Abstract
This is the initial report of results from the AURORA multisite longitudinal study of adverse post-traumatic neuropsychiatric sequelae (APNS) among participants seeking emergency department (ED) treatment in the aftermath of a traumatic life experience. We focus on n = 666 participants presenting to EDs following a motor vehicle collision (MVC) and examine associations of participant socio-demographic and participant-reported MVC characteristics with 8-week posttraumatic stress disorder (PTSD) adjusting for pre-MVC PTSD and mediated by peritraumatic symptoms and 2-week acute stress disorder (ASD). Peritraumatic Symptoms, ASD, and PTSD were assessed with self-report scales. Eight-week PTSD prevalence was relatively high (42.0%) and positively associated with participant sex (female), low socioeconomic status (education and income), and several self-report indicators of MVC severity. Most of these associations were entirely mediated by peritraumatic symptoms and, to a lesser degree, ASD, suggesting that the first 2 weeks after trauma may be a uniquely important time period for intervening to prevent and reduce risk of PTSD. This observation, coupled with substantial variation in the relative strength of mediating pathways across predictors, raises the possibility of diverse and potentially complex underlying biological and psychological processes that remain to be elucidated with more in-depth analyses of the rich and evolving AURORA data.
Similar content being viewed by others
Introduction
Forty million Americans come to an emergency department (ED) after a traumatic experience each year [1]. A substantial proportion of these people develop adverse post-traumatic neuropsychiatric sequelae (APNS) [2, 3], including posttraumatic stress disorder (PTSD), major depression, post-concussion syndrome, and chronic pain syndrome [1, 4,5,6]. These APNS are an important source of population morbidity and mortality [7, 8] that are partially preventable because opportunities exist to develop preventive interventions for them in the immediate aftermath of trauma exposure. Efforts to develop these early interventions are hampered, though, by the fact that integrated research on the pathogenesis of APNS at the molecular, neural, physiological, cognitive, and behavioral levels is only in its infancy [9].
The scale and complexity of the work needed to address existing knowledge gaps in this area require a programmatic approach. Recognizing this fact, the National Institute of Mental Health recently initiated a cooperative effort, the AURORA (Advancing Understanding of RecOvery afteR traumA) study, to collect a broad range of biobehavioral data from thousands of trauma survivors recruited from EDs and followed for one year [10]. In this initial AURORA report we focus on PTSD, the most widely-studied APNS, among participants experiencing motor vehicle collision (MVC), the most common life-threatening traumatic experience in industrialized countries [11], and examine patterns and associations of socio-demographic characteristics and MVC experiences with peritraumatic symptoms and 8-week PTSD.
Previous research has documented associations of socio-demographic characteristics (age, sex, race-ethnicity, socioeconomic status) and aspects of MVC severity with PTSD [12, 13]. But it is unknown how much these associations are mediated by peritraumatic symptoms that can be assessed in the ED and predict PTSD [14, 15] or by acute stress reactions that develop in the early weeks after MVC and also predict PTSD [16]. Nor do we know the extent to which these associations are explained by pre-MVC PTSD. We focus on these questions in the current report. An understanding of these different possibilities could be valuable in designing preventive interventions for PTSD.
Participants and methods
Participants
AURORA enrollment began September 2017. The n = 666 cases considered here are from the first data freeze, which included respondents who completed 8-week assessments before April 2019. This cut-off was chosen to yield enough cases for preliminary descriptive analyses early enough in the field process to allow mid-course corrections if data problems were detected. We recognize that these early cases are too few in number to allow powerful analyses to be carried out of complex associations but are sufficient to allow prevalence estimates in the expected range to be obtained with standard errors of 0.2% and to examine basic time-lagged associations. Enrollment occurred at 23 urban EDs across the US. Enrollment focused on patients ages 18–75 presenting within 72 h of MVC who could speak and read English, were oriented to time-space and able to follow the enrollment protocol, were physically able to use a smart phone and possessed a smart phone for >1 year. (Supplementary Fig. 1) We excluded participants with a solid organ injury Grade >1 based on American Association for the Surgery of Trauma (AAST) criteria, significant hemorrhage, need for a chest tube or operation with general anesthesia, or likely to be admitted for >72 h. A total of 867 participants met all criteria, provided informed consent, and completed baseline assessments in the ED. We focus here on the 666 such participants who completed a 2-week survey (Mean [25th–75th percentiles]) 9.7 (7–11) days after MVC and an 8-week survey 50.5 (46–52) days after MVC.
