Abstract
Background
The neutrophil-to-lymphocyte ratio (NLR) and the platelet-to-lymphocyte ratio (PLR), as markers of systematic inflammation response, have been reported to be indicators in metastatic castration-resistant prostate cancer (mCRPC), whereas their prognostic values remain conflict. This study was to assess the prognostic value of NLR and PLR in mCRPC patients and to assess the response of abiraterone or enzalutamide through using NLR and PLR.
Methods
Databases searching was conducted in the PubMed, EMBASE, Google Scholar, and the Cochrane Library for relevant published literature up to October 2019. Data extraction and quality evaluation were performed on the eligible studies. STATA 14.0 software was used to pooled hazard ratios (HRs) and their 95% confidence intervals (CIs) for overall survival (OS) and progression-free survival (PFS).
Results
A total of 3144 mCRPC patients were enrolled from 15 cohort studies in this meta-analysis. The pooled results demonstrated that elevated NLR had a significant association with inferior OS in mCRPC patients treated with abiraterone (HR = 1.63, 95% CI: 1.43–1.85, P < 0.001) and enzalutamide (HR = 1.48, 95% CI: 1.27–1.72, P < 0.001), whereas elevated NLR had no significant association with unfavorable PFS treated with abiraterone and enzalutamide, respectively. Elevated PLR had a significant association with an inferior OS (HR = 1.52, 95% CI: 1.16–1.98, P < 0.001) in mCRPC patients treated with abiraterone.
Conclusions
NLR and PLR were effective biomarkers for predicting prognosis in mCRPC patients and served as indicators of the efficacy of personalized treatment of mCRPC using abiraterone or enzalutamide. Future, more randomized control trials (RCTs) are needed to investigate the promising value of hematologic parameters.
Similar content being viewed by others
Introduction
Prostate cancer (PCa) is the most common cancerous malignancy and the leading cause of cancer-related mortality among men worldwide [1]. As diagnostic methods and surgical procedures have progressed, localized PCa, an early stage of the tumor, can have a favorable outcome [2]. For tumor heterogeneity, however, a large proportion of cases are prone to metastatic castration-resistant prostate cancer (mCRPC), and their prognosis is not satisfactory, in spite of previous treatment, such as androgen deprivation therapy or chemotherapy [3]. Lately, several novel agents, including docetaxel, cabazitaxel, sipuleucel-T [4], abiraterone [5], enzalutamide [6, 7], and radium-223 [8] have proved beneficial to the survival of mCRPC patients.
Abiraterone is a CYP17A1 enzyme inhibitor that restrains testosterone synthesis. Enzalutamide is an androgen receptor (AR) inhibitor that blocks nuclear translocation and AR biding [9]. Both are recommended to use either before or after chemotherapy to improve the survival of mCRPC patients. Nevertheless, the indicator of these two new hormonal agents remains unclear. Hence, effective prognostic biomarkers are needed for therapy management and to guide individual-based treatment.
Increasing evidence indicates that systemic inflammatory response plays an essential role in many solid tumors, including PCa [10]. Currently, two circulating hematologic parameters, the neutrophil-to-lymphocyte ratio (NLR) and the platelet-to-lymphocyte ratio (PLR), are recognized as hallmarks of malignancy progression and, as a research hotspot, have been reported to have prognostic value for mCRPC. The conclusions of various studies, however, are inconsistent [11]. What is more, therapy selection and medication sequences are still challenging issues for both clinicians and patients, putting better prognostic biomarkers in high demand. Nevertheless, no meta-analysis has yet evaluated the prognostic value of pretreatment NLR and PLR for mCRPC, and no specific indicator exists to evaluate the responses to abiraterone and enzalutamide. To fill this gap, we synthesized the relevant studies published in recent years and conducted this meta-analysis.
Methods
The present study was conducted following the guidelines of the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) [12].
