Abstract
Longitudinal connectivity studies might guide our understanding of the underlying neurodegenerative processes. We report the results of a longitudinal study in patients at different stages of Parkinson’s disease (PD), who performed motor and non-motor evaluations and serial resting state (RS) functional MRI (fMRI). Cluster analysis was applied to demographic and clinical data of 146 PD patients to define disease subtypes. Brain network functional alterations were assessed at baseline in PD relative to 60 healthy controls and every year for a maximum of 4 years in PD groups. Progression of brain network changes were compared between patient clusters using RS fMRI. The contribution of network changes in predicting clinical deterioration was explored. Two main PD clusters were identified: mild PD (86 patients) and moderate-to-severe PD (60 patients), with the latter group being older and having earlier onset, longer PD duration, more severe motor, non-motor and cognitive deficits. Within the mild patient cluster, two clinical subtypes were further identified: mild motor-predominant (43) and mild-diffuse (43), with the latter being older and having more frequent non-motor symptoms. Longitudinal functional connectivity changes vary across patients in different disease stages with the coexistence of hypo- and hyper-connectivity in all subtypes. RS fMRI changes were associated with motor, cognitive and non-motor evolution in PD patients. Baseline RS fMRI presaged clinical and cognitive evolution. Our network perspective was able to define trajectories of functional architecture changes according to PD stages and prognosis. RS fMRI may be an early biomarker of PD motor and non-motor progression.
Similar content being viewed by others
Introduction
Parkinson’s disease (PD) is the second most common neurodegenerative disorder after Alzheimer’s disease and is characterized by motor symptoms such as bradykinesia, rigidity, tremor and postural instability [1]. PD patients also experience a multitude of non-motor symptoms such as cognitive impairment, disorder of mood and affect, dysautonomia, disorders of sleep, hyposmia, and visual hallucinations [1]. Non-motor symptoms become increasingly prevalent over the course of the illness and are a major determinant of impaired quality of life and progression of disability [1]. However, both motor and non-motor symptoms are variable between individual patients [1]. Rate of disease progression is also heterogeneous [2].
Pathologically, the cardinal features of PD are the loss of dopaminergic neurons in the nigrostriatal system, and the widespread intracytoplasmic Lewy bodies and Lewy neurites, the main component of which is α-synuclein [3]. Emerging evidence suggests that α-synuclein pathology may propagate across interconnected networks throughout the nervous system [4]. Magnetic resonance imaging (MRI) provides biomarkers that can objectively detect the widespread consequences of network changes in neurodegenerative diseases [5]. Resting state (RS) functional MRI (fMRI) allows for the exploration of the reorganization of neural pathways and functional disruptions. RS fMRI studies in PD described the presence of abnormalities in a large number of widely distributed regions within and beyond the basal ganglia-thalamo-cortical and cerebello-thalamo-cortical circuits [6,7,8]. Brain functional connectivity (FC) alterations have been related to motor and cognitive deficits, indicating a potential contribution to clinical progression [6,7,8]. However, a large heterogeneity among studies was revealed dependent upon not only the use of different fMRI techniques but also the inclusion of patients at different disease stage as FC can present with opposite patterns along the disease course [6,7,8]. In addition, the presence of diverse motor symptoms, cognitive deficits and other non-motor manifestations may correspond to specific patterns of RS functional changes [6,7,8].
As a result of advances in computational neuroscience, it is now possible to model and characterize topologically, from a local to a global level, the intricate functional integrative bases that support brain behavior [9]. Using graph analysis, brain network (the “connectome”) can be regarded as a graph of nodes, representing specialized neural elements, linked by edges, representing measures of structural or FC between nodes [9]. These techniques can provide a detailed description on how the disease alters brain organization [10] and, more recently, allowed to make hypotheses about underlying physiopathology [11]. Recent cross-sectional analyses of the functional brain connectome in PD patients suggested an altered global architecture with reduced local efficiency and global integration [12,13,14,15,16,17,18,19,20] starting from the earliest disease phase [15, 21, 22]. Regional decreases and increases in functional interactions were reported in sensorimotor, default mode (DMN), frontal, and temporal-occipital networks [16, 18,19,20,21]. Although altered functional organization of brain network correlated with PD motor severity and cognitive impairment [14, 16,17,18,19, 21, 22], how functional disorganization relates to different PD subtypes and disease progression is still not known.
Longitudinal connectivity studies have the potential to provide a characterization of disease progression related to clinical phenotype, and might guide our understanding of the underlying neurodegenerative processes. Longitudinal data assessing the dynamic evolution of FC in relation to PD heterogeneity are critically missing. To the best of our knowledge, only 3 studies so far attempted to investigate FC changes over time in small and clinically heterogeneous PD samples using two time point RS fMRI [23,24,25].
