Abstract
This study aimed to explore the effects of a decision support intervention (DSI) and shared decision making (SDM) on knowledge, perceptions about treatment, and treatment choice among men diagnosed with localized low-risk prostate cancer (PCa). At a multidisciplinary clinic visit, 30 consenting men with localized low-risk PCa completed a baseline survey, had a nurse-mediated online DS session to clarify preference for active surveillance (AS) or active treatment (AT), and met with clinicians for SDM. Participants also completed a follow-up survey at 30 days. We assessed change in treatment knowledge, decisional conflict, and perceptions and identified predictors of AS. At follow-up, participants exhibited increased knowledge (p < 0.001), decreased decisional conflict (p < 0.001), and more favorable perceptions of AS (p = 0.001). Furthermore, 25 of the 30 participants (83 %) initiated AS. Increased family and clinician support predicted this choice (p < 0.001). DSI/SDM prepared patients to make an informed decision. Perceived support of the decision facilitated patient choice of AS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Currently, more than 90 % of all prostate cancer (PCa) cases are detected at a local and potentially curable stage, and the 5-year relative survival rate for these cases approaches 100 % [1]. Active treatment (AT) with surgery and/or radiation therapy constitutes the mainstay of therapy for the majority of men diagnosed with localized PCa [2, 3]. However, while potentially curative, these treatments can result in substantial morbidity, including sexual impotence, urinary incontinence, and injury to adjacent organs [4]. Active surveillance (AS) is another approach to treating patients with localized low-risk PCa that involves periodic monitoring of prostate-specific antigen (PSA) kinetics and prostate biopsy for with change to AT prompted by tumor progression or reclassification to more aggressive disease. Although the use of AS is increasing [5–8], most patients undergo AT, because of anxiety about their diagnosis, lack of knowledge about the risks and benefits of both AS and AT, and inadequate support for deliberation about treatment options [9–11]. Effective methods for providing decision support that facilitate shared decision making (SDM) are needed.
Lin et al. [12] reviewed studies of decision aids (DAs) for patients who faced treatment decisions about low-risk PCa. They found that providing patients with educational handouts, booklets, videos, etc. improved patient knowledge, decreased anxiety, and increased readiness to be involved in treatment decision making. The effect of DA exposure on treatment decisions was mixed, although there was evidence suggesting that patients who received DAs were less likely to undergo surgery than historical controls. A more recent meta-analysis on the effectiveness of traditional DAs in this patient population found mixed results related to their impact on knowledge, decisional conflict, and treatment choice [13].
Decision support interventions (DSIs) are interactive tools designed not only to educate patients about their choices, but also to generate information on patient preference that can be used in SDM [14]. Research on the effects of patient exposure to DSIs in PCa treatment decision making is limited. The study reported here, which was approved by the Thomas Jefferson University Institutional Review Board, aimed to explore the effects of a nurse-mediated online software application, known as the Decision Counseling Program© (DCP), on treatment decision making among men diagnosed with localized, low-risk PCa. For eligible men, treatment options consisted of AS or AT (radical prostatectomy or radiation therapy).
Patients and Methods
Study Eligibility
This study included men who were newly diagnosed with localized, low-risk PCa and were seen in the Thomas Jefferson University Multidisciplinary Genitourinary Oncology Center (MGOC) from October 2013 to December 2014 to discuss treatment options. To be eligible for participation, men had to be 18 or more years of age; be able to read and speak English; have clinical and biopsy features that suggested a favorable disease risk (i.e., PSA of less than or equal to 10 ng/ml, a clinical stage of less than or equal to T2a, a Gleason score of less than or equal to 6, no more than 3 positive biopsy cores from among 12 systematic cores (or ≤25 % of all biopsy cores), and less than or equal to 50 % tumor involvement in any one biopsy core); and have no prior treatment for PCa.
Participant Recruitment and Enrollment
On a weekly basis, a clinic nurse coordinator identified new patients who met eligibility criteria and were scheduled to visit the MGOC. At an early morning case conference, all cases to be seen that day were reviewed by the clinical team and initial treatment plans were discussed [15]. Patients who met eligibility requirements were referred to the research team (a research assistant and nurse educator trained in decision counseling). The research assistant met each patient at the clinic, explained the study, obtained informed consent, and provided a self-administered baseline survey.
Baseline Survey
The 15–20 min survey included an 8-item scale to assess the patient’s knowledge about PCa and treatment (α = 0.74). The survey also included items that assessed patient perceptions regarding PCa and treatment using 15 items based on the Preventive Health Model, or PHM [16, 17]. Each PHM item was scored on a 5-point Likert scale (1 = “strongly disagree,” 2 = “disagree,” 3 = “undecided,” 4 = “agree,” and 5 = “strongly agree”). Five PHM subscales (i.e., perceived susceptibility to aggressive PCa, salience and coherence of AS, worries and concerns about AS, AS response efficacy, and social support) were included on the survey. Twelve items from the decisional conflict scale were included, representing the following constructs: feeling uncertain, uninformed, unclear, and unsupported [18]. Lastly, the survey included items to assess participant sociodemographic background characteristics (i.e., age, race/ethnicity, education, and marital status).