Search strategy
Database searching was conducted in the PubMed, EMBASE, Google Scholar, and the Cochrane Library for relevant published literature up to October 2019. The language was restricted to English. The following keywords and medical subject headings were used as search terms: (“metastatic castration-resistant prostate cancer,” OR “mCRPC,”) AND (“neutrophil-to-lymphocyte ratio,” OR “NLR,” OR “platelet-to-lymphocyte ratio,” OR “PLR,”) AND (“abiraterone acetate,” OR “enzalutamide”). The literature searching process was performed iteratively until no additional article could be identified. The references cited in the literature were manually retrieved.
Selection criteria
Studies were eligible if they met the following defined criteria: (1) mCRPC patients were treated with abiraterone or enzalutamide prior to or post chemotherapy; (2) they were cohort studies of the evaluated prognostic value of pretreatment NLR or PLR and reported survival outcomes including overall survival (OS) and progression-free survival (PFS). OS was defined as the time from the start of abiraterone or enzalutamide until death from any cause; PFS was defined as the time from the start of abiraterone or enzalutamide until disease progression or death from any cause or last tumor evaluation; (3) the original hazard ratio (HR) with a 95% confidence interval (CI) could be extracted from sufficient information. Duplicate studies, reviews, case reports, comments, letters, unpublished studies, abstracts of conferences, animal experiments, and incomplete or erroneous data were excluded. Radiographic-PFS and prostate-specific antigen (PSA)-PFS were also excluded.
Data extraction
Two investigators (YPG and TYT) independently extracted and cross-checked the following data: first author, publication year, nation, region, duration time, data source, study design, sample size, mean age, hormonal agents, sequence, median follow-up, analysis mode, NLR cutoff value, PLR cutoff value, survival outcome, and quality scores. Engauge Digitizer software was used to digitize and extract the relevant survival data of the Kaplan–Meier curves. In case of a disagreement, discrepancies were resolved through discussion or third-party ruling.
Quality evaluation
Two investigators (YPG and HYX) independently evaluated eligible studies using the Newcastle–Ottawa Scale (NOS) quality assessment tool. Each cohort study included was assessed by three categories: selection, comparability, and outcome. A study was awarded a maximum of one star for each numbered item within the selection and outcome categories. A maximum of two stars could be given for the comparability category. Up to nine stars could be awarded. Each star represented one score. Studies with scores above 6 were regarded as high-quality. In case of a disagreement, discrepancies were resolved through discussion or third-party ruling.
Statistical analysis
STATA 14.0 software was used to conduct the present meta-analysis. HRs with 95% CIs were pooled to evaluate survival values. The I2 statistic and Cochrane Q test were used to evaluate the heterogeneity of the selected studies. An α value equal to 0.1 and a P value smaller than 0.05 were considered statistically significant. An I2 greater than 50% was considered a significant level of heterogeneity. The fixed-effect model was used to calculate the pooled effect when a Pheterogeneity value greater than 0.1 or an I2 statistic was equal to or smaller than 50%; otherwise, the random effect model was used. Sensitivity analysis was performed to assess the stability of the pooled results by omitting any single study in sequence. Egger’s tests were used to test publication bias, a P value greater than 0.05 indicating negligible potential publication bias.
Results
Search results
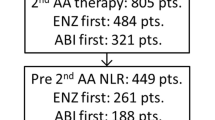
The flow chart (Fig. 1) illustrates the literature selection process. The initial searching retrieved a total of 94 studies including 89 studies form database searching and five studies were identified through other sources. Forty studies remained after duplicated studies were removed, and 17 studies were excluded after scanning their titles and abstracts. Full-text article assessments for eligibility were conducted in 23 studies, eight of which studies were excluded due to five being reviews, case reports, and comments, two lacking available data, and one having an overlapping subject. Eventually, 15 studies were eligible and included in the qualitative synthesis [11, 13,14,15,16,17,18,19,20,21,22,23,24,25,26]. All included studies were retrospective cohorts written in English.