Measures
After providing written informed consent, each participant received an interviewer-administered ED assessment with both self-report questions and biological sample collections described elsewhere [10]. Subsequent 2-week and 8-week web surveys were sent by text or e-mail for self-completion or were completed with telephone interviewer assistance. Each participant was reimbursed $60 for the ED assessment, $40 for the 2-week survey, and $40 for the 8-week survey. These procedures were approved by each participating institution’s institutional review board.
Socio-demographics
Information was recorded on each participant’s age (18–24, 25–34, 35–49, 50–75), sex, race-ethnicity (Non-Hispanic Black, Non-Hispanic White, Hispanic, Other), marital status (married/cohabitating, previously married, never married), education (less than high school graduate, high school graduate, some college, college graduate), family income before taxes (divided into approximate tertiles of less than $19K, $19–35K, more than $35K), and employment status (employed versus others).
MVC characteristics
Participant-reported MVC characteristics included: participant was a driver versus passenger; collision with a moving vehicle versus stationary object; amount of vehicle damage (participant-rated from “none” to “severe”); severity of injuries sustained by people other than the participant (participant-rated using the same “none” to “severe” scale); timing and method of transport to the ED; details about participant injuries (hit head; traumatic brain injury [TBI] defined by self-report of hitting head with either loss of consciousness, amnesia, or disorientation[17]; severity of injury based on Abbreviated Injury Scale [AIS] [18]; admission versus discharge from ED), and participant self-ratings in the ED on current overall pain and other symptoms compared to the prior 30 days. Pain was assessed with a 0–10 visual response scale, where “0” was defined as “no pain or tenderness” and “10” as “severe pain or tenderness” [19]. A difference score was then constructed and standardized to a within-sample mean of 0 and variance of 1. Comparable pairs of questions about severity of other somatic symptoms (Supplementary Table 1) were obtained for the same time periods by asking “how much of a problem” each symptom was on a 0–10 visual response scale where “0” was defined as “no problem” and “10” as “a major problem”. Symptoms included 12 adapted from the Pennebaker Inventory of Limbic Languidness scale [20] and 8 adapted from the Rivermead Post-Concussion Symptoms Questionnaire [21]. (Supplementary Table 1) As with pain, each individual-level difference score was standardized to a mean of 0 and variance of 1, then summed into a single overall scale. The decision to create a single scale was based on finding a unidimensional factor structure (Supplementary Table 1) and high inter-correlations (Cronbach’s α = 0.85) among responses.
Peritraumatic distress and dissociation
Peritraumatic distress and dissociation were assessed in the ED with a rationally-selected 8-item short-form of the 13-item Peritraumatic Distress Inventory (PDI; [22]) and the 5-item revised Michigan Critical Events Perception Scale (MCEPS; [23]). (Supplementary Table 2) We modified the introduction to both series to ask about frequency of feelings and experiences “during and immediately after” the MVC and used a 0–4 response scale of “none of the time”, “a little”, “some”, “most”, and “all or almost all the time”. Scores were summed to create 0–32 PDI and 0–20 MCEPS scales and then standardized to a mean of 0 and variance of 1. Cronbach’s α of the PDI is 0.80 and of the MCEPS is 0.77.
Acute stress disorder and post-traumatic stress disorder
The PTSD Checklist for DSM-5 (PCL-5; [23]) was administered in the ED for PTSD in the 30 days before the MVC. The same scale was administered in the 8-week survey to assess PTSD in the 30 days before that survey. The PCL-5 is a 20-item self-report scale that uses a 0–4 response format indicating how much the participant was “bothered by” each of the 20 DSM-5 Criteria B-E symptoms of PTSD (“not at all”, “a little bit”, “moderately”, “quite a bit”, “extremely”) in the past 30 days. We used both the continuous 0–80 symptom score (Cronbach’s α = 0.96) and a dichotomous diagnostic classification for the 30 days before the MVC as predictors of 8-week PTSD diagnoses. Several different diagnostic classification rules have been proposed for the PCL-5 [24, 25]. We used the 31+ threshold. A modification of the PCL-5 was also used to assess DSM-5 Acute Stress Disorder (ASD) Criterion B symptoms since the MVC in the 2-week survey. Questions were added to assess Criteria B5 (negative mood) and B6-B7 (dissociation), which are not criteria for PTSD and are not included in the standard PCL-5. Scores for the 14 DSM-5 Criterion B ASD symptoms were summed to create a 0–56 symptom scale (Cronbach’s α = 0.95) and a dichotomous diagnostic classification was defined as requiring 9+ responses of “moderate” or more.
