Abstract
Background
Shared decision-making (SDM) for metastatic prostate cancer (mPC) engages patients in the decision-making process and may be associated with better outcomes relative to physician- or patient-directed decision-making. We assessed the association between decision locus of control (DLOC) and patient-reported quality of life (QOL), functional outcomes, and decision satisfaction among mPC patients.
Methods
After a clinic visit in which a treatment decision was made (baseline), mPC patients completed DLOC and QOL surveys. QOL was re-assessed at 2- and 4-months post-baseline. Mean scores for each QOL dimension (physical, emotional, cognitive, social, and role functioning) were compared by DLOC group using mixed effects models. Patient preferences for DLOC and provider communication techniques were similarly collected via survey.
Results
Median age of participants (N = 101) was 69 years (range: 49-92); most were White (80%) and married (82%). 62% reported using SDM. At baseline, there were no differences in QOL dimensions between DLOC groups. At 4 months, patient-directed (p = 0.01) and SDM (p = 0.03) were associated with better physical functioning than physician-directed decision-making, and there was an indication of potentially greater decision satisfaction among patients who reported patient-directed (p = 0.06) or SDM (p = 0.10). SDM was the most reported preferred DLOC.
Conclusion
mPC patients reporting SDM had better physical functioning at 4 months than physician- or patient-directed decision-making, suggesting measurable benefit from patient involvement in decision-making. Future investigations of these associations in larger, more diverse populations can further clarify these previously unmeasured benefits of patient engagement in treatment decisions.
Similar content being viewed by others
Introduction
Prostate cancer remains the most common malignancy among American men and an important cause of cancer-related morbidity and mortality [1]. Despite continuing advances in care, metastatic prostate cancer (mPC) is an incurable disease, and the second leading cause of cancer death among men in the US. Recent advances have created a multitude of treatment options, each with a unique set of benefits and side effects. To date, there have been no direct comparisons of the various treatment options for mPC. This suggests differential benefit in terms of disease control, making treatment decision-making a complicated process for providers and patients. Thus, treatment decisions commonly depend on physician preferences and experience. An individualized approach to treatment decisions is preferred based on efficacy, as well as patient preferences, priorities, potential side effects, follow-up requirements, and cost of care [2]. This approach may be facilitated by shared decision-making (SDM) among patients, physicians, and caregivers, which has been identified by the National Academy of Medicine, the American Urological Association, and others as a priority method to improve the quality of cancer care in the US through patient engagement and autonomy.
Decision-making preferences are highly individualized and vary widely among cancer patients, with patients reporting heterogeneous preferences for decision-making roles [3,4,5,6]. Decision-making roles can be described via decision locus of control (DLOC) as primarily SDM, physician- or patient-directed. The extent that decision-making roles have impacted patient functional outcomes and decision satisfaction in mPC have not been described. Therefore, the primary goal of this study was to assess the impact of DLOC on functional outcomes and decision satisfaction for mPC patients. We hypothesized that SDM may positively impact functional outcomes and decision satisfaction. This study also assessed patients’ preferences for DLOC when making decisions regarding their treatment. We have also previously reported the communication techniques that patients, caregivers, and physicians felt aided decision-making, and this study further assessed patient preferences for communication techniques [7].
Materials and methods
Participants and procedures
We assessed DLOC following a clinic visit in which a treatment decision occurred (baseline), and assessed patient-reported functional outcomes at baseline, 2-months post-treatment decision, and 4-months post-treatment decision. We evaluated patient-reported preferences for DLOC among mPC patients following a clinic visit in which a treatment decision had occurred. Treatment decisions included any decision to change the treatment approach to the prostate cancer, associated pain or comorbidities, or to maintain the current treatment approach. This study was approved by the Institutional Review Board at Vanderbilt University Medical Center (VUMC; approval #161441) and Northwestern Memorial Hospital (NMH, approval #STU00206080). Between 2018 and 2020, patients with mPC were recruited from Genitourinary Oncology clinics at VUMC and NMH, with an accrual goal of 94 patients. Eligible patients spoke English, were able to recall a decision at a clinic visit within the preceding 48 h and signed informed consent to participate. There were no restrictions or requirements regarding prior local or systemic treatment exposure. Patients completed electronic surveys describing the decision-making process, decision satisfaction, and quality of life (QOL) outcomes via REDCap on tablets in clinic. Patient sociodemographic and clinical characteristics, including age, race/ethnicity, marital/partner status, self-reported health status (i.e., excellent, good, fair, or poor), and insurance status were collected by patient self-report and electronic medical record when possible to reduce missing data. The study was supported by a grant from the Department of Defense Prostate Cancer Research Program (PC150398).
