Abstract
Rodent studies indicate that ghrelin receptor blockade reduces alcohol consumption. However, no ghrelin receptor blockers have been administered to heavy alcohol drinking individuals. Therefore, we evaluated the safety, tolerability, pharmacokinetic (PK), pharmacodynamic (PD) and behavioral effects of a novel ghrelin receptor inverse agonist, PF-5190457, when co-administered with alcohol. We tested the effects of PF-5190457 combined with alcohol on locomotor activity, loss-of-righting reflex (a measure of alcohol sedative actions), and on blood PF-5190457 concentrations in rats. Then, we performed a single-blind, placebo-controlled, within-subject human study with PF-5190457 (placebo/0 mg b.i.d., 50 mg b.i.d., 100 mg b.i.d.). Twelve heavy drinkers during three identical visits completed an alcohol administration session, subjective assessments, and an alcohol cue-reactivity procedure, and gave blood samples for PK/PD testing. In rats, PF-5190457 did not interact with the effects of alcohol on locomotor activity or loss-of-righting reflex. Alcohol did not affect blood PF-5190457 concentrations. In humans, all adverse events were mild or moderate and did not require discontinuation or dose reductions. Drug dose did not alter alcohol concentration or elimination, alcohol-induced stimulation or sedation, or mood during alcohol administration. Potential PD markers of PF-5190457 were acyl-to-total ghrelin ratio and insulin-like growth factor-1. PF-5190457 (100 mg b.i.d.) reduced alcohol craving during the cue-reactivity procedure. This study provides the first translational evidence of safety and tolerability of the ghrelin receptor inverse agonist PF-5190457 when co-administered with alcohol. PK/PD/behavioral findings support continued research of PF-5190457 as a potential pharmacological agent to treat alcohol use disorder.
Similar content being viewed by others
Introduction
Only a few medications (disulfiram, oral and intramuscular naltrexone and acamprosate) are approved by the Food and Drug Administration (FDA) for alcohol use disorder (AUD), and each has limited efficacy [1, 2]. Therefore, developing new medications for AUD is a high priority.
The peptide ghrelin is produced by endocrine cells primarily localized in the stomach [3]; its biological functions include regulating growth hormone (GH) secretion, the GH/insulin-like growth factor-1 (IGF-1) axis, food intake, energy expenditure and glucose homeostasis [4, 5]. Ghrelin is acylated by ghrelin-O-acyltransferase (GOAT), and acyl-ghrelin (hereafter mostly referred to as ‘ghrelin’) binds to its G-protein coupled GH secretagogue receptor (GHS-R1a) [6].
Ghrelin has recently been investigated in the context of excessive alcohol consumption and AUD. Central (intracerebroventricular [ICV] or to tegmental areas) or peripheral administration of ghrelin increases alcohol conditioned place preference (CPP) [7, 8] and intake [8]. In AUD individuals, the urge to drink alcohol in response to alcohol cues increased under intravenous ghrelin administration compared to placebo and there was a positive correlation between post-infusion ghrelin concentrations and the increased urge to drink [9]. In a subsequent human laboratory study, intravenous ghrelin administration, compared to placebo, increased alcohol self-administration and modulated brain activity in areas involved in reward processing and stress regulation [10].
There is also evidence that the endogenous ghrelin system is altered in AUD as blood ghrelin concentrations are lower in AUD individuals who are currently drinking compared to healthy controls, while they are higher in AUD individuals who are abstinent [11,12,13,14]. Human studies also indicated a significant positive correlation between blood concentrations of endogenous ghrelin and alcohol craving [11, 14, 15], but see conflicting results in: [16]. Furthermore, human work indicates that blood ghrelin concentrations may predict relapse to alcohol drinking [14].
Preclinical studies with GHS-R1a antagonists (D-Lys3-GHRP-6, BIM28163 or JMV2959) reported a reduction in (a) alcohol-induced locomotor activity, alcohol CPP and accumbal dopamine release in mice [8, 17]; (b) alcohol intake and preference in mice and prairie voles [8, 18,19,20,21,22]; (c) alcohol intake and operant self-administration in mice and alcohol-preferring rats [20, 23]; and (d) alcohol deprivation effect in rats [24].
These studies provide evidence that the GHS-R1a represents a novel pharmacological target to treat AUD, GHS-R1a antagonists are in early preclinical development. Furthermore, GHS-R1a has high intrinsic (ligand-independent) activity [25], therefore, GHS-R1a inverse agonism may be a superior approach compared to competitive antagonism [5]. Reducing constitutive activity of the receptor may provide greater in vivo efficacy through reductions in basal receptor signaling [26,27,28]. As such, we have previously proposed GHS-R1a inverse agonism as an attractive approach to treat AUD patients [5].
PF-5190457 is a GHS-R1a inverse agonist [29] that inhibits constitutive activity of GHS-R1a and competitively blocks its activation by acyl-ghrelin [30]. PF-5190457 is the first GHS-R1a inverse agonist to progress to clinical development. In a Phase 1a trial in healthy humans, PF-5190457 was well-tolerated and safe [31]. However, no clinical studies have been conducted to determine the safety and tolerability of PF-5190457 or any GHS-R1a blocker in people with AUD, or its interaction with alcohol. PF-5190457 may increase sedation/sleepiness and heart rate and lower blood glucose concentrations [31]. These are side-effects that may be exacerbated by alcohol co-administration in addition to other potentially serious consequences of drug–alcohol interactions [32].
Here, we carried out a translational study of the interaction of PF-5190457 and alcohol. We first conducted preclinical experiments to rule out significant safety concerns due to interactions between PF-5190457 and alcohol. Then, in a human laboratory study, we determined (1) the safety and tolerability of two doses of PF-5190457 (50 mg b.i.d. and 100 mg b.i.d) compared to placebo when each was co-administered with alcohol; and (2) the pharmacokinetic (PK) profile of each dose of the drug when co-administered with alcohol. We also explored (1) pharmacodynamic (PD) biomarkers of PF-5190457, i.e., plasma ghrelin (acyl and total), GH and IGF-1 concentrations; and (2) the effects of PF-5190457 on reactivity to alcohol cues.
Materials and methods
Study drug
PF-5190457 (molecular weight = 512 Da) is a member of a spiro-azetidino-piperidine series identified by Pfizer Pharmaceuticals using high-throughput screening for its potential beneficial effects on body weight and glucose homeostasis [33]. PF-5190457 is an orally bioavailable, potent and selective GHS-R1a inverse agonist [29].
Rat experiments
Study approval
The animal experiments were carried out following the National Institutes of Health (NIH) Guidelines for Care and Use of Laboratory Animals and were approved by the Animal Care and Use Committee of the National Institute on Alcohol Abuse and Alcoholism (NIAAA).
Rats
Male Wistar rats (Charles River, Wilmington, MA), were housed two per cage in a temperature and humidity controlled vivarium maintained on a reverse 12 h light/dark cycle, with the light switched off at 7:00 A.M. Experiments were conducted during the dark cycle. Prior to initiating the experiments, rats were repeatedly handled to ensure habituation to the experimenters. Food and water were available ad libitum.
Pilot dose-finding experiment
The doses and pre-treatment times for PF-5190457, administered intraperitoneally (i.p.), were determined from previous rodent studies conducted by the manufacturer that administered this compound by gavage. Wistar rats were injected with PF-5190457 given at five doses (0.3, 1, 3, 10 and 30 mg/kg i.p.), 15 min (n = 2 rats per each dose) or 60 min (n = 2 rats per each dose). Before harvesting, brains were perfused with saline to remove any residual blood. Receptor occupancy was estimated from (1) PF-5190457 concentrations in plasma and brain tissue measured by ultra-performance liquid chromatography-mass spectrometry-tandem mass spectrometry (UPLC-MS/MS) assays that our team developed previously [34]; and (2) IC50 value from rat GHS-R1a filter study and unbound fraction of PF-5190457, measured using equilibrium dialysis (information provided by Pfizer).