The present study reports the results of an ongoing longitudinal project in PD patients at different disease stage assessed using comprehensive motor and non-motor evaluations and serial RS fMRI scans. Cluster analysis was applied to define disease subtypes based on demographic characteristics, disease duration, motor severity, and certain non-motor features at study entry. The aims of our study were to: (i) investigate brain network functional alterations at baseline in a large cohort of PD patients stratified in different subtypes; (ii) compare longitudinal trends of progression of brain network changes between PD subtypes using multiple serial RS fMRI scans; and (iii) explore the contribution of network changes in predicting clinical deterioration.
Methods
Participants and cluster/subtype definition
154 patients with PD were prospectively recruited within the framework of an ongoing longitudinal project. Patients received a comprehensive evaluation including clinical, cognitive/behavioral and MRI assessments at study entry and every year for a maximum of 4 years (Supplementary Fig. 1). Sixty age- and sex-matched healthy controls performed clinical, cognitive and MRI assessments at baseline. Supplementary material reports details on inclusion/exclusion criteria and clinical and cognitive/behavioral evaluations.
Eight PD patients were excluded from the analysis due to incomplete MRI or movement artifacts (Supplementary Fig. 1). Cluster analysis based on k-medoids method for data partitioning was applied on the remaining 146 patients using the Gower distance calculated for baseline data on demographic/general clinical information (age, sex, education, age at onset, disease duration, family history), motor symptoms/signs (Hoehn and Yahr [HY], Unified Parkinson’s Disease Rating Scale [UPDRS] II-III total, UPDRS III axial and bradykinesia, presence of dyskinesia and fluctuations, Freezing of Gait-Questionnaire, motor phenotype), levodopa equivalent daily-dose (LEDD), cognition and mood (Addenbrooke’s Cognitive Examination [ACE]-revised, Hamilton Depression Rating Scale [HDRS], Hamilton Anxiety Rating Scale [HAMA], Apathy Evaluation Scale), and the presence of other non-motor manifestations (hallucinations, REM Sleep Behavior Disorder [RBD], orthostatic hypotension, and olfactory, gastrointestinal, urinary, sexual dysfunctions). Missing data were imputed using the Random Forest algorithm. According to the clustering, the highest silhouette index was estimated with respect of two identified PD clusters (mild and moderate-to-severe PD). Within the mild PD cluster, two clinical subtypes were further identified: mild motor-predominant and mild-diffuse.
Local ethical standards committee on human experimentation approved the study protocol and all participants provided written informed consent prior to study inclusion.
MRI analysis
Baseline and follow-up MRI scans were acquired on the same 1.5 Tesla scanner. Supplementary material reports the MRI protocol and details on RS fMRI pre-processing and construction of brain networks. Head motion parameters (mean absolute cumulative translation and mean rotation) are reported in the Supplementary Table 1. Global and mean lobar functional network characteristics were explored using the Brain Connectivity Matlab toolbox (http://www.brain-connectivity-toolbox.net). 83 regions of interest from both hemispheres were grouped into six anatomical macro-areas (hereafter referred to as brain lobes): temporal, parietal, occipital, fronto-insular, basal ganglia, and sensorimotor areas. Network metrics (nodal strength, characteristic path length, local efficiency, clustering coefficient) were assessed to characterize the topological organization of global brain and lobar networks [26, 27]. Network-based statistic (NBS) [28] assessed FC in PD subtypes and healthy controls.
Statistical analysis
Demographic and clinical general data were compared between groups using ANOVA models or Fisher exact test. For clinical motor, non-motor and cognitive variables, Poisson regressions, which accounted for overdispersion, were performed. Global and lobar nodal metrics were compared between groups using age- and sex-adjusted ANOVA models. Changes in continuous variables over time were assessed by the annualized mean rate of change (%), calculated from the regression slope of a generalized linear model for longitudinal data (using Poisson as link function) for clinical continuos variables and from the regression slope of ANOVA model for longitudinal data for MRI variables, using time as continuous variable. Test for linear trend (associated with the annualized mean rate) was estimated in PD groups and group-by-time interaction was assessed to evaluate longitudinal between-group differences. Such models were adjusted for age, sex and LEDD (treated as time-varying covariate) in case of MRI variables. p-values were adjusted for multiple comparisons controlling the False Discovery Rate at level 0.05 using Benjamini-Hochberg step-up procedure. Two-sided p-value < 0.05 was considered for statistical significance. Analyses were performed using SAS (Release 9.4, SAS Institute, Cary, NC, USA).