Characteristics of eligible studies
Table 1 summarizes the general characteristics of the fifteen eligible cohort studies [11, 13,14,15,16,17,18,19,20,21,22,23,24,25,26]. A total of 3144 mCRPC patients were included in the present meta-analysis, the mean age of whom ranged from 42.8 to 92 years old. The sample size ranged from 101 to 872 patients. The publication year ranged from 2014 to 2019, the duration time ranged from 2014 to 2018, and the median follow-up time ranged from 0.3 to 55 months. The overall quality of the eligible studies was good, and the range of NOS scores being 6–9, with an average score of 7.5 (Table 2). Five articles came from Asia (Japan [13, 16], Korea [17], China [25], and Turkey [21]) and ten from non-Asian regions (Italy [15, 18, 23], France [14], Spain [19], Germany [20, 22], America [24, 26], and Canada [11]). Ten studies investigated the agent response of abiraterone [11, 13, 14, 18,19,20,21,22, 24, 25], and five studies [15,16,17, 23, 26] investigated the agent response of enzalutamide. Fifteen studies evaluated NLR [11, 13,14,15,16,17,18,19,20,21,22,23,24,25,26], of which the cutoff values ranged from 2.14 to 5. Three studies evaluated PLR [18, 19, 21] of which the cutoff values ranged from 150 to 210. Fifteen studies reported on OS and four studies reported on PFS. Four studies provided univariate analysis [14, 18, 19, 22], five studies provided multivariate analysis [13, 15, 16, 25, 26], and six provided both univariate and multivariate analysis modes [11, 17, 20, 21, 24].
The prognostic value of the neutrophil-to-lymphocyte ratio (NLR) on overall survival (OS) in mCRPC
Forest plots (Fig. 2a, b) shows the pooled results. Ten studies demonstrated that elevated NLR had a significant association with inferior OS in mCRPC patients treated with abiraterone (HR = 1.63, 95% CI: 1.43–1.85, P <0.001) with slight heterogeneity (I2 = 47%, Pheterogeneity = 0.049) [11, 13, 14, 18,19,20,21,22, 24, 25]. Similarly, five studies demonstrated that elevated NLR had a significant association with inferior OS in mCRPC patients treated with enzalutamide (HR = 1.48, 95% CI: 1.27–1.72, P < 0.001) with significant heterogeneity (I2 = 59.1%, Pheterogeneity = 0.044) [15,16,17, 23, 26].
Subgroup analyses were performed for OS. For mCRPC patients using abiraterone (Fig. 3a–c: (a) region, (b) analysis mode, (c) cutoff), the results showed that elevated NLR predicted inferior OS in Asian patients (HR = 2.54, 95% CI: 1.38–4.65, P = 0.003), multivariate analysis (HR = 1.76, 95% CI: 1.46–2.11, P < 0.001), and NLR cutoff >3 (HR = 1.84, 95% CI: 1.46–2.33, P < 0.001). Similarly, for mCRPC patients using enzalutamide (Fig. 3d, e: (d) region, (e) analysis mode), the pooled results showed that elevated NLR predicted inferior OS in non-Asian patients (HR = 1.53, 95% CI: 1.21–1.93, P < 0.001) and univariate analysis (HR = 2.07, 95% CI: 1.59–2.70, P < 0.001). The pooled results were shown in Table 3.
The prognostic value of the neutrophil-to-lymphocyte ratio (NLR) on progression-free survival (PFS) in mCRPC
Forest plots (Fig. 4a, b) shows the pooled results. Two studies demonstrated that elevated NLR had no significant association with PFS in mCRPC patients treated with abiraterone (HR = 1.62, 95% CI: 0.81–3.26, P = 0.176) with significant heterogeneity (I2 = 71.5%, Pheterogeneity = 0.061) [20, 21]. Similarly, two studies demonstrated that elevated NLR had no significant association with inferior OS in mCRPC patients treated with enzalutamide (HR = 1.55, 95% CI: 0.98–2.45, P < 0.001) with significant heterogeneity (I2 = 89.9%, Pheterogeneity = 0.002) [15, 23].
The prognostic value of the platelet-to-lymphocyte ratio (PLR) in mCRPC
Forest plots (Fig. 5) shows the pooled results. Three studies demonstrated that elevated PLR had a significant association with inferior OS in mCRPC patients treated with abiraterone (HR = 1.52, 95% CI: 1.16–1.98, P < 0.001) with slight heterogeneity (I2 = 4.1%, Pheterogeneity = 0.352) [18, 19, 21].