Locomotor activity experiments
Based on procedures previously described [35], we used a 3 × 2 design, in which rats (N = 20) were first injected with saline or PF-5190457 (3, 10 mg/kg), followed after 60 min by saline or alcohol [0.5 g/kg 20% v/v i.p.]. Immediately upon receiving the second injection, rats were placed in locomotor boxes, and the total distance traveled was recorded for 30 min by a video-tracking system. The same experiment was repeated with alcohol at 1 g/kg (20% v/v). A separate group of rats was used for each of the six conditions.
Loss-of-righting-reflex (LORR) was measured in rats (N = 39) based on procedures previously described [35]. A highly sedating dose of alcohol, 3.5 g/kg (20% v/v) i.p. was used and the same doses of PF-5190457 (0, 3, 10 mg/kg) as above were tested. The time required for each rat to lose and then regain its righting reflex was recorded.
Alcohol - PF-5190457 PK experiment. Rats (N = 40) were tested in a 3 × 2 design: PF-5190457 (0, 3, 10 mg/kg) x alcohol (3.5 g/kg; 20% v/v) or saline i.p. Tail blood draws were taken 60 min after injections and PF-5190457 concentrations were measured.
Human laboratory study
Study design
This was a phase 1b, within-subjects, dose-escalating, single-blind, placebo-controlled human laboratory study with oral PF-5190457 (placebo/0 mg b.i.d., 50 mg b.i.d. and 100 mg b.i.d.), conducted at the NIH Clinical Center, Bethesda, Maryland, USA.
Study approvals
The human study was approved by the NIH Addictions Institutional Review Board and monitored by a Data Safety Monitoring Board. Written informed consent was obtained from participants prior to inclusion in the study. The study was conducted under a federal Certificate of Confidentiality. The use of PF-5190457 in this study was under the FDA Investigational New Drug (IND) 119,365. Alcohol administration procedures were consistent with the NIAAA Council Guidelines on Alcohol Administration (https://www.niaaa.nih.gov/Resources/ResearchResources/job22.htm).
PF-5190457 doses
Doses were chosen based on previous human data, in which PF-5190457 dose-dependently inhibited GHS-R1a-mediated responses. Specifically, the 100 mg b.i.d. dose of PF-5190457 resulted in maximum receptor inhibition (i.e., 77% inhibition in intravenous ghrelin-induced GH release in humans) with acceptable safety and tolerability; the 50 mg b.i.d. dose was pharmacologically active but less likely to give potential dose-related side-effects [31].
Study sample
Eligible participants were current heavy alcohol drinking males and females (≥21 drinks/week for men or ≥14 drinks/week for women based on the 90-day timeline follow-back (TLFB) at screening) who were not seeking treatment for alcohol-related problems. Participants were consumers of beer, wine and/or spirits. Participants were recruited through word of mouth and local advertisements posted in electronic and printed local media and websites. Potential candidates were first evaluated over the phone. Qualified candidates came to the NIH Clinical Center, signed an informed consent to enroll in a screening protocol that allowed investigators to assess inclusion/exclusion criteria (see Supplementary Appendix S1). Participants received monetary compensation for participation in this study.
Study procedures
Study procedures began after signing an informed consent.
There were three identical inpatient stays (Visits 1–3) separated by ≥3 days. The inpatient setting allowed us to ensure 100% compliance with the study medication and experimental procedures, as well as abstinence from alcohol and close safety monitoring. Study medication was administered from Day 1 to Day 3 for a total of 5 doses (Supplementary Table S1) to reach steady-state before the alcohol administration procedure on Day 3.
Each day, a battery of assessments was conducted, as detailed below and in Supplementary Tables S2–S3. On Day 3, approximately 30 min after the 5th dose of PF-5190457, a drink containing the same type of alcohol (40% Alcohol By Volume; 80% Proof) for all subjects was administered. The quantity of alcohol was calculated for each subject to achieve a blood alcohol concentration of approximately 0.06 mg/dL. The calculation was based on total body water using standard equations and consistent with previous work [36]. The alcohol was administered as a mixed drink containing the subject’s preferred mixer (subjects chose from a list of seven common mixers). Alcohol administration was followed by a battery of repeated assessments as detailed below. The following day, participants were discharged after a clinical assessment and debriefing about which drug condition they thought they received.
During each inpatient stay, participants received meals standardized for macronutrients and caloric content (Supplementary Table S4). Approximately 1–2 weeks after Visit 3, participants came back for a brief outpatient clinical assessment and interview, during which participants’ health, safety and alcohol consumption were evaluated and a counseling session was delivered according to NIAAA guidelines (https://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/clinicians_guide.htm). Their alcohol consumption since Visit 3 was also assessed using TLFB [37].
Assessments
For the study assessments, please see Supplementary Tables S2–S3
Adverse events (AEs)
A health care provider queried the study participant about AEs using a Symptoms Checklist. A ‘yes’ answer to any symptom triggered an AE which was evaluated and documented by a study physician and recorded on an Adverse Events Form (Supplementary Appendices S2–S3). Evaluation included determination of the relationship between the AE and the study procedures (unknown, not related, remotely related, possibly, probably or definitely related) as well as the severity of the AE (mild, moderate, severe, life-threatening). Weight, vital signs, 12-lead electrocardiograms (EKGs), blood tests of liver and renal function, urinalysis and urine drug tests were performed (Supplementary Table S2). Blood glucose concentrations and level of sedation/sleepiness were monitored with fingersticks and the Stanford Sleepiness Scale (SSS [38]), respectively.
PF-5190457 pharmacokinetics
PK blood samples were collected and PF-5190457 plasma concentrations were determined using UPLC–MS/MS [34].
Alcohol concentrations
Alcohol concentrations were determined via breathalyzer.
Neuroendocrine PD biomarkers
Blood total- and acyl-ghrelin, GH and IGF-1 concentrations were determined. Single determinations of these hormones were done in the A.M. of Day 1–3 as well as during the alcohol session on Day 3 (Supplementary Table S2). Total ghrelin was measured by ELISA (EMD Millipore, Billerica, MA), acyl-ghrelin was measured using the Milliplex method (EMD Millipore, Billerica, MA) and GH and IGF-1 were measured by Solid Phase Sandwich ELISAs (R&D Systems Inc., Minneapolis, MN). Procedures for blood collection and storage were consistent with standard operations (including the use of appropriate inhibitors to preserve acyl-ghrelin concentrations) and kit manufacturer guidelines.
Behavioral assessments
The Biphasic Effects of Alcohol Scale (BAES [39]) and the Drug Effects Questionnaire (DEQ [40]) assessed the subjective effects of alcohol after the alcohol administration on Day 3. Mood was assessed with the Profile of Mood States POMS [41]. Food craving was assessed using the General Food-Cravings Questionnaire—State and Trait GFCQ-S/T [42]. Alcohol craving was measured on Day 1 and Day 2 with an 11-point anchored Likert-type Alcohol-Visual Analog Scale A-VAS [43]. This scale was also used on Day 3 during the alcohol session. These assessments were conducted in the patient’s hospital room.
Cue-reactivity procedure
On Day 2, subjects were brought to a bar-like laboratory, where cue-induced alcohol craving was assessed using a cue-reactivity (CR) procedure modified from Monti and colleagues [44]. Personalized food cues were also used during the CR procedure to control for non-alcoholic appetitive behaviors. In order to avoid habituation, we conducted the CR procedure in the placebo and PF-5190457 100 mg b.i.d. conditions only. The procedure consists of three consecutive trials (3 min/trial) done in fixed order: relaxation, food, and alcohol. During the food and alcohol trials, individuals were exposed to visual, tactile, olfactory, and proprioceptive stimuli associated with their preferred food and alcohol choices. However, participants were not allowed to consume the alcohol nor the food they were exposed to during the CR procedure. Unlike the alcohol administration session on Day 3, the type of alcohol beverage was personalized to the type and brand typically consumed by the participant. At baseline and after each trial, subjective alcohol craving was assessed with the Alcohol Urge Questionnaire (AUQ [45]) and food craving with the G-FCQ-S43. The Alcohol Attention Scale (AAS [46]) was administered after the alcohol trial. Physiological changes, including blood pressure, heart rate, and salivation were measured as in other CR studies [9, 36, 44, 47, 48].
