Abstract
Chronic peer victimization has long-term impacts on mental health; however, the biological mediators of this adverse relationship are unknown. We sought to determine whether adolescent brain development is involved in mediating the effect of peer victimization on psychopathology. We included participants (n = 682) from the longitudinal IMAGEN study with both peer victimization and neuroimaging data. Latent profile analysis identified groups of adolescents with different experiential patterns of victimization. We then associated the victimization trajectories and brain volume changes with depression, generalized anxiety, and hyperactivity symptoms at age 19. Repeated measures ANOVA revealed time-by-victimization interactions on left putamen volume (F = 4.38, p = 0.037). Changes in left putamen volume were negatively associated with generalized anxiety (t = −2.32, p = 0.020). Notably, peer victimization was indirectly associated with generalized anxiety via decreases in putamen volume (95% CI = 0.004–0.109). This was also true for the left caudate (95% CI = 0.002–0.099). These data suggest that the experience of chronic peer victimization during adolescence might induce psychopathology-relevant deviations from normative brain development. Early peer victimization interventions could prevent such pathological changes.
Similar content being viewed by others
Introduction
Adolescence is a period of significant change, both personally and biologically. While the individual is encountering a host of new life experiences and stressors, the adolescent brain is undergoing extensive development as evidenced by decreases in gray matter volume and increases in white matter volume [1, 2]. Peer relationships are a significant source of stress: up to 30% [3, 4] of adolescents are bullied by their peers. While the frequency of peer victimization decreases across adolescence [5, 6], for some individuals the victimization is chronic and persisting [7, 8].
Peer victimization, especially if it is chronic and persisting, can have dramatic and long-term effects on physical and mental health [9, 10]. Numerous studies have shown that peer victimization in childhood and adolescence is associated with higher rates of psychopathology in adulthood [11,12,13,14]. Two recent studies took the association further and identified a causal contribution of peer victimization to a range of internalizing and externalizing symptoms [15, 16]. Although these studies have suggested causal effects, the biological mediators of such effects have largely not been identified.
Neuroimaging is an useful tool for elucidating possible mediators. Of note, there is a dearth of published neuroimaging studies of peer victimization. There is good reason to pursue this line of research, as primarily retrospective adult studies have associated differences in brain structure with reports of earlier life stress and childhood maltreatment. Generally, children who have experienced early life stress, such as maltreatment, have smaller brain volumes in adulthood compared to control groups in areas important for emotion regulation, impulsivity, and reward processing [17,18,19,20,21], psychological traits implicated in common psychiatric disorders [22,23,24]. Such areas include the anterior cingulate, caudate, putamen, hippocampus, parahippocampal gyrus, amygdala, orbitofrontal cortex, and insula.
These studies have focused on childhood exposure to stress; however, the negative impact of stress on the brain is likely compounded when it occurs during a period of neurobiological maturation such as adolescence [2, 25, 26]. Furthermore, as stated, the existing data are largely based on retrospective or cross-sectional research; while we know that childhood stress leads to altered neural signatures in adulthood we do not know how these differences arose. Therefore, prospective longitudinal studies are needed to identify relationships between victimization, brain development, and vulnerability for psychopathologies.
The longitudinal, multidisciplinary, adolescent IMAGEN cohort enabled us to explore how chronic peer victimization across adolescence impacts structural adolescent brain development and whether such effects underlie the known relationship between peer victimization and mental health. To do this, we used the peer victimization data to generate trajectories from ages 14–19. We then related these trajectories to brain regions previously shown to be sensitive to stress and maltreatment and hypothesized chronically victimized adolescents would show larger decreases in volume over time. We also incorporated measures of stressful life events and childhood maltreatment in our analyses to elucidate whether observed effects were specific to peer victimization or related to stress in general.
Materials and methods
Participants
Participants were part of the IMAGEN project, a community-based longitudinal study of adolescent brain development and mental health. Participants were assessed at eight study sites in England, Ireland, France, and Germany. Individuals were included in the analyses if they had peer victimization data at ages 14, 16, and 19 as well as structural magnetic resonance imaging (MRI) data at ages 14 and 19 (neuroimaging assessments were not carried out at age 16). The comparison of observed characteristics between those included and excluded from the analyses can be found in the online Supplement (Supplementary Table 1). Questionnaires were self-administered on home computers using the Psytools software package (Delosis, London). The local research ethics committees approved this study and written consent was obtained from participants (and from their legal guardian at ages 14 and 16). A detailed description of recruitment and assessment procedures, as well as general inclusion and exclusion criteria, has been published previously [27].
Peer victimization
The peer victimization questions were adapted from a questionnaire used in a large international study entitled Health Behaviour in School-Aged Children (HSBC). These questions were initially utilized in the revised Olweus Bully/Victim Questionnaire [28]. Of the six questions inquiring about victimization during the previous 6 months, two asked about bullying from family members. We engaged in exploratory analysis to examine reliability and external validity of the remaining items to derive a meaningful scale of peer victimization experiences. The selected three items were specifically descriptive about the victimization actions of their peers (for details, please see the Supplementary Information). Because these items do not explicitly mention bullying or capture the imbalance of power associated with bullying, we refer to them as a measure of “peer victimization.” These items were summed to create peer victimization scores at ages 14, 16, and 19.