Sensitivity analysis and publication bias
A sensitivity analysis was performed to assess the stability of the pooled results by omitting any single study in sequence. The sensitivity analysis results demonstrated that the pooled HRs for OS and PFS did not significantly change, suggesting the robustness of the results (Fig. 6a, b). Publication bias was assessed by Egger’s test. A study was considered to have significant publication bias when P < 0.05. OS of mCRPC patients treated with abiraterone (P = 0.111) and enzalutamide (P = 0.391) for NLR, respectively, and the OS (P = 0.441) for PLR. The results of Egger’s test did not indicate and publication bias in the present meta-analysis (Fig. 6c, d).
Discussion
Currently, mCRPC is a global cause of one of the highest mortality rates across the world, threatening male populations everywhere but especially in Western countries [1]. As a novel generation of hormonal agents, abiraterone and enzalutamide have been reported to prolong the survival of mCRPC patients [27]. However, despite the emergence of these new drugs, the prognosis of mCRPC remains inadequate, as the responses of patients to these new agents is still unclear. Previous meta-analyses have focused on the correlations between CRPC and hematologic parameters, but their conclusions have been inconsistent. Therefore, the present study conducted a comprehensive systematic review and meta-analysis to assess the precise values of NLR and PLR in mCRPC patients treated with abiraterone or enzalutamide and thus provide valuable information and optimized choices to clinicians and patients.
The main finding of this meta-analysis demonstrated that elevated NLR was significantly associated with inferior OS in mCRPC patients treated with abiraterone or enzalutamide, whereas elevated NLR had no significant correlation with unfavorable PFS. Similarly, increasing PLR was associated with poor OS in mCRPC patients treated with abiraterone. In addition, according to subgroup analyses, an elevated NLR was more specific to predict an inferior prognosis in Asian patients of mCRPC treated with abiraterone than non-Asian patients, whereas, an elevated NLR appeared to be a stronger predictor of risk in non-Asian patients treated with enzalutamide. An NLR cutoff value >3 had a more significant prognostic value than a cutoff value ≤3, which indicated that a higher NLR cutoff was more specific to predict a poor prognosis in patients of mCRPC treated with abiraterone. Due to insufficient study data, the relationship between PLR and PFS could not be estimated. It is worth notice that the PREVAIL study prognostic model demonstrated that NLR acted as an independent prognostic factor for OS in mCRPC during enzalutamide treatment but not predictive factor [26], the incorporation of NLR may prove useful for risk stratification in mCRPC patients. Intriguingly, Loubersac et al. suggested that baseline NLR may predict response to abiraterone in mCRPC, however, the changes in NLR could not hold significant value during treatment to predict subsequent response to continued therapy [14].
Some past meta-analyses have also investigated hematologic parameters [28,29,30,31]. Gu et al. [32], for instance, demonstrated that elevated NLR predicted poor OS and PFS in 16,266 patients with prostate cancer. Interestingly, Li et al. [33] investigated the prognostic significance of PLR in urological cancers and found that elevated PLR was negatively related to OS in urological cancers, except for bladder cancer. These studies reported that elevated NLR or PLR levels were significantly associated with the inferior survival outcomes (OS, PFS, RFS, and cancer-specific survival (CSS)) of prostate cancer patients (localized PCa or CRPC), whereas the correlation between mCRPC and survival outcomes has not been investigated synthetically. In addition, the prognostic values of NLR and PLR in gauging responses to specific agents, including abiraterone or enzalutamide, have also not been evaluated. In contrast to those meta-analyses, the present study mainly focused on NLR and PLR values by connecting the survival outcomes of mCRPC patients and their responses to abiraterone or enzalutamide. The present study also included more updated, eligible studies that could provide the multivariate HRs, as data are more reliable through multivariate analysis adjusting.
