Abstract
Objective
To determine the rate, maternal characteristics, timing, and indicators of severe maternal morbidity (SMM) that occurs at postpartum readmission.
Study design
Women with a birth in California during 2008–2012 were included in the analysis. Readmissions up to 42 days after delivery were investigated. SMM was defined as presence of any of the 21 indicators defined by ICD-9 codes.
Results
Among 2,413,943 women with a birth, SMM at readmission occurred in 4229 women. Of all SMM, 12.1% occurred at readmission. Over half (53.5%) of the readmissions with SMM occurred within the first week after delivery hospitalization. The most common indicators of SMM were blood transfusion, sepsis, and pulmonary edema/acute heart failure.
Conclusion
Twelve percent of SMM was identified at readmission with the majority occurring within 1 week after discharge from delivery hospitalization. Because early readmission may reflect lack of discharge readiness, there may be opportunities to improve care.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
In the United States, there has been a steady increase in pregnancy-related mortality and severe maternal morbidity (SMM) [1, 2]. Based on vital statistics, maternal mortality increased by 26.6% during 2000–2014 [3], and SMM during delivery hospitalizations doubled during 1998–2011 [1].
With the documented increase in pregnancy-related mortality, it has been suggested that more careful investigation of SMM, which is almost 50 times more common than maternal death, could provide clinically-relevant measures for quality of maternal care [4]. However, the current knowledge of SMM and its causes is mostly limited to studies of delivery hospitalization [5, 6]. The investigation of SMM at postpartum readmission has been limited to a single large dataset study that did not link the delivery and readmission hospitalizations [1]. Nevertheless, using ICD-9 codes, this study reported that in the period of 2008–2009, for every 10,000 delivery hospitalizations, there were 129 delivery hospitalizations and 29 postpartum hospitalizations with at least one severe complication [1]. Thus, so far there have not been longitudinal investigations of the prevalence and characteristics of SMM that presents at postpartum readmission. To understand the totality of SMM, we wanted to focus on the morbidity presenting at postpartum readmission in order to improve care.
We investigated SMM that occurred during postpartum readmissions up to 42 days after discharge from delivery hospital, using linked birth cohort files for California births. Our specific study aims were to determine (1) the rate of SMM that occurs at postpartum readmission, (2) the maternal characteristics among women with SMM at readmission, (3) the timing of readmission with SMM, and (4) the common indicators of SMM at readmission.
Material and methods
We performed a cohort study using the California birth cohorts from 2008–2012, which link the birth records with Office of Statewide Health and Planning maternal and infant hospital discharge data during pregnancy through postpartum period. The datasets include maternal and pregnancy characteristics from birth certificates and discharge diagnosis and procedure codes from maternal antenatal, intrapartum and postpartum hospitalizations [7]. Stanford University Institutional Review Board and the California State Committee for the Protection of Human Subjects reviewed and approved this study before its initiation.
From 2008 to 2012, a total of 2,637,896 California women had a hospital delivery of a live birth or a fetal death after 20 weeks of gestation including singleton and multifetal gestations. We excluded women with unlinked mother-delivery records (n = 96,852), records with a missing gestational age (n = 66,405), women who died before discharge from the delivery hospital (n = 113), and pregnancies with gestational age <20 weeks or >45 weeks (n = 21,929, to minimize data errors). Women who had multiple gestations were included, but we included only one delivery record for each multiple-gestation delivery (n = 38,654 duplicate records excluded), leaving 2,413,943 women for analysis. Information on fetal deaths was only available for years 2008–2011, not for 2012. For women who were transferred as part of their delivery-related hospitalization, we included diagnosis and procedure codes from all relevant contiguous hospitalizations.
We investigated readmissions up to 42 days after discharge from delivery hospital. SMM was defined as presence of any of the 21 SMM indicators based on International Classification of Disease, 9th Edition, Clinical Modification (ICD-9) diagnosis or procedure codes as recommended by the Centers for Disease Control and Prevention (see Supplementary information) [8, 9]. To avoid the bias of multiple readmissions, we limited the investigation of indicators of SMM at readmission to the first postpartum readmission.
We compared maternal characteristics of women with SMM at readmission to women with no SMM at readmission and to women with no readmission. Maternal age at delivery, race/ethnicity, parity, education, insurance type for prenatal care, the timing of initiation of prenatal care, prepregnancy weight, and height were from the birth certificate. Prepregnancy body mass index was calculated from maternal weight and height. Maternal comorbidities were obtained from ICD-9 diagnosis codes at delivery or postpartum hospitalization record and/or birth certificate. Cesarean delivery was reported either in the delivery hospitalization record or on the birth certificate.