Psychopathology symptoms
Internalizing and externalizing psychopathology symptoms were evaluated as an outcome at age 19. Preliminary DSM–IV psychiatric diagnoses (depression and generalized anxiety) were obtained via the computer-administered Developmental and Well-Being Assessment (DAWBA [29]). Based on participants’ answers to the DAWBA questions, the well-defined computer algorithm (see www.dawba.com) assigns an individual to one of six ordered-categorical diagnostic “probability bands” (i.e., from <0.1% likely to >70% likely). These “bands” have been validated in two European youth cohorts and perform similarly to clinician-generated diagnoses regarding associations with risk factors [30]. We also used continuous severity scores of internalizing (emotional symptoms) and externalizing (hyperactivity) symptoms on the Strengths and Difficulties Questionnaire (SDQ; www.sdqinfo.com; ref. [31]).
Childhood maltreatment and stressful life events
The childhood trauma questionnaire (CTQ [32]) was used to assess childhood maltreatment across childhood and adolescence. It consists of five domains: emotional abuse, emotional neglect, physical abuse, physical neglect, and sexual abuse. The scores for each of the five domains were summed for a total CTQ score; the higher the score the greater the severity of maltreatment.
The self-report Life Events Questionnaire (LEQ [33]) was used to record the occurrence of stressful life events across adolescence. Twenty events were classed as stressful based on the valence reports of IMAGEN participants as reported previously [34] who experienced the event and rated it as distressing (“unhappy” or “very unhappy”). A stressful life event (SLE) frequency score was calculated based on the number of negative events the participants experienced. For age 14, the number of stressful life events experienced during the previous 12 months was used to generate the SLE score. For ages 16 and 19, the number of stressful life events experienced since their previous assessment was used to generate the SLE score.
MRI acquisition and processing
MRI data
High-resolution T1-weighted structural MRI data were acquired on 3 T MRI scanners (Philips, GE, Siemens). Scanning protocol parameters were harmonized across all sites’ manufacturers.
Voxel-based morphometry
All ages 14 and 19, MPRAGE data were preprocessed in SPM8 (http://www.fil.ion.ucl.ac.uk/spm/) using the VBM8 toolbox with default settings, including the usage of high-dimensional spatial normalization with an already integrated Dartel template in MNI space. All images were subjected to nonlinear modulations and corrected for each individual head size. Images were then smoothed with an 8 mm full-width at half-maximum Gaussian kernel with the resulting voxel size 1.5 mm3. The automated anatomical labeling (AAL) atlas was employed to exclude the voxels outside the gray matter. For each brain area defined by the AAL atlas, the volume of the area was estimated by summing the gray matter volume over all voxels within that area. Total intracranial volume, used as a covariate of no interest, was estimated by the summation of the gray matter, white matter, and CSF volumes in native space.
Eighteen AAL regions of interest (ROIs; nine bilateral) were entered into the analyses considering their relationships with stress and maltreatment [21, 35,36,37,38]. These regions were the inferior orbitofrontal cortex, anterior cingulate cortex, insula, hippocampus, parahippocampal gyrus, amygdala, caudate, putamen, and thalamus. Although individual variability in regional brain volumes is expected, individuals with volumes>3 times the interquartile range away from the 25th and 75th percentiles [39, 40] were considered outliers and their volumes were winsorized. Thirty-six individuals had their ROI volumes winsorized. Of those, 35 were from the non-chronic peer victimization group. The change in brain ROI volumes was calculated as the volume at age 19 minus the volume at age 14.
Statistical analysis
All statistical analyses were two-tailed with a significance threshold of p < 0.05. All statistical tests, except latent profile analysis (LPA) and indirect effect analysis, used SPSS software version 24.
Peer victimization trajectories
We estimated peer victimization trajectories using longitudinal LPA in MPlus version 7 (Muthen & Muthen, Los Angeles, CA). Latent profile analysis enables identification of classes of adolescents who may follow different experiential patterns of peer victimization (e.g., high versus low levels at different ages). With LPA, one can test how well the class model fits the data as well as confidence that the individuals are likely to be following the identified developmental profile. Peer victimization sum scores from ages 14, 16, and 19 were entered into LPA and we fit a series of trajectory models, progressing from a one-class model to a four-class model (trajectory criteria can be found in the Supplementary Information).
Nonparametric partial correlations
As we were interested in whether peer victimization was related to changes in brain structure, we first ran nonparametric partial correlations (rho, ρ) between peer victimization class and the change in ROI volumes from ages 14 to 19. Site, sex, socioeconomic status (SES; indexed used the family stresses subsection of the DAWBA), age 14 pubertal status [41], and change in intracranial volume were included as covariates. Regions associated with peer victimization were included in subsequent multivariate analyses. At this stage, we applied false discovery rate correction [42] to the two-tailed p-values.
Repeated measures ANOVA
We carried out repeated measures analyses of variance (ANOVAs) (partial eta-squared, ηp²; Sum of squares, SS; F-statistic, F) to identify a longitudinal relationship between chronic peer victimization and adolescent brain development. Peer victimization latent profile grouping was the between-subjects variable and the age 14 and age 19 T1-derived AAL volumes were the within-subjects variables. We controlled for site, sex, SES, age 14 pubertal status, and change in intracranial volume. Additional analyses also included sex as a between-subjects variable to determine whether it might influence the victimization-brain relationship.
Mann–Whitney U-test
Because the psychopathology symptoms between the groups did not meet homogeneity of variance assumptions, a two-tailed Mann–Whitney U-test (U-statistic, U; correlation, r) was used to identify relationships between peer victimization and psychopathology symptoms. At this stage, we applied false discovery rate correction [42] to the two-tailed p-values.
Linear regression analyses
We ran multivariable linear regression analyses (t-statistic, t) to identify the relationship between changes in regional brain volumes and psychopathology symptoms. Sex, study site, SES, pubertal status, and change in intracranial volume across adolescence were added as covariates in these analyses.