NBS [28] compared FC in PD subtypes and controls at baseline at p < 0.05. A corrected p-value was calculated using age- and sex-adjusted permutation analyses (10000 permutations). Patient-group comparisons were adjusted also for LEDD. Linear mixed-effects models were implemented in NBS to investigate FC changes over time. The effects of age, sex, baseline LEDD and LEDD changes, and individual follow-up duration were considered in the regression model.
Correlations between functional measures and global composite outcomes (GCOs) were tested (see Supplementary material for GCO definition) at baseline. Partial Spearman correlations were assessed between baseline fMRI metrics (both nodal and NBS-connectivity values), which were found to be different between PD subgroups and healthy controls, and the four baseline GCOs. Analysis was adjusted for age, sex and baseline LEDD. Furthermore, to test the effect of brain network changes on clinical progression in patient groups, correlations between functional measures and GCO changes were explored (see Supplementary material for GCO changes definition). Using SAS, partial Spearman correlations were assessed between changes over time of the nodal metrics presenting significant trend within patient groups or a differential trend between groups, and the four GCO changes. Analysis was adjusted for age, sex, baseline LEDD, LEDD changes, and individual follow-up duration. Mean FC values of each connection presenting changes over time were obtained from the FC matrices for each subject at each timepoint and their changes over time were correlated with the four GCO changes.
Finally, in each PD group, linear regression models in SAS assessed the association between baseline fMRI metrics (both nodal and NBS-connectivity values) which were found to be different between groups and the four GCO changes. Each GCO was considered as the dependent variable into each model, which also included age, sex, baseline LEDD, individual follow-up duration and baseline nodal or NBS metric as covariates (independent variables). R2 goodness of fit statistic was estimated for each model at issue, for each PD subtype separately.
Results
PD clusters
According to cluster analysis, two main PD subtypes were identified: 86 mild and 60 moderate-to-severe PD patients, with the latter group being older and having earlier PD onset, longer disease duration, lower education, higher LEDD, more severe motor signs/symptoms, more severe and frequent non-motor manifestations and more severe cognitive deficits (Supplementary Tables 2 and 3). Within the mild PD cluster, two subtypes were further identified: mild motor-predominant (N 43) and mild-diffuse (N 43), with the latter group being slightly older, more frequently male, taking lower LEDD, shorter PD duration, more frequent non-motor manifestations (i.e., urinary dysfunction) and greater memory deficits (Supplementary Tables 4 and 5).
Longitudinal clinical changes
Clinical and cognitive changes in PD clusters are reported in Supplementary Tables 2–5. Both mild and moderate-to-severe PD patients showed a significant worsening of motor signs/symptoms, which was greater in mild cases (Supplementary Table 2). Mild-diffuse and motor-predominant subjects worsened in all motor variables, without difference between groups (Supplementary Table 4). Both mild and moderate-to-severe PD patients showed a significant worsening of fluctuations (p < 0.001 and p = 0.02, respectively) and dyskinesia (p = 0.02 and p = 0.01, respectively), with the mild group showing also an increased frequency of orthostatic (p = 0.03) and RBD (p = 0.001) symptoms. Both mild motor-predominant and mild-diffuse PD patients had a worsening of fluctuations (p = 0.002 and p = 0.005, respectively) and RBD (p = 0.02 and p = 0.01, respectively), while only the motor-predominant subtype developed more dyskinesia (p = 0.02) and orthostatic symptoms (p = 0.04). Moderate-to-severe PD patients worsened in all cognitive domains, except for language (Supplementary Table 3). Cognitive deterioration in mild PD patients was less severe (Supplementary Tables 3 and 5). Both mild and moderate-to-severe PD groups showed increased depression and apathy, while only moderate-to-severe PD patients had an increased anxiety (Supplementary Tables 3 and 5).
Baseline functional connectome in PD patients
PD subtypes vs controls
Both moderate-to-severe and mild PD clusters showed a relatively preserved global functional brain architecture relative to controls at baseline (Table 1). On the contrary, lobar network analysis showed reduced mean nodal strength and longer path length of the parietal areas in both patient groups and longer path length of the sensorimotor areas in moderate-to-severe patients relative to controls (Supplementary Table 6). In the regional FC analysis (Supplementary Fig. 2a), a widespread pattern of decreased connectivity involving the basal ganglia, sensorimotor, frontal, parietal and temporal networks was found in moderate-to-severe PD patients relative to controls. Regional FC was not affected in mild PD patients.
Mild motor-predominant PD cases showed no global and lobar nodal as well as regional FC abnormalities relative to controls (Table 1 and Supplementary Table 7). Mild-diffuse PD patients did not show any difference in global network architecture relative to controls (Table 1), while they had a reduced mean nodal strength in parietal areas and an increased path length in sensorimotor areas compared with controls (Supplementary Table 7). Regional FC analysis showed that mild-diffuse PD patients presented alterations in basal ganglia, sensorimotor, frontal, parietal and temporal networks relative to controls (Supplementary Fig. 2b).