Statistics
Rat experiments
All data were analyzed using an analysis of variance (ANOVA), unless otherwise noted, with factors for the respective analysis indicated in conjunction with its results. When appropriate, post hoc comparisons were performed using the Newman-Keuls or Tukey test. The accepted level of significance for all tests was p ≤ 0.05.
Human laboratory study
The sample size of completers (N = 12) was based on Phase 1a clinical studies conducted by the manufacturer [31] that assured that such a number was sufficient to assess the primary aims (safety) and PK data generated in this Phase 1b study. Outcome data were examined for distribution and tested for normality using the Shapiro–Wilks test and, if necessary, transformed to meet these criteria.
As this was a within-subjects design, repeated measures analysis of variance (ANOVA) was used to analyze the primary outcomes (number of AEs and drug concentration), with PF-5190457 dose as the within-subjects factor. Similarly, for secondary outcome measures, repeated measures ANOVAs were used. Post-hoc comparisons were performed using Tukey tests. All analyses were conducted using SAS® software version 9.3 (SAS Institute Inc., Cary, NC). A probability level of 0.05 or lower was considered significant. The Kenward–Roger correction [49] was used in all models analyzed using SAS PROC MIXED, as the use of this correction is highly recommended in repeated measures models [50]. We note that this correction may result in atypical denominator degrees of freedom compared to traditional repeated measures models (e.g., denominator degrees of freedom may actually be higher than the number of subjects).
Non-compartmental analysis (NCA), implemented in Phoenix 64 WinNonlin 6.3 (Certara, Princeton, NJ), was employed in estimating the PK and PD parameters. For PD, only partial area under the curve (AUC) values were computed and compared. Where appropriate, statistical analyses were performed using paired T-test or linear mixed-effects (LME) models with dose and time as fixed effects and subjects as random effect. Tukey post-hoc test was used where appropriate. PK and PD statistical evaluation were implemented in SAS software, version 9.4 (SAS Institute Inc., Cary, NC).
Results
Rat experiments
Dose finding experiment
Supplementary Figure S1 shows the drug concentrations in the brain and plasma as a function of the five PF-5190457 drug conditions (0.3, 1, 3, 10 and 30 mg/kg) at 15 min (Supplementary Figure S1A) and 60 min (Supplementary Figure S1B) post-injection. Modeling estimated a central receptor occupancy of approximately 70% at 3 mg/kg, while near complete receptor occupancy was estimated at both 10 and 30 mg/kg (Supplementary Figure S2). At 60 min, the total brain-to-plasma ratio was 0.4 ± 0.17 (M ± SD). Subsequent experiments used doses of 3 and 10 mg/kg, administered at 60 min prior to the experimental session.
Locomotor activity experiments
There were no alcohol x drug dose interactions for distance traveled at either alcohol dose: 0.5 g/kg (Supplementary Figure S3A) or 1.0 g/kg (Supplementary Figure S3B).
LORR experiment
There was no main effect of drug dose on time required to regain the righting reflex in the alcohol conditions (Supplementary Figure S4A).
Alcohol–PF-5190457 PK experiment
As expected, there was a main effect of drug dose, regardless of alcohol or saline administration, on plasma concentration of PF-5190457, but there was no drug dose x alcohol interaction (Supplementary Figure S4B).
Human laboratory study
Sample description
Fourteen eligible participants signed the informed consent and 12 completed the study. Supplementary Figure S5 outlines the trial flow chart and Supplementary Table S5 outlines the demographics and baseline characteristics. In addition to being active heavy drinkers, most of the participants enrolled in the study (~90%; see Supplementary Table S5) had a current diagnosis of alcohol dependence based on the Diagnostic and Statistical Manual of Mental Disorders IV Edition-Text Revision (DSM-IV-TR) criteria.
Adverse events (AEs)
All AEs were reported as mild or moderate in intensity, and no severe AEs occurred. Tolerability was excellent and there were no discontinuations or dose reductions due to AEs. Total number of AEs was assessed for each drug dosing day (Days 1–3) at each Visit. There was no main effect of drug dose or dosing day on number of AEs. There was no drug dose x dosing day interaction, indicating that there was no drug x alcohol interaction on number of AEs (Supplementary Table S6).
For sleepiness measured with the SSS during drug dosing, there were no main effects of drug dose or time and there was no drug x time interaction. During the alcohol session, there was no main effect of drug dose or drug dose x time interaction, indicating that PF-5190457 did not alter the sedative response as measured by the SSS (Supplementary Figure S6). There was no main effect of drug dose during dosing, or during the alcohol session, on blood glucose concentrations, liver and renal function blood tests, weight, heart rate, respiratory rate, temperature or blood pressure. Analysis of the change in EKG variables from baseline (Day 0: day before drug dosing) to Day 3 showed a main effect (F2,22 = 4.81; p = 0.02) (Supplementary Figure S7) of drug dose on the change in QTcf interval, measured as the difference between Day 3 and the baseline value.
Pharmacokinetic variables
Alcohol concentrations and rate of elimination. PF-5190457 did not affect alcohol concentration (Fig. 1) or elimination (Supplementary Table S7) during the alcohol session.
Human study. Mean (SD) breath alcohol concentration in response to each PF-5190457 drug dose (placebo/0 mg b.i.d.; 50 mg b.i.d.; 100 mg b.i.d.) during the alcohol session (Day 3). The smaller graph in the upper right corner indicates mean breath alcohol concentration expressed as Ln. Study drug was administered at t = 0 min and alcohol at t = 30 min
PF-5190457 concentrations and rate of elimination. The plasma concentration-time profile of PF-5190457 after oral administration increased in a dose-dependent manner and produced similar exposure irrespective of the dose (Fig. 2). The pharmacokinetic parameters of PF-5190457 are presented in Supplementary Table S8. The area under the time curve extrapolated to an infinite time (AUC0-inf) approximately doubled, maximum concentration (Cmax) increased at a rate greater than the dose (~2.4 fold); and the time to Cmax (Tmax), apparent clearance (Cl/F) and apparent volume of distribution (Vd/F) were approximately the same for both PF-5190457 50 mg b.i.d. and 100 mg b.i.d. doses. The half-life of PF-5190457 was estimated to be ~ 6 h. A LME model with Dose and Time Interval as fixed effects and subject as random effect showed that the weighted mean AUC was mainly affected by the drug dose (p ≤ 0.0001). Additionally, the weighted mean AUC was affected by intra- (p < 0.0001) and inter-subject variability (p < 0.0136). The time at which plasma concentration of PF-5190457 was sampled, however, did not affect the weighted mean AUC (p = 0.08).
Human study. Geometric mean concentration–time profile showing the pharmacokinetic profile of PF-5190457 in response to each PF-5190457 drug dose (placebo/0 mg b.i.d.; 50 mg b.i.d.; 100 mg b.i.d.) during the dosing phase and alcohol session. Specifically, the graphs show the pharmacokinetic profile: for both dosing phase and alcohol session combined (a); only during the drug dosing phase (Days 1–2) (b); only during the alcohol session (Day 3) (c); and the natural log-transformed (Ln) concentration–time profile of PF-5190457 during the alcohol session (d)
Finally, we compared PF-5190457 PK data from this study to those generated in the previous Phase 1a first-in-man clinical study by the manufacturer [31]. This comparative analysis, despite differences in the study design, time of blood sampling and analytical methods, did not reveal meaningful differences in pharmacokinetic parameters, suggesting that the alcohol administration in the present study did not change PF-5190457 disposition (Supplementary Table S9).
Pharmacodynamics (PD) neuroendocrine markers
Blood acyl-ghrelin, total ghrelin, IGF-1 and GH concentrations were measured, and the ratio of acyl-to-total ghrelin was calculated on Day 2 (dosing phase) and Day 3 (alcohol session) (Fig. 3). During the drug dosing, there was a significant main effect of drug dose on the acyl-to-total ghrelin ratio (F2,10 = 5.08, p = 0.03; Fig. 3c). During the alcohol session, for total ghrelin (Fig. 3g), there was a significant main effect of time (F8,86 = 9.6, p < 0.0001) and a significant drug dose x time interaction (F16,143 = 2.23, p = 0.007); there was no main effect of drug dose (F2,19 = 2.83, p = 0.09). For IGF-1, during the alcohol session, there was also a significant main effect of time (F8,63 = 9.61, p < 0.0001) and drug dose x time interaction (F16,148 = 4.60, p < 0.0001) which was due to a delayed (22 h post alcohol) increase in IGF-1 concentrations in the PF-5190457 50 mg b.i.d. and 100 mg b.i.d. drug conditions (Fig. 3i). For additional details, see panels a–j of Fig. 3.