Decision Support
Following survey completion, the nurse educator met each participant together with any accompanying companion, and initiated a decision counseling session. In the session, the nurse educator and participant reviewed a one-page educational summary that described AS and AT and compared the treatment options in terms of relative survival, side effects, and cost. Then, the nurse educator and patient accessed the online DCP and together completed a simple structured exercise to determine if the patient favored initiating AS (option 1) or having AT (option 2).
Specifically, the nurse educator asked the patient to identify in his own words factors that would influence his choice (decision factors) either to initiate AS (option 1) or undergo AT (option 2). The nurse educator entered verbatim text describing each factor into the program. Next, the nurse educator asked the patient to review his decision factors and select the top three factors that were most likely to affect his treatment decision. For these factors, the nurse encouraged the participant to indicate the importance of each factor (1.1 = not at all, 1.3 = a little, 1.5 = somewhat, 1.7 = much, 1.9 = very much, and 9.9 = overwhelming), and report the relative importance of each factor using a similar weighting scheme. Then, the nurse educator entered discrete and relative factor weights into the DCP, and used the program to generate a treatment preference score that indicated whether the patient preferred to initiate AS, was uncertain about his preference for AS versus AT, or preferred to have AT. The nurse educator printed out a copy of the summary page, which included text indicating the patient’s preference, top three decision factors, and displayed his treatment preference score in a bar graph. A copy of the summary form was provided to each man and to the clinical team for use in SDM in the subsequent encounter. As part of the multidisciplinary team approach, each patient met with a radiation oncologist and a urologist.
Follow-up Survey
At 30 days after the clinic visit, the study research assistant administered a follow-up telephone survey to participants. The survey included all knowledge, PHM, and decisional conflict scale items from the baseline survey. Furthermore, participants were asked to report their treatment status (initiated AS, neither AS or AT, and scheduled or had AT).
Statistical Analysis
Baseline survey data were inspected to generate frequencies of participant sociodemographic characteristics, knowledge, decisional conflict, and PHM measures. Participant knowledge was measured by summing the number of correct answers to the eight knowledge scale items. The internal consistency of each set of scale measures was evaluated using the Cronbach’s alpha reliability coefficient.
Change in knowledge between baseline and the follow-up survey was assessed using the paired t test. Changes in baseline to follow-up scores for the decisional conflict scale and subscales (uncertain, uninformed, unclear, and unsupported) and for the global PHM scale and subscales (susceptibility, salience and coherence, worries and concerns, response efficacy, and social support) were computed as the mean of all component questions. The mean and standard deviation of each scale and subscale were computed. Two susceptibility scale items, “I think it is likely that I will develop aggressive PCa in the future” and “I think that the chance that I will develop aggressive PCa is high” were reverse-coded. Similarly, both worries and concerns subscale items were reverse-scored. Paired t tests were used to assess significant changes in scale and subscale scores.
The relationship between the treatment preference score (dichotomized as prefers AS or equal preference for AS and AT versus prefers AT) and treatment status was summarized using frequencies and percentages and their independence tested by Fisher’s exact test. Similarly, the associations between treatment status and demographic characteristics were assessed using Fisher’s exact test. For each participant, changes from baseline to follow-up survey in knowledge score, decisional conflict, and PHM scores were summarized by mean and standard deviation and differences were assessed using t tests. The significance level for all tests was set in advance as α = 0.05. All statistical analyses were conducted using SAS version 9.4.
Results
Study Population
In 2013–2014, the research team approached 39 potentially eligible patients at the MGOC. Of those approached, 35 consented and enrolled in the study. Thirty patients completed a baseline survey, the DCP session, and the follow-up survey; four patients could not be contacted after the office visit; and one patient withdrew from the study. We completed the 180-day chart audit for 23 participants in the study; seven participants were lost to follow-up.
Participant Characteristics
Of the 30 participants, 22 were white, seven were African American, and one was of Asian descent (Table 1). Twelve of the men were under the age of 60, while 18 were 60 years of age or older. Twenty-four men had more than a high school education, and 23 were married or living with a partner.
Knowledge, Decisional Conflict, and PHM Measures
The internal consistency coefficients for the participant knowledge scale (alpha = 0.74), decisional conflict scale (alpha = 0.84) and subscales, the global PHM scale (alpha = 0.83), and subscales, showed that the knowledge, decisional conflict, and global PHM scales were highly reliable.