Surveys
Decision locus of control
Patients were enrolled after completing a physician visit in which a treatment decision was made before leaving the clinic. Participants completed a survey describing the role they played in the decision using a modified version of the Control Preferences Scale [4, 8, 9], which has been used in assessments of decision making among patients with cancer and is reliable in defining decisional preferences in a unidimensional scale [10,11,12]. This modified version of the 5-item scale asks participants to describe decision roles as physician-directed (e.g., “Your doctors made the decision with little or no input from you”), SDM (e.g., “You and your doctors made the decisions together”), or patient-directed (e.g., “You made the decisions after seriously considering your doctor’s opinion”).
Quality of life
Patients completed the European Organization for Research and Treatment of Cancer Quality of Life of Cancer Patients (EORTC-QLQ-30) questionnaire at baseline immediately following a treatment decision, 2-months post-treatment decision, and 4-months post-treatment decision. The EORTC-QLQ-30 questionnaire is a validated study tool to evaluate patient functioning and provides scales in domains of physical, emotional, cognitive, social, and role functioning, with higher scores on each domain indicating better functioning [13].
Decision satisfaction
Patients completed the Satisfaction with Decisions survey regarding their current satisfaction with their decision at baseline immediately following a treatment decision, 2-months post-treatment decision, and 4-months post-treatment decision [14]. The survey explored how patients felt they were informed (i.e., “I am satisfied that I am adequately informed about the issues important to my decision”), consistency with personal values (i.e., “I am satisfied that my decision was consistent with my personal values”), expectations to carry out decision (i.e., “I expect to successfully carry out... the decision I made”), and overall satisfaction (i.e., “I am satisfied with my decision”).
Communication preference surveys
In addition to the responses regarding DLOC described above, participants completed surveys before leaving the clinic describing their preference for their DLOC. They were reminded of a recent treatment decision with the following prompt: “Consider a recent treatment decision that you made for your prostate cancer. Describe how you prefer to make treatment decisions”, and then provided with a modified version of the Control Preferences Scale [4, 8, 9]. This modified version of the 5-item scale classifies preferences for decision roles as physician-controlled (“You prefer that the doctors make the decision with little or no input from you.” or “You prefer that the doctors make the decision after seriously considering your opinion.”), SDM (“You prefer that you and your doctors made the decision together.”), or patient-controlled (“You prefer to make the decision after seriously considering your doctor’s opinion.” or “You prefer to make the treatment decision with little or no input from your doctors.”). Patients also completed the Communication Assessment Tool, a 15-item survey that is reliable and valid in identifying patient perceptions of physicians’ interpersonal and communication skills [15]. The analysis was modified by asking participants to identify the five most important things that physicians can do to help them make treatment decisions, and patients’ answers were ranked in order of most commonly identified.
Data analysis
Preferences
We used descriptive statistics to summarize patients’ sociodemographic characteristics, clinical factors, and participants’ preferences for DLOC. We used Fisher’s exact tests to evaluate the relationships between patients’ perceptions of DLOC and their sociodemographic characteristics including age, overall health status, and physician specialty. We used relative frequencies to rank the most identified communication techniques that physicians could use to help patients make treatment decisions. Finally, pairwise comparisons between pairs of proportions with correction for multiple testing and Fisher’s exact test were used to evaluate differences in relative frequencies of the communication techniques among DLOC preference groups.
Outcomes
We used descriptive statistics to summarize patients’ perceptions of DLOC. We examined the effects of decision-making on different functional and symptom domains, overall scores, and average satisfaction using a mixed effects model. Least-squared means of QOL dimensions were compared for each time point among DLOC groups to evaluate for associations. Overall health status was evaluated as a covariate for decision satisfaction.
Results
Participant Characteristics
Data from 101 patients in the QOL/satisfaction analysis and 103 patients in the preferences analysis were collected and are summarized in Table 1. Most patients were White, married, living with a spouse/partner, and had insurance.