Comparisons between PD subtypes
No difference was found in global and lobar functional topological properties as well as in FC in moderate-to-severe and mild PD patients as a whole (Table 1 and Supplementary Table 6). Moderate-to-severe and mild-diffuse PD patients showed no global, lobar and regional FC differences (p > 0.05). Mild motor-predominant and moderate-to-severe PD patients showed no global and lobar nodal differences (p > 0.05), while a decreased connectivity was observed in sensorimotor, basal ganglia, frontal, parietal and temporal networks in moderate-to-severe patients (Supplementary Fig. 2c). Mild motor-predominant and mild-diffuse PD patients showed no RS fMRI differences (Table 1 and Supplementary Table 7).
Correlations between baseline functional network alterations and GCOs
Supplementary Table 8 reports significant correlations between baseline functional network alterations and motor, cognitive, mood, and non-motor GCOs in PD clusters.
Longitudinal functional network changes in PD subtypes
Table 1, Supplementary Tables 6, 7, 9 and 10, and Figs. 1 and 2 report functional network changes in PD subtypes. Moderate-to-severe PD patients showed a progressive alteration of the global network properties relative to mild PD cases (decreased mean nodal strength, local efficiency and clustering coefficient, and longer path length), while no global changes were observed in mild PD (Table 1). Nodal properties changes in moderate-to-severe PD patients involved sensorimotor, fronto-insular, temporal and parietal regions (Supplementary Table 6). In the occipital lobe, mild PD patients showed increased mean nodal strength, local efficiency and clustering coefficient and decreased path length over time relative to moderate-to-severe cases (Supplementary Table 6). No significant nodal changes were found in the two mild PD subtypes (Table 1 and Supplementary Table 7).
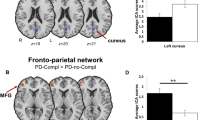
Three distinct patterns of progression are represented: a different trend of change between subtypes; b similar trend of change (increase or decrease), with or without functional connectivity difference between the subtypes; and c different but stable functional connectivity values over time in the two subgroups. The effects of age, sex, levodopa equivalent daily dose at study entry and changes of treatment over time were considered in the model. In the upper part of the figure, the affected connections are shown in blue and the corresponding connected cortical regions are represented in yellow. In the bottom part of the figure, affected subcortical and hippocampal regions are shown (amygdala = red; caudate = cyan; globus pallidus = blue; hippocampus = yellow; putamen = green; thalamus = magenta). See “Methods” section for further details.
Three distinct patterns of progression are represented: a different trend of change between subtypes; b similar trend of change (increase or decrease), with or without functional connectivity difference between the subtypes; and c different but stable functional connectivity values over time in the two subgroups. The effects of age, sex, levodopa equivalent daily dose at study entry and changes of treatment over time were considered in the model. In the upper part of the figure, the affected connections are shown in blue and the corresponding connected cortical regions are represented in yellow. In the bottom part of the figure, affected subcortical and hippocampal regions are shown (amygdala = red; caudate = cyan; globus pallidus = blue; hippocampus = yellow; putamen = green; thalamus = magenta). See “Methods” section for further details.
When FC changes over time were compared between PD subtypes using NBS (Figs. 1 and 2; Supplementary Tables 9 and 10), four distinct patterns of progression were identified: (1) different trend of changes between subtypes (increase vs decrease, increase or decrease vs stable); (2) similar trend of change (increase or decrease), with or without FC difference between the groups; (3) different but stable FC in the two subtypes; (4) stable FC with no difference between groups. In moderate-to-severe and mild PD, both decreased and increased FC were observed in basal ganglia-cortical, sensorimotor-cortical, and cortico-cortical connections (Fig. 1; Supplementary Table 9). However, when a different trend of change was observed, increased FC prevailed in mild PD patients and decreased connectivity over time was the predominant pattern in moderate-to-severe cases (Fig. 1; Supplementary Table 9). In both mild motor-predominant and mild-diffuse subtypes, decreased and increased FC were observed (Fig. 2; Supplementary Table 10). In the two mild PD subtypes, decreased connectivity involved predominantly basal ganglia-sensorimotor and sensorimotor-cortical connections, while increased FC was observed in basal ganglia-basal ganglia and cortico-cortical connections (Fig. 2; Supplementary Table 10).