Indirect effect analysis
To determine whether the changes in regional brain volume mediate the relationship between peer victimization and psychopathology symptoms, indirect effect analyses were carried out in MPlus (version 7) using maximum likelihood estimation. The indirect effects were defined by the product term of the two pathways of interest (i.e., peer victimization to change in brain volume × change in brain volume to psychopathology symptoms). Because SEs underlying indirect effects are often skewed, we bootstrapped all indirect effects 10,000 times with bias-corrected 95% confidence intervals. These models controlled for sex, study site, SES, pubertal status, and change in intracranial volume.
Results
Participants
Of the 682 participants, 46% were male. Their age at each study time point was as follows: baseline: 14.4 ± 0.4 (mean ± SD); follow-up 1: 16.5 ± 0.6; follow-up 2: 19.0 ± 0.7.
Latent profile analysis of peer victimization
Latent profile analysis was used to identify classes (i.e., subgroups) of individuals with a chronically high level of peer victimization across adolescence using the peer victimization sum scores from ages 14, 16, and 19. Peer victimization scores for each time point were as follows (mean ± SD; range): age 14 (4.0 ± 1.6; 3–13); age 16 (3.5 ± 1.2; 3–13); age 19 (3.3 ± 1.0; 3–15).
Latent profile analysis of peer victimization identified a chronically victimized group of 36 individuals (entropy = 0.99; see Fig. 1; 38% male), representing 5% of the overall sample. Latent profile analysis also identified a much larger low peer victimization group (n = 646; 46% male). There was no significant difference in sex between the chronic and low peer victimization groups (χ2 = 0.751, df = 1, p = 0.386). Considering the substantial group size difference, we tested for homogeneity of variance in our variables of interest (i.e., changes in brain volumes and psychopathology symptoms). All variables met the assumption of homogeneity of variance (i.e., p-value >0.05) except the depression probability rating from the DAWBA (Levene’s statistic = 11.48, p = 0.001).
Peer victimization and psychopathology symptoms
To validate the peer victimization trajectories with regard to psychopathology, we used the Mann–Whitney U-test to compare psychopathology symptoms between the peer victimization groups. Individuals in the chronically peer-victimized group had higher symptoms scores on the SDQ (emotional symptoms: U = 7829.0, r = −0.13, p = 0.001; hyperactivity: U = 8223.0, r = −0.11, p = 0.003) and greater symptom diagnostic probabilities on the DAWBA (depression: U = 6557.0, r = −0.13, p = 0.001 and generalized anxiety: U = 9101.5, r = −0.10, p = 0.006).
Peer victimization and adolescent brain development (nonparametric partial correlation)
As described above, 18 bilateral frontal, limbic, and basal ganglia ROIs were entered into the analyses considering they have previously been identified as having a relationship with stress and maltreatment [21, 35,36,37]. Only two ROIs were associated with peer victimization and survived false discovery rate correction and were included in subsequent analyses: changes in left caudate (ρ = −0.086, p = 0.032) and putamen (ρ = −0.101, p = 0.012) volume were negatively associated with peer victimization.
Peer victimization and adolescent brain development (repeated measures ANOVA)
We then carried out a 2-by-2 repeated measures ANOVA analyses to further probe the longitudinal relationship between peer victimization and adolescent brain development. Region-of-interest volumes at ages 14 and 19 were the within-subject variable and peer victimization class was the between-subjects variable. The repeated measures ANOVAs identified a significant brain volume-by-peer victimization interaction for the left putamen (ηp² = 0.006, SS = 30850.41, F = 4.38, p = 0.037; Table 1).
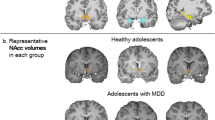
On average, the volume of the putamen decreased across adolescence in all individuals (left putamen: −83.62 ± 86.79). As shown in Fig. 2, the brain volume-by-peer victimization interaction suggests that individuals who have been chronically victimized have steeper decreases in putamen volume than their less victimized counterparts.
Post-hoc analyses
Comparison of the age 14 and age 19 volumes between groups suggests that putamen volume is significantly larger in the chronically victimized group at age 14 (t = −2.966, p = 0.003, d = 0.49) but not at age 19 (t = −1.834, p = 0.067, d = 0.30). We also found that greater peer victimization at age 14 was related to larger putamen volumes at age 14 (r = 0.076, p = 0.049) and that peer victimization score at age 14 did significantly relate to change in putamen volume (r = −0.087, p = 0.024) such that individuals with higher victimization scores had greater decreases in putamen volume over time.
Sensitivity analyses
Considering the observed brain volume-by-peer victimization interaction might differ according to sex, repeated measures ANOVA were rerun including sex as a between-subjects variable. However, there was no influence by sex as the 3-way interaction was not significant (Supplementary Table 2).
To verify that the brain volume-by-peer victimization interaction was uniquely significant when also examining other types of early life stress, we reran the model controlling for childhood trauma and SLE. After controlling for childhood trauma and stressful life events, the interaction remained significant (Supplementary Table 3), suggesting that the effect is unique to peer victimization and not stressful life events in general.
Adolescent brain development and psychopathology symptoms
Considering the observed relationships of peer victimization with putamen volume changes and psychopathology symptoms, we used multiple regression analyses to determine whether there might also be a relationship between changes in putamen volumes and psychopathology symptoms. Regression analyses identified a negative relationship between the change in putamen volume and generalized anxiety (t = −2.32, p = 0.020). This relationship remained significant after controlling for childhood trauma and SLE (t = −2.31, p = 0.021) in the model. Neither depression nor hyperactivity was significant.
