Abstract
Purpose
Recently neutrophil–lymphocyte ratio (NLR) and platelet–lymphocyte ratio (PLR) have been reported to be inflammatory parameters that confer poorer outcome in metastatic castration-resistant prostate cancer (mCPRPC). However, these ratios have not been analyzed in patients treated with abiraterone acetate. We explored the relationship between different values of PLR and NLR and survival in mCPRCP treated with abiraterone and their possible relation with a prostate specific antigen (PSA) response.
Methods
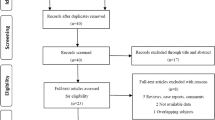
We retrospectively analyzed 101 patients with mCRPC treated with abiraterone from January of 2012 to November of 2015 in two different hospitals. A cut-off value of 5 for NLR and 150 for PLR were used to compare survival by Kaplan–Meier method. Moreover, an association between these cut-off values and the PSA response was analyzed by a χ 2 test.
Results
In the case of NLR, the median DFS were 12, 1 months for NLR <5 and 7 months for NLR ≥5, p = 0.061. The median OS were 23.9 months for NLR <5 and 16.3 months for NLR ≥5, p = 0.046. In the case of PLR, the median DFS were 11.8 months for PLR <150 and 10.6 months for PLR ≥150, p = 0.549. The median OS were 27.4 months for PLR <150 and 15.9 months for PLR ≥150, p = 0.005. It was not observed a correlation between the different cut-off values of PLR or NLR and a PSA response ≥25% (p = 0.31).
Conclusions
It is shown a better prognostic relationship between PLR and NLR low values and OS that is statistically significant in mCPRC patients treated with abiraterone. Furthermore, it was not shown a relation between PLR and NLR values and PSA response.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Several new agents have been shown to prolong survival and quality-of-life of patients who have been diagnosed of metastatic castration-resistant prostate cancer (mCRPC) before and after chemotherapy, including abiraterone, enzalutamide, radium-223, sipuleucel-T and cabazitaxel [1,2,3,4,5].
Abiraterone acetate is a CYP17 inhibitor and was shown to improve overall survival post-chemotherapy and pre-chemotherapy. Subsequently, it was shown to prolong radiographic progression-free survival, a longer period of time to start opioids and a longer period of time to start chemotherapy in patient’s chemo-naive [1, 2].
Despite the increased number of novel therapies, the prognosis, however, is still poor for mCRPC. Therefore, an accurate prognostic model is important in informing patients, selecting individualized treatment, and making a proper surveillance program. Tumor staying, PSA levels, PSA doubling time, and Gleason Score are conventionally used to stratify patients in terms of prognosis. Also relevant metabolic factors, such as platelet count, alkaline phosphatase, hemoglobin, and albumin are reported to be associated with prognosis of prostate cancer and are enrolled into the predictive models in some studies [6, 7].
Systemic inflammation response has been associated with poor outcome independent of tumor stage. [8, 9]. It can be measured by neutrophil, lymphocyte and platelet count, neutrophil–lymphocyte ratio (NRL), platelet–lymphocyte ratio (PLR) and Glasgow Prognostic Score (GPS), that have been reported to have prognostic value [10]. In several studies, The NRL measured is associated with overall and cancer specific mortality [11].
Moreover, cancer-associated systemic inflammation is likely to interfere with effective treatments due to the interaction between the systemic inflammation and the inhibition of cytochrome P450, which is known to participate in the inactivation and activation of anticancer drugs.
Recently, neutrophil to lymphocyte ratio (NLR) and platelet to lymphocyte ratio (PLR) have been reported to be inflammatory parameters that influence the prognosis in prostate cancer [10,11,13]. There are also data showing significant differences in prognosis between different levels of NLR in mCPRC treated with docetaxel and cabazitaxel [5, 14, 15]. However, currently, there are no predictive markers of response to these agents or abiraterone acetate, and the optimal drug sequencing in mCRPC is still controversial.
The primary objective of this study was to identify differences in prognosis between different levels of NLR and PLR, and to determine if these were predictive of the PSA response, so we could interpret these ratios, NLR and PLR, as predictive of response to abiraterone acetate.
Methods
Study design
We retrospectively analyzed 101 patients with mCRPC treated with abiraterone acetate from two different hospitals, from January of 2012 to November of 2015. All patients had a histologically or cytologically confirmed adenocarcinoma of the prostate, PSA progression according to Prostate Cancer Clinical Trials Working Group 2 (PCWG2) or radiographic progression suitable for metastasis according to the RECIST guidelines with or without PSA progression. Every patient had an Eastern Cooperative Oncology Group (ECOG) performance status grade of 0 or 1 to be able to receive abiraterone.