Human study. Pharmacodynamic neuroendocrine markers in response to each PF-5190457 drug dose (placebo/0 mg b.i.d.; 50 mg b.i.d.; 100 mg b.i.d.) during the drug dosing phase (Day 2 morning; a–e) and the alcohol session (Day 3; f–j). Arrows denote times of drug (t = 0 min) and alcohol (t = 30 min) administration. Data points at t = 30 min represent baseline for alcohol administration session; alcohol administration occurred following blood draw for these data points. Data are shown as Means (SEM). Details: Drug dosing phase: a acyl-ghrelin; drug dose: F2,10 = 1.18, p = 0.35. b Total ghrelin; drug dose: F2,10 = 0.02, p = 0.97. c Acyl-to-total ghrelin ratio; drug dose: F2,10 = 5.08 *p = 0.03 (significant difference between Placebo and 100 mg b.i.d. drug doses). d IGF-1; drug dose: F2,10 = 1.49, p = 0.27. e GH; drug dose: F2,8 = 2.4, p = 0.15. Alcohol session: f Acyl-ghrelin; drug dose: F2,4 = 0.1, p = 0.91; time: F8,86 = 7.89, p < 0.0001; drug dose x time: F16,144 = 0.99, p = 0.48; time effect: * = different from 30 min time point. g Total ghrelin; drug dose: F2,19 = 2.83, p = 0.09; time: F8,56 = 9.6, p < 0.0001; drug dose x time: F16,143 = 2.23, p = 0.007; interaction effect: # = PF-5190457 100 mg b.i.d. different from both Placebo (0 mg b.i.d.) and PF-5190457 50 mg b.i.d. values. h Acyl-to-total ghrelin ratio; drug dose: F2,29 = 1.62, p = 0.21; time: F8,72 = 2.58, p = 0.02; drug dose x time: F16,146 = 0.88, p = 0.59; time effect: * = different from 30 min time point. i IGF-1; drug dose: F2,17 = 0.78, p = 0.48; time: F8,63 = 9.61, p < 0.0001; drug dose x ime: F16,148 = 4.60, p < 0.0001; time effect: * = different from 60, 120, 180, 240, 360 min time points. For the dose x time interaction, the elevated concentrations at 1350 and 1440 compared to concentrations during the alcohol session are only seen in PF-5190457 50 mg b.i.d. and 100 mg b.i.d. doses. j GH; drug dose: F2,32 = 1.51, p = 0.24; time: F8,57 = 0.49, p = 0.86; drug dose x time: F16,83 = 0.85, p = 0.63
Behavioral assessments
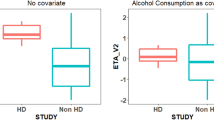
During the alcohol session, PF-5190457 did not significantly affect alcohol-induced sedation or stimulation (Supplementary Figure S8), subjective effects of alcohol (Supplementary Figure S9), or ratings of mood (Supplementary Figure S10). PF-5190457 did not reduce alcohol craving while in the regular hospital room (Fig. 4a). During the alcohol session, there was a drug dose x time interaction (F18, 171 = 2.05, p = 0.01) on alcohol priming-elicited craving (Fig. 4b).
Human Study. Alcohol craving during different phases of the study. Data are shown as Means (SEM). a Alcohol craving during drug dosing phase: there were no main effects of drug dose (F2,11 = 0.22; p = 0.80) or time of day (F1,10 = 0.60; p = 0 .46) and no drug dose x time interaction (F2,14 = 1.52, p = 0.25) on spontaneous alcohol craving (Alcohol-Visual Analog Scale (A-VAS)) in a hospital room. b Alcohol Craving during alcohol session: there was a significant drug dose x time interaction (F18,171 = 2.05; p = 0.01) on alcohol priming-elicited craving (Alcohol-Visual Analog Scale (A-VAS)) during the alcohol session conducted in a hospital room; Tukey post-hoc tests were not significant. There were no main effects of drug dose (F2,19 = 0.30, p = 0.75) or time (F 9,90 = 1.29, p = 0.25) on this measure. Arrows denote times of drug (t = 0 min) and alcohol (t = 30 min) administration. c Alcohol Craving during Cue Reactivity in a bar-like room: there was a main effect of drug (F1,13 = 4.45; p = 0.05; effect size (dz): 0.78), such that alcohol cue-elicited craving (AUQ: Alcohol Urge Questionnaire) in a bar-like room was reduced for the PF-5190457 100 mg b.i.d. versus Placebo. There was also a main effect of Cue type (F2,23 = 4.86; p = 0 .02), where ratings at the end of the alcohol cue trial were significantly higher than the previous relaxation and food trials (*Tukey, p < 0.05). There was no drug x Cue type interaction (F2,30 = 2.69, p = 0.08). d Attention to Alcohol Cues during Cue Reactivity in a bar-like room: The Alcohol Attention Scale (AAS) item “How much did you think about drinking the alcoholic drink when it was presented?” was rated significantly lower at the PF-05190457 100 mg b.i.d. versus Placebo (Mean = 6.8, SEM = 1.0 versus M = 8.9, SEM = 0.6, respectively; F1,11 = 7.07, p = 0.02)
PF-5190457 did not significantly reduce food craving in the regular hospital room, as there was no significant effect of drug dose on food craving assessed by the GFCQ-S score (Fig. 5a).
Human Study. Food craving, as assessed by the General Food-Cravings Questionnaire (G-FCS-Q) – State, during different phases of the study. Data are shown as Means (SEM). a Food Craving during drug dosing phase: there was no main effect of drug dose (F2,10 = 3.14; p = 0.09) on food craving ratings during the drug dosing phase in a hospital room. b–d Food Craving during Cue Reactivity in a bar-like room: b there was a significant drug X Cue type interaction (F2,32 = 8.85; p = .0.001) and a main effect of Cue type (F2,19 = 5.28, p = 0.01) but no main effect of drug (F1,9 = 0.26; p = 0.77) on total food craving G-FCS-Q-State score. Craving was significantly elevated from the Relaxation to the Food trial (*Tukey, p < 0.05) in the Placebo, but not in the PF-5190457 100 mg b.i.d. condition. c There was a significant drug X Cue type interaction (F2,30 = 21.33; p < .0.0001) on the Intense Desire to Eat subscale of the G-FCS-Q-State score. Intense Desire to Eat was significantly elevated from the Relaxation to the Food trial (*Tukey, p < 0.05) in the Placebo, but not in the PF-5190457 100 mg b.i.d. condition. There was no main effect of drug (F1,12 = 3.85, p = 0.07) but there was a main effect of Cue type (F2,30 = 21.33, p = 0.0001). d There was a significant drug X Cue type (F2,31 = 5.21; p = 0.01) on the Anticipation of Positive Reinforcement subscale of the G-FCS-Q-State food craving scale. Anticipation of Positive Reinforcement ratings in the Food trial were significantly higher (+Tukey, p < 0.05) in the Placebo compared to the PF-5190457 100 mg b.i.d. condition. There was a main effect of Cue type (F2,31 = 5.21, p = 0.01) but no main effect of drug (F1,11 = 4.42, p = 0.06)
CR procedure
On Day 2, during the CR procedure conducted in a bar-like laboratory (only PF-5190457 100 mg b.i.d. versus placebo comparison): (a) PF-5190457 versus placebo reduced alcohol cue-elicited craving (F1,13 = 4.45, p = 0.05; effect size (dz) = 0.78) (Fig. 4c); and (b) the AAS item “How much did you think about drinking the alcoholic drink when it was presented?” was rated significantly lower in the PF-05190457 condition versus placebo (F1,11 = 7.07, p = 0.02; Fig. 4d); no significant differences were found on the other four AAS items. With respect to physiologic measurements, during the CR, there was a trend for PF-5190457 to decrease salivation over time compared to placebo with a main effect of drug (F1,6 = 4.31, p = 0.08) and a drug x time interaction (F1,20 = 3.66, p = 0.07). There was a main effect of drug on heart rate during the CR (F1,13 = 15.87, p = 0.002) with higher heart rate in the PF-5190457 condition compared to placebo. This, however, was not clinically significant as all heart rate readings were within normal limits. There was no main effect of PF-5190457 on systolic (F1,11 = 0.22, p = 0.65) or diastolic (F1,11 = 0.72, p = 0.41) blood pressure readings. In addition, during the CR procedure, PF-5190457 compared to placebo blunted food cue-elicited craving (Fig. 5b), as well as G-FCQ-S subscales “Intense Desire to Eat” (Fig. 5c) and “Anticipation of Positive Reinforcement” (Fig. 5d) sub-scales (see Fig. 5 for additional details).