We investigated the timing of readmission with SMM by week within 42 days of discharge from delivery hospital. All readmissions for each woman were calculated within 42 days of discharge. We assessed the distribution of 21 SMM indicators among women with SMM at readmission. In order to determine whether events or conditions at delivery admission would predict readmission with SMM in this longitudinal dataset, we selected the three most common indicators for SMM at readmission and looked for possible predictors at delivery admission.
Statistical analysis was performed using SAS program SAS 9.4 (SAS Institute, Cary, NC). Women with missing data for any of the variables were excluded from the analysis. We calculated the frequencies of SMM during delivery and readmission hospitalizations. Comparisons between groups were performed using Chi-square test for categorical variables and ANOVA for continuous variables. The level of significance was set at p < 0.05.
Results
Among 2,413,943 women included in the analysis, 24,442 (1.0% of all women) had one or more postpartum readmissions within 42 days of delivery. Of these women, 4229 (17.3% of women with readmission) had SMM at readmission.
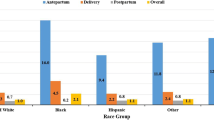
In Table 1, we present the maternal and obstetric characteristics of women with SMM at readmission compared with those without SMM at readmission and to those with no readmission. Compared with women with readmission but no SMM and to women with no readmission, those with SMM at readmission were older, more likely to be non-Hispanic black, less likely to be Hispanic, more educated, and more often had private insurance and a multifetal gestation. In addition, they more often had SMM at delivery hospitalization, a cesarean delivery, a preexisting comorbidity, or a pregnancy complication. The mean length of stay at delivery hospitalization for all three groups was 2.6–2.7 days (Table 1).
In addition to 4229 women who had SMM at readmission, 34,830 women had SMM at delivery admission, thus, 12.1 percent of SMM occurred at readmission. Only 459 women had SMM at both delivery and at readmission.
In Fig. 1, we present the timing of readmission with SMM. The majority of readmissions with SMM (53.5%) occurred during the first week after discharge from delivery hospitalization (Fig. 1).
The indicators of SMM are presented in Table 2. The three most common indicators of SMM at readmission were blood transfusion (40.3%), sepsis (21.7%), and pulmonary edema/acute heart failure (17.0%); whereas the frequencies of other causes were <10% each (Table 2). Of 1704 women with blood transfusion as an SMM indicator at readmission, 181 (10.6%) had anemia coded at delivery hospitalization and 42 (2.5%) had postpartum hemorrhage coded at delivery hospitalization. Of 918 women with sepsis as an SMM indicator at readmission, only 42 (4.6%) had chorioamnionitis at delivery. Similarly, of 718 women with pulmonary edema/acute heart failure as an SMM indicator at readmission, 15 (2.1%) had adult respiratory distress syndrome at delivery, 12 (1.7%) had acute renal failure, and 10 (1.4%) had heart failure/arrest during surgery or procedure.
Discussion
Our results from a diverse population-based cohort in California show that over twelve percent of women with SMM were identified at the postpartum readmission. About half of readmissions with SMM occurred within the first week of discharge from delivery hospital.
National attention has focused on reducing maternal mortality and SMM [1, 2, 4]. However, few studies have specifically focused on investigating SMM occurring during postpartum readmission—a vital component in understanding the overall burden. Harvey and colleagues investigated the risk of hospital encounters within one year after SMM during delivery hospitalization among women with no preexisting medical conditions [6]. They found that having severe morbidity at delivery increased a woman’s risk of postpartum hospitalization by twofold [6]. These results are in line with our finding that women with postpartum readmission with SMM were more likely to have had SMM at delivery hospitalization. By including women with various preexisting conditions, we believe that our data provide a more complete picture of SMM.
In a large nationwide study, Callaghan et al. using ICD-9 codes reported that in the period of 2008–2009, for every 10,000 delivery hospitalizations, there were 129 delivery hospitalizations and 29 postpartum hospitalizations with at least one severe complication [1]. For comparison, using linked maternal hospital discharge and birth certificate data, we were able to report that approximately twelve percent of all SMM occurred at postpartum readmission. Thus, a significant number of women at risk for SMM remain unidentified during delivery hospitalization. Furthermore, over half of the readmissions with severe morbidity occurred during the first week after discharge from the delivery hospitalization.
We found significant differences in demographic and medical/obstetric characteristics at delivery between those with SMM at readmission vs. those without SMM at readmission vs. those without a readmission. Perhaps, these differences are driven by maternal age, cesarean delivery, and comorbidities. In addition, we looked for potential predictors for SMM at readmission present at the delivery admission. Few women with SMM at readmission had precursor conditions coded at delivery admission. Although these predictors at delivery for SMM at readmission may have been undercoded, it seems more likely that events leading to SMM solely representing at readmission had an onset after the delivery admission.