The systemic inflammatory response has been considered as a hallmark of cancer [10, 34, 35]. Neutrophils, lymphocytes, platelets, and monocytes from peripheral blood all play roles in the systemic inflammatory response. Lately, the most evaluated indices are NLR, PLR, and the lymphocyte-to-monocyte ratio [36, 37]. Accumulating evidence shows these ratios to reliable prognostic factors of the survival of many solid tumors, including non-small-cell lung cancer [38], breast cancer [39], melanoma [40], colorectal cancer [41], hepatocellular carcinoma [42], prostate cancer [22], bladder cancer [43], and others. Unlike abiraterone, enzalutamide is not taken with prednisone, which might alter NLR values by redistributing lymphocytes in the bone marrow, lymph nodes, and spleen by reducing and accelerating the release of neutrophils from the bone marrow to the peripheral blood [7]. Nonetheless, the mechanisms underlying the mutual effects of elevated NLR and PLR on the inferior oncologic outcomes of mCRPC patients have remained indistinct.
Inflammation exerts a crucial role in oncogenesis, progression, and metastasis by facilitating angiogenesis, proliferation, and antiapoptosis [44]. Tumor cells attract pro-inflammatory cells into the tumor microenvironment by secreting a variety of chemokines [10]. Neutrophils act as a significant factor not only in promoting an array of cytokines such as IL-1β, IL-6, tumor necrosis factor, or granulocyte colony-stimulating factor secreting but also in facilitating angiogenesis and vascular endothelial growth production and subsequently stimulating tumor cells growth [34]. On the contrary, lymphocytes play a crucial role in regulating the immunologic antitumor activity, meaning that a decreased lymphocyte count may indicate tumor cells escaping from the normal immune system, thus worsening the survival outcomes of cancer patients. In Brief, the inflammatory response is characterized by increasing neutrophil-dependent levels accompanied by decreasing lymphocyte-mediated levels. For one thing, platelets accelerate tumor aggressiveness by deriving cytokines, such as platelet-derived growth factor and vascular endothelial growth factor, and promoting cancer cell adhering to the vascular endothelium; for another thing, platelets might interact with tumor cells through their ligands and help guard tumor cells from the elimination of immune system, which are regarded as correlations with inferior cancer prognosis [35]. NLR and PLR, therefore, seem to reflect a systemic inflammatory response to cancer progression leading to pronounced ratios in advanced cancer. NLR and PLR can thus provide Supplementary Information in therapeutic surveillance and decision-making regarding treatment changes regarding mCRPC. The present study supports the use of pretreatment NLR and PLR in mCRPC, along with other hematologic parameters and physical functional status, providing effective estimates of host response in determining long-term survival.
Several limitations of this study should be acknowledged. First, relevant studies were scarce, so we could not acquire robust conclusions in some endpoint analyses. Second, CSS, biochemical recurrence-free survival, and disease-free survival, essential outcomes for cancer survival analysis, were not pooled due to a lack of sufficient survival data. In addition, we lacked research from Southern America and Oceania, shrinking the number of included studies. Third, searching only relevant studies published in English may have excluded studies with negative results published in other languages. Fourth, the cutoff values of NLR and PLR varied among the eligible studies, ranging from 2.14 to 5 and 150 to 210, respectively. This heterogeneity might impede the clinical application of these ratios. Accordingly, more credible evidence is needed to identify the optimal cutoff values of these hematologic parameters. Fifth, the NLR and PLR values were derived from peripheral blood and were thus easily affected by patients’ elementary conditions such as age, tumor burden, histological features, stage of disease, infection, inflammatory disease, chronic disease, specific medications, and so on. Sixth, only retrospective cohort studies were included in this study. We, therefore, interpreted the results of the present meta-analysis with caution.
In the future, more randomized control trials (RCTs) and wider-ranging researches are pressing needed to study the prognostic role of hematologic parameters in predicting the survival of mCRPC patients and the therapeutic evaluation of abiraterone and enzalutamide.
Conclusions
In summary, hematologic parameters, including NLR and PLR, can be promising biomarkers for the prognosis of mCRPC, and pretreatment NLR and PLR can provide useful information for individual-based treatment by reflecting patient responses to abiraterone and enzalutamide. In the future, more RCTs and large sample sizes are called for to confirm the potentially profound values of hematologic parameters.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69:7–34.