Indirect effects analysis
Because peer victimization was associated with changes in regional brain volumes that were, in turn, associated with psychopathology symptoms, we ran an indirect effect model to test whether changes in brain volumes might be a biological means by which peer victimization influences psychopathology symptoms at age 19. The indirect effect model (Fig. 3a; “c” path) showed that peer victimization was indirectly associated with generalized anxiety via decreases in the volume of the putamen, as the 95% confidence intervals excluded 0 (β = 0.439, bias-corrected bootstrapping 95% CI = 0.004–0.109; Table 2).
Diagram of path model of indirect effects. The “c” path indicates the direct effect of peer victimization on generalized anxiety. The “a” path indicates the relationship between peer victimization and the mediating variable, change in brain volume, whereas the “b” path indicates that the change in brain volume is correlated with the outcome, generalized anxiety. The “c′” path indicates that peer victimization is indirectly associated with generalized anxiety via changes in putamen volume (ab). Standardized path coefficients are presented for the putamen (a) and caudate (exploratory; b) models
Because the caudate is functionally related to the putamen, and the volumetric change of the left caudate was also associated with generalized anxiety, we ran an exploratory indirect effect model with the left caudate. We found that peer victimization was also indirectly associated with generalized anxiety via decreases in caudate volume (β = 0.036, 95% CI = 0.002–0.099; Fig. 3b; Table 2).
Since the volumetric changes in these two regions are correlated (left caudate–left putamen partial correlation: r = 0.541, p = 3 × 10−52), we put both victimization-brain-symptom models into one indirect effects analysis. By doing this and, therefore, accounting for the associations between the two brain regions, we found that peer victimization was still associated with generalized anxiety via decreases in left putamen volume (β = 0.039, bias-corrected bootstrapping 95% CI = 0.004–0.103) as well as left caudate volume (β = 0.039, bias-corrected bootstrapping 95% CI = 0.004–0.108).
Sensitivity analyses
We conducted sensitivity analyses for the “all-in-one” models and found peer victimization was still associated with generalized anxiety via decreases in both the left putamen and caudate when controlling for both stressful life events and childhood maltreatment, as well as comorbid depressive symptoms at ages 14 and 19. The result statistics are included in the online Supplement (Results and Table 5).
Discussion
This study examined how chronic peer victimization affects adolescent brain development and whether such developmental changes are associated with the relationship between victimization and mental health. Our findings validated literature linking peer victimization with mental health problems. However, there are two novel ways in which our findings extend the current literature: first, chronic adolescent peer victimization impacts structural brain development and, second, changes in brain structure are related to psychopathology symptoms in late adolescence/early adulthood. Furthermore, we found that peer victimization positively associates with anxiety symptoms indirectly via these brain changes. Specifically, we found that chronic peer victimization was associated with steeper decreases in left putamen volume. Importantly, these findings were unique to peer victimization and not other types of stress or comorbid depression. Together, these results are, to our knowledge, the first to identify a possible mechanism by which adolescent peer victimization impacts the development of anxiety in young adults.
The striatum, comprised in part by the putamen, matures from late adolescence into adulthood [43,44,45], evidenced by volumetric decreases [46], but there are inconsistencies as to how stress affects maturation trajectories during childhood and adolescence versus adulthood. Cross-sectional neuroimaging studies of early life stress such as childhood maltreatment find both smaller and larger gray matter volumes during early adolescence [35, 47, 48]. However, cross-sectional studies carried out in adults who have experienced early life stress and maltreatment find they have smaller gray matter volumes compared to controls [17, 21, 37, 38].
The current results revealed that the putamen, and to a lesser degree the caudate, were larger in the chronically peer-victimized group at age 14 but became more similar in volume to the non-victimized group by age 19. This raised the question of whether the degree of initial peer victimization (age 14) was also related to brain volumes and indeed it was correlated with age 14 putamen volume as well as the change in putamen volume across adolescence. The difference in volumes at age 14 might be due to the chronically victimized individuals having been exposed to victimization long before their participation in the IMAGEN study, as peer victimization can begin as early as preschool and kindergarten [49, 50]. Recent studies have explored peer victimization trajectories in childhood and adolescence, identifying three to five victimization classes [51,52,53,54], one of which is a chronic/severe group. There is no consensus as to the number and composition of peer victimization trajectories identified in these studies, and the age ranges examined differ not only between the studies but also with our sample. Altogether the findings from these studies suggest that ours does not fully capture the lifetime extent of peer victimization in the chronic group and this could indeed help explain the brain volume differences we see at age 14.
Our results support the finding that putamen volume decreases across adolescence [45], the likely result of increased synaptic pruning, decreased glial cell number, or increases in myelination/axon caliber [2]—neurobiological processes believed to underlie the neuroimaging-derived changes observed across adolescence. Considering the decrease in putamen volume was more pronounced in the chronically victimized group, it suggests an exaggeration of the aforementioned neurobiological processes in the chronically victimized group. We speculate that the temporal snapshot presented herein does not capture the full neurobiological extent of peer victimization-related changes. If the current study had a subsequent third neuroimaging time point, perhaps it might reveal that indeed putamen and caudate volumes are significantly smaller in the chronically victimized group further into adulthood.