Additional descriptive analyses
Study medication check
Overall subjects guessed their drug condition correctly 48.6% of the time. In the placebo condition they guessed 33.3% correctly, 58.3% correctly in the PF-5190457 50 mg b.i.d. condition, and 54.5% correctly in the PF-5190457 100 mg b.i.d. condition. No significant differences were found among the three conditions (Chi-square = 1.73, df = 2, p = 0.42).
Interval between Visit 1 and Visit 3.
The number of days between Visit 1 and Visit 3 was, on average, 35.33 days (SD = 22.41; min = 11 and max = 82).
Alcohol drinking between visits.
There were no significant differences between visits in the average drinks per drinking day or average drinks per day (TLFB) during the three days prior to each visit (three days was analyzed because that was the minimum interval between visits) (p's > 0.05; data not shown).
Baseline endogenous ghrelin concentrations
Baseline ghrelin refersto its pre-drug concentration on the morning of Day 1 of each visit. There were no significant differences for acyl-ghrelin, total ghrelin or acyl-to-total ghrelin ratio at any of the three visits (p's > 0.05; data not shown). Furthermore, there were no significant correlations between pre-visit alcohol drinking (3 days prior) and baseline ghrelin concentrations (acyl-ghrelin, total ghrelin, acyl-to-total ghrelin ratio) for any of the three visits (p's > 0.05; data not shown).
Alcohol drinking after Visit 3
The average number of drinks per drinking day (TLFB) in the interval between visit 3 and the follow up visit was 6.3 drinks. This was significantly lower compared to that at screening (11.8 drinks) (paired t-test, t = 4.54, p = 0.001). This indicates that the study procedures including study drug and alcohol administration did not increase drinking as assessed over this short interval.
Discussion
This is the first human study of the clinical effects of a GHS-R1a inverse agonist (PF-5190457) when administered with alcohol in heavy drinkers, >90% of whom were alcohol dependent. We found that PF-5190457 has an acceptable concentration–time profile for daily oral dosing and is safe when given with alcohol. This information is critical from a medication development perspective [32]. Therefore PF-5190457 represents a promising compound to investigate GHS-R1a inverse agonism as a novel pharmacotherapy for patients with AUD [5].
Although there was a significant effect of drug on the change of the EKG QTcf interval from Day 0 (before drug dosing) to Day 3, all QTcf values were in the normal range making it difficult to determine the clinical significance of this effect. In addition, this may be due to the decrease by chance in the QTcf interval in the placebo condition. Since the Phase 1a study indicated that somnolence was a common side-effect of PF-5190457 [31], we ruled out significant sedative effects related to PF-5190457 or to the co-administration of alcohol and PF-5190457 with our study in rats before starting our Phase 1b clinical trial. Our human study also indicated a safe and tolerable profile of PF-5190457, even when the drug was combined with alcohol and administered to a population with a history of chronic excessive alcohol use. We did not observe increased sedation with PF-5190457 alone or with PF-5190457 and alcohol, as there was no main effect of time during the alcohol session on Day 3 for measures of sedation. This implies that heavy drinkers may be more tolerant to the sedative effects of PF-5190457, alcohol and PF-5190457/alcohol combined, possibly an effect of neuroadaptations in GABAergic pathways in the context of AUD [51]. Notably, a complex interaction between GABA and ghrelin signaling has been suggested wherein changes in the presynaptic GABA function after chronic alcohol exposure are modulated by ghrelin and GHS-R1a blockade; this interaction results in a significant inhibitory effect on both evoked and spontaneous GABAergic activity [52]. However, there are several study limitations that may have contributed to the absence of significant sedative effects during the combined administration of alcohol and PF-5190457. These include the small sample, the high variability in the BAES Sedation subscales scores (see panel A of Supplementary Figure S8) and the low-medium dose of alcohol administered during the drug-alcohol interaction session. Therefore, future studies are needed to investigate the effects of PF-5190457 on the sedative and stimulant effects of higher doses of alcohol and in larger samples. Such future directions are especially intriguing given recent human work indicating that endogenous ghrelin concentrations predict subjective responses to alcohol in healthy social drinkers [53]. Furthermore, it is important to highlight that ~90% of study participants in our study were African-American and male; therefore, future studies are needed to investigate this novel compound in women and in individuals with different ancestral backgrounds.
A goal of this study was to investigate the PK profile of PF-5190457 in heavy drinkers and in the context of alcohol administration. Our human data indicate that PF-5190457 does not affect alcohol concentrations or elimination. In addition, together with the previous Phase 1 study in healthy controls [31], our human data indicate that alcohol administration did not result in meaningful changes in PF-5190457 disposition in humans. These conclusions are further corroborated by our PK PF-5190457 experiment conducted in rats (see panel B of Supplementary Figure S4).
During the alcohol session, there was a main effect of time where the acyl-ghrelin concentration and the acyl-to-total ghrelin ratio were significantly reduced at early time-points compared to baseline concentrations of those hormones for the session. Without a control group that did not receive alcohol, we cannot exclude the possibility that these reductions were due to mere fluctuations in blood ghrelin concentration over time. Nonetheless, this observation is consistent with previous studies that measured the effect of oral alcohol administration compared to placebo on endogenous ghrelin concentrations. These studies reported a main effect of oral alcohol administration but not a main effect of time in the placebo condition suggesting that ghrelin concentrations, at least in a similar timeframe, do not fluctuate significantly over time [54,55,56,57]. Similarly, we found no significant fluctuation in ghrelin concentrations over a comparable time frame (up to 2 h) in the placebo condition of IV ghrelin/placebo administration studies in alcohol-dependent individuals [9, 10]. Taken together, the present results suggest that the early reduction of both acyl-ghrelin and the acyl-to-total ghrelin ratio during the alcohol session involves some suppression of the endogenous ghrelin system because of alcohol, possibly by action at the ghrelin receptor and/or in other ghrelin-related pathways, e.g., ghrelin synthesis/secretion and/or the GOAT enzyme. However, we do not know the effect of alcohol on GHSR-1a and/or GOAT.
Also, during the alcohol session, there was a PF-5190457 dose x time interaction for total ghrelin that was due to a late (8 h post drug and alcohol) increase in total ghrelin, but not acyl-ghrelin, in the PF-5190457 100 mg b.i.d. condition compared to the other conditions. This may represent a rebound of unacylated ghrelin secretion after GHS-R1a blockade, at the PF-5190457 dose of 100 mg b.i.d., while perhaps GOAT activity was limited or saturated. Albeit speculative, this hypothesis would explain the selective effect for total ghrelin, which represents mostly unacylated ghrelin [58,59,60,61,62,63]. However, this late increase in total ghrelin was absent in the drug dosing phase and became apparent after alcohol administration in our study (or an acute intravenous ghrelin challenge as in [31]). Further work should be done on the effect of alcohol on the downstream components of the ghrelin/GOAT/GHS-R system to understand the biobehavioral responses in humans in the context of alcohol consumption and modulation of the endogenous ghrelin system.