QOL/Patient Functioning
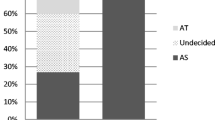
Patients reported their DLOC for the treatment decision that had occurred during their medical visit (Fig. 1). Patients then reported their QOL at baseline, 2 months, and 4 months after a treatment decision was made (Fig. 2). At 4 months post-treatment decision, physical functioning was significantly greater among patients who experienced a shared decision or patient-directed decision than among patients who experienced a physician-directed decision (p = 0.03 and p = 0.005, respectively). This effect was not seen at 2 months post-decision. There were no significant differences among DLOC groups for the other measures of patient functioning (social, cognitive, role, or emotional functioning) at either the 2-month or 4-month timepoint. All measures of functioning, including physical functioning, were similar among DLOC groups at baseline.
Decision Satisfaction
Patients reported their decision satisfaction at baseline, 2 months, and 4 months after a decision was made (Fig. 3). At 4 months post-treatment decision, there was an indication of potentially increased decision satisfaction among patients who experienced a shared decision or patient-directed decision compared with patients who experienced a physician-directed decision (p = 0.097 and p = 0.056, respectively). Decision satisfaction increased over time (from baseline to 2 months to 4 months) for both the SDM group and the patient-directed group, while satisfaction decreased over time for the physician-directed group. Decision satisfaction was similar among all DLOC groups at baseline. Notably, decision satisfaction was significantly associated with overall health scores reported by patients (p < 0.001).
Decision satisfaction measured via Satisfaction with Decisions survey (scale: 4 = “agree” that “I am satisfied with my decision”; 5 = “strongly agree” that “I am satisfied with my decision”) at baseline, 2 months, 4 months (Dashed = physician-directed; Dotted = shared decision-making; Solid = patient-directed).
Patient Preference for Decision Locus of Control and Physician Communication Style
Patients identified their preferences for DLOC during treatment decisions (Fig. 1). SDM was the most common patient preference (72%). The next most common preference was for patient-directed (18%), which was more common than physician-directed (11%). No patients reported a preference for a decision made with “little to no input” from the treating physician.
Patients also identified the most important communication techniques physicians could use to aid decision-making. The most important techniques in descending order of frequency were discussing follow-up plans (68%), involving patients as much as they wanted (52%), understanding patients’ health concerns (51%), speaking in terms patients could understand (50%), and giving as much information as patients wanted (48%). Patients with a preference for physician-directed decisions were less likely to rank “involving patients as much as they wanted” among their top five most important techniques compared with patients who preferred shared decisions (p = 0.041) or patient-directed decisions (p = 0.007). See Supplementary Information for detailed Table S1.
Discussion
This study investigated the impact of patients’ locus of control during a treatment decision on their QOL and decision satisfaction over time. Patients who experienced a shared decision or a patient-directed decision had significantly better physical functioning at 4 months post-decision than patients who experienced a physician-directed decision. Importantly, there were no significant differences in physical functioning among the DLOC groups at baseline. These findings suggest that patients who are more involved in their treatment decision-making may more successfully maintain their physical functioning than those who are less actively engaged. Patients with prostate cancer have a relatively high level of physical functioning compared with other malignancies, thus it is important for patients to maintain this high level of function rather than lose this ability. Therefore, active engagement in decision-making can increase QOL for patients. The Federal Drug Administration considers physical functioning and other EORTC QOL metrics in the regulatory review process for novel therapeutics, which speaks to the importance of maintaining QOL in patients undergoing cancer treatment [16].
Other QOL domains (i.e., social, emotional, cognitive, and role functioning) were not significantly associated with the degree of patient engagement in decision-making in this study. The underlying reasons for physical functioning potentially being affected by DLOC are unknown, but it may be related to heightened self-efficacy empowering patients to engage in decision-making and in activities that strengthen physical functioning. It is possible that the greater levels of pain reported by patients who reported physician-directed decisions were associated with poorer disease prognosis, more advanced disease, or other factors associated with declining physical function. Other QOL domains may be less dramatically affected by disease related decline than physical functioning. However, in separate therapeutic trials, emotional/social/cognitive/role functioning domains appeared to be affected by disease progression, suggesting that DLOC may be related to the effects seen in physical functioning [17].
Over time, decision satisfaction increased among patients who experienced a shared decision or a patient-directed decision. However, patients who reported experiencing a physician-directed decision exhibited declining satisfaction with their treatment decision. This trend suggests patients may be more satisfied with their treatment decisions in the long-term if they feel they had a more active role in the decision. Many patients with mPC will have inevitable declines in general health and wellbeing, and a subset will experience decreased decision satisfaction or regret [18]. Our study similarly found a significant positive association between overall health status and decision satisfaction. For patients experiencing declining health, it is possible they may come to regret their treatment plan if they felt the decision was made primarily by the physician, even if they did not initially feel negatively toward the decision [19]. Conversely, patients who are empowered to play an active role in decision-making and feel confident they made the best choice for themselves may maintain their satisfaction in the decision, despite declining health.