We found that changes in putamen and caudate volumes were related to psychopathology outcomes at age 19, specifically, generalized anxiety, even when controlling for other types of stress and comorbid depressive symptoms. Although not classically considered relevant to anxiety, the importance of structural changes in the putamen and caudate to the development of anxiety most likely lies in their contribution to related behaviors such as reward sensitivity, motivation, conditioning, attention, and emotional processing [55]. Along with the nucleus accumbens, the putamen and caudate comprise the “striatum.” While they appear structurally separate (i.e., divided by the white matter of the internal capsule), there is functional integration between the two regions; interneurons in the striatum have been shown to cross-functional pathway boundaries in animal models supporting the notion that these nearby areas have overlapping functions [56]. It is well established that with the incoming projections from the frontal cortex, the striatum is essential for voluntary motor control and, therefore, behavior. But considering the striatum is essential for reward processing (i.e., learning) and also receives projections from the amygdala, which itself plays a key role in the emotional processing of incoming information, the striatum is involved in processes that drive complex behaviors disrupted in anxiety. In support of this, functional MRI studies have found that caudate and putamen activation [57, 58] and connectivity [59,60,61] differ in individuals with anxiety disorders.
The most salient finding was that peer victimization’s effect on psychopathology was due, in part, to decreases in caudate and putamen volume. Many correlational studies of stress–brain–mental health relationships exist, but few studies have identified whether stress affects mental health via the brain. One such study found that reduced gray matter volume in the orbitofrontal cortex mediated the relationship between maltreatment and peer problems in childhood [62], while another found reduced parahippocampal gyrus thickness mediated the relationship between childhood maltreatment and adolescent antisocial behavior [63]. Our findings add to the nascent literature linking smaller brain structures with stress and mental health but are the first to do so related to peer victimization.
We did not find time-by-peer victimization effects on other plausible brain regions such as the amygdala and hippocampus. One reason might be that stress-sensitivity periods differ across these brain regions [64] and theirs preceded the window of victimization captured in this study. And while we acknowledge that the chronically victimized individuals were likely victimized by peers prior to their entry in the study, we did not have the data to investigate this. An additional reason we do not see the same effects is that the impact of peer victimization in these other areas did not manifest as structural changes but perhaps as molecular changes or functional connectivity changes in the relevant circuits [64].
Limitations of the present study include the fact that we could not account for the experience of peer victimization or other early life stressors before age 14. Perhaps these individuals had been victimized since childhood and some structural brain changes precede the window of time captured in our study. Some studies have shown sex differences in normal brain development trajectories [46, 65, 66], but we did not find a three-way interaction between victimization group, brain volume changes, and sex; we were likely underpowered to detect such an effect. The imbalance in the number of individuals in each of the two victimization groups limited us in terms of statistics that could be carried out, but the imbalance is not surprising since victimization prevalence typically decreases from childhood to adulthood. By examining regions previously implicated in maltreatment and/or victimization, rather than taking an unbiased approach, we might have overlooked changes in other brain regions linked to chronic peer victimization. While methodological approaches like a whole-brain analysis could have uncovered such brain areas, we did not undertake them for reasons of statistical power due to the imbalanced group sizes.
Our data are the first to show that chronic peer victimization during adolescence impacts mental health via structural brain changes. Because frequently peer-victimized adolescents are two to three times more likely to develop an anxiety disorder [12], early interventions to limit peer victimization could mitigate the adolescent neurobiological changes underlying the development of psychopathology.
References
Fuhrmann D, Knoll LJ, Blakemore SJ. Adolescence as a sensitive period of brain development. Trends Cogn Sci. 2015;19:558–66.
Paus T, Keshavan M, Giedd JN. Why do many psychiatric disorders emerge during adolescence? Nat Rev Neurosci. 2008;9:947–57.
Juvonen JGS. Peer harassment in school: the plight of the vulnerable and victimized. Guilford Press; 2001.
Hunter SC, Boyle JM, Warden D. Perceptions and correlates of peer-victimization and bullying. Br J Educ Psychol. 2007;77(Pt 4):797–810.
Sumter SR, Baumgartner SE, Valkenburg PM, Peter J. Developmental trajectories of peer victimization: off-line and online experiences during adolescence. J Adolesc Health. 2012;50:607–13.
Pellegrini A, Long J. A longitudinal study of bullying, dominances, and victimization during the transition from primary school through secondary school. Br J Dev Psychol. 2002;20:259–80.
Barker ED, Arseneault L, Brendgen M, Fontaine N, Maughan B. Joint development of bullying and victimization in adolescence: relations to delinquency and self-harm. J Am Acad Child Adolesc Psychiatry. 2008;47:1030–8.
Sourander A, Helstela L, Helenius H, Piha J. Persistence of bullying from childhood to adolescence--a longitudinal 8-year follow-up study. Child Abus Negl. 2000;24:873–81.
Takizawa R, Maughan B, Arseneault L. Adult health outcomes of childhood bullying victimization: evidence from a five-decade longitudinal British birth cohort. Am J Psychiatry. 2014;171:777–84.
Arseneault L, Bowes L, Shakoor S. Bullying victimization in youths and mental health problems: ‘much ado about nothing’? Psychol Med. 2010;40:717–29.
Gladstone GL, Parker GB, Malhi GS. Do bullied children become anxious and depressed adults? A cross-sectional investigation of the correlates of bullying and anxious depression. J Nerv Ment Dis. 2006;194:201–8.
Stapinski LA, Bowes L, Wolke D, Pearson RM, Mahedy L, Button KS, et al. Peer victimization during adolescence and risk for anxiety disorders in adulthood: a prospective cohort study. Depress Anxiety. 2014;31:574–82.