Apart from the alcohol session, PF-5190457 per se affected neither peripheral acyl-ghrelin concentrations during the drug dosing phase, a finding consistent with Denney et al. [31], nor total ghrelin concentrations. In contrast, there was a significant effect of PF-5190457 to reduce the acyl-to-total ghrelin ratio in the 100 mg b.i.d. condition compared to placebo. This indicates that either unacylated ghrelin (which is the majority of circulating total ghrelin [58,59,60,61,62,63]) is increasing, acyl-ghrelin is decreasing, or both, under PF-5190457. While little is known about the acyl-to-total ghrelin ratio in AUD individuals, Prader-Willi patients with a higher ratio, compared to those with lower ratio, exhibit more pronounced symptoms typical of that phenotype, such as hyperphagia and weight gain [64]. The reduction in the ratio in the PF-5190457 100 mg b.i.d. condition versus placebo may reflect changes to the ghrelin/GOAT/GHS-R system induced by PF-5190457, e.g., metabolic state, changes in hepatic clearance of acyl-ghrelin, differences between acyl-ghrelin and unacylated ghrelin clearance rates, availability of substrate (octanoate/octanoyl-CoA) and/or changes in GOAT activity [61, 62, 65, 66].
During the alcohol session, there was a late increase in IGF-1 concentrations for both drug conditions compared to placebo. Ghrelin stimulates GH release by the pituitary. IGF-1, a mediator of the effects of GH and negative regulator of GH secretion, holds a longer half-life compared to GH and is a surrogate measure of GH which has a pulsatile secretion [67]. As such, IGF-1 might represent a better biomarker of the downstream effects of GHS-R1a blockade with PF-5190457, at least in the context of alcohol administration.
Finally, we provided preliminary findings that PF-5190457 100 mg b.i.d. may reduce alcohol-primed craving over time and alcohol cue-elicited craving in a bar-like laboratory setting. By contrast, there was no effect on craving during drug dosing as assessed in a normal hospital room in absence of a priming or of cues in the bar-like laboratory. Therefore, the behavioral effects of PF-5190457 are apparent in the presence of stimuli that elicit craving such as cues and alcohol priming, both of which represent typical risks factor for relapse and heavy drinking [68]. These findings mirror our previous human laboratory study where we found a robust effect of intravenous acyl-ghrelin administration in increasing alcohol cue-induced craving [9]. During the CR procedure, we also exposed participants to personalized food cues to specifically control for non-alcoholic appetitive behaviors. Together, these findings are consistent with increasing preclinical evidence that GHS-R1a blockade may result in reduced reward processing and seeking behaviors to both alcohol [8, 17,18,19,20,21,22,23,24] and food [69]. These data must be interpreted with caution, however, given the small sample and the fixed order of the drug dosing. Future larger randomized trials are needed to test the efficacy of PF-5190457 in AUD patients.
It will also be relevant in the future to understand whether the effects of PF-5190457 are mediated centrally, peripherally or both. Phase 1a clinical studies with PF-5190457 were not terminated due to safety findings, rather, due to tachyphylaxis, which was, however, limited to peripheral but not central effects [31]. Indeed, Denney and colleagues [31] speculated that, while peripheral GHS-R1a was blocked 24/7, central blockade was only for a shorter period daily, which in turn may allow PF-05190457 to not lose efficacy. As such, the profile of PF-05190457 favors its use in centrally-mediated mechanisms [31]. Our rat experiments indicate PF-5190457 brain penetrance; however, this work was limited to measuring PF-5190457 concentrations in brain homogenates and we did not use any isotopically labeled PF-5190457 to test in vivo central target engagement. Investigations of rate, extent and distribution of PF-05190457 within the CNS and binding studies with radiolabeled compound remain the goal of future work.
In conclusion, this study provides evidence on the safety and tolerability of the GHS-R1a inverse agonist PF-5190457 in heavy drinkers during alcohol administration. The PK/ PD/behavioral findings further support future research towards investigating GHS-R1a as a novel pharmacological target to treat AUD.
References
Edwards S, Kenna GA, Swift RM, Leggio L. Current and promising pharmacotherapies, and novel research target areas in the treatment of alcohol dependence: a review. Curr Pharm Des. 2011;17:1323–32.
Jonas DE, Amick HR, Feltner C, Bobashev G, Thomas K, Wines R, et al. Pharmacotherapy for adults with alcohol use disorders in outpatient settings: a systematic review and meta-analysis. JAMA. 2014;311:1889–1900.
Kojima M, Hosoda H, Date Y, Nakazato M, Matsuo H, Kangawa K. Ghrelin is a growth-hormone-releasing acylated peptide from stomach. Nature. 1999;402:656–60.
Muller TD, Nogueiras R, Andermann ML, Andrews ZB, Anker SD, Argente J, et al. Ghrelin. Mol Metab. 2015;4:437–60.
Leggio L. Role of the ghrelin system in alcoholism: acting on the growth hormone secretagogue receptor to treat alcohol-related diseases. Drug News Perspect. 2010;23:157–66.
Howard AD, Feighner SD, Cully DF, Arena JP, Liberator PA, Rosenblum CI, et al. A receptor in pituitary and hypothalamus that functions in growth hormone release. Science. 1996;273:974–7.
Jerlhag E. Systemic administration of ghrelin induces conditioned place preference and stimulates accumbal dopamine. Addict Biol. 2008;13:358–63.
Jerlhag E, Egecioglu E, Landgren S, Salome N, Heilig M, Moechars D, et al. Requirement of central ghrelin signaling for alcohol reward. Proc Natl Acad Sci USA. 2009;106:11318–23.
Leggio L, Zywiak WH, Fricchione SR, Edwards SM, de la Monte SM, Swift RM, et al. Intravenous ghrelin administration increases alcohol craving in alcohol-dependent heavy drinkers: a preliminary investigation. Biol Psychiatry. 2014;76:734–41.
Farokhnia M, Grodin EN, Lee MR, Oot EN, Blackburn AN, et al. Exogenous ghrelin administration increases alcohol self-administration and modulates brain functional activity in heavy-drinking alcohol-dependent individuals. Mol Psychiatry. 2017. https://doi.org/10.1038/mp.2017.226.
Addolorato G, Capristo E, Leggio L, Ferrulli A, Abenavoli L, Malandrino N, et al. Relationship between ghrelin levels, alcohol craving, and nutritional status in current alcoholic patients. Alcohol Clin Exp Res. 2006;30:1933–7.
Badaoui A, De Saeger C, Duchemin J, Gihousse D, de Timary P, Starkel P. Alcohol dependence is associated with reduced plasma and fundic ghrelin levels. Eur J Clin Invest. 2008;38:397–403.
de Timary P, Cani PD, Duchemin J, Neyrinck AM, Gihousse D, Laterre PF, et al. The loss of metabolic control on alcohol drinking in heavy drinking alcohol-dependent subjects. PLoS ONE. 2012;7:e38682.
Leggio L, Ferrulli A, Cardone S, Nesci A, Miceli A, Malandrino N, et al. Ghrelin system in alcohol-dependent subjects: role of plasma ghrelin levels in alcohol drinking and craving. Addict Biol. 2012;17:452–64.
Koopmann A, von der Goltz C, Grosshans M, Dinter C, Vitale M, Wiedemann K, et al. The association of the appetitive peptide acetylated ghrelin with alcohol craving in early abstinent alcohol dependent individuals. Psychoneuroendocrinology. 2012;37:980–6.
Kraus T, Schanze A, Groschl M, Bayerlein K, Hillemacher T, Reulbach U, et al. Ghrelin levels are increased in alcoholism. Alcohol Clin Exp Res. 2005;29:2154–7.
Suchankova P, Engel JA, Jerlhag E. Sub-chronic ghrelin receptor blockade attenuates alcohol- and amphetamine-induced locomotor stimulation in mice. Alcohol Alcohol. 2016;51:121–7.
Kaur S, Ryabinin AE. Ghrelin receptor antagonism decreases alcohol consumption and activation of perioculomotor urocortin-containing neurons. Alcohol Clin Exp Res. 2010;34:1525–34.