Analysis methods
We began by examining predictive bivariate and multivariate associations of pre-MVC PTSD with peritraumatic symptoms, 2-week ASD, and 8-week PTSD. Linear regression models were used to predict peritraumatic symptoms and logistic models to predict 2-week ASD diagnoses and 8-week PTSD diagnoses. Associations of socio-demographic characteristics and MVC characteristics were then examined in predicting peritraumatic symptoms, 2-week ASD, and 8-week PTSD both with and without controls for the intermediate outcomes. The latter decompositions allowed us to examine how much gross associations of predictors with 8-week PTSD were mediated by peritraumatic symptoms and 2-week ASD. No attempt was made to weight the data to adjust for differences between participants and patients who refused to participate in AURORA given lack of information about non-participants. Logits and logits ±2 standard errors were exponentiated to create odds-ratios (ORs) with 95% confidence intervals (CIs). Statistical significance was consistently evaluated using .05-level two-sided tests without corrections for multiple comparisons. Computer code are available from the senior author on request.
Results
Imputing item missing values
There was no missing information on participant age, sex, MVC characteristics, or pre-MVC PTSD. Some missing data existed for head injury (for 8.6% of participants), current pain severity (2 participants), and severity of other somatic symptoms (1–2 items for 34 participants, all 20 items for 2 participants). We coded missing head injury data as meaning no head injury given that none of these participants was evaluated for post-concussion syndrome. Central tendency imputations were then used for the small amount (1–5 participants per item) of missing data on peritraumatic symptoms (mean imputation), education and income (median imputation), and race/ethnicity, marital status, and employment status data (mode imputation). Larger numbers of missing values occurred for 2-week ASD (n = 43) and 8-week PTSD (n = 32), but diagnoses could be imputed for most such cases because participants either were above diagnostic thresholds with answered questions or could not score above these thresholds even if missing responses had highest values. Median item-level imputations were used for the small number of remaining cases.
Sensitivity of PTSD prevalence estimates to PCL-5 scoring rules
Prevalence of 8-week DSM-5/PCL-5 PTSD is 39.0% compared to 31.2% prevalence of pre-MVC PTSD. (Table 1) Prevalence estimates are 30.3–49.2% for 8-week PTSD and 19.4–30.8% for pre-MVC PTSD using other recommended PCL-5 diagnostic thresholds between scores of 38+ and 28+. Tetrachoric correlations of diagnoses based on PCL-5 thresholds with diagnoses using DSM-5 criteria are 0.92–0.95. We used the PCL-5 = 31+ threshold in our analysis (42.0% prevalence for 8-week PTSD; 26.3% for pre-MVC PTSD) based on the recommendation of the developers of the PCL-5 [25].
Associations of Pre-MVC PTSD, peritraumatic symptoms, and 2-week ASD, with 8-week PTSD
Preliminary analysis found that associations of pre-MVC PTSD with subsequent peritraumatic symptoms, 2-week ASD diagnoses, and 8-week PTSD diagnoses were all linear. (Supplementary Table 3) This univariate association is significant predicting peritraumatic distress (b = 0.3 [0.2–0.3]), peritraumatic dissociation (b = 0.3 [0.3–0.4]), 2-week ASD (OR = 1.9 [1.6–2.2]), and 8-week PTSD diagnoses (OR = 1.9 [1.6–2.2]). (Table 2) Peritraumatic symptoms are significant univariate predictors of 2-week ASD diagnoses (OR = 2.1 [1.7–2.5] for both distress and dissociation) and 8-week PTSD diagnoses (OR = 2.0 [1.6–2.3] for peritraumatic distress; OR = 1.7 [1.4–2.0] for peritraumatic dissociation). The continuous 2-week ASD symptom scale, finally, which was found in preliminary analysis to be the best functional form of that measure (Supplementary Table 3), is significant in a univariate model predicting 8-week PTSD diagnoses (OR = 4.7 [3.7–5.9]).