Lereya ST, Copeland WE, Costello EJ, Wolke D. Adult mental health consequences of peer bullying and maltreatment in childhood: two cohorts in two countries. Lancet Psychiatry. 2015;2:524–31.
Evans-Lacko S, Takizawa R, Brimblecombe N, King D, Knapp M, Maughan B, et al. Childhood bullying victimization is associated with use of mental health services over five decades: a longitudinal nationally representative cohort study. Psychol Med. 2017;47:127–35.
Singham T, Viding E, Schoeler T, Arseneault L, Ronald A, Cecil CM, et al. Concurrent and longitudinal contribution of exposure to bullying in childhood to mental health: the role of vulnerability and resilience. JAMA Psychiatry. 2017;74:1112–9.
Schaefer J, Moffitt T, Arseneault L, Danese A, Fisher HL, Houts R, et al. Adolescent victimization and early-adult psychopathology: approaching causal inference using a longitudinal twin study to rule out noncausal explanations. Clin Psychol Sci. 2017. 2018 May; 6:352–371.
van Harmelen AL, van Tol MJ, van der Wee NJ, Veltman DJ, Aleman A, Spinhoven P, et al. Reduced medial prefrontal cortex volume in adults reporting childhood emotional maltreatment. Biol Psychiatry. 2010;68:832–8.
Teicher MH, Anderson CM, Polcari A. Childhood maltreatment is associated with reduced volume in the hippocampal subfields CA3, dentate gyrus, and subiculum. Proc Natl Acad Sci USA. 2012;109:E563–72.
Lim L, Radua J, Rubia K. Gray matter abnormalities in childhood maltreatment: a voxel-wise meta-analysis. Am J Psychiatry. 2014;171:854–63.
Dannlowski U, Stuhrmann A, Beutelmann V, Zwanzger P, Lenzen T, Grotegerd D, et al. Limbic scars: long-term consequences of childhood maltreatment revealed by functional and structural magnetic resonance imaging. Biol Psychiatry. 2012;71:286–93.
Cohen RA, Grieve S, Hoth KF, Paul RH, Sweet L, Tate D, et al. Early life stress and morphometry of the adult anterior cingulate cortex and caudate nuclei. Biol Psychiatry. 2006;59:975–82.
Berking M, Wupperman P. Emotion regulation and mental health: recent findings, current challenges, and future directions. Curr Opin Psychiatry. 2012;25:128–34.
Cardinal RN, Winstanley CA, Robbins TW, Everitt BJ. Limbic corticostriatal systems and delayed reinforcement. Ann N Y Acad Sci. 2004;1021:33–50.
Kalivas PW, Volkow ND. The neural basis of addiction: a pathology of motivation and choice. Am J Psychiatry. 2005;162:1403–13.
Andersen SL, Teicher MH. Stress, sensitive periods and maturational events in adolescent depression. Trends Neurosci. 2008;31:183–91.
Gogtay N, Giedd JN, Lusk L, Hayashi KM, Greenstein D, Vaituzis AC, et al. Dynamic mapping of human cortical development during childhood through early adulthood. Proc Natl Acad Sci USA. 2004;101:8174–9.
Schumann G, Loth E, Banaschewski T, Barbot A, Barker G, Buchel C, et al. The IMAGEN study: reinforcement-related behaviour in normal brain function and psychopathology. Mol Psychiatry. 2010;15:1128–39.
Olweus D. The revised Olweus Bully/Victim Questionnaire for students. Bergen, Norway: Res. Cent. Health Promot. (HEMIL), Univ. Bergen; 1996.
Goodman R, Ford T, Richards H, Gatward R, Meltzer H. The Development and Well-Being Assessment: description and initial validation of an integrated assessment of child and adolescent psychopathology. J Child Psychol Psychiatry. 2000;41:645–55.
Goodman A, Heiervang E, Collishaw S, Goodman R. The ‘DAWBA bands’ as an ordered-categorical measure of child mental health: description and validation in British and Norwegian samples. Soc Psychiatry Psychiatr Epidemiol. 2011;46:521–32.
Goodman R. The Strengths and Difficulties Questionnaire: a research note. J Child Psychol Psychiatry. 1997;38:581–6.
Bernstein DP, Ahluvalia T, Pogge D, Handelsman L. Validity of the Childhood Trauma Questionnaire in an adolescent psychiatric population. J Am Acad Child Adolesc Psychiatry. 1997;36:340–8.
Newcomb MD, Huba GJ, Bentler PM. A multidimensional assessment of stressful life events among adolescents. J Health Soc Behav. 1981;22:400–15.
Quinlan EB, Cattrell A, Jia T, Artiges E, Banaschewski T, Barker G, et al. Psychosocial stress and brain function in adolescent psychopathology. Am J Psychiatry. 2017;174:785–94.
Edmiston EE, Wang F, Mazure CM, Guiney J, Sinha R, Mayes LC, et al. Corticostriatal-limbic gray matter morphology in adolescents with self-reported exposure to childhood maltreatment. Arch Pediatr Adolesc Med. 2011;165:1069–77.
Hart H, Rubia K. Neuroimaging of child abuse: a critical review. Front Hum Neurosci. 2012;6:52.
Saleh A, Potter GG, McQuoid DR, Boyd B, Turner R, MacFall JR, et al. Effects of early life stress on depression, cognitive performance and brain morphology. Psychol Med. 2017;47:171–81.
Baker LM, Williams LM, Korgaonkar MS, Cohen RA, Heaps JM, Paul RH. Impact of early vs. late childhood early life stress on brain morphometrics. Brain Imaging Behav. 2013;7:196–203.