Mottet N, Bellmunt J, Bolla M, Briers E, Cumberbatch MG, De Santis M, et al. EAU-ESTRO-SIOG guidelines on prostate cancer. Part 1: screening, diagnosis, and local treatment with curative intent. Eur Urol. 2017;71:618–29.
Cornford P, Bellmunt J, Bolla M, Briers E, De Santis M, Gross T, et al. EAU-ESTRO-SIOG guidelines on prostate cancer. Part II: treatment of relapsing, metastatic, and castration-resistant prostate cancer. Eur Urol. 2017;71:630–42.
Handy CE, Antonarakis ES. Sipuleucel-T for the treatment of prostate cancer: novel insights and future directions. Future Oncol. 2018;14:907–17.
Ryan CJ, Smith MR, de Bono JS, Molina A, Logothetis CJ, de Souza P, et al. Abiraterone in metastatic prostate cancer without previous chemotherapy. N Engl J Med. 2013;368:138–48.
Higano C. Enzalutamide, apalutamide, or darolutamide: are apples or bananas best for patients? Nat Rev Urol. 2019;16:335–6.
Schalken J, Fitzpatrick JM. Enzalutamide: targeting the androgen signalling pathway in metastatic castration-resistant prostate cancer. BJU Int. 2016;117:215–25.
Parker C, Nilsson S, Heinrich D, Helle SI, O’Sullivan JM, Fosså SD, et al. Alpha emitter radium-223 and survival in metastatic prostate cancer. N Engl J Med. 2013;369:213–23.
Antonarakis ES, Lu C, Wang H, Luber B, Nakazawa M, Roeser JC, et al. AR-V7 and resistance to enzalutamide and abiraterone in prostate cancer. N Engl J Med. 2014;371:1028–38.
Shaul ME, Fridlender ZG. Tumour-associated neutrophils in patients with cancer. Nat Rev Clin Oncol. 2019;16:601–20.
Templeton AJ, Pezaro C, Omlin A, McNamara MG, Leibowitz-Amit R, Vera-Badillo FE, et al. Simple prognostic score for metastatic castration-resistant prostate cancer with incorporation of neutrophil-to-lymphocyte ratio. Cancer. 2014;120:3346–52.
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;350:g7647.
Yasui M, Hasegawa Y, Kawahara T, Kumano Y, Miyoshi Y, Matsubara N, et al. Baseline neutrophil-to-lymphocyte ratio predicts the prognosis of castration-resistant prostate cancer treated with abiraterone acetate. Mol Clin Oncol. 2018;8:592–4.
Loubersac T, Nguile-Makao M, Pouliot F, Fradet V, Toren P. Neutrophil-to-lymphocyte ratio as a predictive marker of response to abiraterone acetate: a retrospective analysis of the COU302 study. Eur Urol Oncol. 2019;1:e144.
Conteduca V, Crabb SJ, Jones RJ, Caffo O, Elliott T, Scarpi E, et al. Persistent neutrophil to lymphocyte ratio >3 during treatment with enzalutamide and clinical outcome in patients with castration-resistant prostate cancer. PLoS ONE. 2016;11:e0158952.
Kumano Y, Hasegawa Y, Kawahara T, Yasui M, Miyoshi Y, Matsubara N, et al. Pretreatment neutrophil to lymphocyte ratio (NLR) predicts prognosis for castration resistant prostate cancer patients underwent enzalutamide. Biomed Res Int. 2019;2019:9450838.
Choi SY, Ryu J, You D, Jeong IG, Hong JH, Ahn H, et al. Prognostic factors of oncologic outcomes in metastatic chemotherapy-naive castration-resistant prostate cancer treated with enzalutamide in actual clinical practice in East Asia. Urol Oncol. 2018;36:401 e411–401 e418.
Lolli C, Caffo O, Scarpi E, Aieta M, Conteduca V, Maines F, et al. Systemic immune-inflammation index predicts the clinical outcome in patients with mCRPC treated with abiraterone. Front Pharmacol. 2016;7:376.