Table 2 shows that from the baseline to the follow-up survey, participant knowledge about treatment increased significantly (p < 0.001). In addition, overall decisional conflict and each of the decisional conflict subscale scores decreased significantly (p < 0.001). At 30 days, compared to baseline, the men were also significantly more likely to have an favorable overall perception of AS (p = 0.001); more likely to have higher levels of AS salience and coherence (p = 0.012), AS response efficacy (p = 0.014), and AS social support (p < 0.001); were significantly less likely to believe they had aggressive disease (p = 0.021); and were significantly less worried about developing aggressive prostate cancer (p = 0.030).
Treatment Preference and Treatment Status
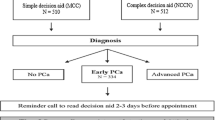
Findings obtained from the DCP session indicated that 8 (27 %) men preferred AS, 10 (33 %) were undecided about their treatment preference, and 12 (40 %) preferred AT. When the follow-up survey was administered, 25 (83 %) men said that they had decided to initiate AS and 5 (17 %) had decided to undergo AT (Fig. 1).
Predictors of Treatment
Data presented in Table 3 show that men who reported a greater change in perceived social support score were significantly more likely to initiate AS than AT (p < 0.001).
Discussion
In the past several years, AS has been recommended as a viable treatment option for men diagnosed with localized, low-risk PCa. During this time, DAs have been developed to educate men about their treatment options [19–21] and have shown to be effective in increasing patient knowledge while decreasing anxiety, decisional conflict, and regret [12–14, 22]. Recently, there has been increased attention on the development of DSIs that can be deployed in clinical practice settings to facilitate the engagement of patients and providers in SDM. In the study reported here, we successfully implemented a nurse-mediated online DSI in a multidisciplinary clinic setting and assessed the impact of the intervention on patients and treatment decision making.
In a cohort of patients with localized, low-risk PCa, decision support and SDM increased participant knowledge about available treatment options, lowered decisional conflict related to treatment decision making, and increased favorable perceptions about AS. We also observed that men felt significantly more supported in making a decision to initiate AS. These effects suggest that the intervention moved men towards being more receptive to AS and are consistent with previously reported DA research findings.
Novel features of the study include the use of a combined online DSI to clarify participant preference for AS and AT and patient-clinician SDM. At baseline, 27 % of study participants preferred AS while, at 30 days, 83 % reported that they had initiated AS. It appears that exposure to the combined intervention produced a substantial shift in treatment preference, as signaled by the high AS rates [3, 23, 24]. The strength of this effect is remarkable, given that prior studies have reported mixed or only modest effects of DAs on treatment decision making [12, 13]. We can hypothesize that a rise in knowledge about the treatment options, reduction in decisional conflict, increased favorable perceptions of AS, and the reinforcement of AS by clinicians during the physician-patient encounter may account for the high AS rate. Research is needed on a larger scale to sort out these effects, and to determine if decision support may have differential effects in population subgroups.
It is useful to note that the research team used self-reported baseline and follow-up survey data to measure the extent to which participant perceptions related to treatment changed in response to exposure to the combined intervention. While self-reported data of this type are useful in assessing intervention effects, it would be better to collect data to directly observe intervention effects during the SDM process.
Recent developments in genomic risk assessment may influence treatment decision making in this patient population. Such tests can predict risk for developing aggressive PCa and, potentially, reduce patient uncertainty about PCa aggressiveness. Recommendations for using such tests as part of routine care have been incorporated into treatment guidelines [25, 26]. In the future, the use of genomic risk assessment is expected to increase dramatically, a practice change that is likely to impact treatment choice among men with localized PCa. Research is needed to determine how decision support interventions like the DCP could be used to provide patients with information on personal risk, and how these interventions can be incorporated into practice to facilitate SDM about treatment.
Finally, there are several aspects of the study that limit generalizability. First, this was a one-arm, non-randomized study that included a small number of men. Second, men were recruited from a single multidisciplinary center at an urban, academic medical center, which may limit the applicability of our findings to the general population. As mentioned earlier, we only included 30 men in the study, limiting the power of our statistical analyses. Moreover, we relied on patient self-reported treatment status at the time of the 30-day follow-up survey when medical chart data was not available.
Conclusion
The implementation of a nurse-directed online DSI in a clinical setting for men diagnosed with localized, low-risk PCa boosted patient knowledge, reduced patient decisional conflict, and increased favorable patient perceptions related to treatment options. The AS rate was much higher than what is typically observed in practice.