This study characterized patient preferences for DLOC and physician communication techniques. Most patients preferred a shared decision rather than a physician or patient-dominated decision-making process. Of those that did not prefer a shared decision, there was a greater preference for patient-directed compared with physician-directed decisions. While there is limited data regarding preferences for DLOC in mPC, our finding that the majority of patients prefer SDM is consistent with studies in other fields of oncology and beyond [20]. Other studies have suggested that younger generations value SDM more than the older populations that currently make up the majority of cancer patients. This indicates that collaborating with patients will likely become essential to the training and practice of early-career physicians [21].
The five most identified preferences for communication techniques reported by patients as important to aiding the decision-making process were as follows: discussing next steps, involving patients in decisions, understanding patients’ health concerns, speaking in patient-friendly terms, and sharing information as requested by patients. These are similar to those previously reported by patients, as well as caregivers, as being helpful based on their experiences making decisions [7]. These techniques are common examples of ways for physicians to demonstrate empathy, which has been correlated to patient perception of SDM. Others have stated that a patient’s perception of SDM may be more about feeling that the physician has heard and processed the patient’s cognitive and emotional needs, concerns, and preferences than about the patient actively deliberating over treatment options [22]. The proportion of patients valuing communication techniques largely did not differ significantly according to DLOC preference. However, patients who preferred a physician-directed decision were less likely to value “involving patients in decisions” compared with those who preferred shared or patient-directed decisions.
Our study has limitations that should be considered. First, the sample size was relatively small, particularly in patients with DLOCs other than SDM, but was identified as a sample size that was feasible to enroll and sufficient to identify clinically meaningful changes in QOL. Second, although participants were enrolled from two separate institutions, both have populations that are predominantly White and insured. Further, only patients who felt comfortable with reading English surveys were eligible to participate, which restricted participation from non-English speaking patients and limits generalizability. Finally, this study was designed as a relatively short-term longitudinal investigation. Whether these findings would change with longer follow up is unknown. Additional studies are needed to investigate these findings in larger and more diverse populations over a longer period.
In conclusion, our study suggests that greater patient involvement in decision-making may provide benefits to patients in the form of improved physical functioning and greater decision satisfaction. This finding is particularly notable given the recognition by the scientific community, including the Food and Drug Administration, of the importance of physical functioning on patient outcomes [22]. Our study identified techniques, such as asking degree of involvement desired and focus on follow-up, used by physicians that were most valued by patients to achieve shared decisions. Adoption of these often-simple techniques may improve outcomes in patients with mPC.
Disclosure
This paper was presented at the American Society of Clinical Oncology Genitourinary meeting as a poster presentation with interim findings.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
American Cancer Society. Cancer Facts & Figures 2022. Atlanta: American Cancer Society; 2022.
Oswald LB, Schumacher FA, Gonzalez BD, Moses KA, Penson DF, Morgans AK. What do men with metastatic prostate cancer consider when making treatment decisions? A mixed-methods study. Patient Prefer Adherence. 2020;14:1949–59.
Elkin EB, Kim SHM, Casper ES, Kissane DW, Schrag D. Desire for information and involvement in treatment decisions: elderly cancer patients’ preferences and their physicians’ perceptions. J Clin Oncol. 2007;25:5275–80.
Degner LF, Sloan JA. Decision making during serious illness: what role do patients really want to play? J Clin Epidemiol. 1992;45:941–50.
Keating NL, Guadagnoli E, Landrum MB, Borbas C, Weeks JC. Treatment decision making in early-stage breast cancer: should surgeons match patients’ desired level of involvement? J Clin Oncol. 2002;20:1473–1479.
Oswald LB, Kasimer R, Rappazzo K, Fought AJ, Penson DF, Morgans AK. Patient expectations of benefit from systemic treatments for metastatic prostate cancer. Cancer Med. 2020;9:980–7.
Schumacher FA, Helenowski IB, Oswald LB, Gonzalez BD, Benning JT, Morgans AK. Treatment decision-making in metastatic prostate cancer: perceptions of locus of control among patient, caregiver, and physician triads. Patient Prefer Adherence. 2022;16:235–44.