The effect of brain network changes on clinical PD progression
Table 2 reports significant correlations between functional network changes and clinical evolution (i.e., motor, cognitive, mood, and non-motor GCO changes) in PD subtypes. Table 3 summarizes the ability of functional network alterations at baseline to predict mood and non-motor evolution in moderate-to-severe PD patients and motor, cognitive, mood and non-motor evolution in mild-diffuse PD patients.
Discussion
Graph analysis and connectomics were applied to multiple serial RS fMRI to explore brain functional network changes over maximum 4 years in 146 PD patients. Longitudinal clinical data showed that the course and prognosis of disease differ between the subtypes. Brain functional network alterations and their longitudinal changes varied across groups of patients in different disease stages with distinctive clinical features. A key finding was that RS fMRI changes were associated with motor, cognitive and non-motor evolution in PD patients. Moreover, baseline RS fMRI significantly predicted the severity of clinical evolution differently according to PD subtypes. Collectively, our findings suggest that RS fMRI may be an early biomarker of PD motor and non-motor progression.
PD subtypes showed a relatively preserved global topological organization of the functional brain network but significant focal alterations in lobar nodal topological properties. Both mild and moderate-to-severe patients had decreased mean nodal strength, which is the simplest estimator of the “wiring cost” of the network [9], and longer path length, which estimates the potential for functional integration between brain regions [9], in parietal lobe compared to controls. This suggests that the parietal brain networks of PD patients have more nodes with fewer connections (low degree) and fewer nodes with many connections (high degree), and a weaker potential for integration. FC alterations of the parietal lobe within the DMN have been usually related to cognitive deficits; [29] however previous studies showed reduced efficiency of the brain parietal nodes also regardless of the stage of the disease and cognitive impairment of PD patients [6, 8]. In accordance with the clinical core motor features of PD [1] and previous studies [6, 8], moderate-to-severe PD patients also showed a significant increase in the path length of sensorimotor areas relative to controls.
Unlike nodal analysis, regional FC showed different deterioration patterns among PD clusters. The severe FC breakdown in the basal ganglia, sensorimotor areas, frontal and posterior brain regions, particularly in bilateral occipital, temporal and parietal lobes in moderate-to-severe PD patients suggests a widespread FC modification with the motor and non-motor severity progression. Reduced FC in the cortico-striatal-thalamic-cortical circuits in moderate-to-severe patients with PD is a robust finding in previous literature [6, 8]. The specific involvement of associative frontal, parietal, temporal and occipital connections was related with a spectrum of cognitive deficit [14, 18, 21, 22]. Non-motor PD manifestations such as RBD [30], hallucinations [31], and dysautonomia [32] were previously associated with a loss of network functional efficiency.
Of particular interest are the findings obtained in the two mild PD subtypes. Mild motor-predominant PD patients appear to be the least impaired in their network connectivity organization, in accordance with the less severe motor and clinical symptoms and the relatively lower frequency of other non-motor manifestations. On the contrary, mild-diffuse PD patients were characterized by a disrupted organization of parietal and sensorimotor nodes at baseline as well as by widespread connectivity alterations. In addition, as no significant difference was noted in mild-diffuse relative to moderate-to-severe patients, it can be speculated that the same amount of functional brain disruption occurred in a shorter time span in mild-diffuse cases (disease duration <2 years) pointing to this subtype as an aggressive form of the disease. Importantly, this group were characterized by more severe memory impairment and more frequent urinary symptoms at study entry as well as with a trend toward a more severe cognitive decline over follow-up compared with mild motor-predominant cases. Our findings deepen previous graph analysis fMRI studies in smaller samples suggesting that disrupted FC in the mild PD phase is related to cognitive deficits [21, 22].
As the disease progressed, moderate-to-severe patients progressed with greater cognitive and non-motor decline relative to mild cases and had a less integrated global network configuration. Local alterations of nodal topological properties worsened in sensorimotor and parietal regions and evolved to include fronto-insular and temporal areas. The spreading of network changes observed in moderate-to-severe patients resembles PD pathology progression from brainstem to higher cortical layers [33], demonstrating a greater degeneration along the PD disease-specific pathways in the advanced disease phase.