References
American Cancer Society (2015) Cancer facts & figures 2015. American Cancer Society, Atlanta, GA
Welch HG, Albertsen PC (2009) Prostate cancer diagnosis and treatment after the introduction of prostate-specific antigen screening: 1986–2005. J Natl Cancer Inst 101:1325–3
Cooperberg MR, Broering JM, Carroll PR (2010) Time trends and local variation in primary treatment of localized prostate cancer. J Clin Oncol 28:1117–4
Chou R, Croswell JM, Dana T et al (2011) Screening for prostate cancer: a review of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med 155:762–771
Cooperberg MR, Carroll PR (2015) Trends in management for patients with localized prostate cancer, 1990–2013. JAMA 314:80–82
Ritch CR, Grave AJ, Keegan KA et al (2015) Increasing use of observation among men at low risk for prostate cancer mortality. J Urol 193:801–806
Weiner AB, Patel SB, Etzioni R et al (2015) National trends in the management of low and intermediate risk prostate cancer in the United States. J Urol 193:95–102
Womble PR, Montie JE, Ye Z (2015) Contemporary use of initial active surveillance among men in Michigan with low-risk prostate cancer. Eur Urol 67:44–50
Volk RJ, McFall SL, Cantor SB et al (2014) ‘It’s not like you just had a heart attack’: decision making about active surveillance by men with localized prostate cancer. Psychooncology 23:467–472
Xu J, Neale AV, Dailey RK et al (2012) Patient perspective on watchful waiting/active surveillance for localized prostate cancer. J Am Board Fam Med 25:763–770
Anandadas CN, Clarke NW, Davidson SE et al (2011) Early prostate cancer—which treatment do men prefer and why? BJU Int 107:1762–1768
Lin GA, Aaronson DS, Knight SJ et al (2009) Patient decision aids for prostate cancer treatment: a systematic review of the literature. CA Cancer J Clin 59:379–390
Violette PD, Agoritsas T, Alexander P et al (2015) Decision aids for localized prostate cancer treatment choice: systematic review and meta-analysis. CA J Clin 65:239–251
Stacey D, Légaré F, Col NF et al (2014) Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev 1, CD001431
Gomella LG, Lin J, Hoffman-Censits J et al (2010) Enhancing prostate cancer care through the multidisciplinary approach: a 15-year experience. J Oncol Pract 6:e5–e10
Vernon SW, Myers RE, Tilley BC (1997) Development and validation of an instrument to measure factors related to colorectal cancer screening adherence. Cancer Epidemiol Biomarkers Prev 6:825–832
Tiro JA, Vernon SW, Hyslop T et al (2005) Factorial validity and invariance of a survey measuring psychosocial correlates of colorectal cancer screening among African Americans and Caucasians. Cancer Epidemiol Biomarkers Prev 14:2855–2861
O’Connor AM (1995) Validation of a decision conflict scale. Med Decis Making 15:25–30
Wilt TJ (2014) Management of low risk and low PSA prostate cancer: long term results from the Prostate Cancer Intervention versus Observation Trial. Recent Results Cancer Res 202:149–169
Heidenreich BPJ, Bellmunt J et al (2013) EAU guidelines on prostate cancer. Part 1: screening, diagnosis, and local treatment with curative intent-update, 2013. Euro Urol 65:124–137
Hayes JH, Ollendorf DA, Pearson SD et al (2010) Active surveillance compared with initial treatment for men with low-risk prostate cancer: a decision analysis. JAMA 304:2373–2380
Christie DR, Sharpley CF, Bitsika V (2015) Why do patients regret their prostate cancer treatment? A systematic review of regret after treatment for localized prostate cancer. Psych-Oncol 24:1002–1011
Jang TL, Bekelman JE, Liu Y et al (2010) Physician visits prior to treatment for clinically localized prostate cancer. Arch Intern Med 170:440–450
Shappley WV, Kenfield SA, Kasperzyk JL et al (2009) Prospective study of determinants and outcomes of deferred treatment or watchful waiting among men with prostate cancer in a nationwide cohort. J Clin Oncol 27:4980–4985
National Comprehensive Cancer Network guidelines for prostate cancer (2015) Corrections to Version 1.2015 of the NCCN Guidelines for Prostate Cancer.
Chen RC, Rumble B, Loblaw DA et al. (2016) Active surveillance for the management of localized prostate cancer (Cancer Care Ontario Guideline): American Society of Clinical Oncology Clinical Practice Guideline Endorsement. J Clin Oncol doi: 10.1200/JCO.2015.65.7759.
Acknowledgment
This project was funded, in part, under a grant with the Pennsylvania Department of Health (SAP No. 41000062221). The Department specifically disclaims responsibility for any analyses, interpretations, or conclusions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved by the Thomas Jefferson University Institutional Review Board.
Rights and permissions
About this article
Cite this article
Myers, R.E., Leader, A.E., Censits, J.H. et al. Decision Support and Shared Decision Making About Active Surveillance Versus Active Treatment Among Men Diagnosed with Low-Risk Prostate Cancer: a Pilot Study. J Canc Educ 33, 180–185 (2018). https://doi.org/10.1007/s13187-016-1073-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-016-1073-7