All patients received abiraterone acetate 1000 mg plus prednisone 10 mg daily. Bone metastases were found in all patients, and visceral metastasis in 14 patients.
All patients were treated with hormonal therapy consisted in LH-RH agonists. Forty patients were treated with docetaxel previous to abiraterone acetate with a dose of 70–75 mg/m2 every 3–4 weeks with 10 mg of prednisolone daily and 61 patients did not receive chemotherapy.
Clinical evaluation
All data of the patients, including pathological, clinical, radiological, biochemical and hematological data, were assessed retrospectively using clinical records. NLR and PLR ratios were evaluated in the blood tests that had been taken one week prior to the start of the treatment with abiraterone.
Statistical analysis
Collected data were analyzed and displayed in SPSS v.22 and Microsoft Excel 14.5. Overall survival (OS) and the disease-free survival(DFS) were analyzed by Kaplan–Meier method comparing different cut-off values for PLR and NLR obtained from data (cut-off value of 5 for NLR and 150 for PLR). Differences in DFS and OS were performed for the different groups depending on the PLR and NLR cut-off values, by Long-Rank test and p < 0.05 was considered statically significant.
In addition, a PSA response greater than 25% and a PSA response greater than 50% were considered. PSA responses were analyzed depending on the NLR and PLR. Moreover, a possible relation between the PSA responses and NLR, (NLR ≥ 5 and NLR < 5) and PLR (PLR ≥ 150 and PLR < 150) were performed by a χ 2 test.
Results
101 patients treated with abiraterone acetate were analyzed. The median age of patients at the start of treatment was 73 years (range 50–92 years). Seventy-five patients left the treatment due to disease progression or death.
The mean DFS was 11.3 months (CI 95% 9.6–12.8 months) and the median 9.6 months (CI 95% 6.7–12.4 months) (Fig. 1). The mean OS according to the Kaplan–Meier method was 23.6 months (CI 95% 20.7–26.5 months) and the median 21.7 months (CI 95% 17.8–25.5 months) (Fig. 2).
Association between PLR and NLR and survival
In the case of NLR, patients with and elevated NLR (≥5) showed a shorter DFS, mean 7.7 vs 12.1 months and median 7.0 vs 11.1 months, p = 0.061 Log Rank test (Fig. 3).
And a shorter OS, mean 16.3 vs 23.9 months and median 12.8 vs 21.7 months, p = 0.046 Log Rank test (Fig. 4).
In the case of PLR, patients with and elevated PLR (≥150) showed a shorter DFS, mean 10.6 vs 11.8 months and median 7.1 vs 10.3 months, p = 0.549 Log Rank test (Fig. 5).
And a shorter OS, mean 17.5 vs 25.9 months and median 15.9 vs 27.4 months, p = 0.005 Log Rank test (Fig. 6).
Both cases (PLR and NLR) showed a better prognosis in terms of OS with lower values (PLR < 150 and NLR < 5) that was statistically significant. Lower values also showed an increase in DFS but these differences were not statistically significant.
In the case of PLR, an increase of 8.4 months in the median OS was found in the group of PLR <150 (p = 0.005). NLR <5 showed an increase of 7.6 months in the median OS (p = 0.046).
Association between PLR and NLR and PSA response
Thirty-six patients showed a PSA response higher than 25% of its initial value (32 of these higher than 50%). A benefit in DFS and OS was observed in patients with a PSA response in our sample that was statistically significant. The mean DFS in patients with a PSA response and without a PSA response were 14.7 months(CI 95% 12.3–17.2 months) and 8.1 months (CI 95% 6.1–10.1) respectively, p < 0.001 Log Rank (Fig. 7) and the mean OS were 28.9 months (CI 95% 24.9–32.9 months) and 16.8 months(CI 95% 14.0–19.7) respectively, p < 0.001 Log Rank test (Fig. 8).
A correlation between PSA response ≥25% or PSA response ≥50% and the PLR or NLR values were studied. Despite the benefit observed in patients that experimented a PSA response in terms of DFS and OS, It was not observed a correlation between the different cut-off values of PLR or NLR and a PSA response ≥25%, in the χ 2 test (p = 0.31).
Discussion
In the present study, we investigated the effect of high PLR and NLR on survival in 101 patients with mCRPC who were treated with abiraterone acetate, and the relationship between these ratios values and PSA response. The PLR and NLR are easily reproducible markers of systemic inflammation that can be calculated from routinely available data without the need for increased time or cost. Total blood cell count is a simple and cheap routine test, which gives us the parameters to calculate NLR and PLR.