Over the follow up, moderate-to-severe and mild PD patients showed a widespread reorganization of brain functional connections. Both decreases and increases in FC were observed in all PD patients, although hypoconnectivity prevailed in patients at later disease stage and hyperconnectivity in mild cases. The classical explanation of this finding is that decreased functional integration and connectivity are a direct effect of neurodegeneration, while increased connectivity may reflect compensation. As the disease progresses and the burden of pathology increases, this early adaptive and plastic response might then be overwhelmed. However, this can be an oversimplification of a more complex scenario, in which increased topology and connectivity could be playing an active role in the pathogenesis of the disease. Indeed, it is plausible that increased integration and connectivity in remote sites might also be caused by loss of cortical inhibitory influence. These hypotheses can only be tested longitudinally by correlating functional network changes with clinical evolution. In mild PD subtypes, the correlation between the motor/cognitive deterioration and the FC reduction among basal ganglia, sensorimotor, frontal and inferior parietal areas might represent a neurodegeneration-related effect. On the contrary, with disease progression, the increased nodal strength, local efficiency and clustering coefficient in the occipital lobe observed in mild PD patients may be compensatory because posterior regions are relatively spared early in the disease [33]. As the disease progresses, posterior regions become targeted by Lewy Bodies pathology [33], thus moderate-to-severe PD patients showed decreased nodal properties and connectivity in the occipital lobe associated with non-motor symptoms and mood worsening. On the other hand, correlation analysis between functional network and clinical changes over time suggest that many increased connections in PD brains are maladaptive as they do associate with clinical worsening. This was the case for instance in mild-diffuse PD cases where the enhanced FC between precentral cortex and postcentral and inferior parietal lobe was associated with greater motor disability, and the increased FC among basal ganglia, parietal, temporal, frontal and hippocampal regions correlated with more severe mood disturbances.
Importantly, our study also showed that RS fMRI abnormalities at baseline not only correlated with baseline clinical findings but also presaged clinical and cognitive evolution in PD patients. In mild PD patients, lower the strength and longer the path length in the parietal lobe, greater the motor disability at baseline. In addition, reduced nodal strength of the parietal lobe and decreased connections of the parietal regions with brainstem, insular, frontal, and temporal areas predicted more rapid decline in motor, cognitive and non-motor scores in mild-diffuse cases. These findings corroborate the baseline and longitudinal observations of the central role of parietal disconnectivity in identifying most severe PD cases. In addition, baseline correlation analysis and prediction models confirmed that both hypo- and hyperconnectivity were associated with clinical deficits in PD at different stage of the disease.
This study is not without limitations. First, the mean age at onset of our cohort is slightly lower than expected [34]. Although these data are in line with recent epidemiological findings suggesting that the improved awareness of early parkinsonian signs among clinicians could have contributed to shift the timing of PD diagnosis earlier [35], differences in age at disease onset between groups may explain some clinical results. For instance, mild-diffuse PD patients were slightly older compared with mild motor-predominant cases and this could be associated with the higher frequency of non-motor features at disease onset [34]. Nevertheless, results in the moderate-to-severe group should not have been influenced by the patients’ age at onset because previous findings of clinico-pathological investigations suggested that, in the advanced PD stages, the pattern of disease progression is similar both in cases with younger and older age at onset [36]. In addition, in our PD cohort, only few subjects are between 40 and 50 years and they can be representative of the possible heterogeneity of PD population [34]. Second, PD patients were evaluated in ON status. Unlike previous longitudinal fMRI studies [23,24,25], our analysis accounted for both LEDD at baseline and change over time. Third, we do not have longitudinal RS fMRI data in healthy controls. Thus, we cannot ignore that part of the functional reorganization we observed in patients was related to aging effects. However, our findings demonstrate that brain network properties change differentially among PD subtypes with a similar age. Fourth, we used a 1.5 T MRI scanner, which is characterized by a lower BOLD signal to noise ratio compared with higher field strength scanners. Fifth, several studies have attempted to divide PD patients into subtypes [37]. Our data-driven cluster analysis needs to be validated in independent cohorts. Finally, longer follow-up of our cohort will allow continued assessment of changes.
In conclusion, capitalizing on the large sample size, the comprehensive clinical evaluations and the multiple RS fMRI scanning, our network perspective was able to define trajectories of functional architecture changes according to PD subtypes and prognosis. Future studies that integrate different imaging modalities will be helpful to clarify whether the disease-specific patterns of functional changes in PD are associated with specific structural connectivity alterations.
References
Poewe W, Seppi K, Tanner CM, Halliday GM, Brundin P, Volkmann J, et al. Parkinson disease. Nat Rev Dis Prim. 2017;3:17013.
Greenland JC, Williams-Gray CH, Barker RA. The clinical heterogeneity of Parkinson’s disease and its therapeutic implications. Eur J Neurosci. 2019;49:328–38.
Dickson DW, Braak H, Duda JE, Duyckaerts C, Gasser T, Halliday GM, et al. Neuropathological assessment of Parkinson’s disease: refining the diagnostic criteria. Lancet Neurol. 2009;8:1150–7.
Goedert M, Masuda-Suzukake M, Falcon B. Like prions: the propagation of aggregated tau and alpha-synuclein in neurodegeneration. Brain. 2017;140:266–78.