The significant univariate associations of pre-MVC PTSD and peritraumatic symptoms with 2-week ASD diagnoses remain significant in a multivariate model that includes all three predictors, although the ORs shrink from 1.9–2.1 in the univariate models to 1.5–1.6. In addition, two of the three significant univariate predictors remain significant in a multivariate model predicting 8-week PTSD: pre-MVC PTSD (OR = 1.7 [1.4–2.0]) and peritraumatic distress (OR = 1.7 [1.4–2.1]). These same two predictors remain significant in an expanded model that adds 2-week ASD as a predictor of 8-week PTSD (OR = 4.1 [3.2–5.3]), although the ORs for pre-MVC PTSD and peritraumatic distress shrink to 1.4–1.4. We also investigated the possibility of nonlinearities and interactions of peritraumatic symptoms predicting 2-week and 8-week diagnoses, but none was significant (Supplementary Tables 4–5).
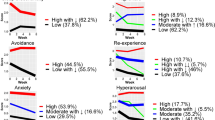
Socio-demographic predictors of peritraumatic symptoms, 2-week ASD, and 8-week PTSD
Controlling pre-MVC PTSD symptom scores, two socio-demographic variables are significant predictors of 8-week PTSD in univariate models: female sex (OR = 1.7 [1.2–2.4]) and education (χ23 = 9.1, p = 0.028), with a non-significantly elevated OR for less than high school graduation (OR = 1.6 [0.9–3.0]) and two non-significant ORs marginally lower than 1.0 (OR = 0.7–0.8) for high school graduate and some college (compared to the omitted category of college graduate). (Table 3) In a multivariate model with all socio-demographics as predictors (χ215 = 21.9, p = 0.101), the sex OR becomes slightly smaller (OR = 1.6 [1.1–2.4]) and the OR for less than high school graduate somewhat higher (OR = 1.7 [0.8–3.3]).
Decomposition of the sex difference in 8-week PTSD shows that females have significantly elevated peritraumatic distress (b = 0.4 [0.3–0.6]) and 2-week ASD (OR = 1.4 [1.0–2.1]) in multivariate models for these outcomes (F15,649 = 2.8, p < 0.001 for distress; χ215 = 17.3, p = 0.30 for ASD). Controlling these intermediate outcomes, the association of female sex with 8-week PTSD becomes non-significant (OR = 1.2 [0.7–1.9]). A comparable decomposition of the association between low education and 8-week PTSD shows a different pattern, as low education is not a significant predictor of either peritraumatic symptoms or 2-week ASD and the OR of low education with 8-week PTSD after controlling mediators is virtually identical to the OR in the model without these controls. No other predictor is globally significant predicting either peritraumatic distress, peritraumatic dissociation, or 2-week ASD.
MVC characteristics predicting peritraumatic symptoms, 2-week ASD, and 8-week PTSD
Controlling socio-demographics and pre-MVC PTSD symptom scores, four MVC characteristics are significant univariate predictors of 8-week PTSD: being a passenger versus driver (OR = 1.6 [1.0–2.4]), number of other passengers injured (OR = 1.3 [1.1–1.5]), TBI (OR = 1.5 [1.0–2.2]), and pain severity reported in the ED (OR = 1.3 [1.1–1.6]). (Table 4) One of these predictors remains significant in a multivariate model (χ217 = 29.3, p = 0.031): pain severity in the ED (OR = 1.3 [1.1–1.6]).
Decomposition of the association between pain and 8-week PTSD through the intervening outcomes shows that pain is associated with significantly elevated peritraumatic distress (b = 0.1 [0.0–0.2]) and 2-week ASD (OR = 1.4 [1.1–1.7]) in multivariate models for these outcomes (F17,632 = 7.5, p < 0.001 for peritraumatic distress; χ217 = 46.3, p = 0.002 for ASD). When we control these intermediate outcomes, the association of pain with 8-week PTSD becomes non-significant (OR = 1.1 [0.9–1.4]). In addition, several other MVC characteristics are significant predictors of intervening outcomes. Severe damage to the participant’s vehicle predicts elevated peritraumatic distress (b = 0.6 [0.3–0.9]) and dissociation (b = 0.3 [0.0–0.6]). Being transported to the ED by ambulance also predicts peritraumatic distress (b = 0.3 [0.1–0.5]) and dissociation (b = 0.2 [0.1–0.4]). Coming to the ED immediately after the MVC in a private vehicle predicts elevated peritraumatic dissociation (b = 0.2 [0.0–0.5]) and 2-week ASD (OR = 2.6 [1.4–4.7]). Physical symptom severity other than pain in the ED predicts peritraumatic distress (b = 0.1 [0.0–0.2]).