Several studies have evaluated the prognostic role of the NLR and PLR in different tumors, and also mCRPC. Cancer-related inflammation is considered a hallmark of progressive malignancy [16]. In the tumor microenvironment, sustained inflammation contributes to proliferation and survival of malignant cells, angiogenesis, metastasis, subversion of adaptive immunity, and reduced response to therapies. Furthermore, cancer-related inflammation is thought to be the result of genetic instability, with increased production of inflammatory mediators leading to tumor progression [17].
Neutrophils and platelets have a significant impact on the tumor microenvironment, and mediate many processes associated with tumor progression through their production of cytokines and chemokines, such as VEGF, a pro-angiogenic circulating molecule. In addition, intratumoral infiltration of neutrophils was shown to stimulate tumor invasion [18].
Several new agents were shown to prolong the survival of patients with mCRPC before and after chemotherapy, including abiraterone acetate [1,2,3,4]. Baseline NRL (<3) was a valid prognosis biomarker in mCRPC, and was associated with survival, PSA and RECIST responses in metastatic CRPC patients treated with cabazitaxel as second-line chemotherapy [5]. Leibowitz-Amit et al. reported that lower pretreatment baseline NRL (>5) was associated with the PSA response and OS in metastatic CRPC patients treated with abiraterone acetate [19]. Akihisa Yao et al. reported that a lower pretreatment baseline NLR (>3.5) was associated with a better OS and PFS in patients treated with docetaxel [14]. So it is shown that NRL may be associated with an independent poor prognostic impact in post-docetaxel patients with mCRPC. In our study, we tried to find a predictive role of NRL, and our finding was a better OS and PFS in the NRL <5 group as well as literature.
Sumbul et al. [20] investigated the response rate between pretreatment NLR and the response to docetaxel chemotherapy. This study showed no correlation between the response to docetaxel, but showed reduction in the PSA levels in the NLR <3 group significantly higher than NRL <3. By contrast, in our study, we did not find a correlation between the different cut-off values of PLR or NLR and a PSA response ≥25%. This result can be associated with the underpowered size of our study.
Diletta Bianchini et al. [21] reported 141 patients with abiraterone and showed radiological disease stabilization beyond PSA progression in a high proportion of, CRPC patients treated with abiraterone. So at this point, we could interpret that PSA is not the best marker of response to abiraterone acetate.
Concerning PLR, whereas Turkmen et al. discovered PLR was a better marker in predicting inflammation severity [11]. Neofytou et al. [22] used data from 17 studies which included 4968 CRC patients to investigate the prognostic value of PRL and showed that elevated PRL was associated with poor tumor stage, pT category, and degree of differentiation and suggested that PRL may predict a poor prognosis in CRC. Besides, Templeton et al. did a meta-analysis and found PLR’s significant role in the diagnosis of various kinds of solid tumors (e.g. Gastric cancer, lung cancer and hepatic carcinoma), and PLR was generally high in tumor patients, and patients with higher value of PLR had lower survival [11]. Our study showed a better prognosis in terms of OS with lower values (PRL < 150) that was statistically significant.
The underlying mechanisms responsible for the role of PLR in CRC have not yet been elucidated, but recent experimental and clinical data may provide several potential explanations. An elevated PLR represents an increased number of platelets and/or a decreased number of lymphocytes, and elevated platelets could promote metastatic potential of tumor cells in several biological pathways. Platelets could secrete cellular growth factors and then stimulate tumor angiogenesis and growth [22].
Conclusions
It is shown a prognostic relation between low values of PLR and NLR and OS and PFS for patients with mCPRC who received abiraterone acetate. Furthermore, it was not shown a relation between PLR and NLR values and PSA response in our sample, however, PSA levels could be questionable as a response marker to abiraterone acetate at this point.
References
Fizazi K, Scher HI, Molina A, et al. Abiraterone acetate for treatment of metastatic castration-resistant prostate cancer: final overall survival analysis of the COU-AA-301 randomised, double-blind, placebo-controlled phase 3 study. Lancet Oncol. 2012;13(10):983–92.
Ryan CJ, Smith MR, de Bono JS, et al. Abiraterone in metastatic prostate cancer without previous chemotherapy. N Engl J Med. 2013;368(2):138–48.
Beer TM, Armstrong AJ, Rathkopf DE, Loriot Y, Sternberg CN, Higano CS, et al. Enzalutamide in metastatic prostate cancer before chemotherapy. N Engl J Med. 2014;371(5):424–33.
Parker C, Heinrich D, O’Sullivan JM, et al. Overall survival benefit of radium-223 chloride (AlpharadinTM) in the treatment of patients with symptomatic bone metastases in Castration-resistant Prostate Cancer (CRPC): a phase III randomized trial (ALSYMPCA). Eur J Cancer. 2011;47(Suppl. 2):3.