Yau Y, Zeighami Y, Baker TE, Larcher K, Vainik U, Dadar M, et al. Network connectivity determines cortical thinning in early Parkinson’s disease progression. Nat Commun. 2018;9:12.
Cerasa A, Novellino F, Quattrone A. Connectivity changes in Parkinson’s disease. Curr Neurol Neurosci Rep. 2016;16:91.
Tahmasian M, Eickhoff SB, Giehl K, Schwartz F, Herz DM, Drzezga A, et al. Resting-state functional reorganization in Parkinson’s disease: An activation likelihood estimation meta-analysis. Cortex. 2017;92:119–38.
Filippi M, Sarasso E, Agosta F. Resting-state functional MRI in Parkinsonian syndromes. Mov Disord Clin Pr. 2019;6:104–17.
Rubinov M, Sporns O. Complex network measures of brain connectivity: uses and interpretations. Neuroimage. 2010;52:1059–69.
Crossley NA, Mechelli A, Scott J, Carletti F, Fox PT, McGuire P, et al. The hubs of the human connectome are generally implicated in the anatomy of brain disorders. Brain. 2014;137(Pt 8):2382–95.
Fornito A, Zalesky A, Breakspear M. The connectomics of brain disorders. Nat Rev Neurosci. 2015;16:159–72.
Skidmore F, Korenkevych D, Liu Y, He G, Bullmore E, Pardalos PM. Connectivity brain networks based on wavelet correlation analysis in Parkinson fMRI data. Neurosci Lett. 2011;499:47–51.
Gottlich M, Munte TF, Heldmann M, Kasten M, Hagenah J, Kramer UM. Altered resting state brain networks in Parkinson’s disease. PLoS ONE. 2013;8:e77336.
Baggio HC, Sala-Llonch R, Segura B, Marti MJ, Valldeoriola F, Compta Y, et al. Functional brain networks and cognitive deficits in Parkinson’s disease. Hum Brain Mapp. 2014;35:4620–34.
Fang J, Chen H, Cao Z, Jiang Y, Ma L, Ma H, et al. Impaired brain network architecture in newly diagnosed Parkinson’s disease based on graph theoretical analysis. Neurosci Lett. 2017;657:151–8.
Suo X, Lei D, Li N, Cheng L, Chen F, Wang M, et al. Functional brain connectome and its relation to Hoehn and Yahr stage in Parkinson disease. Radiology. 2017;285:904–13.
Abos A, Baggio HC, Segura B, Garcia-Diaz AI, Compta Y, Marti MJ, et al. Discriminating cognitive status in Parkinson’s disease through functional connectomics and machine learning. Sci Rep. 2017;7:45347.
Gratton C, Koller JM, Shannon W, Greene DJ, Maiti B, Snyder AZ, et al. Emergent functional network effects in Parkinson disease. Cereb Cortex. 2019;29:1701.
Lopes R, Delmaire C, Defebvre L, Moonen AJ, Duits AA, Hofman P, et al. Cognitive phenotypes in parkinson’s disease differ in terms of brain-network organization and connectivity. Hum Brain Mapp. 2017;38:1604–21.
de Schipper LJ, Hafkemeijer A, van der Grond J, Marinus J, Henselmans JML, van Hilten JJ. Altered whole-brain and network-based functional connectivity in Parkinson’s disease. Front Neurol. 2018;9:419.
Luo CY, Guo XY, Song W, Chen Q, Cao B, Yang J, et al. Functional connectome assessed using graph theory in drug-naive Parkinson’s disease. J Neurol. 2015;262:1557–67.
Lin SJ, Baumeister TR, Garg S, McKeown MJ. Cognitive profiles and hub vulnerability in Parkinson’s disease. Front Neurol. 2018;9:482.
Olde Dubbelink KT, Schoonheim MM, Deijen JB, Twisk JW, Barkhof F, Berendse HW. Functional connectivity and cognitive decline over 3 years in Parkinson disease. Neurology. 2014;83:2046–53.
Zeng Q, Guan X, Law Yan Lun JCF, Shen Z, Guo T, Xuan M, et al. Longitudinal alterations of local spontaneous brain activity in Parkinson’s disease. Neurosci Bull. 2017;33:501–9.
Tuovinen N, Seppi K, de Pasquale F, Muller C, Nocker M, Schocke M, et al. The reorganization of functional architecture in the early-stages of Parkinson’s disease. Parkinsonism Relat Disord. 2018;50:61–8.
Sporns O, Chialvo DR, Kaiser M, Hilgetag CC. Organization, development and function of complex brain networks. Trends Cogn Sci. 2004;8:418–25.
Watts DJ, Strogatz SH. Collective dynamics of ‘small-world’ networks. Nature. 1998;393:440–2.