Lozano Martinez AJ, Moreno Cano R, Escobar Paramo S, Salguero Aguilar R, Gonzalez Billalabeitia E, Garcia Fernandez R, et al. Platelet-lymphocyte and neutrophil-lymphocyte ratios are prognostic but not predictive of response to abiraterone acetate in metastatic castration-resistant prostate cancer. Clin Transl Oncol. 2017;19:1531–6.
Boegemann M, Schlack K, Früchtenicht L, Steinestel J, Schrader AJ, Wennmann Y, et al. A prognostic score for overall survival in patients treated with abiraterone in the pre- and post-chemotherapy setting. Oncotarget. 2019;10:5082–91.
Onal C, Sedef AM, Kose F, Oymak E, Guler OC, Sumbul AT, et al. The hematologic parameters in metastatic castration-resistant prostate cancer patients treated with abiraterone acetate. Future Oncol. 2019;15:1469–79.
Boegemann M, Schlack K, Thomes S, Steinestel J, Rahbar K, Semjonow A, et al. The role of the neutrophil to lymphocyte ratio for survival outcomes in patients with metastatic castration-resistant prostate cancer treated with abiraterone. Int J Mol Sci. 2017;18:380.
Conteduca V, Caffo O, Galli L, Maugeri A, Scarpi E, Maines F, et al. Association among metabolic syndrome, inflammation, and survival in prostate cancer. Urol Oncol. 2018;36:240 e241–240 e211.
Schiff JP, Cotogno P, Feibus A, Steinwald P, Ledet E, Lewis B, et al. Early prostate-specific antigen response post-abiraterone as predictor of overall survival in metastatic castrate-resistant prostate cancer. BMC Cancer. 2019;19:524.
Fan L, Wang X, Chi C, Wang Y, Cai W, Shao X, et al. Prognostic nutritional index predicts initial response to treatment and prognosis in metastatic castration-resistant prostate cancer patients treated with abiraterone. Prostate. 2017;77:1233–41.
Armstrong AJ, Lin P, Higano CS, Sternberg CN, Sonpavde G, Tombal B, et al. Development and validation of a prognostic model for overall survival in chemotherapy-naive men with metastatic castration-resistant prostate cancer. Ann Oncol. 2018;29:2200–7.
Litwin MS, Tan HJ. The diagnosis and treatment of prostate cancer: a review. JAMA. 2017;317:2532–42.
Guo J, Fang J, Huang X, Liu Y, Yuan Y, Zhang X, et al. Prognostic role of neutrophil to lymphocyte ratio and platelet to lymphocyte ratio in prostate cancer: a meta-analysis of results from multivariate analysis. Int J Surg. 2018;60:216–23.
Peng H, Luo X. Prognostic significance of elevated pretreatment systemic inflammatory markers for patients with prostate cancer: a meta-analysis. Cancer Cell Int. 2019;19:70.
Wang Z, Peng S, Xie H, Guo L, Jiang N, Shang Z, et al. Neutrophil-lymphocyte ratio is a predictor of prognosis in patients with castration-resistant prostate cancer: a meta-analysis. Cancer Manag Res. 2018;10:3599–610.
Yin X, Xiao Y, Li F, Qi S, Yin Z, Gao J. Prognostic role of neutrophil-to-lymphocyte ratio in prostate cancer: a systematic review and meta-analysis. Medicine. 2016;95:e2544.
Gu X, Gao X, Li X, Qi X, Ma M, Qin S, et al. Prognostic significance of neutrophil-to-lymphocyte ratio in prostate cancer: evidence from 16,266 patients. Sci Rep. 2016;6:22089.
Li DY, Hao XY, Ma TM, Dai HX, Song YS. The prognostic value of platelet-to-lymphocyte ratio in urological cancers: a meta-analysis. Sci Rep. 2017;7:15387.
Ohno Y. Role of systemic inflammatory response markers in urological malignancy. Int J Urol. 2019;26:31–47.
Shaul ME, Fridlender ZG. Cancer-related circulating and tumor-associated neutrophils—subtypes, sources and function. FEBS J. 2018;285:4316–42.
Li M, Deng Q, Zhang L, He S, Rong J, Zheng F. The pretreatment lymphocyte to monocyte ratio predicts clinical outcome for patients with urological cancers: a meta-analysis. Pathol Res Pr. 2019;215:5–11.