Gomez JL, Ryabinin AE. The effects of ghrelin antagonists [D-Lys(3)]-GHRP-6 or JMV2959 on ethanol, water, and food intake in C57BL/6J mice. Alcohol Clin Exp Res. 2014;38:2436–44.
Gomez JL, Cunningham CL, Finn DA, Young EA, Helpenstell LK, Schuette LM, et al. Differential effects of ghrelin antagonists on alcohol drinking and reinforcement in mouse and rat models of alcohol dependence. Neuropharmacology. 2015;97:182–93.
Stevenson JR, Buirkle JM, Buckley LE, Young KA, Albertini KM, Bohidar AE. GHS-R1A antagonism reduces alcohol but not sucrose preference in prairie voles. Physiol Behav. 2015;147:23–29.
Stevenson JR, Francomacaro LM, Bohidar AE, Young KA, Pesarchick BF, Buirkle JM, et al. Ghrelin receptor (GHS-R1A) antagonism alters preference for ethanol and sucrose in a concentration-dependent manner in prairie voles. Physiol Behav. 2016;155:231–6.
Landgren S, Simms JA, Hyytia P, Engel JA, Bartlett SE, Jerlhag E. Ghrelin receptor (GHS-R1A) antagonism suppresses both operant alcohol self-administration and high alcohol consumption in rats. Addict Biol. 2012;17:86–94.
Suchankova P, Steensland P, Fredriksson I, Engel JA, Jerlhag E. Ghrelin receptor (GHS-R1A) antagonism suppresses both alcohol consumption and the alcohol deprivation effect in rats following long-term voluntary alcohol consumption. PLoS ONE. 2013;8:e71284.
Chollet C, Meyer K, Beck-Sickinger AG. Ghrelin—a novel generation of anti-obesity drug: design, pharmacomodulation and biological activity of ghrelin analogues. J Pept Sci Off Publ Eur Pept Soc. 2009;15:711–30.
Els S, Beck-Sickinger AG, Chollet C. Ghrelin receptor: high constitutive activity and methods for developing inverse agonists. Methods Enzymol. 2010;485:103–21.
Pantel J, Legendre M, Cabrol S, Hilal L, Hajaji Y, Morisset S, et al. Loss of constitutive activity of the growth hormone secretagogue receptor in familial short stature. J Clin Invest. 2006;116:760–8.
Holst B, Schwartz TW. Ghrelin receptor mutations—too little height and too much hunger. J Clin Invest. 2006;116:637–41.
Bhattacharya SK, Andrews K, Beveridge R, Cameron KO, Chen C, Dunn M, et al. Discovery of PF-5190457, a potent, selective, and orally bioavailable ghrelin receptor inverse agonist clinical candidate. ACS Med Chem Lett. 2014;5:474–9.
Kong J, Chuddy J, Stock IA, Loria PM, Straub SV, Vage C, et al. Pharmacological characterization of the first in class clinical candidate PF-05190457: a selective ghrelin receptor competitive antagonist with inverse agonism that increases vagal afferent firing and glucose-dependent insulin secretion ex vivo. Br J Pharmacol. 2016;173:1452–64.
Denney WS, Sonnenberg GE, Carvajal-Gonzalez S, Tuthill T, Jackson VM. Pharmacokinetics and pharmacodynamics of PF-05190457: the first oral ghrelin receptor inverse agonist to be profiled in healthy subjects. Br J Clin Pharmacol. 2017;83:326–38.
Haass-Koffler CLAF, Swift RM, Leggio L. Altering ethanol pharmacokinetics to treat alcohol use disorder: can you teach an old dog new tricks?. J Psychopharmacol. 2017;31:812–8.
Kung DW, Coffey SB, Jones RM, Cabral S, Jiao W, Fichtner M, et al. Identification of spirocyclic piperidine-azetidine inverse agonists of the ghrelin receptor. Bioorg Med Chem Lett. 2012;22:4281–7.
Ghareeb M, Leggio L, El-Kattan A, Akhlaghi F. Development and validation of an UPLC-MS/MS assay for quantitative analysis of the ghrelin receptor inverse agonist PF-5190457 in human or rat plasma and rat brain. Anal Bioanal Chem. 2015;407:5603–13.
Cippitelli A, Karlsson C, Shaw JL, Thorsell A, Gehlert DR, Heilig M. Suppression of alcohol self-administration and reinstatement of alcohol seeking by melanin-concentrating hormone receptor 1 (MCH1-R) antagonism in Wistar rats. Psychopharmacol. 2010;211:367–75.
Farokhnia M, Schwandt ML, Lee MR, Bollinger JW, Farinelli LA, et al. Biobehavioral effects of baclofen in anxious alcohol-dependent individuals: a randomized, double-blind, placebo-controlled, laboratory study. Transl Psychiatry. 2017;7:e1108.
Sobell LC, Brown J, Leo GI, Sobell MB. The reliability of the Alcohol Timeline Followback when administered by telephone and by computer. Drug Alcohol Depend. 1996;42:49–54.
MacLean AW, Fekken GC, Saskin P, Knowles JB. Psychometric evaluation of the Stanford Sleepiness Scale. J Sleep Res. 1992;1:35–39.
Martin CS, Earleywine M, Musty RE, Perrine MW, Swift RM. Development and validation of the Biphasic Alcohol Effects Scale. Alcohol Clin Exp Res. 1993;17:140–6.
Fraser HF, Van Horn GD, Martin WR, Wolbach AB, Isbell H. Methods for evaluating addiction liability. (A) “Attitude” of opiate addicts toward opiate-like drugs. (B) a short-term “direct” addiction test. J Pharmacol Exp Ther. 1961;133:371–87.
McNair DM, Lorr M, Droppleman LF Manual for the Profile of Mood States. Educational and Industrial Testing Services: San Diego, CA, 1971.
Nijs IM, Franken IH, Muris P. The modified Trait and State Food-Cravings Questionnaires: development and validation of a general index of food craving. Appetite. 2007;49:38–46.
Rohsenow DJ, Monti PM, Hutchison KE, Swift RM, Colby SM, Kaplan GB. Naltrexone’s effects on reactivity to alcohol cues among alcoholic men. J Abnorm Psychol. 2000;109:738–42.
Monti PM, Rohsenow DJ, Hutchison KE, Swift RM, Mueller TI, Colby SM, et al. Naltrexone’s effect on cue-elicited craving among alcoholics in treatment. Alcohol Clin Exp Res. 1999;23:1386–94.
Bohn MJ, Krahn DD, Staehler BA. Development and initial validation of a measure of drinking urges in abstinent alcoholics. Alcohol Clin Exp Res. 1995;19:600–6.
Rohsenow DJ, Monti PM, Rubonis AV, Sirota AD, Niaura RS, Colby SM, et al. Cue reactivity as a predictor of drinking among male alcoholics. J Consult Clin Psychol. 1994;62:620–6.
Leggio L, Zywiak WH, McGeary JE, Edwards S, Fricchione SR, Shoaff JR, et al. A human laboratory pilot study with baclofen in alcoholic individuals. Pharmacol Biochem Behav. 2013;103:784–91.
Leggio L, Zywiak WH, Edwards SM, Tidey JW, Swift RM, Kenna GA. A preliminary double-blind, placebo-controlled randomized study of baclofen effects in alcoholic smokers. Psychopharmacol. 2015;232:233–43.
Kenward MG, Roger JH. Small sample inference for fixed effects from restricted maximum likelihood. Biometrics. 1997;53:983–97.
Littell RC, Milliken GA, Stroup WW, Wolfinger RD, Schabenberger O. SAS for Mixed Models. Second edn. SAS Institute Inc: Cary, NC, 2006.
Clapp P, Bhave SV, Hoffman PL. How adaptation of the brain to alcohol leads to dependence: a pharmacological perspective. Alcohol Res Health. 2008;31:310–39.
Cruz MT, Herman MA, Cote DM, Ryabinin AE, Roberto M. Ghrelin increases GABAergic transmission and interacts with ethanol actions in the rat central nucleus of the amygdala. Neuropsychopharmacology. 2013;38:364–75.
Ralevski E, Horvath TL, Shanabrough M, Hayden R, Newcomb J, Petrakis I. Ghrelin is supressed by intravenous alcohol and is related to stimulant and sedative effects of alcohol. Alcohol Alcohol. 2017;52:431–8.