De Bono JS, Oudard S, Ozguroglu M, et al. Prednisone plus cabazitaxel or mitoxantrone for metastasis castration-resistant prostate cancer progressing after docetaxel treatment: a randomized open-label trial. Lancet. 2010;376(9747):1147–54.
Kattan MW, Cuzick J, Fisher G, et al. Nomogram incorporating PSA level to predict cancer-specific survival for men with clinically localized prostate cancer managed without curative intent. Cancer. 2008;112(1):69–74.
Halabi S, Small EJ, Kantoff PW, et al. Prognostic model for predicting survival in men with hormone-refractory metastatic prostate cancer. J Clin Oncol. 2003;21(7):1232–7.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646–74.
Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140:883–99.
Ferro M, De Cobelli O, Buonerba C, et al. Modified Glasgow Prognostic Score is associated with risk of recurrence in bladder cancer after radical cystectomy: a multicenter experience D. Medicine (Baltimore). 2015;94(42):e1861.
Templeton AJ, McNamara MG, Seruga B, et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst. 2014;106(6):dju124.
Turkmen K, Erdur FM, Ozcicek F, Ozcicek A, Akbas EM, Ozbicer A, Demirtas L, Turk S, Tonbul HZ. Platelet-to-lymphocyte ratio better predicts inflammation than neutrophil-to-lymphocyte ratio in end-stage renal disease patients. Hemodial Int. 2013;17:391–6.
Templeton AJ, Pezaro C, Omlin A, et al. Simple prognostic score for metastatic castration-resistant prostate cancer with incorporation of neutrophil-to-lymphocyte ratio. Cancer. 2014;120(21):3346–52.
Yao A, Sejima T, Iwamoto H, et al. High neutrophil-to-lymphocyte ratio predicts poor clinical outcome in patients with castration-resistant prostate cancer treated with docetaxel chemotherapy. Int J Urol. 2015;22(9):827–33.
Nuhn P, Vaghasia AM, Goyal J, et al. Association of pretreatment neutrophil-to-lymphocyte ratio (NLR) and overall survival (OS) in patients with metastatic castration-resistant prostate cancer (mCRPC) treated with first-line docetaxel. Br J Urol Int. 2014;114(6b):E11–7.
Colotta F, Allavena P, Sica A, et al. Cancer-related inflammation, the seventh hallmark of cancer: links to genetic instability. Carcinogenesis. 2009;30(7):1073–81.
Guthrie GJ, Charles KA, Roxburgh CS, et al. The systemic inflammation-based neutrophil–lymphocyte ratio: experience in patients with cancer. Crit Rev Oncol Hematol. 2013;88(1):218–30.
Gregory AD, Houghton AM. Tumor-associated neutrophils: new targets for cancer therapy. Cancer Res. 2011;71(7):2411–6.
Leibowitz-Amit R, Templeton AJ, Omlin A, et al. Clinical variables associated with PSA response to abiraterone acetate in patients with metastatic castration-resistant prostate cancer. Ann Oncol. 2014;25(3):657–62.
Sumbul AT, Sezer A, Abali H, et al. Neutrophil-to-lymphocyte ratio predicts PSA response, but not outcomes in patients with castration-resistant prostate cancer treated with docetaxel. Int Urol Nephrol. 2014;46(8):1531–5.
Bianchini D, Kaur Sandhu S, Mulick A, Zivi A, Mezynski J, Mukherji D, et al. Durable radiologic and clinical disease stability beyond PSA progression in patients with metastatic castration-resistant prostate cancer (mCRPC) treated with abiraterone acetate (AA). J Clin Oncol. 2012;30(suppl):abstr 4553.
Neofytou K, Smyth EC, Giakoustidis A, Khan AZ, Cunningham D, Mudan S. Elevated platelet to lymphocyte ratio predicts poor prognosis after hepatectomy for liver-only colorectal metastases, and it is superior to neutrophil to lymphocyte ratio as an adverse prognostic factor. Med Oncol. 2014;31(10):239.
Acknowledgements
This author’s work was independent of the funders.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no potential conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Each participant signed an institutional informed consent form in accordance with national and institutional guidelines.
Rights and permissions
About this article
Cite this article
Lozano Martínez, A.J., Moreno Cano, R., Escobar Páramo, S. et al. Platelet–lymphocyte and neutrophil–lymphocyte ratios are prognostic but not predictive of response to abiraterone acetate in metastatic castration-resistant prostate cancer. Clin Transl Oncol 19, 1531–1536 (2017). https://doi.org/10.1007/s12094-017-1699-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-017-1699-x