Discussion
Our 8-week PTSD prevalence estimates, which are in the range 30.3–49.2% depending on operational definition, are higher than estimates based on retrospective reports in community surveys from representative samples of people who had MVCs [13], although not substantially higher than in previous ED-based studies [26,27,28]. The discrepancy in prevalence estimates between community samples and ED samples is probably related to the fact that only a small minority of individuals who experience MVCs come to the ED [29, 30]. The 2 568 ED patients who refused to participate in AURORA might also have had lower levels of 8-week PTSD than participants. The likelihood of bias is indicated by the fact that the pre-MVC PTSD prevalence estimate of 31.2% in this sample is dramatically higher than estimates of population prevalence [31]. We currently have no way of evaluating this bias directly, though, as we have no information about PTSD either among people who experienced an MVC but did not come to the ED or among qualifying ED patients who refused to participate in AURORA. However, we are designing a methodological sub-study to obtain such data by administering a brief survey both to people who experienced an MVC but did not come to an ED and ED non-respondents.
The finding that peritraumatic distress and dissociation both predict ASD and 8-week PTSD in univariate models is consistent with previous research showing that peritraumatic symptoms predict onset of PTSD [14, 15]. It was striking, though, given the focus of recent research on peritraumatic dissociation [32], that only peritraumatic distress, not peritraumatic dissociation, predicted 8-week PTSD in the multivariate model. The failure of dissociation to predict PTSD net of distress might reflect the fact that dissociation is reported primarily by people with high distress, which could reduce statistical power to detect meaningful net associations of dissociation with later outcomes in a multivariate model. Although this possibility is inconsistent with our failure to find a significant interaction between peritraumatic distress and peritraumatic dissociation in predicting 8-week PTSD, that test had low statistical power given the small current sample size. We will revisit this issue once the sample size increases.
It was also somewhat surprising to find that symptoms of pre-MVC PTSD were significant predictors of 8-week PTSD (OR = 1.4) even after controlling peritraumatic symptoms and 2-week ASD. Although this is broadly consistent with evidence from other studies that prior trauma and PTSD predict subsequent PTSD after later traumas [33], previous studies did not investigate intervening effects through peritraumatic symptoms or ASD. It is unclear what other pathways are involved in this distal effect. We hope to shed light on this question in future AURORA analyses of mediating pathways once we have access to biomarker time series data being assessed with wearable devices, a phone app, and brief weekly neurocognitive tests administered on smartphones [10].
The gross associations of the socio-demographic and MVC-related predictors with 8-week PTSD are consistent with previous research documenting elevated PTSD risk among women, people from low socioeconomic positions, and people exposed to more severe MVCs [12, 13]. However, decomposition showed that the gross associations of these predictors with 8-week PTSD are mediated more by peritraumatic symptoms than by 2-week ASD and that substantial variation exists across predictors in the relative importance of these mediating pathways. We plan to investigate the underpinnings of this variation in mediation analyses once the AURORA biomarker time series data become available.
Several limitations of this initial report need to be acknowledged. The first was alluded to above when we noted that response bias might have been introduced by the high proportion of patients refusing to participate in the study. As described above, we are designing a brief non-respondent survey to evaluate this bias. Second, the number of participants is well below the number needed to estimate mediating pathways directly with precision, leading us to focus on comparisons of association in univariate and multivariate models rather than carry out a formal decomposition of total predictive effects. We will do the latter once AURORA sample size increases. Third, our measures of peritraumatic symptoms were truncated versions of longer scales. These might have been more important predictors if the full scales had been used. Fourth, the decision to carry out short-term follow-up surveys at 2 and 8 weeks was relatively arbitrary and resulted in the surveys not being able to detect instances when patients met DSM criteria for PTSD as of 1 month but remitted before the 8-week assessment. Many other prospective studies of PTSD among ED patients can do this because they include a 1-month assessment [34] in order to address the DSM requirement that symptoms persist more than 1 month to qualify for a diagnosis of PTSD. However, AURORA administers short smart phone symptom surveys to all respondents each day for 8 weeks. This will allow us to capture PTSD symptoms in a more fine-grained fashion once these flash survey data become available for analysis. A final noteworthy limitation is that we focused in this initial report only on 8-week PTSD. Meta-analysis shows that up to 25% of PTSD cases among people followed for several years after trauma exposure do not meet full PTSD criteria until more than 6 months later [35]. And fine-grained analyses of changes in PTSD symptoms over a period of 24 months document a complex and fluctuating course of illness for many cases [36]. We were unable to study either of these complexities in this initial analysis of 8-week PTSD. We plan to do so, though, once data become available from ongoing AURORA follow-up surveys carried out 6, 9, and 12 months after MVC exposure.