Calissendorff J, Gustafsson T, Holst JJ, Brismar K, Rojdmark S. Alcohol intake and its effect on some appetite-regulating hormones in man: influence of gastroprotection with sucralfate. Endocr Res. 2012;37:154–62.
Calissendorff J, Danielsson O, Brismar K, Rojdmark S. Inhibitory effect of alcohol on ghrelin secretion in normal man. Eur J Endocrinol. 2005;152:743–7.
Calissendorff J, Danielsson O, Brismar K, Rojdmark S. Alcohol ingestion does not affect serum levels of peptide YY but decreases both total and octanoylated ghrelin levels in healthy subjects. Metabolism. 2006;55:1625–9.
Zimmermann US, Buchmann A, Steffin B, Dieterle C, Uhr M. Alcohol administration acutely inhibits ghrelin secretion in an experiment involving psychosocial stress. Addict Biol. 2007;12:17–21.
Tong J, Dave N, Mugundu GM, Davis HW, Gaylinn BD, Thorner MO, et al. The pharmacokinetics of acyl, des-acyl, and total ghrelin in healthy human subjects. Eur J Endocrinol. 2013;168:821–8.
Bang AS, Soule SG, Yandle TG, Richards AM, Pemberton CJ. Characterisation of proghrelin peptides in mammalian tissue and plasma. J Endocrinol. 2007;192:313–23.
Hosoda H, Kojima M, Mizushima T, Shimizu S, Kangawa K. Structural divergence of human ghrelin. Identification of multiple ghrelin-derived molecules produced by post-translational processing. J Biol Chem. 2003;278:64–70.
Howick K, Griffin BT, Cryan JF, Schellekens H. From Belly to Brain: targeting the ghrelin receptor in appetite and food intake regulation. Int J Mol Sci. 2017;18 pii: E273.
Liu J, Prudom CE, Nass R, Pezzoli SS, Oliveri MC, Johnson ML, et al. Novel ghrelin assays provide evidence for independent regulation of ghrelin acylation and secretion in healthy young men. J Clin Endocrinol Metab. 2008;93:1980–7.
Takagi K, Legrand R, Asakawa A, Amitani H, Francois M, Tennoune N, et al. Anti-ghrelin immunoglobulins modulate ghrelin stability and its orexigenic effect in obese mice and humans. Nat Commun. 2013;4:2685.
Kuppens RJ, Diene G, Bakker NE, Molinas C, Faye S, Nicolino M, et al. Elevated ratio of acylated to unacylated ghrelin in children and young adults with Prader-Willi syndrome. Endocrine. 2015;50:633–42.
Kirchner H, Gutierrez JA, Solenberg PJ, Pfluger PT, Czyzyk TA, Willency JA, et al. GOAT links dietary lipids with the endocrine control of energy balance. Nat Med. 2009;15:741–5.
Wren AM, Small CJ, Ward HL, Murphy KG, Dakin CL, Taheri S, et al. The novel hypothalamic peptide ghrelin stimulates food intake and growth hormone secretion. Endocrinology. 2000;141:4325–8.
Anil Kumar P, Welsh GI, Saleem MA, Menon RK. Molecular and cellular events mediating glomerular podocyte dysfunction and depletion in diabetes mellitus. Front Endocrinol. 2014;5:151.
Shaham Y, Shalev U, Lu L, De Wit H, Stewart J. The reinstatement model of drug relapse: history, methodology and major findings. Psychopharmacol. 2003;168:3–20.
Dickson SL, Egecioglu E, Landgren S, Skibicka KP, Engel JA, Jerlhag E. The role of the central ghrelin system in reward from food and chemical drugs. Mol Cell Endocrinol. 2011;340:80–87.
Acknowledgements
This work was supported by NIH intramural funding ZIA-AA000218 (Section on Clinical Psychoneuroendocrinology and Neuropsychopharmacology; PI: Dr. Lorenzo Leggio), jointly supported by the Division of Intramural Clinical and Biological Research of the National Institute on Alcohol Abuse and Alcoholism (NIAAA) and the Intramural Research Program of the National Institute on Drug Abuse (NIDA); and by the National Center for Advancing Translational Sciences (NCATS) grant UH2/UH3-TR000963 (PIs: Drs Lorenzo Leggio and Fatemeh Akhlaghi). The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.The authors would like to thank the clinical and research staff involved in data collection and support at the NIAAA Division of Intramural Clinical and Biological Research, i.e., in the NIAAA/NIDA Section on Clinical Psychoneuroendocrinology and Neuropsychopharmacology (in particular Christian Frable, Allison Daurio and Sara Deschaine), in the Section on Molecular Pathophysiology (in particular Andrew Pilling and Caroline Rauffenbart) and in the NIAAA clinical intramural program. The authors would also like to thank the research staff involved in samples and data analysis in the Clinical Pharmacokinetics Research Laboratory at the University of Rhode Island (in particular Anitha Sravankumar, Ben Barlock and Sravani Adusumalli). The authors would also like to thank the clinical and research staff involved in data collection and patient care at the NIH Clinical Center, i.e., in the Department of Nursing (in particular the nurses of the 1SE Inpatient Unit and of the 1-HALC 1SE Outpatient Clinic), in the Department of Nutrition (in particular LT Kelly Ratteree, MPH, RDN and CDR Merel Kozlosky, MS, RD) and in the Department of Pharmacy. The authors would also like to thank Ms. Karen Smith and Ms. Holly Thompson from the NIH Library for bibliographic assistance. Furthermore, the authors would like to express their gratitude to the participants who took part in this study. Finally, the authors would like to thank the Steering Committee of the UH2/UH3-TR000963 grant (PIs: Drs Lorenzo Leggio and Fatemeh Akhlaghi) whose members included members from the NIAAA Division of Medication Development (in particular Dr. Joanne Fertig), the Drug Development Partnership Programs of the National Center for Advancing Translational Sciences (NCATS) and Pfizer, which kindly provided the study drug under the NCATS grant UH2/UH3-TR000963. Pfizer did not have any role in the study design, execution or interpretation of the results, and this publication does not necessarily represent the official views of Pfizer.
Author contributions
Study neuroscientific basis, rationale, concept and design: LL; Provided funding: LL, MH, and FA; Statistical analysis: MRL, JDT, MLS, and FA; Acquisition and management of data: MRL, JDT, MG, AAD, ANL, EC, LAF, SB, MF, MH, FA, and LL; Clinical and Safety monitoring: MRL, and LL; Administrative, technical, or material support: MRL, JDT, MG, MLS, AAD, ANL, EC, LAF, SB, MF, MH, FA, and LL; Analysis and interpretation of data: MRL, JDT, MG, MLS, AAD, ANL, EC, LAF, SB, MF, MH, FA, and LL; Drafting the manuscript: MRL, and LL. All authors have critically reviewed the manuscript for important intellectual content and approved the final version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Lee, M.R., Tapocik, J.D., Ghareeb, M. et al. The novel ghrelin receptor inverse agonist PF-5190457 administered with alcohol: preclinical safety experiments and a phase 1b human laboratory study. Mol Psychiatry 25, 461–475 (2020). https://doi.org/10.1038/s41380-018-0064-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-018-0064-y
- Springer Nature Limited
This article is cited by
-
GHSR blockade, but not reduction of peripherally circulating ghrelin via β1-adrenergic receptor antagonism, decreases binge-like alcohol drinking in mice
Molecular Psychiatry (2024)
-
Ghrelin decreases sensitivity to negative feedback and increases prediction-error related caudate activity in humans, a randomized controlled trial
Neuropsychopharmacology (2024)
-
Des-acyl ghrelin reduces alcohol intake and alcohol-induced reward in rodents
Translational Psychiatry (2024)
-
Pharmacological Treatments for Alcohol Use Disorder: Considering the Role of Sex and Gender
Current Addiction Reports (2024)
-
Behandlungsstrategien bei Patient:innen mit Alkoholkonsumstörung und eingeschränkter Leberfunktion
psychopraxis. neuropraxis (2024)