Zalesky A, Fornito A, Bullmore ET. Network-based statistic: identifying differences in brain networks. Neuroimage. 2010;53:1197–207.
Wolters AF, van de Weijer SCF, Leentjens AFG, Duits AA, Jacobs HIL, Kuijf ML. Resting-state fMRI in Parkinson’s disease patients with cognitive impairment: a meta-analysis. Parkinsonism Relat Disord 2019;62:16–27.
Rolinski M, Griffanti L, Piccini P, Roussakis AA, Szewczyk-Krolikowski K, Menke RA. et al. Basal ganglia dysfunction in idiopathic REM sleep behaviour disorder parallels that in early Parkinson’s disease. Brain. 2016;139:2224–34.
Hepp DH, Foncke EMJ, Olde Dubbelink KTE, van de Berg WDJ, Berendse HW, Schoonheim MM. Loss of functional connectivity in patients with Parkinson disease and visual hallucinations. Radiology. 2017;285:896–903.
Chung SJ, Bae YJ, Jun S, Yoo HS, Kim SW, Lee YH et al. Dysautonomia is associated with structural and functional alterations in Parkinson disease. Neurology 2019;92:e1456–67.
Braak H, Bohl JR, Muller CM, Rub U, de Vos RA, Del Tredici K. Stanley Fahn Lecture 2005: The staging procedure for the inclusion body pathology associated with sporadic Parkinson’s disease reconsidered. Mov Disord. 2006;21:2042–51.
Pagano G, Ferrara N, Brooks DJ, Pavese N. Age at onset and Parkinson disease phenotype. Neurology. 2016;86:1400–7.
Darweesh SK, Koudstaal PJ, Stricker BH, Hofman A, Ikram MA. Trends in the incidence of Parkinson disease in the general population: the Rotterdam study. Am J Epidemiol. 2016;183:1018–26.
Kempster PA, O’Sullivan SS, Holton JL, Revesz T, Lees AJ. Relationships between age and late progression of Parkinson’s disease: a clinico-pathological study. Brain. 2010;133(Pt 6):1755–62.
Greenland JC, Williams-Gray CH, Barker RA. The clinical heterogeneity of Parkinson’s disease and its therapeutic implications. Eur J Neurosci. 2019;49:328–38.
Acknowledgements
The authors thank the patients and their families for the time and effort they dedicated to the research, and Dr. Homa Zahedmanesh, Dr. Marta Gandolla and Prof. Alessandra Pedrocchi from Politecnico di Milano, Italy for the fruitful discussion.
Funding
Ministry of Education, Science, and Technological Development of the Republic of Serbia (project #175090).
Author information
Authors and Affiliations
Contributions
M.F. is Editor-in-Chief of the Journal of Neurology; received compensation for consulting services and/or speaking activities from Biogen Idec, Merck-Serono, Novartis, Teva Pharmaceutical Industries; and receives research support from Biogen Idec, Merck-Serono, Novartis, Teva Pharmaceutical Industries, Roche, Italian Ministry of Health, Fondazione Italiana Sclerosi Multipla, and ARiSLA (Fondazione Italiana di Ricerca per la SLA). S.B., E.S., I.S., A.F., A.T., N.P. and V.M. report no disclosures. T.S. has received speaker honoraria from Actavis and Alzheimer’s Association International Research Grant. E.S. has received speaker honoraria from Actavis. V.S.K. has received speaker honoraria from Actavis and Solveo. F.A. is Section Editor of NeuroImage: Clinical; has received speaker honoraria from Novartis, Biogen Idec and Philips; and receives or has received research supports from the Italian Ministry of Health, AriSLA (Fondazione Italiana di Ricerca per la SLA), and the European Research Council.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Filippi, M., Basaia, S., Sarasso, E. et al. Longitudinal brain connectivity changes and clinical evolution in Parkinson’s disease. Mol Psychiatry 26, 5429–5440 (2021). https://doi.org/10.1038/s41380-020-0770-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-020-0770-0
- Springer Nature Limited
This article is cited by
-
Brain network centrality and connectivity are associated with clinical subtypes and disease progression in Parkinson’s disease
Brain Imaging and Behavior (2024)
-
Clinical and MRI features of gait and balance disorders in neurodegenerative diseases
Journal of Neurology (2023)
-
Rehabilitative interventions for impaired handwriting in people with Parkinson’s disease: a scoping review
Neurological Sciences (2023)
-
Cerebellar alterations in Parkinson’s disease with postural instability and gait disorders
Journal of Neurology (2023)
-
Functional connectivity in Parkinson’s disease candidates for deep brain stimulation
npj Parkinson's Disease (2022)