Conclusions
This initial report sought to establish the prevalence of 8-week PTSD, to investigate transitions between peritraumatic symptoms, ASD, and 8-week PTSD, and to examine the extent to which gross associations of baseline socio-demographic and MVC characteristics with 8-week PTSD were mediated by peritraumatic symptoms and ASD. We found relatively high 8-week PTSD prevalence, expected univariate predictors of 8-week PTSD, and evidence that these associations were largely mediated through peritraumatic symptoms and to a lesser extent 2-week ASD, suggesting that the first 2 weeks after trauma exposure might be of unique importance in intervening to prevent PTSD in the 8 weeks after trauma exposure. This observation, coupled with our finding of considerable variation across predictors in the relative strength of mediating pathways, raises the possibility of diverse and potentially complex underlying biological and psychological processes that remain to be elucidated in more in-depth analyses of the rich and evolving AURORA data. Supplementary information is available at Molecular Psychiatry’s website.
References
Roberts AL, Gilman SE, Breslau J, Breslau N, Koenen KC. Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychol Med. 2011;41:71–83.
Santiago PN, Ursano RJ, Gray CL, Pynoos RS, Spiegel D, Lewis-Fernandez R, et al. A systematic review of PTSD prevalence and trajectories in DSM-5 defined trauma exposed populations: intentional and non-intentional traumatic events. PLoS ONE. 2013;8:e59236.
Koenen KC, Ratanatharathorn A, Ng L, McLaughlin KA, Bromet EJ, Stein DJ, et al. Posttraumatic stress disorder in the World Mental Health Surveys. Psychol Med. 2017;47:2260–74.
Kessler RC. Posttraumatic stress disorder: the burden to the individual and to society. J Clin Psychiatry. 2000;61:4–12.
Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:1048–60.
Boscarino JA. Posttraumatic stress disorder and mortality among U.S. Army veterans 30 years after military service. Ann Epidemiol. 2006;16:248–56.
Pacella ML, Hruska B, Delahanty DL. The physical health consequences of PTSD and PTSD symptoms: a meta-analytic review. J Anxiety Disord. 2013;27:33–46.
Atwoli L, Stein DJ, Koenen KC, McLaughlin KA. Epidemiology of posttraumatic stress disorder: prevalence, correlates and consequences. Curr Opin Psychiatry. 2015;28:307–11.
Dean KR, Hammamieh R, Mellon SH, Abu-Amara D, Flory JD, Guffanti G, et al. Multi-omic biomarker identification and validation for diagnosing warzone-related post-traumatic stress disorder. Mol Psychiatry. 2019. https://doi.org/10.1038/s41380-019-0496-z.
McLean SA, Ressler KJ, Koenen KC, Neylan TC, Germine LT, Jovanovic T, et al. The AURORA study: a longitudinal, multimodal library of brain biology and function after traumatic stress exposure. Mol Psychiatry. 2020;25:283–96.
Benjet C, Bromet E, Karam EG, Kessler RC, McLaughlin KA, Ruscio AM, et al. The epidemiology of traumatic event exposure worldwide: results from the World Mental Health Survey Consortium. Psychol Med. 2016;46:327–43.
Kazantzis N, Kennedy-Moffat J, Flett RA, Petrik AM, Long NR, Castell B. Predictors of chronic trauma-related symptoms in a community sample of New Zealand motor vehicle accident survivors. Cult Med Psychiatry. 2012;36:442–64.