Price RB, Kuckertz JM, Siegle GJ, Ladouceur CD, Silk JS, Ryan ND, et al. Empirical recommendations for improving the stability of the dot-probe task in clinical research. Psychol Assess. 2015;27:365–76.
Shete S, Beasley TM, Etzel CJ, Fernandez JR, Chen J, Allison DB, et al. Effect of winsorization on power and type 1 error of variance components and related methods of QTL detection. Behav Genet. 2004;34:153–9.
Petersen AC, Crockett L, Richards M, Boxer A. A self-report measure of pubertal status: reliability, validity, and initial norms. J Youth Adolesc. 1988;17:117–33.
Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J Roy Stat Soc B Met. 1995;57:289–300.
Lenroot RK, Gogtay N, Greenstein DK, Wells EM, Wallace GL, Clasen LS, et al. Sexual dimorphism of brain developmental trajectories during childhood and adolescence. Neuroimage. 2007;36:1065–73.
Teicher MH, Andersen SL, Hostetter JC Jr. Evidence for dopamine receptor pruning between adolescence and adulthood in striatum but not nucleus accumbens. Brain Res Dev Brain Res. 1995;89:167–72.
Sowell ER, Thompson PM, Holmes CJ, Jernigan TL, Toga AW. In vivo evidence for post-adolescent brain maturation in frontal and striatal regions. Nat Neurosci. 1999;2:859–61.
Lenroot RK, Giedd JN. Brain development in children and adolescents: insights from anatomical magnetic resonance imaging. Neurosci Biobehav Rev. 2006;30:718–29.
Liao M, Yang F, Zhang Y, He Z, Song M, Jiang T, et al. Childhood maltreatment is associated with larger left thalamic gray matter volume in adolescents with generalized anxiety disorder. PLoS ONE. 2013;8:e71898.
De Brito SA, Viding E, Sebastian CL, Kelly PA, Mechelli A, Maris H, et al. Reduced orbitofrontal and temporal grey matter in a community sample of maltreated children. J Child Psychol Psychiatry. 2013;54:105–12.
Barker ED, Boivin M, Brendgen M, Fontaine N, Arseneault L, Vitaro F, et al. Predictive validity and early predictors of peer-victimization trajectories in preschool. Arch Gen Psychiatry. 2008;65:1185–92.
Crick NR, Casas JF, Ku HC. Relational and physical forms of peer victimization in preschool. Dev Psychol. 1999;35:376–85.
Sheppard CS, Giletta M, Prinstein MJ. Peer victimization trajectories at the adolescent transition: associations among chronic victimization, peer-reported status, and adjustment. J Clin Child Adolesc Psychol. 2016;1–10.
Geoffroy MC, Boivin M, Arseneault L, Renaud J, Perret LC, Turecki G, et al. Childhood trajectories of peer victimization and prediction of mental health outcomes in midadolescence: a longitudinal population-based study. CMAJ. 2018;190:E37–43.
Ladd GW, Etteka I, Kochenderfer-Ladd B. Peer victimization trajectories from kindergarten through high school: differential pathways for children’s school engagement and achievement? J Educ Psychol. 2017;109:826–41.
Rosen LH, Beron KJ, Underwood MK. Social victimization trajectories from middle childhood through late adolescence. Soc Dev. 2017;26:227–47.
Lago T, Davis A, Grillon C, Ernst M. Striatum on the anxiety map: small detours into adolescence. Brain Res. 2017;1654(Pt B):177–84.
Haber SN. Corticostriatal circuitry. Dialogues Clin Neurosci. 2016;18:7–21.
Perez-Edgar K, Hardee JE, Guyer AE, Benson BE, Nelson EE, Gorodetsky E, et al. DRD4 and striatal modulation of the link between childhood behavioral inhibition and adolescent anxiety. Soc Cogn Affect Neurosci. 2014;9:445–53.
Guyer AE, Choate VR, Detloff A, Benson B, Nelson EE, Perez-Edgar K, et al. Striatal functional alteration during incentive anticipation in pediatric anxiety disorders. Am J Psychiatry. 2012;169:205–12.
Wang X, Li J, Yuan Y, Wang M, Ding J, Zhang J, et al. Altered putamen functional connectivity is associated with anxiety disorder in Parkinson’s disease. Oncotarget. 2017;8:81377–86.
Liu WJ, Yin DZ, Cheng WH, Fan MX, You MN, Men WW, et al. Abnormal functional connectivity of the amygdala-based network in resting-state FMRI in adolescents with generalized anxiety disorder. Med Sci Monit. 2015;21:459–67.
Qiao J, Li A, Cao C, Wang Z, Sun J, Xu G. Aberrant functional network connectivity as a biomarker of generalized anxiety disorder. Front Hum Neurosci. 2017;11:626.
Kelly PA, Viding E, Puetz VB, Palmer AL, Mechelli A, Pingault JB, et al. Sex differences in socioemotional functioning, attentional bias, and gray matter volume in maltreated children: a multilevel investigation. Dev Psychopathol. 2015;27(4 Pt 2):1591–609.
Busso DS, McLaughlin KA, Brueck S, Peverill M, Gold AL, Sheridan MA. Child abuse, neural structure, and adolescent psychopathology: a longitudinal study. J Am Acad Child Adolesc Psychiatry. 2017;56:321–8.e1.
Teicher MH, Samson JA, Anderson CM, Ohashi K. The effects of childhood maltreatment on brain structure, function and connectivity. Nat Rev Neurosci. 2016;17:652–66.