Caglayan V, Onen E, Avci S, Sambel M, Kilic M, Oner S, et al. Lymphocyte-to-monocyte ratio is a valuable marker to predict prostate cancer in patients with prostate specific antigen between 4 and 10 ng/dl. Arch Ital Urol Androl. 2019;90:270–5.
Diem S, Schmid S, Krapf M, Flatz L, Born D, Jochum W, et al. Neutrophil-to-Lymphocyte ratio (NLR) and Platelet-to-Lymphocyte ratio (PLR) as prognostic markers in patients with non-small cell lung cancer (NSCLC) treated with nivolumab. Lung Cancer. 2017;111:176–81.
Guo W, Lu X, Liu Q, Zhang T, Li P, Qiao W, et al. Prognostic value of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio for breast cancer patients: an updated meta-analysis of 17079 individuals. Cancer Med. 2019;8:4135–48.
Ferrucci PF, Ascierto PA, Pigozzo J, Del Vecchio M, Maio M, Antonini Cappellini GC, et al. Baseline neutrophils and derived neutrophil-to-lymphocyte ratio: prognostic relevance in metastatic melanoma patients receiving ipilimumab. Ann Oncol. 2016;27:732–8.
Haram A, Boland MR, Kelly ME, Bolger JC, Waldron RM, Kerin MJ. The prognostic value of neutrophil-to-lymphocyte ratio in colorectal cancer: a systematic review. J Surg Oncol. 2017;115:470–9.
Yang T, Zhu J, Zhao L, Mai K, Ye J, Huang S, et al. Lymphocyte to monocyte ratio and neutrophil to lymphocyte ratio are superior inflammation-based predictors of recurrence in patients with hepatocellular carcinoma after hepatic resection. J Surg Oncol. 2017;115:718–28.
Lucca I, Jichlinski P, Shariat SF, Roupret M, Rieken M, Kluth LA, et al. The neutrophil-to-lymphocyte ratio as a prognostic factor for patients with urothelial carcinoma of the bladder following radical cystectomy: validation and meta-analysis. Eur Urol Focus. 2016;2:79–85.
Dupre A, Malik HZ. Inflammation and cancer: what a surgical oncologist should know. Eur J Surg Oncol. 2018;44:566–70.
Acknowledgements
We greatly acknowledge Prof. Qianyun Tang, from Central South University, for her excellent advice on the paper.
Funding
This study was funded by the National Natural Science Foundation of China (Grant Number: 81772754) and the Guangdong Provincial Natural Science Foundation-Major Basic Research and Cultivation Project, China (Grant Number: 2017A030308009).
Author information
Authors and Affiliations
Contributions
Conceptualization: YG and HX. Methodology: YG, YF, and GL. Writing, editing, and revision: YG. Supervision and review: JP.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Guan, Y., Xiong, H., Feng, Y. et al. Revealing the prognostic landscape of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in metastatic castration-resistant prostate cancer patients treated with abiraterone or enzalutamide: a meta-analysis. Prostate Cancer Prostatic Dis 23, 220–231 (2020). https://doi.org/10.1038/s41391-020-0209-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-020-0209-3
- Springer Nature Limited
This article is cited by
-
Analysis of the immune-inflammatory indices for patients with metastatic hormone-sensitive and castration-resistant prostate cancer
BMC Cancer (2024)
-
Prognostic value of the pretreatment systemic immune-inflammation index in patients with prostate cancer: a systematic review and meta-analysis
Journal of Translational Medicine (2023)
-
Neutrophil to lymphocyte ratio (NTLR) predicts local control and overall survival after stereotactic body radiotherapy (SBRT) in metastatic sarcoma
Scientific Reports (2023)
-
Comprehensive analysis of tumor mutation burden and immune microenvironment in prostate cancer
Clinical and Translational Oncology (2022)
-
Changes in neutrophile-to-lymphocyte ratio as predictive and prognostic biomarker in metastatic prostate cancer treated with taxane-based chemotherapy
Discover Oncology (2022)