Hawley ST, Lantz PM, Janz NK, Salem B, Morrow M, Schwartz K, et al. Factors associated with patient involvement in surgical treatment decision making for breast cancer. Patient Educ Couns. 2007;65:387–95.
Kehl KL, Landrum MB, Arora NK, Ganz PA, van Ryn M, Mack JW, et al. Association of actual and preferred decision roles with patient-reported quality of care: shared decision making in cancer care. JAMA Oncol. 2015;1:50–58.
Degner LF, Kristjanson LJ, Bowman D, Sloan JA, Carriere KC, O’Neil J, et al. Information needs and decisional preferences in women with breast cancer. JAMA. 1997;277:1485–1492.
Beaver K, Luker KA, Owens RG, Leinster SJ, Degner LF, Sloan JA. Treatment decision making in women newly diagnosed with breast cancer. Cancer Nurs. 1996;19:8–19.
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European organization for research and treatment of cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365–76.
Holmes-Rovner M, Kroll J, Schmitt N, Rovner DR, Breer ML, Rothert ML, et al. Patient satisfaction with health care decisions: the Satisfaction with Decision scale. Med Decis Mak. 1996;16:58–64.
Bilodeau BA, Degner LF. Information needs, sources of information, and decisional roles in women with breast cancer. Oncol Nurs Forum. 1996;23:691–6.
Kluetz PG, O’Connor DJ, Soltys K. Incorporating the patient experience into regulatory decision making in the USA, Europe, and Canada. Lancet Oncol. 2018;19:e267–e274.
Resnick MJ, Penson DF. Quality of life with advanced metastatic prostate cancer. Urol Clin North Am. 2012;39:505–15.
Clark JA, Wray N, Brody B, Ashton C, Giesler B, Watkins H. Dimensions of quality of life expressed by men treated for metastatic prostate cancer. Soc Sci Med. 1997;45:1299–1309.
Clark JA, Wray N, Ashton CM. Living with treatment decisions: regrets and quality of life among men treated for metastatic prostate cancer. J Clin Oncol. 2001;19:72–80.
Nicolai J, Buchholz A, Seefried N, Reuter K, Härter M, Eich W, et al. When do cancer patients regret their treatment decision? A path analysis of the influence of clinicians’ communication styles and the match of decision-making styles on decision regret. Patient Educ Couns. 2016;99:739–46.
Schneider A, Korner T, Mehring M, Wensing M, Elwyn G, Szecsenyi J. Impact of age, health locus of control and psychological co-morbidity on patients’ preferences for shared decision making in general practice. Patient Educ Couns. 2006;61:292–8.
Saha S, Beach MC. The impact of patient-centered communication on patients’ decision making and evaluations of physicians: a randomized study using video vignettes. Patient Educ Couns. 2011;84:386–92.
U.S. Department of Health and Human Services FDA Center for Drug Evaluation and Research, U.S. Department of Health and Human Services FDA Center for Biologics Evaluation and Research & U.S. Department of Health and Human Services FDA Center for Devices and Radiological Health. Guidance for industry: patient-reported outcome measures: use in medical product development to support labeling claims: draft guidance. Health Qual Life Outcomes. 2006;4:79.
Acknowledgements
This work was supported by the Department of Defense Physician Research Training Award PC150398.
Funding
Department of Defense Physician Research Training Award PC150398 (PI Morgans).
Author information
Authors and Affiliations
Contributions
The authors confirm contribution to the paper as follows: study conception and design: AM, data collection: FS, AM, KM, analysis and interpretation of results: FS, IH, ZS, AM, draft manuscript preparation: FS, JB, LO, BG, KM, AM. All authors reviewed the results and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
BDG reports personal fees from SureMed Compliance, KemPharm, and Elly Health, Inc. unrelated to this work. All other authors declare no competing interests.
Ethics approval
This study was conducted in accordance with the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Schumacher, F.A., Helenowski, I.B., Sun, Z. et al. Treatment decision-making among patients with metastatic prostate cancer: Impact of decision locus of control on functional outcomes and decision satisfaction. Prostate Cancer Prostatic Dis 26, 201–206 (2023). https://doi.org/10.1038/s41391-023-00647-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-023-00647-5
- Springer Nature Limited
This article is cited by
-
Prostatectomy in oligometastatic prostate cancer: a call for high-quality evidence
Prostate Cancer and Prostatic Diseases (2024)