Stein DJ, Karam EG, Shahly V, Hill ED, King A, Petukhova M, et al. Post-traumatic stress disorder associated with life-threatening motor vehicle collisions in the WHO World Mental Health Surveys. BMC Psychiatry. 2016;16:257.
Vance MC, Kovachy B, Dong M, Bui E. Peritraumatic distress: a review and synthesis of 15 years of research. J Clin Psychol. 2018;74:1457–84.
van der Velden PG, Wittmann L. The independent predictive value of peritraumatic dissociation for PTSD symptomatology after type I trauma: a systematic review of prospective studies. Clin Psychol Rev. 2008;28:1009–20.
Bryant RA. Acute stress disorder. Curr Opin Psychol. 2017;14:127–31.
McLean SA, Kirsch NL, Tan-Schriner CU, Sen A, Frederiksen S, Harris RE, et al. Health status, not head injury, predicts concussion symptoms after minor injury. Am J Emerg Med. 2009;27:182–90.
Loftis KL, Price J, Gillich PJ. Evolution of the abbreviated injury scale: 1990–2015. Traffic Inj Prev. 2018;19:S109–13.
Farrar JT, Young JP Jr. LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94:149–58.
Pennebaker JW, Watson D. The psychology of somatic symptoms. In: Kirmayer LJ, Robbins JM, editors. Current concepts of somatization: research and clinical perspectives. Arlington, VA: American Psychiatric Association; 1991, pp 21–35.
King NS, Crawford S, Wenden FJ, Moss NE, Wade DT. The Rivermead Post Concussion Symptoms Questionnaire: a measure of symptoms commonly experienced after head injury and its reliability. J Neurol. 1995;242:587–92.
Brunet A, Weiss DS, Metzler TJ, Best SR, Neylan TC, Rogers C, et al. The Peritraumatic Distress Inventory: a proposed measure of PTSD criterion A2. Am J Psychiatry. 2001;158:1480–5.
Michaels AJ, Michaels CE, Moon CH, Smith JS, Zimmerman MA, Taheri PA, et al. Posttraumatic stress disorder after injury: impact on general health outcome and early risk assessment. J Trauma. 1999;47:460–7.
Zuromski KL, Ustun B, Hwang I, Keane TM, Marx BP, Stein MB, et al. Developing an optimal short-form of the PTSD Checklist for DSM-5 (PCL-5). Depress Anxiety. 2019;36:790–800.
Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, et al. Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders-fifth edition (PCL-5) in veterans. Psychol Assess. 2016;28:1379–91.
Heron-Delaney M, Kenardy J, Charlton E, Matsuoka Y. A systematic review of predictors of posttraumatic stress disorder (PTSD) for adult road traffic crash survivors. Injury. 2013;44:1413–22.
Feinberg RK, Hu J, Weaver MA, Fillingim RB, Swor RA, Peak DA, et al. Stress-related psychological symptoms contribute to axial pain persistence after motor vehicle collision: path analysis results from a prospective longitudinal study. Pain. 2017;158:682–90.
Linnstaedt SD, Riker KD, Rueckeis CA, Kutchko KM, Lackey L, McCarthy KR, et al. A functional riboSNitch in the 3’ untranslated region of FKBP5 alters microRNA-320a binding efficiency and mediates vulnerability to chronic post-traumatic pain. J Neurosci. 2018;38:8407–20.
National Center for Statistics and Analysis. Summary of motor vehicle crashes: 2016 data. (Traffic Safety Facts. Report No. DOT HS 812 580). Washington, DC: National Highway Traffic Safety Administration; 2018.
Platts-Mills TF, Hunold KM, Esserman DA, Sloane PD, McLean SA. Motor vehicle collision-related emergency department visits by older adults in the United States. Acad Emerg Med. 2012;19:821–7.
Kessler RC, Aguilar-Gaxiola S, Alonso J, Benjet C, Bromet EJ, Cardoso G, et al. Trauma and PTSD in the WHO World Mental Health Surveys. Eur J Psychotraumatol. 2017;8:1353383.
Lanius RA, Boyd JE, McKinnon MC, Nicholson AA, Frewen P, Vermetten E, et al. A review of the neurobiological basis of trauma-related dissociation and its relation to cannabinoid- and opioid-mediated stress response: a transdiagnostic, translational approach. Curr Psychiatry Rep. 2018;20:118.
