X, Cui S, Fei K, Zou L, Cao J, et al. Clinical application of pharmacogenetic-based warfarin-dosing algorithm in patients of Han nationality after rheumatic valve replacement: a randomized and controlled trial. Int J Med Sci. 2012;9:472–9.
Huang SW, Chen HS, Wang XQ, Huang L, Xu DL, Hu XJ, et al. Validation of VKORC1 and CYP2C9 genotypes on interindividual warfarin maintenance dose: a prospective study in Chinese patients. Pharm Genom. 2009;19:226–34.
Syn NL, Wong AL, Lee SC, Teoh HL, Yip JWL, Seet RC, et al. Genotype-guided versus traditional clinical dosing of warfarin in patients of Asian ancestry: a randomized controlled trial. BMC Med. 2018;16:104.
Xu Z, Zhang SY, Huang M, Hu R, Li JL, Cen HJ, et al. Genotype-guided warfarin dosing in patients with mechanical valves: a randomized controlled trial. Annals Thoracic Surgery. 2018;106:1774–81.
Pengo V, Zambon CF, Fogar P, Padoan A, Nante G, Pelloso M, et al. A randomized trial of pharmacogenetic warfarin dosing in naive patients with non-valvular atrial fibrillation. PloS ONE. 2015;10:e0145318.
Whirl-Carrillo M, McDonagh EM, Hebert JM, Gong L, Sangkuhl K, Thorn CF, et al. Pharmacogenomics knowledge for personalized medicine. Clin Pharmacol Ther. 2012;92:414–7.
Holbrook A, Schulman S, Witt DM, Vandvik PO, Fish J, Kovacs MJ, et al. Evidence-based management of anticoagulant therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e152S–84S.
Shaw K, Amstutz U, Kim RB, Lesko LJ, Turgeon J, Michaud V, et al. Clinical practice recommendations on genetic testing of CYP2C9 and VKORC1 variants in warfarin therapy. Ther Drug Monit. 2015;37:428–36.
Plumpton CO, Roberts D, Pirmohamed M, Hughes DA. A systematic review of economic evaluations of pharmacogenetic testing for prevention of adverse drug reactions. PharmacoEconomics. 2016;34:771–93.
You JH. Pharmacoeconomic evaluation of warfarin pharmacogenomics. Expert Opin Pharmacother. 2011;12:435–41.
Shendure J, Balasubramanian S, Church GM, Gilbert W, Rogers J, Schloss JA, et al. DNA sequencing at 40: past, present and future. Nature. 2017;550:345–53.
Kim S, Misra A. SNP genotyping: technologies and biomedical applications. Annu Rev Biomed Eng. 2007;9:289–320.
Kim DJ, Kim HS, Oh M, Kim EY, Shin JG. Cost effectiveness of genotype-guided warfarin dosing in patients with mechanical heart valve replacement under the fee-for-service system. Appl Health Econ Health Policy. 2017;15:657–67.
Verhoef TI, Redekop WK, Langenskiold S, Kamali F, Wadelius M, Burnside G, et al. Cost-effectiveness of pharmacogenetic-guided dosing of warfarin in the United Kingdom and Sweden. Pharm J. 2016;16:478–84.
You JH. Universal versus genotype-guided use of direct oral anticoagulants in atrial fibrillation patients: a decision analysis. Pharmacogenomics. 2015;16:1089–100.
Arwood MJ, Deng J, Drozda K, Pugach O, Nutescu EA, Schmidt S, et al. Anticoagulation endpoints with clinical implementation of warfarin pharmacogenetic dosing in a real-world setting: a proposal for a new pharmacogenetic dosing approach. Clin Pharmacol Ther. 2017;101:675–83.
Pirmohamed M, Burnside G, Eriksson N, Jorgensen AL, Toh CH, Nicholson T, et al. A randomized trial of genotype-guided dosing of warfarin. New Engl J Med. 2013;369:2294–303.
Shaw K, Amstutz U, Kim RB, Lesko LJ, Turgeon J, Michaud V, et al. Clinical practice recommendations on genetic testing of CYP2C9 and VKORC1 variants in warfarin therapy. Ther Drug Monit. 2015;37:428–36.
Acknowledgements
This work was supported by the National Natural Science Foundation of China (81773823, 81573463, 81403017) and the National Science and Technology Major Project (2017ZX09304014, 2016YFC0905000).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, X., Li, D., Wu, JC. et al. Precision dosing of warfarin: open questions and strategies. Pharmacogenomics J 19, 219–229 (2019). https://doi.org/10.1038/s41397-019-0083-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41397-019-0083-3
- Springer Nature Limited
This article is cited by
-
Association Between NAD(P)H Quinone Oxidoreductase 1 (NQO1) Gene Methylation/Expression and Bleeding Incidence Among an Iranian Population Undergoing Warfarin Therapy
Indian Journal of Hematology and Blood Transfusion (2024)
-
Machine learning models to predict the warfarin discharge dosage using clinical information of inpatients from South Korea
Scientific Reports (2023)
-
Warfarin dosing strategies evolution and its progress in the era of precision medicine, a narrative review
International Journal of Clinical Pharmacy (2022)