Brain Development Cooperative Group. Total and regional brain volumes in a population-based normative sample from 4 to 18 years: the NIH MRI study of normal brain development. Cereb Cortex. 2012;22:1–12.
Herting MM, Sowell ER. Puberty and structural brain development in humans. Front Neuroendocrinol. 2017;44:122–37.
Acknowledgements
This work received support from the following sources: the European Union-funded FP6 Integrated Project IMAGEN (Reinforcement-related behavior in normal brain function and psychopathology) (LSHM-CT- 2007-037286), the Horizon 2020 funded ERC Advanced Grant “STRATIFY” (Brain network based stratification of reinforcement-related disorders) (695313), ERANID (Understanding the Interplay between Cultural, Biological and Subjective Factors in Drug Use Pathways) (PR-ST-0416-10004), BRIDGET (JPND: BRain Imaging, cognition Dementia and next generation GEnomics) (MR/N027558/1), the FP7 projects IMAGEMEND (602450; IMAging GEnetics for MENtal Disorders) and MATRICS (603016), the Innovative Medicine Initiative Project EU-AIMS (115300-2), the Medical Research Council Grant “c-VEDA” (Consortium on Vulnerability to Externalizing Disorders and Addictions) (MR/N000390/1), the Swedish Research Council FORMAS, the Medical Research Council, the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London, the Bundesministeriumfür Bildung und Forschung (BMBF grants 01GS08152; 01EV0711; eMED SysAlc01ZX1311A; Forschungsnetz AERIAL 01EE1406A), the Deutsche Forschungsgemeinschaft (DFG grants SM 80/7-1, SM 80/7-2, SFB 940/1). Further support was provided by grants from: ANR (project AF12-NEUR0008-01-WM2NA, and ANR-12-SAMA-0004), the Fondation de France, the Fondation pour la Recherche Médicale, the Mission Interministérielle de Lutte-contre-les-Drogues-et-les-Conduites-Addictives (MILDECA), the Assistance-Publique-Hôpitaux-de-Paris and INSERM (interface grant), Paris Sud University IDEX 2012; the National Institutes of Health, Science Foundation Ireland (16/ERCD/3797), U.S.A. (Axon, Testosterone and Mental Health during Adolescence; RO1 MH085772-01A1), and by NIH Consortium grant U54 EB020403, supported by a cross-NIH alliance that funds Big Data to Knowledge Centres of Excellence.
Other IMAGEN Consortium members
Pausova Z., Mann K., Barker G.J., Lawrence C., Rietschel M., Robbins T.W., Williams S., Nymberg C., Topper L., Smith L., Havatzias S., Stueber K., Mallik C., Clarke T.K., Stacey D., Peng Wong C., Werts H., Williams S., Andrew C., Häke I., Ivanov N., Klär A., Reuter J., Palafox C., Hohmann C., Lüdemann K., Romanowski A., Ströhle A., Wolff E., Rapp M., Ihlenfeld A., Walaszek B., Schubert F., Connolly C., Jones J., Lalor E., McCabe E., NíShiothcháin A., Spanagel R., Sommer W., Steiner S., Buehler M., Stolzenburg E., Schmal C., Schirmbeck F., Heym N., Newman C., Huebner T., Ripke S., Mennigen E., Muller K., Ziesch V., Lueken L., Yacubian J., Finsterbusch J., Bordas N., Bricaud Z., Galinowski A., Gourlan C., Schwartz Y., Lalanne C., Barbot A., Thyreau B., Subramaniam N., Theobald D., Richmond N., de Rover M., Molander A., Jordan E., Robinson E., Hipolata L., Moreno M., Arroyo M., Stephens D., Ripley T., Crombag H., Lathrop M., Lanzerath D., Heinrichs B., Spranger T., Resch F., Haffner J., Parzer P., Brunner R., Constant P., Mignon X., Thomsen T., Vestboe A., Ireland J., Rogers J.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
T.B. has served as an advisor or consultant to Bristol-Myers Squibb, Desitin Arzneimittel, Eli Lilly, Medice, Novartis, Pfizer, Shire, UCB, and Vifor Pharma; he has received conference attendance support, conference support, or speaking fees from Eli Lilly, Janssen McNeil, Medice, Novartis, Shire, and UCB; and he is involved in clinical trials conducted by Eli Lilly, Novartis, and Shire; the present work is unrelated to these relationships. E.D.B. has received funding for a PhD student and honoraria for teaching on scanner programming courses from General Electric Healthcare; he acts as a consultant for IXICO. H.W. received a speaker honorarium from Servier (2014). The remaining authors declare that they have no conflict of interest.
Additional information
Members of the IMAGEN Consortium are listed below the Acknowledgements.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Quinlan, E.B., Barker, E.D., Luo, Q. et al. Peer victimization and its impact on adolescent brain development and psychopathology. Mol Psychiatry 25, 3066–3076 (2020). https://doi.org/10.1038/s41380-018-0297-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-018-0297-9
- Springer Nature Limited
This article is cited by
-
The impact of psychosocial adversity on brain and behaviour: an overview of existing knowledge and directions for future research
Molecular Psychiatry (2024)
-
Associations of bullying perpetration and peer victimization subtypes with preadolescent’s suicidality, non-suicidal self-injury, neurocognition, and brain development
BMC Medicine (2023)
-
Environmental neuroscience linking exposome to brain structure and function underlying cognition and behavior
Molecular Psychiatry (2023)
-
Emotional processing in bullying: an event-related potential study
Scientific Reports (2022)
-
Biopsychosoziale Therapie der generalisierten Angststörung
Psychotherapeut (2022)