We found that the leading indicators of SMM at readmission were blood transfusion (an indicator of hemorrhage), sepsis, and pulmonary edema/acute heart failure. Previously, two studies have reported causes of maternal readmission, but neither examined indicators of SMM among women with readmission [10, 11]. Belfort et al. investigated readmissions (irrespective of SMM) within 6 weeks after delivery and showed that the major causes were infectious in origin [10]. This is in line with our finding of sepsis being within the three most common indicators of SMM at readmission. Clapp et al. found that among all postpartum readmissions occurring within the first 6 weeks after delivery, the most common causes were hypertensive disorder, wound infection or breakdown, psychiatric disease, and uterine infection (9). These results are also supported by our findings of sepsis and acute heart failure being within the top three indicators of SMM at readmission.
Strengths of our study include a large and diverse population-based cohort we used for this analysis. We examined deliveries during a relatively recent time period, and it is unlikely that the obstetric practice in California has changed substantially since that time. We were able to link the hospital admission with subsequent readmissions and investigate the presence of SMM at readmission. Furthermore, we were able to give details of SMM at readmission including maternal characteristics, the timing and the most common indicators.
Our study is not without limitations. The SMM indicators investigated in this study were defined based on the ICD-9 diagnosis and procedure codes used for billing purposes and might therefore be subject to miscoding or missing information. Although the California population is diverse and large (1 in 8 births in the United States are in California), we acknowledge that limiting our study cohort to one state might affect the generalizability of our results.
Our unique observations in this study are that over twelve percent of women with SMM present at postpartum readmission and that over half of the readmissions with severe morbidity occur within 1 week of discharge from the delivery hospitalization. Because early readmission with SMM may reflect lack of discharge readiness, there may be opportunities to improve care.
References
Callaghan WM, Creanga AA, Kuklina EV. Severe maternal morbidity among delivery and postpartum hospitalizations in the United States. Obstet Gynecol. 2012;120:1029–36.
Creanga AA, Berg CJ, Syverson C, Seed K, Bruce FC, Callaghan WM. Pregnancy-related mortality in the United States, 2006-2010. Obstet Gynecol. 2015;125:5–12.
MacDorman MF, Declercq E, Cabral H, Morton C. Recent Increases in the U.S. Maternal Mortality Rate: Disentangling Trends From Measurement Issues. Obstet Gynecol. 2016;128:447–55.
D’Alton ME. Where is the “M” in maternal-fetal medicine? Obstet Gynecol. 2010;116:1401–4.
Grobman WA, Bailit JL, Rice MM, Wapner RJ, Reddy UM, Varner MW, et al. Frequency of and factors associated with severe maternal morbidity. Obstet Gynecol. 2014;123:804–10.
Harvey EM, Ahmed S, Manning SE, Diop H, Argani C, Strobino DM. Severe maternal morbidity at delivery and risk of hospital encounters within 6 weeks and 1 year postpartum. J Womens Health. 2018;27:140–7.
Lyndon A, Lee HC, Gilbert WM, Gould JB, Lee KA. Maternal morbidity during childbirth hospitalization in California. J Matern Fetal Neonatal Med. 2012;25:2529–35.
CDC. Severe maternal morbidity in the United States. 2017. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/severematernalmorbidity.html#anchor_SMM. Accessed 20 Dec 2018.
Council on Patient Safety in Women’s Health Care. 2018. https://safehealthcareforeverywoman.org/aim-data/. Accessed 20 Dec 2018.
Belfort MA, Clark SL, Saade GR, Kleja K, Dildy GA, Teelkien VR, et al. Hospital readmission after delivery: evidence for an increased incidence of nonurogenital infection in the immediate postpartum period. Am J Obstet Gynecol. 2010;202:35.e1–7.
Clapp MA, Little SE, Zheng J, Robinson JN. A multi-state analysis of postpartum readmissions in the United States. Am J Obstet Gynecol. 2016;215:113.e1–10.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Girsen, A.I., Sie, L., Carmichael, S.L. et al. Rate and causes of severe maternal morbidity at readmission: California births in 2008–2012. J Perinatol 40, 25–29 (2020). https://doi.org/10.1038/s41372-019-0481-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-019-0481-z
- Springer Nature America, Inc.
This article is cited by
-
Risk factors for postpartum readmission: a prediction model in Iranian pregnant women
BMC Pregnancy and Childbirth (2024)
-
The effect of severe maternal morbidity on infant costs and lengths of stay
Journal of Perinatology (2022)