Kessler RC, Aguilar-Gaxiola S, Alonso J, Bromet EJ, Gureje O, Karam EG, et al. The associations of earlier trauma exposures and history of mental disorders with PTSD after subsequent traumas. Mol Psychiatry. 2018;23:1892–9.
Lowe SR, Ratanatharathorn A, Lai BS, van der Mei W, Barbano AC, Bryant, RA, et al. Posttraumatic stress disorder symptom trajectories within the first year following emergency department admissions: pooled results from the international consortium to predict PTSD. Psychol Med. 2020; https://doi.org/10.1017/S0033291719004008.
Utzon-Frank N, Breinegaard N, Bertelsen M, Borritz M, Hurwitz Eller N, Nordentoft M, et al. Occurrence of delayed-onset post-traumatic stress disorder: a systematic review and meta-analysis of prospective studies. Scand J Work Environ Health. 2014;40:215–29.
Bryant RA, O’Donnell M, Creamer M, McFarlane AC, Silove D. A multisite analysis of the fluctuating course of posttraumatic stress disorder. JAMA Psychiatry. 2013;70:839–46.
Acknowledgements
AURORA is supported by NIMH U01MH110925, the US Army Medical Research and Material Command, The One Mind Foundation, and The Mayday Fund. Verily Life Sciences and Mindstrong Health provide some of the hardware and software used to perform study assessments.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
JME reports support from the National Institutes of Health (NIH) through Grant Numbers R01HD079076 & R03HD094577: Eunice Kennedy Shriver National Institute of Child Health & Human Development; National Center for Medical Rehabilitation Research. WFP is supported by research grants from Abbott, Boehringer Ingelheim, Braincheck, CSL Behring, Daiichi-Sankyo, Immunarray, Janssen, Ortho Clinical Diagnostics, Portola, Relypsa, Roche. He has served as a consultant for Abbott, Astra-Zeneca, Bayer, Beckman, Boehrhinger-Ingelheim, Ischemia Care, Dx, Immunarray, Instrument Labs, Janssen, Nabriva, Ortho Clinical Diagnostics, Relypsa, Roche, Quidel, Salix, Siemens. He has also provided expert testimony for Johnson and Johnson. He owns stock or has ownership interest in AseptiScope Inc, Brainbox Inc, Comprehensive Research Associates LLC, Emergencies in Medicine LLC, Ischemia DX LLC. Over the past three years, DAP has received consulting fees from Akili Interactive Labs, BlackThorn Therapeutics, Boehringer Ingelheim, Posit Science, and Takeda Pharmaceuticals, as well as an honorarium from Alkermes for activities unrelated to the current project. LTG is on the scientific advisory board of the nonprofit Sage Bionetworks, for which she receives a small honorarium. She is also a consultant with 23andme, Inc. CWJ reports no direct conflicts related to this paper, and no ongoing conflicts. He has been an investigator on studies funded by Hologic Inc, Janssen, and AstraZeneca, for which his department has received research funding. NGH reports support from NIMH through grant number K00MH119603. LAML reports support from NIH/NIMH through grant K01MH118467. In the past 3 years, RCK received support for his epidemiological studies from Sanofi Aventis; was a consultant for Datastat, Inc., Johnson & Johnson Wellness and Prevention, Sage Pharmaceuticals, Shire, and Takeda. KJR has served on advisory boards for Takeda, Resilience Therapeutics, Janssen and Verily/Google. His research has been sponsored by Alkermes and Brainsway and he has worked as a consultant for Alkermes. The remaining authors declare no conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Kessler, R.C., Ressler, K.J., House, S.L. et al. Socio-demographic and trauma-related predictors of PTSD within 8 weeks of a motor vehicle collision in the AURORA study. Mol Psychiatry 26, 3108–3121 (2021). https://doi.org/10.1038/s41380-020-00911-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-020-00911-3
- Springer Nature Limited
This article is cited by
-
MMPI-2-RF Profiles of Treatment-Seeking Veterans in a VA Pain Clinic and Associations with Markers of Physical Performance
Journal of Clinical Psychology in Medical Settings (2024)
-
Polygenic risk scoring to assess genetic overlap and protective factors influencing posttraumatic stress, depression, and chronic pain after motor vehicle collision trauma
Translational Psychiatry (2021)
-
Neural contributors to trauma resilience: a review of longitudinal neuroimaging studies
Translational Psychiatry (2021)